Abstract
Obesity and mental health disorders remain significant public health problems in adolescents. Substantial health disparities exist with minority youth experiencing higher rates of these problems. Schools are an outstanding venue to provide teens with skills needed to improve their physical and mental health, and academic performance. In this paper, the authors describe the design, intervention, methods and baseline data for a randomized controlled trial with 779 culturally diverse high-school adolescents in the southwest United States. Aims for this prevention study include testing the efficacy of the COPE TEEN program versus an attention control program on the adolescents’ healthy lifestyle behaviors, Body Mass Index (BMI) and BMI%, mental health, social skills and academic performance immediately following the intervention programs, and at six and 12 months post interventions. Baseline findings indicate that greater than 40% of the sample is either overweight (n = 148, 19.00%) or obese (n = 182, 23.36%). The predominant ethnicity represented is Hispanic (n = 526, 67.52%). At baseline, 15.79%(n = 123) of the students had above average scores on the Beck Youth Inventory Depression subscale indicating mildly (n = 52, 6.68%), moderately (n = 47, 6.03%), or extremely (n = 24, 3.08%) elevated scores (see 1). Anxiety scores were slightly higher with 21.56% (n = 168) reporting responses suggesting mildly (n = 81, 10.40%), moderately (n = 58, 7.45%) or extremely (n = 29, 3.72%) elevated scores. If the efficacy of the COPE TEEN program is supported, it will offer schools a curriculum that can be easily incorporated into high school health courses to improve adolescent healthy lifestyle behaviors, psychosocial outcomes and academic performance.
Keywords: Adolescents, RCT, High school, Prevention, Overweight, Mental health
1. Introduction
Obesity and mental health disorders in adolescence are two major public health problems in the United States today [1,2]. The incidence of overweight and obesity has dramatically increased over the past 20 years (i.e., overweight, a gender and age-specific body mass index [BMI] percentile at or above the 85th percentile, or obese, which is defined as a gender and age-specific BMI percentile at or above the 95th percentile) [3,4].
Approximately 15 million children and adolescents in the U.S. have a mental health problem that interferes with their functioning at home or at school, yet less than 25% receive treatment [5–9]. Depression among adolescents is associated with disabling morbidity, significant mortality, and substantial healthcare costs [10,11].
Overweight youth have heightened anxiety, depression, suicidal thoughts, body dissatisfaction, and hopelessness in addition to a higher prevalence of school problems, including poor academic performance [5–8,12–15]. Compared to their non-overweight peers, Hispanic and White teens who are overweight are significantly more likely to report depression and feelings of worthlessness [16]. Although there is support from longitudinal studies with adolescents that depression may infer an increased risk of obesity in adults [17], there is also support that obesity in adolescents increases the risk of depression in adults [14,18]. The relationship between depression and obesity in adolescence is complex, multifactorial, and not unidirectional. As obesity and depression are known to coexist, addressing the prevention of both together in an intervention will likely impact the greatest number of students.
Because of the extensive time that youth spend in learning environments, schools are an outstanding venue to provide adolescents with skills needed to improve their healthy lifestyle behaviors, mental health and academic performance. Prior school-based prevention trials for obesity in adolescents have yielded small and typically non-significant changes on measures of weight [19–22]. However, other beneficial effects of preventive interventions have been supported, such as improvements in sedentary activity, eating patterns [23], body/self-image [19], and screen time [23,24].
Findings from a meta-analytic review of school-based programs for the prevention of depression identified small effects [25]. Certain study characteristics increased effect sizes such as targeting high-risk individuals with shorter duration interventions, including homework. A systematic review of school-based prevention and early intervention programs for depression indicated most studies were based on cognitive behavioral therapy. The most effective programs targeted those with existing elevated levels of depression [26].
By integrating some key elements of prior studies with significant findings, this study builds upon current research by implementing a large, well-designed randomized controlled trial. In addition, the study includes the delivery of the healthy lifestyle intervention by teachers and assessment of implementation fidelity.
1.1. Theory
Cognitive Behavior Theory (CBT), informed by cognitive and behavioral theories, guided the content of the COPE (Creating Opportunities for Personal Empowerment) Healthy Lifestyles TEEN (Thinking, Emotions, Exercise, Nutrition) Program [27–30]. The basic premise of CBT is that an individual’s emotions and behaviors are, in large part, determined by the way in which he or she cognitively thinks and appraises the world [31]. Therefore, a person who has negative beliefs tends to have negative emotions (e.g., depression) and behaves in negative ways (e.g., overeating, risky behaviors) [5,32]. Negative emotions and behaviors are even more profound when there are skill deficits (e.g. poor emotional regulation, poor problem-solving and assertiveness skills). Based on this theory, we predicted that teens who lack beliefs/confidence in their abilities to engage in healthy behaviors and perceive those behaviors as difficult to perform will report more depressive/anxiety symptoms and engage in fewer healthy behaviors (see Fig. 1). The adolescent’s beliefs in his or her ability to live a healthy lifestyle are proposed to increase and perceived difficulty in living a healthy lifestyle is contended to decrease through the use of positive self-statements, goal setting, problem-solving, and cognitive reframing. Our prior studies with hundreds of teens have supported significant relationships among these variables [33–36]. Three pilot tests of the COPE TEEN intervention also have been completed prior to this study, including research in: (a) a large suburban New York school, N = 12, 92% white [35], (b) a rural West Virginia school, N = 49, 98% white [37], and (c) an urban Arizona school, N = 19, 100% Hispanic [33]. Findings from our pilot studies testing COPE TEEN have shown a decrease in weight [35,37], anxiety/depression [33], and an increase in the teens’ commitment to make healthy lifestyle choices [35,37].
Fig. 1.
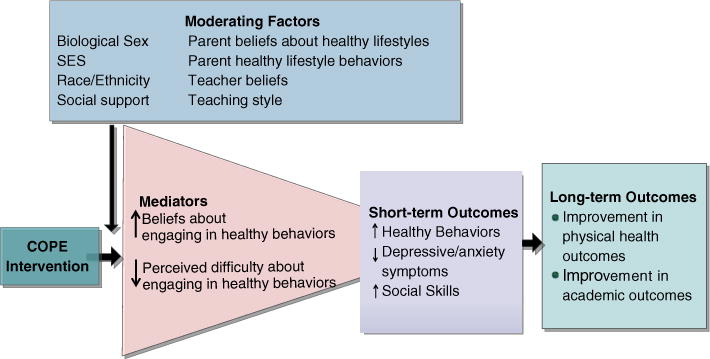
Hypothesized effects of the COPE intervention.
1.2. Mediators and moderators
Based on CBT, we hypothesized that the COPE TEEN intervention will first strengthen the teens’ beliefs/confidence in their ability to engage in healthy lifestyle behaviors, manage their negative emotions, perform well academically and lessen their perceived difficulty of performing healthy behaviors, which in turn, will result in more healthy behaviors, less depressive and anxiety symptoms, and higher social skills (see Fig. 1). Ultimately, engaging in healthy lifestyle behaviors should lead to the prevention of overweight in normal weight teenagers and less weight gain in those who are overweight at baseline. Further, less depressive and anxiety symptoms as well as higher social skills should lead to better academic outcomes. We chose the proximal outcomes of healthy lifestyle behaviors, depressive/anxiety symptoms, and social skills as our key primary outcomes because they are so important at this developmental phase and often precipitate later distal outcomes (e.g., overweight, major depressive disorder, poor academic outcomes).
Mediational analyses of data are important to better understand the mechanisms through which treatments are effective [38]. However, prior studies have not tended to test mediators [39]. Thus, there remain large gaps in knowledge about how interventions impact outcomes. Based on our literature review, there are likely to be key influences outside of cognition that may impact a teen’s healthy behaviors, social skills and emotions. Therefore, we added key variables to our model as potential moderators. For example, we may find that the COPE TEEN intervention works better for certain sub-groups of teens (e.g., those who have parents with stronger beliefs; those in high fidelity classrooms). Analysis of both moderating and mediating variables will allow us to extend the science of healthy lifestyle interventions with adolescents.
The purpose of this study is to test the short and more long-term efficacy of the COPE TEEN intervention, versus an attention control program (Healthy Teens) on the healthy lifestyle behaviors, Body Mass Index (BMI) and BMI percentile, social skills, depressive/anxiety symptoms and academic performance of 779 culturally diverse high school teens enrolled in the southwest region of the U.S. for the ultimate purpose of preventing overweight/obesity, mental health disorders and poor academic functioning. The primary aim of the study is to evaluate if teens in the COPE TEEN intervention have higher healthy lifestyle behaviors, less weight gain and less depressive symptoms than teens receiving the attention control intervention immediately following and at 6 and 12 months post-intervention. The secondary aim is to examine whether the COPE TEEN intervention also improves social skills and academic performance. Two additional aims include: (1) theory building exploration by evaluating mediation of healthy lifestyle behaviors and depressive symptoms by examining adolescents’ perceived difficulty and beliefs in their ability to make healthy lifestyle choices; and (2) evaluation of variables that may moderate the effects of the intervention on healthy lifestyle behaviors and depressive/anxiety symptoms (e.g., ethnicity, gender, SES, family composition, acculturation, and parental healthy lifestyle beliefs and behaviors). This paper includes the design, intervention, methods and baseline data for an ongoing randomized controlled trial with 779 culturally diverse high-school adolescents in the southwest region of the United States.
