Abstract
The objective of this prospective clinical trial was to investigate the influence of the residual coronal structure of endodontically treated teeth and the type of cement used for luting fiber posts on four-year clinical survival. Two groups (n = 60) were defined, depending on the amount of residual coronal dentin after abutment build-up and final preparation: (1) more than 50% of coronal residual structure; and (2) equal to or less than 50% of coronal residual structure. Within each group, teeth were randomly divided into 2 subgroups (n = 30) according to the material used for luting fiber posts: (A) resin core build-up material, Gradia Core; or (B) self-adhesive universal cement GCem Automix. The rate of success was assessed based on clinical and intra-oral radiographic examinations at the follow-up after 6, 12, 24, 36, and 48 months. The highest 48-month success and survival rates were recorded in group 1A (90% and 100%, respectively), whereas teeth in group 2B exhibited the lowest performance (63.3% success rate, 86.6% survival rate). Cox regression analysis revealed that neither the amount of coronal residual structure nor the luting material significantly influenced the failure risk (p > .05) (ClinicalTrials.gov, NCT01532947).
Keywords: post-and-core technique, resin cements, endodontically treated teeth, tooth preparation, clinical trial, survival rate
Introduction
Restoration of endodontically treated teeth with fiber posts and composite core systems has been extensively investigated over the past 20 years (Schwartz and Robbins, 2004; Peroz et al., 2005). Although low percentages of failure rates and satisfactory clinical performance were reported when fiber posts were used (Ferrari et al., 2007a; Schmitter et al., 2007; Cagidiaco et al., 2008b), pulpless teeth are still considered vulnerable and more susceptible to fracture compared with vital teeth (Tang et al., 2010).
The survival of endodontically treated and restored teeth depends on many baseline factors (Naumann et al., 2005), among which the amount of remaining coronal structure, restorative procedures, and material selection (Schwartz and Fransman, 2005; Tang et al., 2010) seem to be key factors affecting tooth longevity. In particular, preservation of at least one residual coronal wall or a circumferential 2-mm ferrule effect may contribute to overall tooth mechanical resistance (Stankiewicz and Wilson, 2002; Ferrari et al., 2012; Juloski et al., 2012).
The load-bearing ability of pulpless teeth may also be improved by the choice of high-filler-content composite resins for restorations. Such materials, suitable for build-up as well as for fiber post luting, would simplify the clinical procedures and result in more mechanically homogeneous restorations (Boschian Pest et al., 2002). Conversely, a laboratory study reported higher polymerization stress, lower push-out bond strength, and higher nanoleakage occurring in resin cements with a higher percentage of filler compared with those with lower filler load (Ferrari et al., 2009). However, no clinical study has so far assessed whether teeth restored with material for simultaneous post luting and core build-up have a clinical outcome significantly different from that of teeth restored with conventional resin luting cements.
Therefore, the aim of this prospective clinical study was to assess whether the amount of residual coronal structure and the type of cement used for fiber post luting (self-adhesive cement vs. composite core material) affected the four-year survival of root-filled premolars. The null hypothesis tested was that both the amount of remaining coronal dentin and the luting agent had no effect on the four-year survival of endodontically treated and crowned premolars.
Materials & Methods
Study Design
The protocol for this prospective clinical study was approved by the Institutional Review Board of the University of Siena, Italy (ClinicalTrials.gov number CT01532947). In total, 120 patients who consecutively presented at a private dental office for receiving endodontic treatment and single-unit crown restoration of premolars participated in the study. The study population consisted of 55 men and 65 women (age range, 18 to 72 yr). After receiving clear information about the purpose of the trial, according to a preliminarily approved protocol, all patients provided written, informed consent before entering the study. Only one tooth in each patient was considered. In total, 120 teeth, 53 maxillary and 67 mandibular premolars, with different amounts of remaining tooth structure, were selected for the study, providing two cohorts of 60 premolars each. The inclusion criteria – occlusal function with a natural tooth and an interproximal contact with 2 adjacent natural teeth – had to be met by the selected teeth. Baseline radiographs of the teeth included in the study did not show any signs of periapical lesions.
