Abstract
Background
Food insecurity is a known barrier to medication adherence among people living with HIV. Antiretroviral therapies (ART) that require food for maximum benefit likely pose added challenges to patients who do not have reliable access to food. This study examines the health implications of prescribing ART that requires food to patients who are food insecure.
Method
A community sample of 538 men and 221 women currently taking ART to treat their HIV infection completed computerized interviews, biweekly-unannounced pill count adherence assessments, and obtained their CD4 cell count and HIV RNA from medical records.
Results
Sixty-three percent of participants experienced at least one indicator of food insecurity during the previous month, of which 274 (57%) were prescribed an ART regimen that requires food. Among participants who were food insecure, individuals taking ART requiring food indicated significantly greater HIV symptoms, lower CD4 cell counts, and poorer HIV suppression. For participants who were food secure, those taking ART that requires food were significantly less adherent than those whose ART regimen does not require food.
Conclusions
People living with HIV who experience food insecurity are significantly more likely to be prescribed ART regimens that require food and experience poorer treatment outcomes. Determination of optimal ART regimens should take patient access to food into account and treatment guidelines should highlight the importance of food access in selecting ART regimens.
Keywords: HIV treatment adherence, food insecurity, antiretroviral
Introduction
Food insecurity is a significant barrier to antiretroviral therapy (ART) adherence in resource-rich as well as resource-limited settings. (1–3) In urban centers with abundant but inequitable access to food, people living with HIV who experience food insecurity are less likely to adhere to ART, have poorer HIV viral suppression, and have greater mortality. (4–7) Food insecurity itself can interfere with medication adherence by disrupting daily routines. In addition, food is recommended for processing, absorption, and optimal clinical benefits for certain ART regimens. For example, pharmacokinetic studies show as much as a 30% increase in the availability of darunavir (Prezista) when taken with food. Similarly, administration of atazanavir (Reyataz) with a light meal increases drug plasma concentration by 70%. (8) People who are food insecure must therefore periodically choose to either take their medications knowing they are not following directions or miss their medications altogether when food is unavailable. Prescribing ART that requires food to those who are food insecure could therefore diminish the efficacy of ART even when patients are adherent. We are not aware of prior research that has examined treatment outcomes in relation to requirements that ART be taken with food among people living with HIV who experience food insecurity.
We examined the modifying effects of food insecurity on the association between antiretroviral regimen and treatment outcomes. We hypothesized an interaction would exist between ART regimens that require food and experiencing food insecurity such that adherence and viral suppression would be impeded among people living with HIV who are both food insecure and prescribed ART that requires food.
Methods
Participants
Participants were 538 men and 221 women recruited from community services and infectious disease clinics during a 12-month period between 2013 and 2014. The site of the study was Atlanta, Georgia with an annual HIV incidence of 30.3 per 100,000. Eligible participants were age 18 or older, HIV positive, and currently taking ART.
Measures
Participants provided three sources of data: audio-computer assisted self-interviews (ACASI) (9, 10); HIV RNA (viral load) and CD4 cell counts from medical records; and unannounced pill counts to assess ART regimens and adherence. The university Institutional Review Board approved all procedures.
Computerized Interviews
Participants reported demographic characteristics, completed a measure of 14 HIV-related symptoms of 2-weeks duration (11) and their experience of 11 common ART side-effects (ranged between 0 = not experiencing to 3 = severely experiencing, summed to composite score). (12) To assess food insecurity we adapted eight items from the US Food Security Scale. (13) The specific items were selected to represent an array of individual and household food insecurity that ranged in severity. We adapted the items to reflect experiences in the previous month rather than past year to coincide with the timeframe of other measures. Food insecurity indicators were dichotomized (experienced/not experienced) and summed to create a food insecurity index.
HIV Viral Load and CD4 Cell Counts
We used a participant assisted method for collecting chart abstracted HIV viral load and CD4 cell counts from medical records. Participants were given a form that asks their physician’s office to provide the results and dates of their most recent, and not older than 3-months, HIV viral load and CD4 cell counts. These data were therefore obtained directly by the participants from their health care providers. The form included a place for the provider’s office stamp or signature to assure authenticity. HIV RNA below detection was defined as less than 200 copies/mL for uniformity across providers. We also transformed HIV RNA using the formula log10(X+1) for a continuous measure of viral load.
