Abstract
Minimal invasive approaches to managing caries, such as partial caries removal techniques, are showing increasing evidence of improved outcomes over the conventional complete caries removal. There is also increasing interest in techniques where no caries is removed. We present the 1-yr results of clinical efficacy for 3 caries management options for occlusoproximal cavitated lesions in primary molars: conventional restorations (CR; complete caries removal and compomer restoration), Hall technique (HT; no caries removal, sealing in with stainless steel crowns), and nonrestorative caries treatment (NRCT; no caries removal, opening up the cavity, teaching brushing and fluoride application). In sum, 169 children (3-8 yr old; mean, 5.56 ± 1.45 yr) were enrolled in this secondary care–based, 3-arm, parallel-group, randomized clinical trial. Treatments were carried out by specialist pediatric dentists or postgraduate trainees. One lesion per child received CR, HT, or NRCT. Outcome measures were clinical failure rates, grouped as minor failure (restoration loss/need for replacement, reversible pulpitis, caries progression, etc.) and major failure (irreversible pulpitis, abscess, etc.). There were 148 children (87.6%) with a minimum follow-up of 11 mo (mean, 12.23 ± 0.98 mo). Twenty teeth were recorded as having at least 1 minor failure: NRCT, n = 8 (5%); CR, n = 11 (7%); HT, n = 1 (1%) (p = .002, 95% CI = 0.001 to 0.003). Only the comparison between NRCT and CR showed no significant difference (p = .79, 95% CI = 0.78 to 0.80). Nine (6%) experienced at least 1 major failure: NRCT, n = 4 (2%); CR, n = 5 (3%); HT, n = 0 (0%) (p = .002, 95% CI = 0.001 to 0.003). Individual comparison of NRCT and CR showed no statistically significant difference in major failures (p = .75, 95% CI = 0.73 to 0.76). Success and failure rates were not significantly affected by pediatric dentists’ level of experience (p = .13, 95% CI = 0.12 to 0.14). The HT was significantly more successful clinically than NRCT and CR after 1 yr, while pairwise analyses showed comparable results for treatment success between NRCT and CR (ClinicalTrials.gov NCT01797458).
Keywords: caries treatment, clinical studies/trials, clinical outcomes, pediatric dentistry, primary teeth, The Hall Technique
Introduction
There has been a paradigm shift in what is considered effective management of carious primary teeth. Conventional restorative or surgical approaches to caries—where carious dentine is totally excised, then a restoration placed (Ricketts and Pitts, 2009; Kandiah et al., 2010)—is being challenged by more biological, less invasive approaches where emphasis is on biofilm alteration to arrest carious lesions (Ricketts et al., 2013; Schwendicke et al., 2013).
These novel biological approaches form a spectrum of techniques. They extend from stepwise caries removal to nonrestorative caries treatment (NRCT), where no caries is removed but the cavity is opened to allow the lesion to be brushed by parent and child; the biofilm is altered through continual disruption/cleaning (Gruythuysen et al., 2011; Kidd, 2012). Additionally, sealing techniques include those with no caries removal, such as the Hall technique (HT; Innes et al., 2006, 2011), partial (Lula et al., 2009) stepwise caries removal (Ricketts et al., 2013), and fissure sealing lesions (Griffin et al., 2008). Although the evidence base supporting biological treatment approaches is growing, the limited comparative evidence for one approach over another leaves clinicians with uncertainty around their efficacy and, therefore, difficulties when planning treatment for children.
In primary teeth, the approximal surfaces experience caries most commonly (Martignon et al., 2010), with around 80% of restorations occlusoproximal (Qvist et al., 2004a). The most effective approach for caries treatment in primary teeth, especially for multisurface lesions, remains the subject of ongoing (Ricketts et al., 2013) and at times vigorous debate (Kidd, 2012).
This study was undertaken to evaluate clinical efficacy of 3 caries management options for occlusoproximal cavitated lesions in primary molars, in a longitudinal randomized clinical trial setting. The treatments were as follows:
Control arm—with complete caries removal and conventional restorations (CR);
Sealing in caries with stainless-steel crowns using the HT; and
NRCT—with cavity opening and fluoride application.