2. Methods
The COPE TEEN study is a four-year prospective, randomized controlled trial for high school adolescents, ages 14 to 16 years. The COPE TEEN intervention is a 15-session educational and cognitive–behavioral skills building (CBSB) intervention that includes 20 min of physical activity in each session. The study design and reporting have been guided by the CONSORT guidelines [40] (see Fig. 2). This study was approved by the University Institutional Review Board and each participating school district.
Fig. 2.
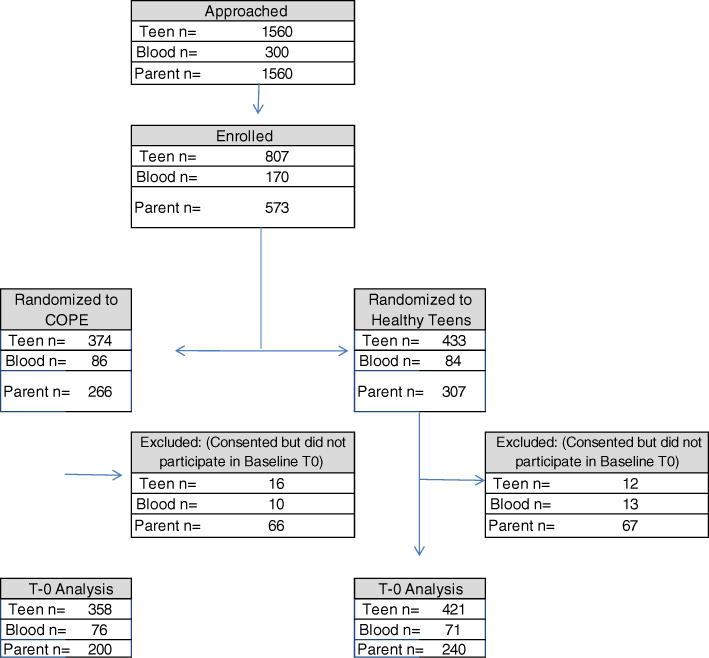
Consort flow chart-recruitment through baseline date collection.
2.1. Sample and setting
Students were invited to participate if they were 14 to 16 years old and enrolled in health education courses at 11 high schools from two school districts in a large metropolitan city in the southwest United States. District administrators in both districts chose which schools could participate in the study. Since the first school district contained a high percentage of Hispanic teens from low socioeconomic (SES) backgrounds, the second school district was targeted to increase diversity of ethnicity and SES status. The first school district is located in the heart of the metropolitan city with the other district being located within a large suburb, which serves students from all socioeconomic backgrounds.
2.2. Eligibility
Inclusion criteria to participate in the study included: (a) teens 14 to 16 years of age enrolled in a health class at one of the 11 participating high schools, (b) Teens who assented to participation, (c) teens with a custodial parent who consented for their teen’s participation in the study and optionally for themselves, (d) teens who could speak and read in English, and (e) parents who could speak and read either Spanish or English.
Exclusion criteria included: (a) teens with a medical condition that would not allow them to participate in the physical activity component of the program.
2.3. Procedure
Schools within each of the two school districts were randomly assigned to receive either the COPE TEEN program or the Healthy Teens attention control program by placing all of the school names in a hat and then randomly drawing them out. Schools were not matched on any characteristics. All teens in the selected health education courses in the 11 high schools were invited to participate in the study (see Fig. 2). Research team members introduced the study to all students in each health class and sent consent/assent packets home with all teens who expressed interest in study participation. Consents were provided in either English or Spanish. Teens who returned a signed assent and parent consent were enrolled in the study. All students in each health class received either the COPE TEEN or attention control curriculum. Only students enrolled in the study completed the research measures. In addition, at the baseline data collection, all teens who had a BMI percentile ≥ 85 were privately invited to have a fasting blood sample drawn by finger stick prior to the start of school at the nurse’s office to assess cholesterol. Fifty-seven percent (n = 170) of the teens approached to have their blood drawn consented and 147 completed the baseline blood work.
The decision was made to randomly assign schools to one of the two interventions (e.g., instead of randomly assigning classrooms within the schools) in order to decrease the probability of cross-contamination and minimize threats to internal validity. Whether they were enrolled in the study or not, all adolescents in the health education courses received either: (a) a 15 week, 15 session multi-component educational and CBSB intervention with physical activity, or (b) a 15 week, 15 session attention control program focusing on common adolescent health topics (e.g., health literacy, safety, skin care). The length of class periods varied between 50 and 57 min. Intervention content was delivered by the teens’ health teachers after a one-day training session. Session content was delivered in 30 min in the COPE TEEN group with 20 min of physical activity, which was completed either in the classroom or as outdoor activities (e.g., walks). Session content was delivered over the entire class period in the Healthy Teens group. Students and parents gave assent/consent prior to participation in the study.
2.4. Measures
Measures were completed by teens, parents and teachers (see Table 2). Time points for collection of measures were baseline, post-intervention, and six and 12 months following completion of the intervention. See Table 2 for scale reliabilities.
Table 2.
Measures.
| Instrument | Role in analysis | Reliability | Time |
|---|---|---|---|
| Teen | |||
| The acculturation, habits, and interests multicultural scale for adolescents (8-items) | Control variable | 0.86 | 0 |
| Healthy Lifestyle Beliefs Scale (16-items) | Mediator | 0.89 | 0, 1, 2, 3 |
| Perceived Difficulty Scale (12-items) | Mediator | 0.88 | 0, 1, 2, 3 |
| Healthy Lifestyle Behaviors Scale (15-items) | Moderator | 0.85 | 0, 1, 2, 3 |
| Physical activity: pedometer (7-days) | Outcome | 0, 1 | |
| Beck Youth Inventory (2nd edition): depressive symptoms, anxiety, disruptive behavior, self-concept, anger (100-items) | Outcomes | >.89 | 0, 1, 2, 3 |
| Anthropometric measures: height, weight, waist circumference | Control variable, outcome | n/a | 0, 1, 2, 3 |
| Nutrition knowledge (20-items) and activity knowledge (12-items) | Fidelity check | .76, .64 | |
| Cholesterol panel: TC, LDL, HDL, Trig | Outcome | n/a | 0, 1, 2 |
| Demographics | Moderator | ||
| Academic outcomes: health class grade and GPA | Outcome | n/a | 1, 2, 3 |
| Youth risk behavioral surveillance survey item for substance use: tobacco, alcohol, marijuana, and illicit drugs | Outcome | n/a | 0, 1, 2, 3 |
| Parents | |||
| Demographics | Moderator | n/a | 0 |
| Healthy Lifestyle Beliefs Scale (16-items) | Moderator | 0.9 | 0, 1 |
| Healthy Lifestyle Behaviors Scale (15-items) | Moderator | 0.87 | 0, 1 |
| Nutrition knowledge (20-items) and activity knowledge (12-items) | 0, 1 | ||
| Teachers | |||
| Demographics | n/a | 0 | |
| Social skills rating system: teen’s social skills, problem behaviors, and academic competence | Outcome | >.82 | 1 |
2.4.1. Acculturation
The Acculturation, Habits, and Interests Multicultural Scale for Adolescents (AHIMSA) measure a wide range of attitudes and preferences for the U.S. culture across several life domains (e.g., friends, media preferences, celebration of holidays, ways of thinking, favorite foods). Youth respond individually as to whether each statement represents: “the U.S.” (indicating assimilation), “the country my family is from” (indicating separation), “both” (indicating integration), and “neither” (indicating marginalization). Scores for each of these four orientations range from 0 to 8 [41].
2.4.2. Healthy lifestyle beliefs scale
The Healthy Lifestyle Beliefs Scale was adapted from other Beliefs scales used in multiple prior studies [34,42–44]. This scale taps beliefs about various facets of maintaining a healthy lifestyle (e.g., “I believe that I can be more active” and “ I am sure that I will do what is best to lead a healthy life”). Subjects respond to each item on a Likert-type scale that ranges from 1 strongly disagree to 5 strongly agree. Face validity was established with 10 teens. Content validity was established by 8 adolescent specialists. Construct validity of the scale was supported through factor analysis with over 400 high school adolescents [45].
2.4.3. Perceived difficulty scale
This instrument measures one’s perceived difficulty in living a healthy lifestyle [46]. Teens respond to each item on the 5-point Likert-type scale that ranges from 1 very hard to do to 5 very easy to do (e.g., how hard or easy it is to do the following things: eat healthy, exercise regularly, cope/deal with stress). The scale was adapted from another similar scale used with teens in a HIV-preventive intervention study [47,48]. Construct validity was supported through factor analysis with 400 high school students.