ART Regimen Determination and Adherence
Participants consented to three unannounced telephone-based pill counts that occurred over a five-week period. Unannounced pill counts are reliable and valid in assessing medication adherence when conducted in homes (14) and on the telephone. (15, 16) In this study we conducted unannounced cell-phone based pill counts. Participants were provided with a free cell phone, were trained in the pill counting procedure, and were subsequently called at unscheduled times over 12 to 16 day intervals. Pharmacy information from pill bottles was also collected to verify the number of pills dispensed between calls. Adherence was defined as the differences between the number of pills counted and the number of pills prescribed, divided by the number prescribed. ART adherence was examined as a continuous variable and as a clinically meaningful categorical variable with adherence defined at three levels; greater than 75%, 85%, and 95% of their medications. (4, 17)
Data Analyses
Participants were grouped on the basis of the food requirements of their ART regimen. We obtained recommended ART administration instructions from the antiretroviral treatment guidelines for adults (http://aidsinfo.nih.gov/guidelines) and recommendations from AIDSMeds.com (http://www.aidsmeds.com/list.shtml). Six protease inhibitors and one non-nucleoside reverse transcriptase inhibitor (NNRTI) were recommended for administration with food; 408 participants were taking ART that requires food and 351 participants were taking ART that did not require food. We further classified participants on the basis of their responses to the food insecurity measure; 281 did not endorse any indicators of food insecurity and 478 participants endorsed at least one food insecurity indicator. We therefore formed four groups of participants based on (a) food secure/food insecure and (b) taking ART that does and does not require food.
Contingency table X2 tests of association were used for ART regimens and food insecurity descriptive analyses. Comparisons of food requirement groups within food secure and food insecure groups used logistic regressions, reporting odds ratios with 95% confidence intervals. To test the main study hypothesis that food security would modify the association between ART regimen and treatment outcomes, two multivariable logistic regressions were conducted. These models tested the interaction of food insecurity and ART food requirements on (a) adherence/non-adherence and (b) HIV suppression/non-suppression. These models tested the food security x ART food requirements interactions after adjusting for HIV symptoms, income, and the main effects of food security and ART food requirements. Statistical significance was defined as p < .05.
Results
Results showed that 478 (63%) participants endorsed at least one indicator of food insecurity for the previous month, of which 274 (57%) were prescribed an ART regimen that required food. Protease inhibitors represented the most commonly prescribed class of ART that requires food, with 68% of food insecure participants prescribed these regimens compared to 59% of those who were food secure. (see Table 1) The association between food insecurity and taking any ART regimen that requires food was significant, X2 (df=1, N = 759) = 6.61, p < .01; food insecure participants were more likely to be prescribed ART that should be taken with food. Table 2 shows that the association between food insecurity and ART regimens requiring food occurred across indicators of food insecurity, with participants who were prescribed an ART regimen that required food reporting significantly greater concern about accessing food and eating less due to lack of money.
Table 1.
Frequency of antiretroviral medications prescribed to food secure and food insecure people living with HIV.
| Food Secure N = 281 |
Food Insecure N = 478 |
X2 | |||
|---|---|---|---|---|---|
| N | % | N | % | ||
| NRTI | 206 | 73 | 360 | 75 | 0.4 |
| Zidovudine+Lamivudine | 16 | 5 | 17 | 3 | |
| Emtricitabine | 4 | 1 | 5 | 1 | |
| Lamivudine | 6 | 2 | 12 | 2 | |
| Abacavir+Lamivudine | 30 | 10 | 54 | 11 | |
| Zidovudine | 17 | 6 | 25 | 5 | |
| Zidovudine+Lamivudine+Abacavir | 9 | 3 | 10 | 2 | |
| Tenofovir+Emtricitabine | 126 | 41 | 247 | 49 | |
| Didanosine | 7 | 2 | 7 | 2 | |
| Tenofovir | 20 | 6 | 34 | 7 | |
| Stavudine | 1 | 1 | 2 | 1 | |
| Abacavir | 9 | 1 | 7 | 1 | |
| NNRTI | 36 | 12 | 44 | 9 | 2.4 |
| Etravine | 9 | 2 | 17 | 3 | |
| Efavirenz | 19 | 6 | 15 | 3 | |
| Nevirapine | 8 | 3 | 12 | 2 | |
| Dual Class | |||||
| Efavirenz+Tenofovir+Emtricitabine | 74 | 26 | 10 | 21 | 1.3 |
| Protease Inhibitor | 166 | 59 | 324 | 68 | 5.8** |
| Indinavir | 2 | 1 | 0 | ||
| Saquinavir | 0 | 2 | 1 | ||
| Lopinavir+Ritonavir | 34 | 11 | 55 | 11 | |
| Fosamprenavir | 1 | 1 | 12 | 2 | |
| Ritonavir | 123 | 43 | 256 | 51 | |
| Darunavir | 39 | 13 | 92 | 18 | |
| Atazanavir | 86 | 30 | 161 | 32 | |
| Nelfinavir | 4 | 1 | 6 | 2 | |
| Entry Inhibitor | |||||
| Maraviroc | 0 | 2 | 1 | N/A | |
| Integrase Inhibitor | |||||
| Raltegravir | 35 | 12 | 59 | 12 | 0.1 |
| Any ART regimen requires food | 134 | 47 | 274 | 57 | 6.6** |
Note: Medications in boldface require food;
p < .01
Table 2.