Two experimental groups (n = 60) were defined as follows, according to the amount of dentin left at the coronal level after endodontic treatment and after abutment preparation:
Group 1 – more than 50% of residual coronal structure and at least 2 sound walls; and
Group 2 – equal to or less than 50% of residual coronal structure, at least 1 sound wall, and a 1.5-mm ferrule effect.
A ‘wall’ was defined as a residual coronal structure of at least 3 mm in height.
Within each group, in half of the teeth (n = 30), fiber posts (GC Fiber Post; GC Corp., Tokyo, Japan) were cemented with a dual-cured composite for core build-up and post luting (Gradia Core, GC Corp.; Subgroup A, GCore), whereas in the remaining half of the premolars, fiber posts were luted with a dual-cured self-adhesive universal resin cement (GCem Automix, GC Corp.; Subgroup B, GCem).
The assignment of the teeth to either subgroup was decided by randomization of data in a Microsoft Excel spreadsheet. In the premolars with 2 roots, only 1 post was placed. For all teeth, the final restoration was a single-unit metal-ceramic crown.
Clinical procedures were performed between May 2008 and October 2008 by a single experienced operator (M.F.) with expertise in the fields of endodontics and prosthodontics.
Clinical Procedures
The procedures followed for the endodontic treatment and post space preparation are described in detail in Table 1. In Subgroup A, Gradia Core Self-Etching Bond was applied after dispensing one drop of Liquid A and B into the dispensing dish, where it was mixed thoroughly for 5 sec with the micro-tip applicator. The mixture was applied inside the post space and on the residual coronal structure, left undisturbed for 30 sec, gently air-dried, and light-cured for 10 sec in a visible-light-curing unit (GC Light, GC Corp.). GCore was dispensed into the prepared root canal through an Automix Endo tip. The post was inserted and light-cured (5 sec) to fix its position temporarily. The paste was then dispensed around the post to form the core. Light-curing from the vestibular and lingual sides (10 sec each side) was performed for final setting.
Table 1.
Detailed Description of Clinical Procedures Followed in Endodontic Treatment and Post Space Preparation
| Endodontic Treatment |
|---|
|
| Post Space Preparation |
|
In Subgroup B, after the post space was rinsed with water and dried with paper points, GCem was dispensed into the post space by means of an Automix Endo tip. The post was inserted immediately into the post space with moderate pressure and light-cured for 20 sec. The material was left to set for another 4 min before abutment build-up (GCore) and tooth preparation.
The crown preparation varied from a full chamfer with interproximal and lingual bevels to a feather finish, depending on the height and thickness of the remaining dentin. Single-unit porcelain-fused-to-metal crowns were fabricated and luted with glass-ionomer cement (Fuji Cem, GC Corp.).
Evaluation Parameters
The rate of success was assessed based on clinical and intra-oral radiographic examinations at the follow-up after 6, 12, 24, 36, and 48 mo. Periapical radiographs were taken with the modified parallel technique and Ultra-Speed films (Eastman Kodak Company, Rochester, NY, USA), and examined at 5x magnification. Evaluation was performed independently by two blinded, well-trained examiners (G.M.F. and J.J.), other than the operator who had carried out the restorative treatment. The following parameters were considered as failures: (1) post debonding, (2) post fracture, (3) vertical or horizontal root fracture, (4) crown dislodgement, and (5) periapical lesions requiring endodontic re-treatment. These occurrences were then categorized as ‘relative’ or ‘absolute’ failures. Root fractures leading to tooth extraction were considered as ‘absolute’ failures. Success was defined as the outcome in the absence of absolute and relative failures, while survival was defined as the outcome in the absence of absolute failures (Zicari et al., 2011).
Statistical Analysis
For descriptive purposes, Kaplan-Meier plots were constructed by subgroup within each group. We applied the Cox regression analysis to assess the influence on failure rate of the amount of residual coronal dentin (more than 50% of residual coronal dentin/equal to or less than 50% of residual coronal dentin), the type of luting agent (GCore/GCem), and the interaction between the 2 variables. To check that the proportional hazard assumption was satisfied in the Cox regression model, we obtained the log-minus-log plot of survival for each variable and verified the lines’ parallelism. The level of significance was set at p < .05, and statistical calculations were handled with SPSS software (SPSS Inc., Chicago, IL, USA).