2.4.4. Healthy lifestyle behaviors
Healthy lifestyle behaviors were measured subjectively (e.g., I exercise on a regular basis; I talk about my worries or stress every day, I do what I should do to lead a healthy life) on a 5-point Likert-type scale that ranges from 0 strongly disagree to 5 strongly agree [49]. Face validity was established with 10 teens and 8 adolescent health experts established content validity.
2.4.5. Physical activity
Physical activity, another measure of healthy lifestyle behaviors, was measured with a pedometer. The Yamex SW-200 pedometer was used in this study. Yamex pedometers are considered the standard in the healthcare and research industry due to their reliability and accuracy. A pedometer step counter was provided to the teens in both the COPE TEEN and attention control groups at the beginning of the study. Teens were instructed by research personnel on the use of the pedometer. Pedometers provide a valid and reliable means to measure habitual physical activity in youth [50]. Step counts were recorded by the teens for 7 days at baseline and immediately following the intervention for 7 days. The teens were asked to record the number of steps taken each day.
2.4.6. Beck Youth Inventory (2nd edition; BYI–II)
This instrument is designed for youth 7 to 18 years of age [51,52]. The five sub-scales each contain 20 statements about thoughts, feelings and behaviors related to emotional and social impairment. Scores on the individual sub-scales are calculated as the sum of the 20 items and standardized to T-scores with a mean of 50 and a standard deviation of 10. The higher the youth’s T score, the higher the distress the youth is experiencing. For example, norms for the depression, anxiety, destructive behavior, and anger sub-scales include: <55 average; 55–59 mildly elevated; 60–69 moderately elevated; and 70+ is extremely elevated.
2.4.7. Anthropometric measures
All anthropometric measures were taken twice during each measurement time point, and the mean of the two measurements was calculated and will be used for analysis. Height and weight were obtained in a private area. Height was measured with a stadiometer to the nearest hundredth of a centimeter. Weight was measured with a Tanita® scale to the nearest hundredth of a kilogram (Tanita Corporation of America, Illinois, USA). Data were used to calculate BMI (kg/m2). Age and gender specific BMI percentile were calculated based on CDC growth charts for SAS (http://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm). Waist circumference was measured with a Power Systems Gulick Tape Measure® (Power Systems, Tennessee, USA) at the level of the umbilicus. This measuring tape is spring loaded to provide a consistent tension that offers a high level of accuracy.
2.4.8. Social Skills Rating System (SSRS)
The Social Skills Rating System has established validity and reliability and documents behaviors in three domains, including social skills, problem behaviors, and academic competence [53]. There are three domains assessed by the problem behaviors including externalizing problems, internalizing problems, and hyperactivity. The SSRS is comprised of three components (teacher, parent, and student) which may be used separately or in combination. This study utilized the teacher report only.
2.4.9. Nutrition and activity knowledge scales
Subjects respond to these scales by answering yes, no, or don’t know [54,55]. Face validity was established with 10 teens and content validity was established by 8 adolescent health experts for both of these instruments.
2.4.10. Cholesterol
Teens with a BMI percentile ≥ 85were invited to have their fasting total cholesterol, high density lipoprotein (HDL), low density lipoprotein (LDL), and triglyceride levels evaluated. Prior to the start of the school day and after an 8 to 12-hour fast, a registered nurse obtained a drop of blood from teens via a finger stick. The blood was analyzed through Cholestech® (Cholestech Corporation, CA, USA).
2.4.11. Demographic variables
Demographic data from the teens and parents were collected with a questionnaire. Examples of items included: (a) age, (b) gender, (c) ethnicity, (d) socioeconomic status, and (e) perceived social support.
2.4.12. Academic achievement
Academic achievement was measured with the student’s health course grade and the Academic Competence sub-scale of the Social Skills Rating System. This sub-scale is completed by the teacher and “includes items measuring reading and mathematics performance, motivation, parental support, and general cognitive functioning” [53].
2.5. Incentives
All participants received incentives for their involvement in the intervention. Teachers at the one-day training received a $25 gift card, a t-shirt and a computer jump drive storage device. Each teacher received $100 at the completion of the study. Teens received store gift cards at the completion of questionnaires and measurements: $10 at baseline and post-intervention, $15 at the 6 month follow-up, and $20 at the 12 month follow-up. Teens who participated in blood analyses received an additional $10 at baseline, post-intervention and 6 month follow-up. Parents received a store gift card for $20 at baseline and post-intervention.
2.6. Data collection
Data were collected on teens enrolled in the study in a separate classroom than their health class. Students were given a packet of questionnaires to complete at a table or desk. Height, weight, and waist circumference were measured during questionnaire completion. When students completed their questionnaires and measures, they brought their packet to a research team member. The research team member evaluated the packet for completeness. If the students missed any items on the questionnaires, they were invited to complete the items or were given the option to not complete those particular items. Once packets were completed, teens received their incentive.
After completion of the questionnaires, two items on the depression sub-scale were checked to identify if students were at risk for self-harm. If risk was identified, the student was referred to a school counselor. Within 24 h following data collection, the BYI depression sub-scale was scored and a letter was sent to the adolescent’s parent if the T-score indicated extremely elevated depression to advise them to take their son or daughter to the primary care provider for evaluation. Community resources also were provided to them.
2.7. Intervention
Driven by CBT, the COPE TEEN intervention is a series of 15 educational and CBSB sessions with a physical activity component that empowers teens to engage in healthy lifestyle behaviors (i.e., nutrition, physical activity, positive strategies to cope with stress, problem-solving, regulation of negative mood and goal setting) (see Table 3). Based on CBT, the teens are taught how to cognitively restructure their thinking when negative events/interpersonal situations arise that lead them into negative thinking and how to turn that thinking into a more positive interpretation of the situation so that they will emotionally feel better and behave in healthy ways. Emphasis is placed on how patterns of thinking impact behavior and emotions (i.e., the thinking, feeling and behaving triangle). Goal setting to promote engagement in healthy lifestyle behaviors and problem-solving for typical adolescent challenges are part of the CBSB component of the program (e.g., peer pressure for fast food, conflicts with parents). The COPE TEEN intervention also includes educational content to increase the teens’ knowledge of how to lead a healthy lifestyle and homework to reinforce skills being learned in the classroom. Approximately 20 min of physical activity is incorporated into each of the 15 COPE TEEN sessions to assist teens in raising their beliefs in their ability to be routinely active. Teachers were able to choose the types of physical activities, which commonly included movement within the classroom, brisk walking, dodge ball, kickball, obstacle course, “Tank” (a game suggested by our research team), and basketball.
Table 3.
Intervention curriculum.
| COPE session content
|
Healthy Teens content
|
|---|---|
| Session # title | Session # title |
| 1 Healthy lifestyles | 1 Health literacy |
| 2 Self-esteem and positive thinking | 2 Sun safety and tanning |
| 3 Setting goals and problem-solving | 3 Allergies and asthma |
| 4 Stress and coping | 4 Health professions |
| 5 Dealing with emotions in healthy ways | 5 Oral hygiene |
| 6 Personality and effective communication | 6 Infectious diseases |
| 7 Activity—let’s keep moving | 7 Immunizations |
| 8 Heart rate and stretching | 8 Anatomy of the eye |
| 9 Nutrition basics | 9 Anatomy of the heart |
| 10 Reading labels | 10 Genetics |
| 11 Portion sizes | 11 Transportation safety |
| 12 Eating for life and social eating—party heart(y) | 12 Environmental safety |
| 13 Snacks | 13 Sustaining the environment |
| 14 Healthy choices | 14 First aid |
| 15 Wrap-up | 15 Wrap-up |
The Healthy Teens attention control curriculum was intended to promote knowledge of common adolescent health topics and health literacy. Content included pertinent health information for teens (see Table 3).
Content for both the COPE TEEN intervention and attention control groups was delivered during one semester by health teachers during the students’ regularly scheduled health class with each group receiving the same amount of attention. Students in each group received 15 weekly sessions of the COPE TEEN or attention control content in addition to their health class curriculum. Each session has accompanying activities to be completed as homework to reinforce session content. The intervention groups also had informational newsletters that were sent home four times during the intervention program highlighting the content the student was learning in class. The students brought the newsletters home and were given the assignment to review the newsletters with their parent(s). Students received homework credit for discussing the COPE TEEN or Healthy Teens content with their parent(s).
2.8. Teacher training
Teachers in each group received a one-day of training on either the COPE TEEN or Healthy Teens intervention programs [56,57]. Teachers were blinded to which curriculum they were delivering (i.e., intervention versus attention control). Training included background information regarding improving health for adolescents, the curriculum, and their role in the research project. Teachers observed implementation of one session’s content. Teachers were provided with a scripted intervention notebook that detailed the delivery of their assigned interventions and PowerPoint presentations which supported the instruction of content. In the two school districts, teachers are required to attend continuing education hours. All teachers received Professional Growth and Development credits for delivering the intervention, which are used to maintain their teaching credentials and also are considered for salary adjustments and promotions. All teachers provided informed consent to participate in the study during the training day.