Indicators of food insecurity among participants prescribed HIV medications that are not and are taken with food.
| Food Insecurity indicator | Food Not Required with ART (N=351) | Food Required with ART (N=408) | X2 | ||
|---|---|---|---|---|---|
|
| |||||
| N | % | N | % | ||
| Worried if food would run out before having money to buy more. | 176 | 50 | 238 | 58 | 5.1** |
| Food didn’t last and didn’t have money to get more. | 177 | 50 | 239 | 58 | 5.0* |
| Couldn’t afford to eat balanced meals. | 161 | 46 | 221 | 54 | 5.2* |
| Adults in household cut meal size for not having money for food. | 120 | 34 | 158 | 39 | 1.6 |
| Eat less than one felt like eating for not having money for food. | 127 | 36 | 177 | 43 | 4.0* |
| Being hungry without eating for not being able to afford food. | 93 | 27 | 119 | 29 | 0.6 |
| Lose weight for not having enough money for food. | 77 | 22 | 88 | 22 | 0.1 |
| Adults in household not eat for a whole day without money for food. | 43 | 12 | 55 | 14 | 0.2 |
Note:
p < .05,
p < .01
ART Food requirements among food secure individuals
Results demonstrated that among people living with HIV who are food secure, those taking ART that requires food were significantly less adherent than those whose ART regimen does not require food. (see Table 3) One in five food secure participants whose ART regimen requires food had taken less than 85% of their ART in the prospective month. Similar results were observed using 75% and 95% cut-offs for defining adherence.
Table 3.
Demographic and health characteristics of people living with HIV who are food secure and food insecure and taking ART that does not or does require food.
| Characteristic |
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Food Secure (N=281)
|
Food Insecure (N=478)
|
|||||||||||
| Food Not Required with ART (N=147) | Food Required with ART (N=134) | Food Not Required with ART (n=204) | Food Required with ART (n=274) | |||||||||
|
| ||||||||||||
| M | SD | M | SD | OR | 95%CI | M | SD | M | SD | OR | 95%CI | |
| Age | 51.3 | 8.5 | 49.7 | 8.1 | 0.97 | 0.84–1.00 | 47.0 | 8.6 | 46.1 | 8.07 | 0.98 | 0.96–1.00 |
| Education | 12.5 | 1.8 | 12.7 | 1.7 | 1.05 | 0.92–1.20 | 12.6 | 1.8 | 12.4 | 1.8 | 0.92 | 0.83–1.01 |
| Years HIV+ | 15.9 | 7.7 | 17.1 | 7.3 | 1.02 | 0.98–1.05 | 14.9 | 8.2 | 14.9 | 7.6 | 1.00 | 0.97–1.02 |
| HIV symptoms | 2.4 | 2.7 | 2.4 | 3.2 | 1.01 | 0.93–1.08 | 4.4 | 3.3 | 5.2 | 3.7 | 1.08** | 1.02–1.13 |
| Side effects | 0.3 | 0.3 | 0.3 | 0.3 | 1.06 | 0.53–2.11 | 0.6 | 0.5 | 0.6 | 0.4 | 1.19 | 0.82–1.72 |
| Adherence | 91.8 | 11.7 | 86.2 | 17.2 | 0.07** | 0.01–0.38 | 86.9 | 16.5 | 85.9 | 16.1 | 0.68 | 0.22–2.10 |