Results
Data were not affected by any loss to follow-up (Fig. 1). The survival probability of the subgroups within each group is presented in Kaplan-Meier plots (Fig. 2). Teeth with more than 50% of coronal structure and posts luted with core material GCore (Group 1, Subgroup A) had the highest 48-month success (90.0%) and survival rates (100%). Conversely, the least satisfactory clinical performance was recorded for fiber posts luted with self-adhesive cement GCem on abutments with equal to or less than 50% of coronal residual structure (Group 2, Subgroup B: success rate 63.3%, survival rate 86.6%). Table 2 reports the recall rate, failure modes, and survival and success rates after a 4-year observation period in the experimental groups. Clinical failure was mainly due to periapical lesions and post debonding, while root fractures were observed after 3 and 4 yr of clinical service.
Figure 1.
Consort flow diagram.
Figure 2.
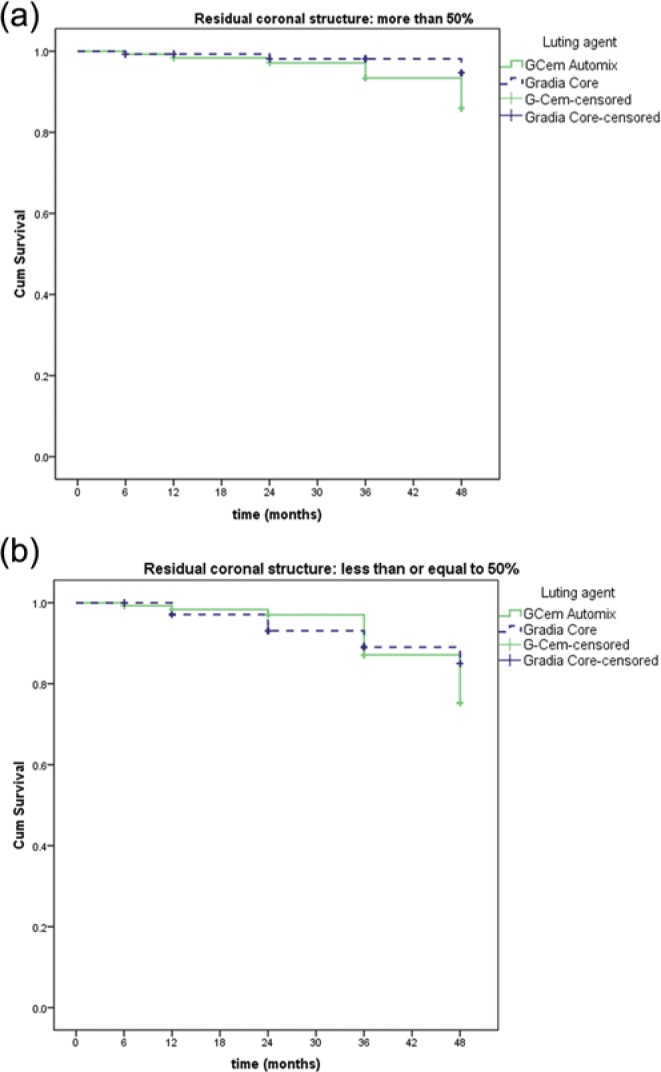
Kaplan-Meier plots. Kaplan-Meier plots by subgroups within each group: (a) more than 50% and (b) less than or equal to 50% residual coronal structure.
Table 2.