2.9. Assessment of intervention fidelity
Monitoring fidelity of the study intervention is essential to having greater confidence in the findings, being able to explain the results obtained, and in helping to ensure internal validity of the study. Recommendations for enhancing and maintaining treatment fidelity include: (1) develop a detailed manualized protocol; (2) determine the dosage, duration and frequency of the intervention; (3) devise intervention strategies based on a theoretical framework; (4) account for variations in intervention dosage statistically; (5) measure participant’s adherence to the intervention; (6) train the interventionists to deliver the intervention consistently and as intended; (7) monitor the intervention with observation fidelity checks; (8) utilize checklists to ensure that all intervention components are included in each session; and (9) evaluate participant receipt of the intervention by building into the protocol quantitative evaluative measures, such as nutrition and activity knowledge [58–60]. We implemented all of these strategies in this trial. Meticulous record keeping was maintained in order to evaluate the number of sessions that each student received; the delivery of the content of each session; and the completion of student homework activities. In an intervention diary, the teachers recorded the tasks accomplished in each intervention session, the methods used to complete the tasks, time spent on each task, and their impressions of the flow, content and student acceptance of the sessions. In addition, observers rated approximately 25% of the teachers’ intervention sessions using an observation instrument of intervention fidelity that was developed for this study. Cronbach’s alpha was .87 for this scale. Inter-rater reliability of 90% for the fidelity observations between raters was established and maintained. Teachers received feedback from the evaluation to help them more closely adhere to the curriculum or to increase student participation.
2.9.1. Data and safety monitoring plan
The potential risk of our current clinical trial is considered to be minimal because of the nature of the intervention. Since this study fits in the category of Clinical Trial (Phase II) study, a plan was developed for appropriate oversight and monitoring of the conduct of the clinical trial to ensure the safety of the participants and the validity and integrity of the data. Plans were made for the Data Safety Monitoring Board to meet at regularly scheduled times during the course of the study.
2.10. Analysis plan
Baseline data were assessed using descriptive statistics (frequencies, means, and standard deviations) and groups were compared using independent sample t-tests and chi-square. Pedometer data will be analyzed without imputation of the data. All data analyses will be completed as intention to treat analyses (i.e., individuals will be analyzed by group, according to original random assignment, without regard to their adherence to the experimental protocol). This procedure more closely approximates the mixed levels of adherence likely to be seen in clinical practice [40]. Linear hierarchical models (also referred to as random coefficient and mixed models) will be used to explore the effect of the intervention over time because these models take in account the clustering inherent in the data. Population average models will be used to compare the two groups over the four repeated measures. Dummy variables will be included to capture the school effect. Any group differences at baseline will be controlled for by added them to the models as covariates. Structural equation modeling (SEM) will be used to examine the role of cognitive beliefs and perceived difficulty in leading a healthy lifestyle in mediating the effects of the COPE TEEN program on healthy lifestyle behaviors as well as depressive symptoms. Change over time in the outcomes will be modeled with a latent growth model with the intervention and mediators added to the model as predictors of the slope of the growth model.
2.11. Sample size justification
Sample size for the study was based on a power analysis for teen outcomes based on published research and pilot data [42,43,51,52,61–64]. Effect sizes considered for depression ranged from .20 to .60; for healthy lifestyle behaviors ranged from .23 to .45; and for weight ranged from .12 to .72. Several scenarios were run to assess power for the omnibus ANOVA tests and the a priori comparison of between group differences at each time point adjusted for the class intraclass correlation (ICC), the most likely cluster variable to have a meaningful ICC. Scenarios varied both the class size (20 to 50) and ICC (.01 to .10). With 800 participants, there is enough power (β = .8) to compare change over time between the intervention and control groups. Power analyses were conducted using PASS 2005 software (NCSS, Inc.).
3. Baseline results
3.1. Recruitment
Three cohorts were recruited from 11 high schools in two districts between January 1010 and August 2011 (see Fig. 2). Recruitment began at the beginning of spring semester 2010 (Cohort 1) with subsequent cohort recruitments during fall semester 2010 (Cohort 2) and fall semester 2011 (Cohort 3). Each cohort was recruited at the beginning of a school semester. A total of 1560 students were approached to participate in the study. Eight hundred and seven returned consent/assent forms and 779 were enrolled in the study completing baseline measures. Parental participation was approximately 56% of the student participation with 440 parents completing baseline questionnaires.
3.2. Baseline characteristics and comparisons between groups: Teens
Slightly more than half of the teens in this trial are female (n = 402, 51.6% female) and in either the 9th (n = 389, 49.94%) or 10th grade (n = 295, 37.87%) (see Table 1). The predominant ethnicity represented is Hispanic (n = 526, 67.52%). There is a greater percentage of Hispanic teens enrolled in the COPE TEEN group than teens enrolled in the Healthy Teens group (p = .00).
Table 1.
Teen demographics by group.
| Characteristic | Total (N = 779) |
COPE (n = 358) |
Control (n = 421) |
p | ||||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | |||
| Age (years)a | 14.74 | 0.73 | 14.75 | 0.76 | 14.74 | 0.70 | 0.89 | |
| BMIa | 24.43 | 5.92 | 24.93 | 6.18 | 24.01 | 5.65 | 0.03 | |
| BMI percentilea | 70.59 | 27.11 | 72.97 | 25.02 | 68.56 | 28.64 | 0.02 | |
| Total
|
COPE
|
Control
|
||||||
| n | % | n | % | n | % | |||
|
| ||||||||
| Genderb | Female | 402 | 51.60% | 195 | 54.47% | 207 | 49.17% | 0.15 |
| Male | 377 | 48.40% | 163 | 45.53% | 214 | 50.83% | ||
| Grade levelb | 9th grade | 389 | 49.94% | 204 | 56.98% | 185 | 43.94% | 0.00 |
| 10th grade | 295 | 37.87% | 107 | 29.89% | 188 | 44.66% | ||
| 11th grade | 89 | 11.42% | 45 | 12.57% | 44 | 10.45% | ||
| 12th grade | 6 | 0.77% | 2 | 0.56% | 4 | 0.95% | ||
| Raceb | American native | 27 | 3.47% | 10 | 2.79% | 17 | 4.04% | 0.00 |
| Asian | 31 | 3.98% | 7 | 1.96% | 24 | 5.70% | ||
| Black | 77 | 9.88% | 30 | 8.38% | 47 | 11.16% | ||
| White | 110 | 14.12% | 31 | 8.66% | 79 | 18.76% | ||
| Hispanic | 526 | 67.52% | 275 | 76.82% | 251 | 59.62% | ||
| Other | 8 | 1.03% | 5 | 1.40% | 3 | 0.71% | ||
| CDC BMI categoriesb | Underweight | 14 | 1.80% | 1 | 0.28% | 13 | 3.09% | 0.02 |
| Healthy weight | 433 | 55.58% | 196 | 54.75% | 237 | 56.29% | ||
| Overweight | 148 | 19.00% | 72 | 20.11% | 76 | 18.05% | ||
| Obese | 182 | 23.36% | 88 | 24.58% | 94 | 22.33% | ||
| Unreported | 2 | 0.26% | 1 | 0.28% | 1 | 0.24% | ||
| Depressionb | Average | 645 | 82.80% | 292 | 81.56% | 353 | 83.85% | 0.91 |
| Mildly elevated | 52 | 6.68% | 25 | 6.98% | 27 | 6.41% | ||
| Moderately elevated | 47 | 6.03% | 23 | 6.42% | 24 | 5.70% | ||
| Extremely elevated | 24 | 3.08% | 12 | 3.35% | 12 | 2.85% | ||
| Not reported | 11 | 1.41% | 6 | 1.68% | 5 | 1.19% | ||
| Anxietyb | Average | 597 | 76.64% | 276 | 77.09% | 321 | 76.25% | 0.24 |
| Mildly elevated | 81 | 10.40% | 31 | 8.66% | 50 | 11.88% | ||
| Moderately elevated | 58 | 7.45% | 31 | 8.66% | 27 | 6.41% | ||
| Extremely elevated | 29 | 3.72% | 16 | 4.47% | 13 | 3.09% | ||
| Not reported | 14 | 1.80% | 4 | 1.12% | 10 | 2.38% | ||
Note. M = mean; SD = standard deviation.
t-test.
Chi-square.
Although there was a significant difference in grade level by group (COPE TEEN has more 9th grade students and Healthy Teens has more 10th grade students), there was no statistically significant difference for their age in years (p = .89).
Greater than 40% of the sample is either overweight (n = 148, 19%) or obese (n = 182, 23.36%) and 7.1% (n = 56) has a BMI percentile ≥ 99. There was a significant difference between groups for BMI (p = .02) and BMI percentile (p = .03) with COPE TEEN participants being higher for each.