| Log Viral load | 1.7 | 0.7 | 1.9 | 0.8 | 1.26 | 0.91–1.75 | 1.9 | 0.8 | 2.1 | 0.9 | 1.49** | 1.17–1.88 |
| CD4 cell count | 536.0 | 363.1 | 475.0 | 322.4 | 0.99 | 0.99–1.00 | 503.0 | 318.6 | 394.5 | 265.4 | 0.99** | 0.98–0.99 |
|
|
||||||||||||
| N | % | N | % | N | % | N | % | |||||
|
|
||||||||||||
| Male | 105 | 73 | 95 | 71 | 167 | 72 | 191 | 70 | ||||
| Female | 42 | 27 | 38 | 29 | 1.00 | 0.59–1.68 | 65 | 28 | 83 | 30 | 1.14 | 0.76–1.70 |
| Income <$10k | 77 | 52 | 86 | 64 | 0.78 | 0.28–1.05 | 160 | 69 | 194 | 71 | 0.99 | 0.74–1.31 |
| Employed | 20 | 13 | 10 | 8 | 0.92 | 0.70–1.19 | 21 | 9 | 18 | 6 | 1.02 | 0.86–1.21 |
| CD4 < 200 | 16 | 12 | 24 | 19 | 0.54 | 0.27–1.07 | 24 | 11 | 62 | 23 | 0.32** | 0.18–0.56 |
| ART Adherence | ||||||||||||
| > 75% | 133 | 90 | 107 | 80 | 0.42** | 0.21–0.83 | 169 | 83 | 210 | 77 | 0.68 | 0.42–1.07 |
| > 85% | 116 | 79 | 91 | 68 | 0.56* | 0.33–0.96 | 171 | 69 | 179 | 65 | 0.84 | 0.57–1.24 |
| > 95% | 82 | 56 | 57 | 43 | 0.58* | 0.36–0.94 | 90 | 44 | 105 | 38 | 0.78 | 0.54–1.13 |
| Unsuppressed HIV | 13 | 9 | 19 | 15 | 1.74 | 0.82–3.6 | 31 | 14 | 62 | 23 | 2.48 | 1.46–4.20 |
Note:
p < .05,
p < .01
ART Food requirements among the food insecure individuals
Among participants who were food insecure, there were significant differences in treatment outcomes for those taking ART that does not and does require food. (see Table 3) Individuals taking ART that requires food indicated significantly greater HIV symptoms, had lower CD4 cell counts, and higher HIV RNA viral loads; 23% of participants whose ART requires food were viral unsuppressed compared to 14% of their counterparts taking ART that does not require food.
Modifying effects of food insecurity
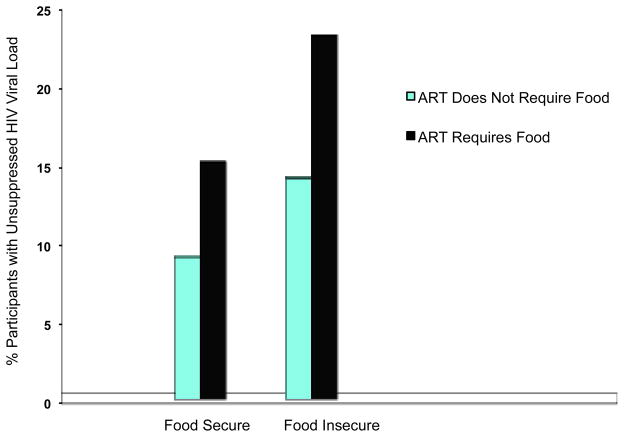
The interaction between food insecurity and ART food restrictions for both ART adherence and HIV suppression were tested using multivariable regressions, adjusting for HIV symptoms, income and the main effects of food insecurity and ART food restriction regimen. In the first model, the food insecurity x ART food requirement interaction effect on 85% ART adherence was not significant, OR = 0.95, 95%CI 0.38–1.04. Models using 75% or 95% adherence were also not significant. In the model for HIV suppression, the food insecurity x ART food requirement interaction was significant, OR = 1.14, 95%CI 1.02–1.27, p < .01; Food insecure participants who were taking ART that requires food were significantly more likely to have unsuppressed HIV, while those who were food secure and taking ART that does not require food were least likely to have unsuppressed HIV. (see Figure 1)
Figure 1.
Modifying effect of food insecurity on the association between ART regimen and HIV viral suppression.
