To the Editor,
In rare cases, cholangiocellular carcinoma (CCC) is associated with a paraneoplastic leukemoid reaction (PLR), but on presentation, it also occasionally mimics a pyogenic liver abscess with pyrexia and leukocytosis [1]. Consequently, potential pitfalls exist in the diagnosis of a PLR as the first manifestation of CCC. Here we present a case of CCC with a PLR mimicking an abscess in a patient who presented with pyrexia and leukocytosis.
A 63-year-old man was admitted to the hospital with intermittent fever occurring over the past 1 month. He also complained of anorexia and progressive generalized weakness. His body temperature was 39℃. Laboratory tests showed a white blood cell (WBC) count of 22,800/µL, with 78.3% neutrophils. The blood chemistry profile was as follows: total bilirubin 0.26 mg/dL, aspartate aminotransferase 27 U/L, alanine aminotransferase 15 U/L, total protein 6.7 g/dL, and albumin 2.5 g/dL. C-reactive protein was 20.2 mg/dL (normal range < 0.3). The coagulation profile was within normal limits. Tests for serum tumor markers showed normal levels of α-fetoprotein (2.8 ng/mL), protein induced by the absence of vitamin K or antagonist II (12 mAU/mL), carbohydrate antigenic determinant (CA19-9; 35.5 U/mL), and carcinoembryonic antigen (6.2 ng/mL). Serologic tests for hepatitis B and C were negative. Computed tomography (CT) of the chest and abdomen did not demonstrate lesions in the lungs but did show a 3.8-cm centrally hypodense lesion with rim enhancement in segment 4 of the liver (Fig. 1).
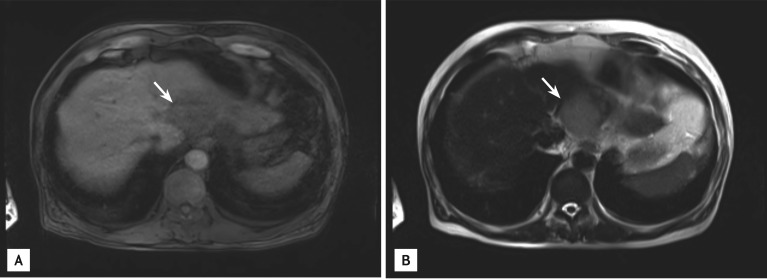
Figure 1.
Arterial-phase helical computed tomography showed a 3.8-cm rim-enhancing, centrally hypodense lesion in segment 4 of the liver.
Initially, an early liver abscess was suspected. However, ultrasonography-guided aspiration or drainage was impossible due to its immature appearance. Accordingly, the patient was given antibiotics intravenously for 14 days, but the fever did not subside, and the WBC count increased to 33,000/µL. Blood cultures were negative for bacteria and fungi. Follow-up liver ultrasonography still failed to show the features of a mature liver abscess, leading us to question our initial diagnosis. We therefore re-evaluated the rim-enhancing centrally hypodense liver lesion and the extreme leukocytosis. Gadoxetate-disodium-enhanced magnetic resonance imaging 10 days after hospitalization showed low T1 and high T2 signal intensities, rim-like arterial enhancement, and a washout lesion in the left lobe of the liver (Fig. 2). An ultrasonography-guided biopsy was performed after 2 weeks of hospitalization. Microscopic examination showed poorly differentiated malignant cells positive for cytokeratin (CK) 7 and CK19 and negative for CK20 and hepatocyte-specific antigen (Fig. 3), suggestive of CCC. Even though infection including a pyogenic liver abscess was excluded, neither the extreme leukocytosis, up to 33,000/µL with 94% segmented neutrophils, nor the fever subsided. Because both may be caused by leukemia, bone marrow examination was performed. The possibility of leukemia was excluded by the bone marrow examination. Based on the above, we concluded that the extreme leukocytosis with pyrexia was a PLR of the CCC.
Figure 2.
Magnetic resonance imaging findings in the liver showed a round nodule with a low signal intensity (arrow) on T1-weighted images (A) and a high signal intensity (arrow) on T2-weighted images (B) in the left hepatic lobe.