At baseline, 15.79% (n = 123) of the students had above average scores on the Beck Youth Inventory Depression Scale indicating mild (n = 52, 6.68%), moderate (n = 47, 6.03%), or extreme (n = 24, 3.08%) elevated scores (see Table 1). At baseline, the number of teens referred to their school counselor for the two trigger questions was 140 (17.3%). The number of teens who had a letter sent to their parents for a depression T-score ≥ 70 was 24 (2.9%). Anxiety symptomology was slightly higher with 21.56% (n = 168) of teens reporting responses suggesting mild (n = 81, 10.4%), moderate (n = 58, 7.45%) or extreme (n = 29, 3.72%) elevated scores. There were no significant differences between groups at baseline for BYI anxiety (p = .24) or BYI depression (p = .91).
There were significant differences between groups on three of the four subscales of the AMHISA including assimilation (p = .00), separation (p = .02), and integration (p = .01). The COPE TEEN intervention teens had lower assimilation scores and higher separation and integration scores when compared to Healthy Teens at baseline. There were no other significant baseline differences between groups on any of the other scales. The COPE TEEN intervention teens reported watching more hours of TV per day than Healthy Teens group teens (p = .02).
3.3. Baseline characteristics and comparisons between groups: Parents
The teens’ parents participating in the study are primarily female (n = 382, 86.82%) and also Hispanic (n = 286, 65%) (see Table 4). Over half of the parents are married (n = 249, 56.59%). A large percentage of parents did not graduate from high school (n = 157, 35.68%) with 15.23% (n = 67) reporting they were college graduates. The percentage of parents reporting public assistance (i.e., food stamps, state health insurance) was 41.59% (n = 183).
Table 4.
Parent demographics by group.
| Characteristic | Total (n = 440) |
COPE (n = 200) |
Control (n = 240) |
p | ||||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | |||
| Age (years)a | 41.11 | 7.33 | 40.73 | 6.83 | 41.43 | 7.72 | 0.32 | |
| BMIa | 29.68 | 7.09 | 30.07 | 6.16 | 29.36 | 7.76 | 0.31 | |
| Total
|
COPE
|
Control
|
||||||
| n | % | n | % | n | % | |||
|
| ||||||||
| Genderb | Female | 382 | 86.82% | 184 | 92.00% | 198 | 82.50% | 0.00 |
| Male | 58 | 13.18% | 16 | 8.00% | 42 | 17.50% | ||
| Raceb | American native | 14 | 3.18% | 7 | 3.50% | 7 | 2.92% | 0.00 |
| Asian | 16 | 3.64% | 4 | 2.00% | 12 | 5.00% | ||
| Black | 32 | 7.27% | 11 | 5.50% | 21 | 8.75% | ||
| White | 86 | 19.55% | 21 | 10.50% | 65 | 27.08% | ||
| Hispanic | 286 | 65.00% | 154 | 77.00% | 132 | 55.00% | ||
| Other | 3 | 0.68% | 2 | 1.00% | 1 | 0.42% | ||
| Not reported | 3 | 0.68% | 1 | 0.50% | 2 | 0.83% | ||
| Ethnicityb | Hispanic or Latino | 286 | 65.00% | 154 | 77.00% | 132 | 55.00% | 0.00 |
| Marital statusb | Married | 249 | 56.59% | 115 | 57.50% | 134 | 55.83% | 0.77 |
| Unmarried | 190 | 43.18% | 85 | 42.50% | 105 | 43.75% | ||
| Not reported | 1 | 0.23% | 0 | 0.00% | 1 | 0.42% | ||
| Educationb | Less than high school | 157 | 35.68% | 92 | 46.00% | 65 | 27.08% | 0.00 |
| High school graduate | 102 | 23.18% | 49 | 24.50% | 53 | 22.08% | ||
| Some college | 111 | 25.23% | 40 | 20.00% | 71 | 29.58% | ||
| College graduate | 67 | 15.23% | 18 | 9.00% | 49 | 20.42% | ||
| Not reported | 3 | 0.68% | 1 | 0.50% | 2 | 0.83% | ||
| Public assistanceb | No | 252 | 57.27% | 99 | 49.50% | 153 | 63.75% | 0.00 |
| Yes | 183 | 41.59% | 99 | 49.50% | 84 | 35.00% | ||
| Not Reported | 5 | 1.14% | 2 | 1.00% | 3 | 1.20% | ||
| Annual household incomec | Less than $7000 | 53 | 12.05% | 30 | 15.00% | 23 | 9.58% | 0.00 |
| $7000-$10,000 | 42 | 9.55% | 23 | 11.50% | 19 | 7.92% | ||
| $10,001–$15,000 | 39 | 8.86% | 23 | 11.50% | 16 | 6.67% | ||
| $15,001–$20,000 | 56 | 12.73% | 33 | 16.50% | 23 | 9.58% | ||
| $20,001–$30,000 | 59 | 13.41% | 27 | 13.50% | 32 | 13.33% | ||
| $30,001–$40,000 | 50 | 11.36% | 19 | 9.50% | 31 | 12.92% | ||
| Greater than $40,000 | 119 | 27.05% | 31 | 15.50% | 88 | 36.67% | ||
| Not reported | 22 | 5.00% | 14 | 7.00% | 8 | 3.33% | ||
| Parent BMI categoriesb | Underweight (<18.5) | 2 | 0.45% | 0 | 0.00% | 2 | 0.83% | 0.08 |
| Normal (18.5–24.9) | 98 | 22.27% | 36 | 18.00% | 62 | 25.83% | ||
| Overweight (25.0–29.9) | 158 | 35.91% | 71 | 35.50% | 87 | 36.25% | ||
| Obese (30.0 and above) | 154 | 35.00% | 78 | 39.00% | 76 | 31.67% | ||
| Not reported | 28 | 6.36% | 15 | 7.50% | 13 | 5.42% | ||
Note. M = mean; SD = standard deviation.
t-test.
Chi-square.
Monte Carlo method.
There are more male parents participating in the Healthy Teens group than the COPE TEEN group (p = .00). More parents are Hispanic in the COPE TEEN group versus the Healthy Teens group (p = 00). COPE TEEN parents have lower education levels (p = .00) and report more public assistance (p = .00) than Healthy Teens parents. COPE TEEN parents reported lower annual household incomes (p = .00). Parent BMI was calculated from self-reported height and weight with 70.91% either being overweight (n = 158, 35.91%) or obese (n = 154, 35%). Although not statistically significant, there is a trend for COPE TEEN parents to be overweight or obese (p = .08) compared to Healthy Teens parents.
3.4. Baseline characteristics and comparisons between groups: Teachers
Thirty health teachers are participating in the study. The average age of the teachers is 43.23 (SD = 9.96) years and average teaching experience in years is 14.45 (SD = 7.81). The average number of years teaching health is 8.15 (SD = 5.93) with a significant difference between groups with greater years of teaching experience in the Healthy Teens teachers (p = .05).
4. Discussion
The COPE TEEN study is a large randomized controlled trial testing a novel cognitive–behavioral skills building intervention to promote healthy behaviors, mental health, social skills and academic performance as well as prevent overweight/obesity in a sample of culturally diverse high school teens whose rates of overweight/obesity are higher than national averages.
Despite the rapidly increasing incidence and adverse health outcomes associated with both overweight and mental health problems, very few theory-based intervention studies have been conducted with adolescents to improve their healthy lifestyle behaviors, mental health outcomes, social skills and academic performance [19,20,23,24,65–67]. Unfortunately, physical and mental health services continue to be largely separated instead of integrated in the nation’s healthcare system, which often leads to inadequate identification and treatment of these significant adolescent health problems. Furthermore, most obesity treatment and prevention trials have focused on school-age children [20–22,68–77].
Middle adolescence is a key time in development to implement prevention programs as teens are beginning to establish long-term health behavior patterns. However, very few rigorously designed, theory-based comprehensive health promotion intervention studies have been conducted with high school teens [67]. There also is a paucity of studies in which school-based health promotion programs have measured academic achievement. A small body of evidence exists to support positive academic outcomes with mental health/social skills building interventions, asthma education, and physical activity programs. However, the majority of these studies are conducted with school-aged children [78,79]. The measurement of academic outcomes when conducting school-based health promotion programs is essential since public education has been tasked to increase and strengthen core content and to improve academic performance and graduation rates of students [79]. Of those intervention studies conducted in high schools, the majority have targeted asingle health outcome, such as substance abuse or depression. Therefore, it is largely unknown whether health promotion programs also can be effective in improving physical and mental health as well as academic outcomes [79]. In the national agenda for improving the state of obesity, it is unfortunate that mental health has been largely missing as a key construct to target in programs even though findings from prior work have indicated that, when teens have elevated anxiety/depressive symptoms, their cognitive beliefs about being able to engage in healthy lifestyle behaviors are weak and they engage less in healthy lifestyle behaviors [34]. Thus, there is little evidence to guide high schools in health curricula content that would positively influence the healthy lifestyle behaviors, mental health, social skills and academic performance of their students.