Discussion
These findings should be interpreted in light of the study limitations. First, we relied on a convenience sample that cannot be considered representative of people living with HIV infection. The sample also came from a wide-range of providers that likely varied in health services and prescription practices. The cross-sectional study design with respect to food security also limits our interpretation of the results. It should also be noted that we adapted the measure of food insecurity without validation. Our data also do not allow precise measurement of whether missed medication doses occurred in relation to times when food was scarce, particularly whether medications that are instructed to be taken with food are missed at those times.
More than half of the persons taking ART in this study reported experiencing food insecurity in the previous month. We found that people living with HIV who are experiencing food insecurity are significantly more likely to be prescribed ART regimens that require food. This difference did not occur as the result of any single indicator of food insecurity. One possible explanation for the association of ART regimen and food security is the use of more forgiving ART regimens, such as boosted protease inhibitors that require food, with less adherent patients who are also food insecure. Among those persons who were food secure, taking ART that requires food was associated with poorer ART adherence. Thus, even for persons who have adequate access to food, requiring food at the time medications are taken may interfere with adherence.
In contrast to those who were food secure, there was no association between taking ART that requires food and ART adherence among persons who were food insecure; adherence was relatively poor for food insecure persons regardless of food requirements. However, we found that food insecure participants who were taking ART that requires food had significantly poorer HIV suppression. Participants who were food insecure and taking ART that requires food also experienced more HIV symptoms and had lower CD4 cell counts. Poorer treatment outcomes for people who are food insecure and are prescribed ART that requires food in the absence of differences in adherence maybe accounted for by insufficient drug absorption that occurs when ART regimens that require meals are taken without food.
Food insecurity is only one of several co-occurring facets of poverty that are related to non-adherence, including unstable housing and lack of transportation. (18, 19) However, requiring food for optimal ART absorption is the only aspect of poverty directly related to the pharmacokinetics of ART. The selection of an ART regimen is individualized on the basis of multiple considerations including virologic efficacy, toxicity, pill burden, dosing frequency, resistance testing results, comorbid conditions, and cost (20)(see http://aidsinfo.nih.gov/guidelines). Given the growing prominence of poverty in HIV epidemics, access to food should be explicitly assessed and prioritized when prescribing ART. Our findings are therefore clinically significant because they show that people living with HIV who lack access to food and are prescribed ART that requires meals have poorer heath outcomes than individuals who are also food insecure but taking ART that does not require meals. When the optimal ART regimen for a food insecure patient requires food, it may be necessary to couple the medication dosing with companion nutritional supplements or small meals. Whether selecting an alternative regimen that does not require food or providing food with ART, it is essential that a patient’s access to food be prioritized among factors in determining optimal treatment options.
Acknowledgments
This project was supported by National Institute of Alcohol Abuse and Alcoholism Grant R01-AA021471 and National Institute of Drug Abuse Grant R01-DA017399.
References
- 1.Anema A, Zhang W, Wu Y, Elul B, Weiser SD, Hogg RS, et al. Availability of nutritional support services in HIV care and treatment sites in sub-Saharan African countries. Pub Health Nutrition. 2012;15(5):938–47. doi: 10.1017/S136898001100125X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weiser SD, Tsai AC, Gupta R, Frongillo EA, Kawuma A, Senkungu J, et al. Food insecurity is associated with morbidity and patterns of healthcare utilization among HIV-infected individuals in a resource-poor setting. AIDS. 2012;26(1):67–75. doi: 10.1097/QAD.0b013e32834cad37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weiser SD, Bangsberg DR, Kegeles S, Ragland K, Kushel MB, Frongillo EA. Food insecurity among homeless and marginally housed individuals living with HIV/AIDS in San Francisco. AIDS Behav. 