Recall Rates, Failure Modes, Survival Rates, and Success Rates Recorded in Experimental Groups over a 48-month Observation Period
| Residual Coronal Dentin | Luting Agent | Baseline | 6 mo | 12 mo | 24 mo | 36 mo | 48 mo | |
|---|---|---|---|---|---|---|---|---|
| Group 1: >50% | Gradia Core | Recall rate | 30/30 (100%) | |||||
| Mode and % of failure | 0/30 (0%) |
1 PAL 1/30 (3.3%) |
2 PAL 2/30 (6.6%) |
2 PAL 1 PoFr 3/30 (10%) |
||||
| Success rate | 30/30 (100%) |
29/30 (96.6%) |
28/30 (93.3%) |
27/30 (90%) |
||||
| Survival rate | 30/30 (100%) | 30/30 (100%) |
30/30 (100%) |
30/30 (100%) |
||||
| GCem Automix | Recall rate | 30/30 (100%) | ||||||
| Mode and % of failure | 0/30 (0%) |
1 PAL 1/30 (3.3%) |
1 PAL 1 PoDe 2/30 (6.6%) |
1 PAL 2 PoDe 3/30 (10%) |
1 PAL 3 PoDe 1 RoFr 5/30 (16.6%) |
2 PAL 3 PoDe 2 RoFr 7/30 (23.3%) |
||
| Success rate | 30/30 (100%) |
29/30 (96.6%) |
28/30 (93.3%) |
27/30 (90%) |
25/30 (83.3%) |
23/30 (76.6%) |
||
| Survival rate | 30/30 (100%) |
30/30 (100%) |
30/30 (100%) |
30/30 (100%) |
29/30 (96.6%) |
28/30 (93.3%) |
||
| Group 2: ≤50% | Gradia Core | Recall rate | 30/30 (100%) | |||||
| Mode and % of failure | 0/30 (0%) |
1 PAL 2 PoDe 3/30 (10%) |
3 PAL 2 PoDe 1 PoFr 6/30 (20%) |
3 PAL 2 PoDe 1 PoFr 2 RoFr 8/30 (26.6%) |
3 PAL 2 PoDe 1 PoFr 3 RoFr 9/30 (30%) |
|||
| Success rate | 30/30 (100%) |
27/30 (90%) |
24/30 (80%) |
22/30 (73.3%) |
21/30 (70%) |
|||
| Survival rate | 30/30 (100%) |
30/30 (100%) |
30/30 (100%) |
28/30 (93.3%) |
27/30 (90%) |
|||
| GCem Automix | Recall rate | 30/30 (100%) | ||||||
| Mode and % of failure | 0/30 (0%) |
1 PAL 1/30 (3.3%) |
1 PAL 1 PoDe 2/30 (6.6%) |
1 PAL 2 PoDe 3/30 (10%) |
1 PAL 5 PoDe 2 RoFr 8/30 (26.6%) |
2 PAL 5 PoDe 4 RoFr 11/30 (36.6%) |
||
| Success rate | 30/30 (100%) |
29/30 (96.6%) |
28/30 (93.3%) |
27/30 (90%) |
22/30 (73.3%) |
19/30 (63.3%) |
||
| Survival rate | 30/30 (100%) |
30/30 (100%) |
30/30 (100%) |
30/30 (100%) |
28/30 (93.3%) |
26/30 (86.6%) |
||
Failure modes: PAL= periapical lesion; PoDe = post debonding; PoFr = post fracture; RoFr = root fracture.
Cox regression analysis revealed that neither the amount of coronal residual structure (p = .057; Hazard ratio, HR = 3.561; 95% Confidence Interval, CI, for HR = 0.964-13.156) nor the restoration material (p = .182; HR = 2.509; 95% CI for HR = 0.649-9.704) had a significant influence on the restorations’ failure risk. Interaction terms were also not significant (p = .359; HR = 0.47; 95% CI for HR = 0.093-2.359).
Discussion
The results of the present study indicated that risk of failure in endodontically treated and fiber-post-restored premolars was not influenced by the amount of residual coronal structure or luting agent during 4 yr of observation. Therefore, the null hypothesis was accepted. While the majority of previously published laboratory (Akkayan, 2004; Lima et al., 2009; da Silva et al., 2010) and clinical studies (Creugers et al., 2005; Ferrari et al., 2007b, 2012; Cagidiaco et al., 2008a) agree on the fact that more coronal structure positively affects the prognosis of endodontically treated teeth, in this study no statistically significant differences were found among the groups. As a possible explanation for such an outcome, it should be taken into consideration that even in Group 2 at least one wall with a 1.5-mm ferrule was preserved. In fact, the aforementioned clinical trials (Ferrari et al., 2007b, 2012; Cagidiaco et al., 2008a) identified similar risks of failure among groups in which teeth maintained one or more coronal walls. Conversely, teeth without any retained coronal wall exhibited a significantly higher risk of failure after 2 (Ferrari et al., 2007b), 3 (Cagidiaco et al., 2008a), and 6 yr (Ferrari et al., 2012) of clinical service, and the presence of ferrule did not seem to have a significant impact. Furthermore, it was found that a non-uniform ferrule still provided higher fracture resistance than complete absence of the ferrule effect (Tan et al., 2005; Dikbas et al., 2007). With these facts taken into account, it could be supposed that sufficient coronal structure allowing the ferrule effect was preserved in both groups in the present study, and, for that reason, no differences emerged. Moreover, considering the variability in the root anatomy, post size and length for each tooth had to be chosen so they best fit the dimensions of the canal. For similar reasons, the size of the composite core was not uniform, since it was adjusted to each tooth. Therefore, it could be speculated that these variables might have influenced the results obtained.