Further, intervention studies targeting high school teens have demonstrated several important limitations in the literature, including lack of theoretical frameworks to guide the interventions, lack of attention control or comparison groups and measurement of only short-term outcomes [80,81]. Recent systematic reviews of treatment and prevention studies for child and teen obesity and a literature review on school-based intervention studies concluded that more research is urgently needed, especially with culturally diverse groups [80–82]. Another review noted that strong conclusions about the efficacy of school-based obesity prevention programs cannot be drawn because there are a small number of published studies, and the ones that have been published have major methodological flaws [76]. The public health problems of obesity and mental health problems along with health disparities among teens highlight the need for evidence-based interventions in high schools to improve their health and academic performance. Our study is significant because it has the potential to not only extend the science on school-based interventions, but to generate a high level of evidence through a rigorously designed trial to support an intervention that could be routinely integrated into health education curricula and delivered by teachers in “real world” high school settings to improve health and academic outcomes high-risk adolescent populations.
In this study, the intervention was delivered by teachers instead of healthcare providers or trained study team members. In prior pilot work, nurse practitioners who delivered the COPE TEEN and attention control interventions did so with excellent intervention fidelity and positive effects for the COPE TEEN intervention [33]. Approximately half of the teachers in this study have been observed to have departures and omissions from the COPE TEEN protocol, which may impact the efficacy of the COPE TEEN intervention on the study’s outcomes. As a result, this trial is in essence testing effectiveness of the intervention (i.e., translation of research to real-world practice). In future studies in which teachers are delivering experimental interventions, it is important for researchers to pay meticulous attention to fidelity and provide ongoing support to the teachers in order to enhance fidelity to the intervention.
This study shows the feasibility of recruiting a large, primarily Hispanic sample. Baseline findings identified a need for implementing a healthy lifestyles program to promote healthy eating, physical activity, and positive strategies for dealing with stressors. Findings are generalizable to the population sampled.
This study has several strengths and limitations. Strengths include the randomized controlled design, large sample size, largely Hispanic population, and measurement of physical health indicators, psychosocial outcomes, and academic performance. This study also has some limitations, including less than adequate time devoted to practicing the cognitive-behavioral skills in the COPE TEEN intervention during the teacher training, and not enough follow-up with the teachers to reinforce important intervention content during the delivery of the program. Increased practice time of COPE TEEN skills and more consistent follow-up with the teachers during the course of intervention delivery may have enhanced fidelity to the program. Another limitation is that fact that only 56% of the parents consented to participate in the study, which may affect moderation analyses. Aggressive attempts to recruit parents into future studies with high school teens are needed in order to determine parental influences on adolescent health outcomes. Additional limitations include that healthy eating was not operationalized in the Perceived Difficulty scale, potential impact of students receiving course credit for discussing information with parents, professional development credit received by the teachers for implementing the curriculum, teacher self-report of objective completion, lack of an academic indicator for comparison at baseline, student self-selection for participation in the study and schools not being matched between intervention and control groups.
4.1. Challenges of school-based interventions with lessons learned
The experience recruiting each cohort differed. The first cohort of teachers were assigned by the principals and the school district’s superintendent to deliver the interventions and did not hear about the study until one to two weeks before the training just prior to their winter break. Therefore, extra time had to be spent with the teachers to fully discuss and address their concerns, one of which was having little time to adjust their curricula to incorporate the interventions. This dampened enthusiasm for the project and may have affected intervention fidelity.
For the second cohort of students, the principals of four new schools in the same school district as Cohort 1 were approached approximately 6 months in advance of implementation. The research team conducted a formal presentation during the district health educators meeting. Principals were approached in person to discuss the project and get administrative support for the project. Teachers were then approached in person to discuss their participation.
With the third school district, presentations began with the superintendent and district administration. Then, the research team presented at a principals meeting at the district. Interested principals sent teacher representatives to a district meeting for a teacher presentation. Interested teachers indicated which schools may want to participate. Each school was visited in person and the project was discussed.
An important lesson learned through the school and teacher recruitment process was that obtaining “buy-in” from the teachers is important for their level of enthusiasm and degree of active participation in the training, which ultimately can affect delivery of interventions. Further, learning about what type of teacher support is needed throughout intervention delivery and the provision of ongoing teacher support is important for intervention fidelity.
Our research team had to respond to other challenges in implementing this trial. The process of obtaining informed consent/assent from parents without direct parent contact is challenging and strategies to increase parent participation need to be thoughtfully considered and implemented with students’ teachers to increase parent participation in research. One factor that may have heavily affected our parent participation rate was that Arizona’s anti-immigrant law, SB 1070, was passed at approximately the same time as our study commenced. Parents who were undocumented may have felt if they signed a document they would risk being identified and deported. Finally, when conducting school-based work, it is important to plan for frequent moves of students between schools in areas where this is commonly encountered. Research teams have to be prepared to be diligent in obtaining alternative contacts for students and tracking them so that outcome measures on as many participating subjects as possible can be obtained. Finally, teacher delivered interventions must be feasible and made easy for teachers to deliver as they are faced with having to comply with state standards for curriculum delivery and multiple competing demands. In addition, making sure that intervention programs are consistent with state health curricula standards will facilitate “buy-in” from schools. Planning on extra time to build support from school superintendents, principals and teachers when planning school-based intervention studies will go a long way in overcoming challenges in implementation.
In summary, there is a paucity of evidence-based interventions to enhance physical, psychosocial, and academic outcomes in at-risk high school adolescents. If the efficacy of the COPE TEEN program is supported, it will offer schools a curriculum that can be easily incorporated into high school health courses to improve adolescent healthy lifestyle behaviors, psychosocial outcomes and academic performance.
Acknowledgments
This study was funded by the National Institutes of Health/National Institute of Nursing Research 1R01NR012171. The authors would like to thank and recognize Kim Weberg MS, Kristine Hartmann, MS, Alan Moreno, Krista Oswalt, PhD, Jonathon Rose, and Megan Paradise, RN for their outstanding contributions and dedication to this study.
References
- 1.Evans D, Seligman M, Evans D, Foa E, Gur R, Hendin H, et al. Introduction. In: Seligman M, et al., editors. Treating and preventing adolescent mental health disorders: what we know and what we don’t know. Oxford, New York: Oxford University Press; 2005. pp. xxv–xl. [Google Scholar]