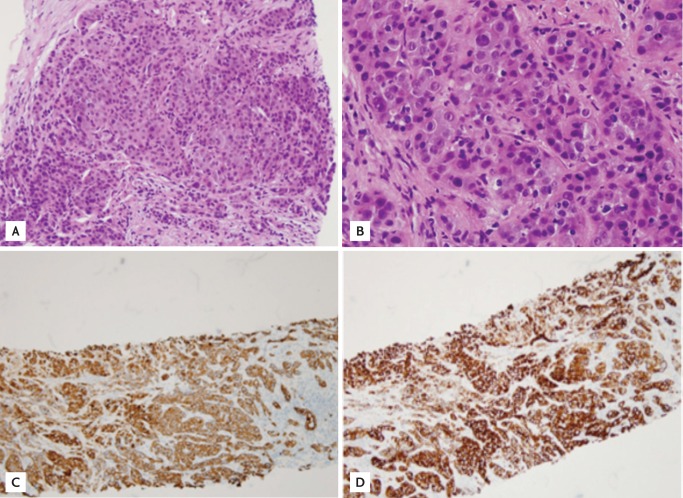
Figure 3.
Microscopic findings of the tumor. Hematoxylin and eosin staining showed poorly differentiated malignant cells suggestive of adenocarcinoma (A, ×100; B, ×400). Positive staining of the tumor cells for (C) cytokeratin 7 (×100) and (D) cytokeratin 19 (×100) was seen on immunohistochemical examination.
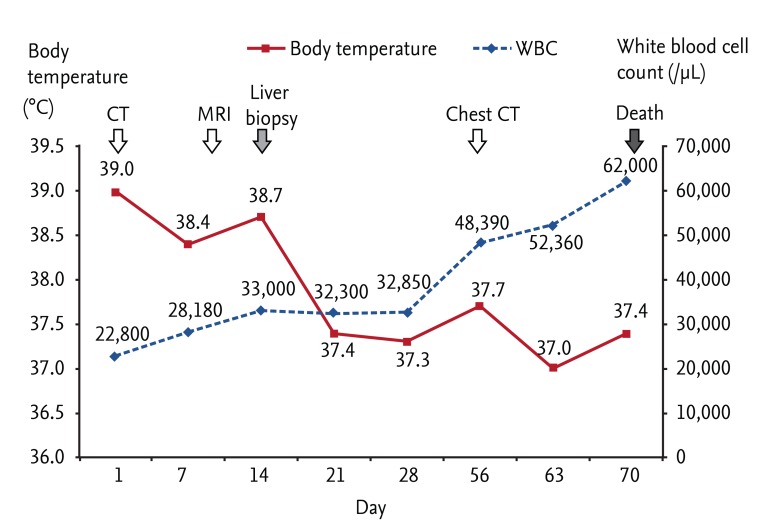
Surgical resection of the liver mass was suggested after 3 weeks of hospitalization. However, it was refused initially by the family because of the patient's deteriorating condition; 2 months after his initial hospitalization, the family was finally persuaded by the doctor to allow surgery. Preoperative chest CT revealed multiple new metastatic lung nodules (Fig. 4), which had not been seen 2 months earlier, and surgery was therefore postponed. The patient's condition deteriorated progressively despite supportive management, and his WBC count increased to 62,000/µL (Fig. 5). He rapidly became hypoxic and hypotensive. On day 71 after admission, he died due to cardiorespiratory failure. Rapid progression of CCC with a PLR was presumed to be the cause of death based on negative blood and urine cultures and the absence of signs of pneumonia on chest X-ray.
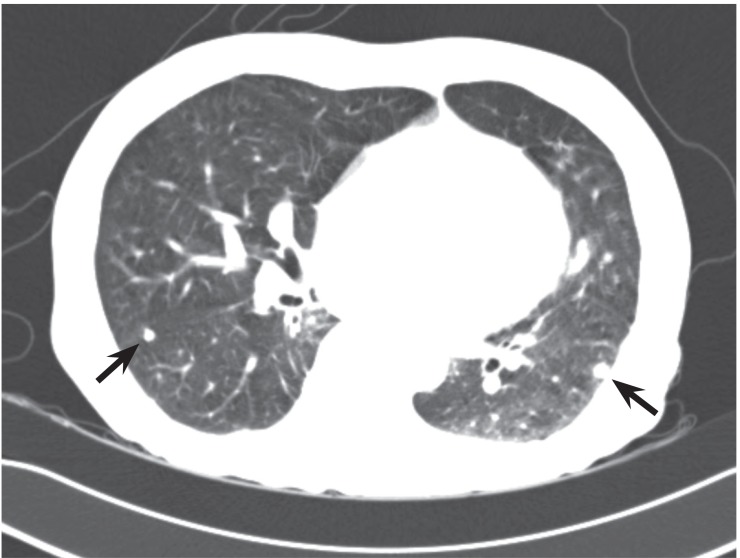
Figure 4.