2009;13(5):841–8. doi: 10.1007/s10461-009-9597-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weiser SD, Hatcher A, Frongillo EA, Guzman D, Riley ED, Bangsberg DR, et al. Food insecurity Is associated with greater acute care utilization among HIV-Infected homeless and marginally housed individuals in San Francisco. J Gen Intern Med. 2013;28:91–8. doi: 10.1007/s11606-012-2176-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vogenthaler NS, Kushel MB, Hadley C, Frongillo EA, Jr, Riley ED, Bangsberg DR, et al. Food insecurity and risky sexual behaviors among homeless and marginally housed HIV-infected individuals in San Francisco. AIDS Behav. 2013;17:1688–93. doi: 10.1007/s10461-012-0355-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kalichman SC, Cherry C, Amaral C, White D, Kalichman MO, Pope H, et al. Health and treatment implications of food insufficiency among people living with HIV/AIDS, Atlanta, Georgia. J Urban Health. 2010;87(4):631–41. doi: 10.1007/s11524-010-9446-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weiser SD, Fernandes KA, Brandson EK, Lima VD, Anema A, Bangsberg DR, et al. The association between food insecurity and mortality among HIV-infected individuals on HAART. J Acquir Immune Defic Syndr. 2009;52:342–9. doi: 10.1097/QAI.0b013e3181b627c2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Le Tiec C, Barrail A, Goujard C, Taburet AM. Clinical pharmacokinetics and summary of efficacy and tolerability of atazanavir. Clin Pharmacokinetics. 2005;44(10):1035–50. doi: 10.2165/00003088-200544100-00003. [DOI] [PubMed] [Google Scholar]
- 9.Gribble JN, Miller HG, Cooley PC, Catania JA, Pollack L, Turner CF. The impact of T-ACASI interviewing on reported drug use among men who have sex with men. Subst Use Misuse. 2000;35(6–8):869–90. doi: 10.3109/10826080009148425. [DOI] [PubMed] [Google Scholar]
- 10.Morrison-Beedy D, Carey MP, Tu X. Accuracy of audio computer-assisted self-interviewing (ACASI) and self-administered questionnaires for the assessment of sexual behavior. AIDS Behav. 2006;10(5):541–52. doi: 10.1007/s10461-006-9081-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kalichman S, Rompa D, Cage M. Reliability and validity of self-reported CD4 lymphocyte count and viral load test results in people living with HIV/AIDS. Int J STD AIDS. 2000;11(9):579–85. doi: 10.1258/0956462001916551. [DOI] [PubMed] [Google Scholar]
- 12.Carrieri MP, Villes V, et al. Self-reported side-effects of anti-retroviral treatment among IDUs: a 7-year longitudinal study. International J Drug Policy. 2007;18(4):288–95. doi: 10.1016/j.drugpo.2007.01.014. [DOI] [PubMed] [Google Scholar]
- 13.Cook JT, Frank DA. Food security, poverty, and human development in the United States. Ann N Y Acad Sci. 2008;1136:193–209. doi: 10.1196/annals.1425.001. [DOI] [PubMed] [Google Scholar]
- 14.Bangsberg DR, Hecht FM, Charlebois ED, Chesney M, Moss A. Comparing objective measures of adherence to HIV antiretroviral therapy: Electronic medication monitors and unannounced pill counts. AIDS Behav. 2001;5:275–81. [Google Scholar]
- 15.Kalichman SC, Amaral CM, Cherry C, Flanagan JA, Pope H, Eaton L, et al. Monitoring Antiretroviral adherence by unannounced pill counts conducted by telephone: Reliability and criterion-related validity. HIV ClinTrials. 2008;9:298–308. doi: 10.1310/hct0905-298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kalichman SC, Amaral CM, Stearns HL, White D, Flanagan JA, Pope H, et al. Adherence to antiretroviral therapy assessed by unannounced pill counts conducted by telephone. J Gen Intern Med. 2007;22:1003–6. doi: 10.1007/s11606-007-0171-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bangsberg D, Deeks SG. Is average adherence to HIV antiretroviral therapy enough? J Gen Intern Med. 2002;17(10):812–3. doi: 10.1046/j.1525-1497.2002.20812.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leaver CA, Bargh G, Dunn JR, Hwang SW. The effects of housing status on health-related outcomes in people living with HIV: a systematic review of the literature. AIDS Behav. 2007;11(6 Suppl):85–100. doi: 10.1007/s10461-007-9246-3. [DOI] [PubMed] [Google Scholar]
- 19.Tuller DM, Bangsberg DR, Senkungu J, Ware NC, Emenyonu N, Weiser SD. Transportation Costs Impede Sustained Adherence and Access to HAART in a Clinic Population in Southwestern Uganda: A Qualitative Study. AIDS Behav. 2010;14:778–84. doi: 10.1007/s10461-009-9533-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marrazzo JM, del Rio C, Holtgrave DR, Cohen MS, Kalichman SC, Mayer KH, et al. HIV prevention in clinical care settings: 2014 recommendations of the International Antiviral Society-USA Panel. JAMA. 2014;312(4):390–409. doi: 10.1001/jama.2014.7999. [DOI] [PMC free article] [PubMed] [Google Scholar]