The null hypothesis was no difference at 1 yr among any of the 3 arms for the primary outcome of success or minor failure and for the secondary outcomes of major failure and plaque and gingival scores. The patient-relevant outcomes at time of treatment—children’s behavior and pain perception, acceptability of the techniques to parents and dentists—have been reported (Santamaria et al., 2014). This report is part of a longitudinal clinical trial that aims to evaluate long-term outcomes of HT, NRCT, and CR.
Material & Methods
Ethics
The Research Ethics Committee of Greifswald University, Germany, gave study approval (BB 39/11; trial registration no. NCT01797458). Parents gave written consent for children to participate.
Study Design
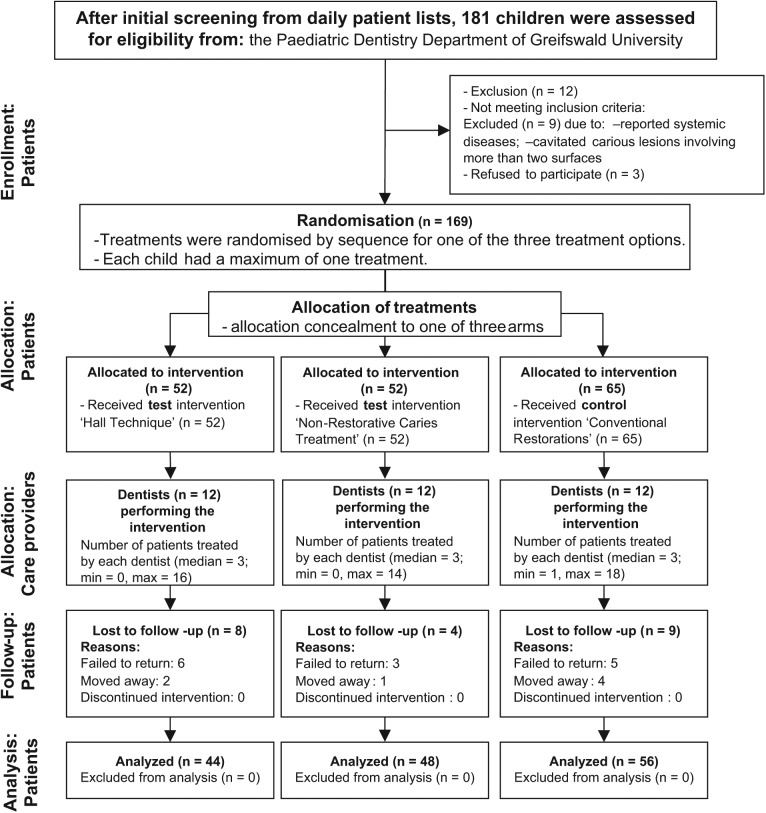
This secondary care–based, 3-arm, parallel-group, patient-randomized controlled trial was conducted in the pediatric dentistry department of Greifswald University. Between 2011 and 2012, 12 dentists were trained to deliver each treatment: 7 pediatric specialists and 5 postgraduate pediatric students (mean age, 35.1 ± 10.3 yr). Treating dentists recruited 169 children (3-8 yr old; mean age = 5.56 ± 1.45 yr) with a primary molar tooth with occlusoproximal caries into dentine (International Caries Detection and Assessment System [ICDAS] codes 3-5). At screening, 2 calibrated dentists (kappa > 0.81) assessed all eligible lesions. Children were randomized through a computer-generated random-number list with allocation concealment to 1 of 3 arms: NRCT, HT, or CR. Children were excluded if they had signs or symptoms of pulpal or periradicular pathology (including pain) or systemic conditions requiring special dental considerations. Only 1 tooth per child was included in the study. Where more than 1 tooth per child fulfilled the inclusion criteria, the next tooth on the prescribed treatment plan (determined by the treating dentist) was chosen for the study. Patient recruitment and follow-up are presented in the CONSORT diagram (Schulz et al., 2010; Figure). Further study methodology details have been reported (Santamaria et al., 2014). Details of outcome criteria are presented in Table 1.
Figure.
Study CONSORT diagram.
Table 1.