From a strictly statistical standpoint, it should be noticed that, despite the lack of statistical significance, the relatively high HR of residual coronal structure implied that this variable had an effect on failure. The lack of sufficient statistical power in relation to the sample size may possibly explain such an outcome. However, a priori sample size calculation was omitted, since, in previous research with similar design and objectives, a sample even smaller than that used in the present investigation had been used (Ferrari et al., 2007b, 2012; Cagidiaco et al., 2008a). A longer observation time in the current study is expected to reveal whether, with prolonged clinical function, the HR of residual coronal structure will reach statistical significance.
The most common types of failure were periapical lesions, which may be attributed to inadequate endodontic treatment, and post debonding, confirming previous findings (Cagidiaco et al., 2008b). Post fracture was noticed only in the GCore groups, while ‘absolute’ failures were observed after 3 and 4 yr and occurred more frequently in teeth with less coronal structure. It may therefore be speculated that differences in clinical performance could have been revealed if the follow-up period had been longer, due to deterioration of the adhesive interface or mechanical stress. Actually, in preceding studies investigating the survival of endodontically treated premolars (Creugers et al., 2005; Ferrari et al., 2007b, 2012; Cagidiaco et al., 2008a), higher occurrences of failures were recorded as the observation time increased. Hence, it seems of interest to collect longer term data to provide stronger evidence.
Furthermore, the current research represents the first clinical trial evaluating the amount of coronal tooth structure after the abutment preparation. All studies published in recent years (Ferrari et al., 2000a,b, 2007a,b, 2012; Mannocci et al., 2002; Malferrari et al., 2003; Monticelli et al., 2003; Creugers et al., 2005; Naumann et al., 2005; Cagidiaco et al., 2008a; Zicari et al., 2011) assessed the residual tooth structure before abutment preparation, which may have led to overestimation of the amount of dentin actually remaining at the coronal level, since preparation of finishing margin and axial walls leads to the additional loss of tooth structure and reduction of the number of residual walls. This concern has already been raised by a recent review (Juloski et al., 2012) and an in vivo study (Ferrari et al., 2012), though so far it has not been considered in clinical circumstances. Therefore, for more dependable facts on the importance of the amount of coronal dentin and ferrule effect on the performance of endodontically treated teeth, it is recommended that, in future clinical studies, the calculation of the remaining tooth structure be performed after the abutment preparation, as in the present investigation.
Regarding the materials used for post luting, in the current study 2 cements were used to verify whether the luting agent influenced the clinical behavior of the restored teeth. The outcome of the statistical analysis showed that the cement was not a significant factor. In line with this result, no difference was found in post push-out bond strength between the same 2 materials, GCore and GCem, investigated in a recent laboratory study (Juloski et al., 2013). Additionally, similar in vitro performance after thermocycling and mechanical loading was recorded in teeth where abutments were restored with a self-adhesive resin composite and 2 conventional composite core build-up materials (Naumann et al., 2010). In that investigation, fiber posts were cemented with a self-adhesive resin cement in all groups. However, in the present study, a lower percentage of success rates was noted when self-adhesive cement was used (Subgroups B) compared with the core material used in Subgroups A. As a matter of fact, when insufficient tooth structure remained, teeth restored with GCem showed the worst performance (63.3% success rate, 86.6% survival rate) during 4-year clinical service.