- 2.Centers for Disease Control Prevention. Youth risk behavior surveillance—United States, 2011. MMRW Surveill Summ. 2012;61:1–162. [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. J Am Med Assoc. 2010;303:242–9. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control, Prevention. Children and teens told by doctors that they were overweight—United States, 1999–2002. MMWR—Morbidity & Mortality Weekly Report. 2005;54:848–9. [PubMed] [Google Scholar]
- 5.Melnyk BM, Moldenhauer Z. The KySS guide to child and adolescent mental health screening Early Intervention and Health Promotion. Cherry Hill, New Jersey: National Association of Pediatric Nurse Practitioners; 2006. [Google Scholar]
- 6.Sjoberg RL, Nilsson KW, Leppert J. Obesity, shame, and depression in school-aged children: a population-based study. Pediatrics. 2005;116:e389–92. doi: 10.1542/peds.2005-0170. [DOI] [PubMed] [Google Scholar]
- 7.Strauss RS. Childhood obesity and self-esteem. Pediatrics. 2000;105:e15. doi: 10.1542/peds.105.1.e15. [DOI] [PubMed] [Google Scholar]
- 8.Bell S, Morgan S. Children’s Attitudes and behavioral intentions toward a peer presented as obese. Does a medical explanation for the obesity make a difference? J Pediatr Psychol. 2002;25:137–45. doi: 10.1093/jpepsy/25.3.137. [DOI] [PubMed] [Google Scholar]
- 9.Stein REK, Zitner LE, Jensen PS. Interventions for adolescent depression in primary care. Pediatrics. 2006;118:669–82. doi: 10.1542/peds.2005-2086. [DOI] [PubMed] [Google Scholar]
- 10.Richardson LP, Katzenellenbogen R. Childhood and adolescent depression: the role of PCPs in diagnosis and treatment. Curr Probl Pediatr Adolesc Health Care. 2005;35:1–24. doi: 10.1016/j.cppeds.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 11.Weisz JR, McCarty CA, Valeri SM. Effects of psychotherapy for depression in children and adolescents: a meta-analysis. Psychol Bull. 2006;132:132–49. doi: 10.1037/0033-2909.132.1.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Falkner NH, Neumark-Sztainer D, Story M, Jeffery RW, Beuhring T, Resnick MD. Social, educational, and psychological correlates of weight status in adolescents. Obes Res. 2001;9:32–42. doi: 10.1038/oby.2001.5. [DOI] [PubMed] [Google Scholar]
- 13.Friedlander SL, Larkin EK, Rosen CL, Palermo TM, Redline S. Decreased quality of life associated with obesity in school-aged children. Arch Pediatr Adolesc Med. 2003;157(12):1206–11. doi: 10.1001/archpedi.157.12.1206. [DOI] [PubMed] [Google Scholar]
- 14.Goodman E, Whitaker R. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics. 2002;109:497–504. doi: 10.1542/peds.110.3.497. [DOI] [PubMed] [Google Scholar]
- 15.Lobstein T, Baur L, Uauy R. Obesity in children and young people: a crisis in public health. London, UK: IASO International Obesity Task Force; 2004. [DOI] [PubMed] [Google Scholar]
- 16.BeLue R, Francis LA, Colaco B. Mental health problems and overweight in a nationally representative sample of adolescents: effects of race and ethnicity. Pediatrics. 2009;123:697–702. doi: 10.1542/peds.2008-0687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Richardson LP, Davis R, Poulton R, McCauley E, Moffitt TE, Caspi A, et al. A longitudinal evaluation of adolescent depression and adult obesity. Arch Pediatr Adolesc Med. 2003;157:739–45. doi: 10.1001/archpedi.157.8.739. [DOI] [PubMed] [Google Scholar]
- 18.Herva A, Laitinen J, Miettunen J, Viejola J, Karvonen JT, Joukamaa M. Obesity and depression: results from the longitudinal Northern Finland 1966 birth cohort study. Int J Obes. 2006;30:520–7. doi: 10.1038/sj.ijo.0803174. [DOI] [PubMed] [Google Scholar]
- 19.Neumark-Sztainer DR, Friend SE, Flattum CF, Hannan PJ, Story MT, Bauer KW, et al. New moves—preventing weight-related problems in adolescent girls: a group-randomized study. Am J Prev Med. 2010;39:421–32. doi: 10.1016/j.amepre.2010.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harris KC, Kuramoto LK, Schulzer M, Retallack JE. Effect of school-based physical activity interventions on body mass index in children: a meta-analysis. Can Med Assoc J. 2009;180:719–26. doi: 10.1503/cmaj.080966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Klesges RC, Obarzanek E, Kumanyika S, Murray DM, Klesges LM, Relyea GE, et al. The Memphis Girls’ health enrichment multi-site studies (GEMS) Arch Pediatr Adolesc Med. 2010;164:1007–14. doi: 10.1001/archpediatrics.2010.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Robinson TN, Matheson DM, Kraemer HC, Wilson DM, Obarzanek E, Thompson NS, et al. A randomized controlled trial of culturally tailored dance and reducing screen time to prevent weight gain in low-income African American Girls: Stanford GEMS. Arch Pediatr Adolesc Med. 2010;164:995–1004. doi: 10.1001/archpediatrics.2010.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Singh AS, Chinapaw MJM, Brug J, van Mechelen W. Dutch obesity intervention in teenagers: effectiveness of a school-based program on body composition and behavior. Arch Pediatr Adolesc Med. 2009;163:309–17. doi: 10.1001/archpediatrics.2009.2. [DOI] [PubMed] [Google Scholar]
- 24.Lubans DR, Morgan PJ, Okely AD, Dewar D, Collins CE, Batterham M, et al. Preventing obesity among adolescent girls: one-year outcomes of the Nutrition and Enjoyable Activity for Teen Girls (NEAT Girls) cluster randomized controlled trial. Arch Pediatr Adolesc Med. 2012;166:821–7. doi: 10.1001/archpediatrics.2012.41. [DOI] [PubMed] [Google Scholar]
- 25.Stice E, Shaw H, Bohon C, Marti CN, Rohde P. A meta-analytic review of depression prevention programs for children and adolescents: factors that predict magnitude of intervention effects. J Consult Clin Psychol. 2009;77:486–503. doi: 10.1037/a0015168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Calear AL, Christensen H. Systematic review of school-based prevention and early intervention programs for depression. J Adolesc. 2010;33:429–38. doi: 10.1016/j.adolescence.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 27.Ellis A. Reason and emotion in psychotherapy. New York, NY: Lyle Stuart; 1962. [Google Scholar]
- 28.Seligman MEP. Helplessness: on depression, development and death. San Francisco, CA: Freeman; 1975. [Google Scholar]
- 29.Skinner B. Science and human behavior. New York, NY: Macmillan; 1953. [Google Scholar]
- 30.Lewinsohn PM. Manual of instructions for the behavioral ratings used for the observation of interpersonal behavior. In: Mash EJ, Terdal LG, editors. Behavior therapy assessment. New York, NY: Springer Publishing Company; 1974. pp. 335–45. [Google Scholar]
- 31.Beck AT, Rush AJ, Shaw B, Emery G. Cognitive therapy of depression. New York: Guilford Press; 1979. [Google Scholar]
- 32.Lam D. A brief overview of CBT techniques. In: Freeman S, Freeman A, editors. Cognitive behavior therapy in nursing practice. New York: Springer Publishing Company; 2005. pp. 29–47. [Google Scholar]
- 33.Melnyk B, Jacobson D, Kelly S, O’Haver J, Small L, Mays M. Improving the mental health, healthy lifestyle choices and physical health of Hispanic adolescents: a randomized controlled pilot study. J Sch Health. 2009;79:575–84. doi: 10.1111/j.1746-1561.2009.00451.x. [DOI] [PubMed] [Google Scholar]
- 34.Melnyk BM, Small L, Morrison-Beedy D, Strasser A, Spath L, Kreipe R, et al. Mental health correlates of healthy lifestyle attitudes, beliefs, choices, and behaviors in overweight adolescents. J Pediatr Health Care. 2006;20:401–6. doi: 10.1016/j.pedhc.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 35.Melnyk BM, Small L, Morrison-Beedy D, Strasser A, Spath L, Kreipe R, et al. The COPE healthy lifestyles TEEN program: feasibility, preliminary efficacy & lessons learned from an after school group intervention with overweight adolescents. J Pediatr Health Care. 2007;21:315–22. doi: 10.1016/j.pedhc.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 36.Kelly S, Melnyk BM, Jacobson D, O’Haver J. Correlates among healthy lifestyle choices, social support, and healthy behaviors in adolescents: implications for behavioral change strategies and future research. J Pediatr Health Care. 2011;25:216–23. doi: 10.1016/j.pedhc.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 37.Ritchie T. Evaluation of the impact of the COPE healthy lifestyles TEEN program in a high school health class. West Virginia University; 2011. [Google Scholar]
- 38.Compton SN, March JS, Brent D, Albano AMt, Weersing R, Curry J. Cognitive–behavioral psychotherapy for anxiety and depressive disorders in children and adolescents: an evidence-based medicine review. J Am Acad Child Adolesc Psychiatry. 2004;43:930–59. doi: 10.1097/01.chi.0000127589.57468.bf. [see comment] [DOI] [PubMed] [Google Scholar]
- 39.Lubans DR, Foster C, Biddle SJH. Review of mediators of behavior in interventions to promote physical activity among children and adolescents. Prev Med. 2008;47:463–70. doi: 10.1016/j.ypmed.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 40.Moher D, Hopewell S, Schultz KF, Montori V, Gotzsche PC, Devereaux PJ, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c869. doi: 10.1136/bmj.c869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Unger BJ, Gallaher P, Shakib S, Ritt-Olson A, Palmer PH, Johnson CA. The AHIMSA acculturation scale: a new measure of acculturation for adolescents in a multicultural society. J Early Adolesc. 2002;22:225–51. [Google Scholar]