Computed tomography of the chest showed newly developed multiple pulmonary nodules (black arrows) suggestive of metastasis.
Figure 5.
The clinical course of body temperature and white blood cell (WBC) counts beginning from initial hospitalization. CT, computed tomography; MRI, magnetic resonance imaging.
A leukemoid reaction refers to a neutrophil-dominant leukocytosis > 50,000/µL, which excludes leukemia. A PLR is a leukemoid reaction that occurs in association with cancer and is thought to be induced by paracrine molecules released from tumor cells. Lung, gastrointestinal, and genitourinary cancers, hepatocellular carcinoma, melanoma, and sarcoma may be associated with a PLR. However, it remains a diagnosis of exclusion, because severe infections or certain drugs can also cause extreme leukocytosis [2].
A PLR is rarely reported in CCC, which on its own has a poor prognosis. To our knowledge, only two cases of a PLR in patients with CCC have been documented [3,4]. The differentiation of CCC from a pyogenic liver abscess can be challenging, because the radiographic findings of a liver abscess can vary depending on the degree of maturation and internal contents. Hepatic abscesses mimicking CCC have often been reported. In most cases, those that mimic a malignant hepatic tumor can usually be identified as true liver abscesses based on the laboratory findings and clinical symptoms [1]. In our patient, radiographic findings, leukocytosis, fever, and a normal CA19-9 level suggested an early liver abscess, but the abscess-mimicking mass-like lesion was unresponsive to antibiotics, thus favoring a diagnosis of malignancy. Our difficulty in differentiating CCC with a PLR from a liver abscess was largely due to the overlapping radiological, clinical, and laboratory findings.
Malignant tumors with a PLR are aggressive with a poor prognosis usually. Management of patients with a PLR involves treating the underlying condition, although a PLR usually manifests during the late stages of cancer [5]. It has been suggested that the degree of leukocytosis is associated with tumor burden in malignant tumors with a PLR. In our case, the patient presented at an early stage, based on the tumor size and WBC count. However, his CCC with a PLR was fatal, because the diagnosis was delayed due to radiological, clinical, and laboratory findings overlapping those of a hepatic abscess, thus resulting in deterioration of the patient's condition and delayed treatment.
As evidenced by our case, even if the clinical and laboratory findings suggest a liver abscess, an abscess-mimicking liver lesion should also be considered and differentiated from CCC with a PLR. In patients with an abscess-mimicking hepatic nodule, pyrexia, and extreme leukocytosis, a prompt diagnostic approach to identify the underlying cause and thus the most effective treatment might result in a better prognosis.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Li C, Li G, Miao R, et al. Primary liver cancer presenting as pyogenic liver abscess: characteristics, diagnosis, and management. J Surg Oncol. 2012;105:687–691. doi: 10.1002/jso.22103. [DOI] [PubMed] [Google Scholar]
- 2.Granger JM, Kontoyiannis DP. Etiology and outcome of extreme leukocytosis in 758 nonhematologic cancer patients: a retrospective, single-institution study. Cancer. 2009;115:3919–3923. doi: 10.1002/cncr.24480. [DOI] [PubMed] [Google Scholar]
- 3.Aizawa M, Koshiyama H, Inoue D, et al. Postoperative aggravation of hypercalcemia-leukocytosis syndrome in a case of squamous cell type cholangiocarcinoma. Intern Med. 1997;36:232. doi: 10.2169/internalmedicine.36.232. [DOI] [PubMed] [Google Scholar]
- 4.Sohda T, Shiga H, Nakane H, Watanabe H, Takeshita M, Sakisaka S. Cholangiocellular carcinoma that produced both granulocyte-colony-stimulating factor and parathyroid hormone-related protein. Int J Clin Oncol. 2006;11:246–249. doi: 10.1007/s10147-006-0560-y. [DOI] [PubMed] [Google Scholar]
- 5.McKee LC., Jr Excess leukocytosis (leukemoid reactions) associated with malignant diseases. South Med J. 1985;78:1475–1482. doi: 10.1097/00007611-198512000-00018. [DOI] [PubMed] [Google Scholar]