Moreover, another study (Naumann et al., 2011) investigated the load capability of teeth restored with fiber posts when the same self-adhesive resin cement was used as post cement and core build-up material. The results revealed inferior performance during simulated function and static loading compared with that of teeth restored with etch-and-rinse-bonded specific core composites (Naumann et al., 2011). However, the authors suggested that promising results may be expected after the mechanical properties of the cement were improved. Hence, it may be presumed that the core material investigated in this study possessed adequate strength and fracture resistance, which led to the highest success rate in Subgroup A of Group 1 (90%). Furthermore, higher bond strength values were observed in resins with higher modulus of elasticity than traditional resin cements when used for fiber post cementation (Boschian Pest et al., 2002). The opposite results were also reported (Ferrari et al., 2009), and lower bond strength and higher nanoleakage in cements with higher filler load were ascribed to the higher contraction stress recorded in those materials.
In conclusion, the results of the present study implied that, over a four-year observation period, the risk of failure of endodontically treated and fiber-post-restored teeth increased with a lower amount of residual coronal structure. However, the clinical performance was not affected by the material used for luting posts, and similar results were achieved with self-adhesive resin cement and resin core material.
Footnotes
The authors received no financial support and declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
References
- Akkayan B. (2004). An in vitro study evaluating the effect of ferrule length on fracture resistance of endodontically treated teeth restored with fiber-reinforced and zirconia dowel systems. J Prosthet Dent 92:155-162. [DOI] [PubMed] [Google Scholar]
- Boschian Pest L, Cavalli G, Bertani P, Gagliani M. (2002). Adhesive post-endodontic restorations with fiber posts: push-out tests and SEM observations. Dent Mater 18:596-602. [DOI] [PubMed] [Google Scholar]
- Cagidiaco MC, Garcia-Godoy F, Vichi A, Grandini S, Goracci C, Ferrari M. (2008a). Placement of fiber prefabricated or custom made posts affects the 3-year survival of endodontically treated premolars. Am J Dent 21:179-184. [PubMed] [Google Scholar]
- Cagidiaco MC, Goracci C, Garcia-Godoy F, Ferrari M. (2008b). Clinical studies of fiber posts: a literature review. Int J Prosthodont 21:328-336. [PubMed] [Google Scholar]
- Creugers NH, Mentink AG, Fokkinga WA, Kreulen CM. (2005). 5-year follow-up of a prospective clinical study on various types of core restorations. Int J Prosthodont 18:34-39. [PubMed] [Google Scholar]
- da Silva NR, Raposo LH, Versluis A, Fernandes-Neto AJ, Soares CJ. (2010). The effect of post, core, crown type, and ferrule presence on the biomechanical behavior of endodontically treated bovine anterior teeth. J Prosthet Dent 104:306-317. [DOI] [PubMed] [Google Scholar]
- Dikbas I, Tanalp J, Ozel E, Koksal T, Ersoy M. (2007). Evaluation of the effect of different ferrule designs on the fracture resistance of endodontically treated maxillary central incisors incorporating fiber posts, composite cores and crown restorations. J Contemp Dent Pract 8:62-69. [PubMed] [Google Scholar]
- Ferrari M, Vichi A, Mannocci F, Mason PN. (2000a). Retrospective study of the clinical performance of fiber posts. Am J Dent 13(Spec No):9B-13B. [PubMed] [Google Scholar]
- Ferrari M, Vichi A, Garcia-Godoy F. (2000b). Clinical evaluation of fiber-reinforced epoxy resin posts and cast post and cores. Am J Dent 13(Spec No):15B-18B. [PubMed] [Google Scholar]
- Ferrari M, Cagidiaco MC, Goracci C, Vichi A, Mason PN, Radovic I, et al. (2007a). Long-term retrospective study of the clinical performance of fiber posts. Am J Dent 20:287-291. [PubMed] [Google Scholar]
- Ferrari M, Cagidiaco MC, Grandini S, De Sanctis M, Goracci C. (2007b). Post placement affects survival of endodontically treated premolars. J Dent Res 86:729-734. [DOI] [PubMed] [Google Scholar]