- 42.Melnyk BM. Coping with unplanned childhood hospitalization: effects of informational interventions on mothers and children. Nurs Res. 1994;43:50–5. [PubMed] [Google Scholar]
- 43.Melnyk BM, Alpert-Gillis LJ, Hensel PB, Cable-Beiling RC, Rubenstein JS. Helping mothers cope with a critically ill child: a pilot test of the COPE intervention. Res Nurs Health. 1997;20:3–14. doi: 10.1002/(sici)1098-240x(199702)20:1<3::aid-nur2>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 44.Melnyk BM. Healthy Lifestyle Beliefs Scale. Hammondsport, NY: COPE for HOPE, Inc; 2003. [Google Scholar]
- 45.Kelly S, Melnyk BM, Belyea M. Predicting healthy lifestyle behaviors in adolescents: a test of the information, motivation, and behavioral skills model. Res Nurs Health. 2012;35:146–63. doi: 10.1002/nur.21462. [DOI] [PubMed] [Google Scholar]
- 46.Melnyk BM. Healthy Lifestyle Perceived Difficulty Scale. Hammondsport, NY: COPE for HOPE, Inc; 2003. [Google Scholar]
- 47.Williams SS, Doyle TM, Pittman LD, Weiss LH, Fisher JD, Fisher WA. Role played safer sex skills of heterosexual college students influenced by both personal and partner factors. AIDS Behav. 1998;2:177–87. [Google Scholar]
- 48.Fisher WA, Williams SS, Fisher JD, Malloy TE. Understanding AIDS risk behavior among sexually active urban adolescents: an empirical test of the information–motivation–behavioral skills model. AIDS Behav. 1999;3:13–23. [Google Scholar]
- 49.Melnyk BM. Healthy Lifestyles Behavior Scale. Hammondsport, NY: COPE for HOPE, Inc; 2003. [Google Scholar]
- 50.Tudor-Locke C, Williams JE, Reis JP, Pluto D. Utility of pedometers for assessing physical activity: construct validity. Sports Med. 2004;34:281–91. doi: 10.2165/00007256-200434050-00001. [DOI] [PubMed] [Google Scholar]
- 51.Beck JS, Beck AT, Beck JJ. Youth inventories for children and adolescents: manual. 2. San Antonio, Texas: Harcourt Assessment; 2005. [Google Scholar]
- 52.Steer RA, Kumar G, Beck AT, Beck JS. Dimensionality of the Beck Youth Inventories with child psychiatric outpatients. J Psychopathol Behav Assess. 2005;27:123–31. [Google Scholar]
- 53.Gresham FM, Elliot SN. Social skills rating system manual. Minneapolis, MN: NCS Pearson, Inc; 1990. [Google Scholar]
- 54.Melnyk BM, Small L. Activity Knowledge Scale. Hammondsport, NY: COPE for HOPE, Inc; 2003. [Google Scholar]
- 55.Melnyk BM, Small L. Nutrition Knowledge Scale. Hammondsport, NY: COPE for HOPE, Inc; 2003. [Google Scholar]
- 56.Han SS, Weiss B. Sustainability of teacher implementation of school-based mental health programs. J Abnorm Child Psychol. 2005;33:665–79. doi: 10.1007/s10802-005-7646-2. [DOI] [PubMed] [Google Scholar]
- 57.Beets MW, Flay BR, Vuchinich S, Acock AC, Li KK, Allred C. School climate and teachers’ beliefs and attitudes associated with implementation of the positive action program: a diffusion of innovations model. Prev Sci. 2008;9:264–75. doi: 10.1007/s11121-008-0100-2. [DOI] [PubMed] [Google Scholar]
- 58.Bellg AJ, Borrelli B, Resnick B, Hecht J, Minicucci D, Ory M, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH behavior change consortium. Health Psychol. 2004;23:443–51. doi: 10.1037/0278-6133.23.5.443. [DOI] [PubMed] [Google Scholar]
- 59.Sidani S, Braden C. Evaluating nursing interventions: a theory-driven approach. Thousand Oaks, CA: Sage Publications, Inc; 1998. [Google Scholar]
- 60.Yeaton W, Sechrest L. Critical dimension in the choice and maintenance of successful treatments: strength, integrity, and effectiveness. J Consult Clin Psychol. 1981;49:156–67. doi: 10.1037//0022-006x.49.2.156. [DOI] [PubMed] [Google Scholar]
- 61.McDowell MA, Fryar CD, Hirsch R, Ogden CL. Anthropometric reference data for children and adults: U.S. population, 1999–2002. Adv Data. 2005;361:1–5. [PubMed] [Google Scholar]
- 62.Tudor-Locke C, Bassett DR. How many steps/day are enough? Preliminary pedometer indices for public health. Sports Med. 2004;34:1–8. doi: 10.2165/00007256-200434010-00001. [DOI] [PubMed] [Google Scholar]
- 63.Berkey CS, Colditz GA. Adiposity in adolescents: change in actual BMI works better than change in BMI z score for longitudinal studies. Ann Epidemiol. 2007;17:44–50. doi: 10.1016/j.annepidem.2006.07.014. [DOI] [PubMed] [Google Scholar]
- 64.Ogden CL, Fryar CD, Carroll MD, Flegal KM. Mean body weight, height, and body mass index, United States 1960–2002. Adv Data. 2004;347:1–17. [PubMed] [Google Scholar]
- 65.Khambalia AZ, Dickinson S, Hardy LL, Gill T, Baur LA. A synthesis of existing systematic reviews and meta-analyses of school-based behavioural interventions for controlling and preventing obesity. Obes Rev. 2012;13:214–33. doi: 10.1111/j.1467-789X.2011.00947.x. [DOI] [PubMed] [Google Scholar]
- 66.Whittemore R, Chao A, Popick R, Grey M. School-based internet obesity prevention programs for adolescents: a systematic literature review. Yale J Biol Med. 2013;86:49–62. [PMC free article] [PubMed] [Google Scholar]
- 67.Melnyk B, Small L, Moore N. The worldwide epidemic of child and adolescent overweight and obesity: calling all clinicians and researchers to intensify efforts in prevention and treatment. Worldviews Evid Based Nurs. 2008;5:109–12. doi: 10.1111/j.1741-6787.2008.00134.x. [DOI] [PubMed] [Google Scholar]
- 68.Harrell J, McMurray R, Bangdiwala S, Frauman A, Gansky S, Bradley C. Effects of a school-based intervention to reduce cardiovascular disease risk factors in elementary-school children: the Cardiovascular Health in Children (CHIC) study. Pediatrics. 1996;128:797–805. doi: 10.1016/s0022-3476(96)70332-3. [DOI] [PubMed] [Google Scholar]
- 69.Harrell J, Gansky S, McMurray R, Bangdiwala S, Frauman A, Bradley C. School-based interventions improve heart health in children with multiple cardiovascular disease risk factors. Pediatrics. 1998;102:371–80. doi: 10.1542/peds.102.2.371. [DOI] [PubMed] [Google Scholar]
- 70.Harrell J, Pearce P, Markland E, Wilson K, Bradley C, McMurray R. Assessing physical activity in adolescents: common activities of children in 6th–8th grades. J Am Acad Nurse Pract. 2003;15:170–8. doi: 10.1111/j.1745-7599.2003.tb00259.x. [DOI] [PubMed] [Google Scholar]
- 71.Harrell J, McMurray R, Baggett C, Pennell M, Pearce P, Bangdiwala S. Energy costs of physical activities in children and adolescents. Med Sci Sports Exerc. 2005;37:329–36. doi: 10.1249/01.mss.0000153115.33762.3f. [DOI] [PubMed] [Google Scholar]
- 72.Hoelscher D, Day R, Lee E, Frankowski R, Kelder S, Ward J, et al. Measuring the prevalence of overweight in Texas schoolchildren. Am J Public Health. 2004;94:1002–8. doi: 10.2105/ajph.94.6.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Huhman M, Potter L, Wong F, Banspach S, Duke J, Heitzler C. Effects of a mass media campaign to increase physical activity among children: year-1 results of the VERB campaign. Pediatrics. 2005;116:e277–84. doi: 10.1542/peds.2005-0043. [DOI] [PubMed] [Google Scholar]
- 74.Lyznicki J, Young D, Riggs J, Davis R, Council on Scientific Affairs AMA Obesity: assessment and management in primary care. Am Fam Physician. 2001;63:2185–96. [PubMed] [Google Scholar]
- 75.Nader P, Sellers D, Johnson C, Perry C, Stone E, Cook K, et al. The effect of adult participation in a school-based family intervention to improve Children’s diet and physical activity: the Child and Adolescent Trial for Cardiovascular Health. Prev Med. 1996;25:455–64. doi: 10.1006/pmed.1996.0077. [DOI] [PubMed] [Google Scholar]
- 76.Kropski J, Keckley P, Jensen G. School-based obesity prevention programs: an evidence-based review. Obesity. 2008;16:1009–18. doi: 10.1038/oby.2008.29. [DOI] [PubMed] [Google Scholar]
- 77.Katz DL, O’Connell M, Njike VY, Yeh M-C, Nawaz H. Strategies for the prevention and control of obesity in the school setting: systematic review and meta-analysis. Int J Obes. 2008;32:1780–9. doi: 10.1038/ijo.2008.158. [DOI] [PubMed] [Google Scholar]
- 78.Evans D, Clark N, Feldman C, Rips J, Kaplan D, Levison M, et al. A school health education program for children with asthma aged 8–11 years. Health Educ Q. 1987;14:267–79. doi: 10.1177/109019818701400302. [DOI] [PubMed] [Google Scholar]
- 79.Murray N, Low B, Hollis C, Cross A, Davis S. Coordinated school health programs and academic achievement: a systematic review of the literature. J Sch Health. 2007;77:589–600. doi: 10.1111/j.1746-1561.2007.00238.x. [DOI] [PubMed] [Google Scholar]
- 80.Jain A. Treating obesity in individuals and populations. BMJ. 2005;331:1387–90. doi: 10.1136/bmj.331.7529.1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Jerum A, Melnyk B. Effectiveness of interventions to prevent obesity and obesity-related complications in children and adolescents. Pediatr Nurs. 2001;27:606–10. [PubMed] [Google Scholar]
- 82.Kelly S, Melnyk B. Systematic review of multicomponent interventions with overweight middle adolescents: implications for clinical practice and future research. Worldviews Evid Based Nurs. 2008;5:113–35. doi: 10.1111/j.1741-6787.2008.00131.x. [DOI] [PubMed] [Google Scholar]