- Ferrari M, Carvalho CA, Goracci C, Antoniolli F, Mazzoni A, Mazzotti G, et al. (2009). Influence of luting material filler content on post cementation. J Dent Res 88:951-956. [DOI] [PubMed] [Google Scholar]
- Ferrari M, Vichi A, Fadda GM, Cagidiaco MC, Tay FR, Breschi L, et al. (2012). A randomized controlled trial of endodontically treated and restored premolars. J Dent Res 91(7 Suppl):72S-78S. [DOI] [PubMed] [Google Scholar]
- Juloski J, Radovic I, Goracci C, Vulicevic ZR, Ferrari M. (2012). Ferrule effect: a literature review. J Endod 38:11-19. [DOI] [PubMed] [Google Scholar]
- Juloski J, Fadda GM, Radovic I, Chieffi N, Vulicevic ZR, Aragoneses JM, et al. (2013). Push-out bond strength of an experimental self-adhesive resin cement. Eur J Oral Sci 121:50-56. [DOI] [PubMed] [Google Scholar]
- Lima AF, Spazzin AO, Galafassi D, Correr-Sobrinho L, Carlini-Junior B. (2009). Influence of ferrule preparation with or without glass fiber post on fracture resistance of endodontically treated teeth. J Appl Oral Sci 18:360-363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malferrari S, Monaco C, Scotti R. (2003). Clinical evaluation of teeth restored with quartz fiber-reinforced epoxy resin posts. Int J Prosthodont 16:39-44. [PubMed] [Google Scholar]
- Mannocci F, Bertelli E, Sherriff M, Watson TF, Ford TR. (2002). Three-year clinical comparison of survival of endodontically treated teeth restored with either full cast coverage or with direct composite restoration. J Prosthet Dent 88:297-301. [DOI] [PubMed] [Google Scholar]
- Monticelli F, Grandini S, Goracci C, Ferrari M. (2003). Clinical behavior of translucent-fiber posts: a 2-year prospective study. Int J Prosthodont 16:593-596. [PubMed] [Google Scholar]
- Naumann M, Blankenstein F, Kiessling S, Dietrich T. (2005). Risk factors for failure of glass fiber-reinforced composite post restorations: a prospective observational clinical study. Eur J Oral Sci 113:519-524. [DOI] [PubMed] [Google Scholar]
- Naumann M, Sterzenbach G, Rosentritt M, Beuer F, Frankenberger R. (2010). In vitro performance of self-adhesive resin cements for post-and-core build-ups: influence of chewing simulation or 1-year storage in 0.5% chloramine solution. Acta Biomater 6:4389-4395. [DOI] [PubMed] [Google Scholar]
- Naumann M, Sterzenbach G, Rosentritt M, Beuer F, Meyer-Lückel H, Frankenberger R. (2011). Self-adhesive cements as core build-ups for one-stage post-endodontic restorations? Int Endod J 44:195-202. [DOI] [PubMed] [Google Scholar]
- Peroz I, Blankenstein F, Lange KP, Naumann M. (2005). Restoring endodontically treated teeth with posts and cores—a review. Quintessence Int 36:737-746. [PubMed] [Google Scholar]
- Schmitter M, Rammelsberg P, Gabbert O, Ohlmann B. (2007). Influence of clinical baseline findings on the survival of 2 post systems: a randomized clinical trial. Int J Prosthodont 20:173-178. [PubMed] [Google Scholar]
- Schwartz RS, Fransman R. (2005). Adhesive dentistry and endodontics: materials, clinical strategies and procedures for restoration of access cavities: a review. J Endod 31:151-165. [DOI] [PubMed] [Google Scholar]
- Schwartz RS, Robbins JW. (2004). Post placement and restoration of endodontically treated teeth: a literature review. J Endod 30:289-301. [DOI] [PubMed] [Google Scholar]
- Stankiewicz NR, Wilson PR. (2002). The ferrule effect: a literature review. Int Endod J 35:575-581. [DOI] [PubMed] [Google Scholar]
- Tan PL, Aquilino SA, Gratton DG, Stanford CM, Tan SC, Johnson WT, et al. (2005). In vitro fracture resistance of endodontically treated central incisors with varying ferrule heights and configurations. J Prosthet Dent 93:331-336. [DOI] [PubMed] [Google Scholar]
- Tang W, Wu Y, Smales RJ. (2010). Identifying and reducing risks for potential fractures in endodontically treated teeth. J Endod 36:609-617. [DOI] [PubMed] [Google Scholar]
- Zicari F, Van Meerbeek B, Debels E, Lesaffre E, Naert I. (2011). An up to 3-year controlled clinical trial comparing the outcome of glass fiber posts and composite cores with gold alloy-based posts and cores for the restoration of endodontically treated teeth. Int J Prosthodont 24:363-372. [PubMed] [Google Scholar]