Outcome Criteria for Procedures: Clinical Assessment in the 3 Treatment Arms
| Nonrestorative Caries Treatment | Hall Technique | Conventional Restoration |
|---|---|---|
| Primary Outcome: Successful | ||
| Caries arrested (hardness/softness; lesion feels hard on gently probing the dentin), No clinical signs or symptoms of pulpal pathology, or Tooth exfoliated without minor or major failure. |
Crown appears satisfactory, No clinical signs or symptoms of pulpal pathology, or Tooth exfoliated without minor or major failure. |
Restoration appears satisfactory (intact tooth surface adjacent to restoration, stained margins consistent with noncarious lesions),No clinical signs or symptoms of pulpal pathology, or Tooth exfoliated without minor or major failure. |
| Primary Outcome: Minor Failure | ||
| Caries progression (hardness/softness; lesion feels soft or leathery on gently probing the dentin) Signs or symptoms of reversible pulpitis treated without requiring pulpotomy or extraction. |
New caries (around margins) Crown perforation Restoration loss but the tooth is restorable Signs or symptoms of reversible pulpitis (no spontaneous pain) treated without requiring pulpotomy or extraction. |
Secondary caries (visible dentin in the interfacial space with signs of caries requiring intervention) Restoration fracture or wear requiring intervention Restoration loss Signs or symptoms of reversible pulpitis treated without requiring pulpotomy or extraction. |
| Secondary Outcome: Major Failure | ||
| Irreversible pulpitis (history of spontaneous pain or precipitated pain caused by thermal or other stimuli) or dental abscess requiring pulpotomy or extraction. | Irreversible pulpitis (history of spontaneous pain or precipitated pain caused by thermal or other stimuli) or dental abscess requiring pulpotomy or extraction Crown loss and tooth is unrestorable. |
Signs or symptoms of reversible pulpitis (no spontaneous pain) requiring pulpotomy Signs or symptoms of irreversible pulpitis (history of spontaneous pain or precipitated pain caused by thermal or other stimuli) or dental abscess Restoration loss and tooth is unrestorable. |
| Secondary Outcome: Plaque Indexa | ||
| 0 = no plaque 1 = thin visible plaque, difficult to identify 2 = thick visible plaque, easily detected | ||
| Secondary Outcome: Gingival Indexb | ||
| 0 = no swelling 1 = mild swelling, no bleeding after gentle probing 2 = moderate to severe gingival swelling, bleeding after air drying | ||
Modified Plaque Index (Löe et al., 1972).
Sample
Sample size calculation was based on the comparison of minor failure rates for HT (5%) vs. CR (46%) (Innes et al., 2007a). Failure rates of 5% for HT and 25% for CR were assumed. For NRCT, there were no reliable failure rate data. From a clinical point of view, it was considered a positive outcome if results were similar to those of HT, proving clinical equivalence. The program G*power 3 was used for sample size calculation (Faul et al., 2007): 2-tail test, α = 0.05 divided by “three” for multiple testing, resulting in 0.016; β = 0.20. This gave a sample size target of 116 children with 30% overestimation to allow for follow-up losses.
Baseline Oral Health Status and Caries Lesions
A full oral examination, dental chart (DMFT/dmft, ICDAS), Gingival Index, and Plaque Index were carried out (Table 1). Plaque Index and Gingival Index measurements were scored on 7 index teeth.
Treatment Procedures
Conventional Restorations
Local anaesthesia was placed when needed. Complete caries removal was carried out with a high-speed handpiece, then a slow handpiece and/or an excavator to clear carious dentine from the pulpal wall. A matrix band and a porta-matrix (Henry Schein Inc., Melville, NY, USA) or a T-Band (Pulpdent, Watertown, MA, USA) and a wedge (Interdental Wedge, Kerr, Biogglo, Switzerland) were used. All cavities were restored with Compomer (Dyract, Dentsply, Konstanz, Germany) under cotton wool roll isolation and continuous aspiration.
Hall Technique
No caries removal or tooth preparation was carried out, and no local anaesthesia was placed. The correct size of crown was chosen then cemented with glass ionomer luting cement (GC Fuji TRIAGE, GC Corporation, Tokyo, Japan). Cotton wool rolls isolation and aspiration were used as required. Further details can be found at http://dentistry.dundee.ac.uk/cariology.
Nonrestorative Caries Treatment
Lesions were opened with a high-speed bur to remove overhanging enamel, making the cavity accessible for plaque removal. No carious dentine was removed from the pulpal wall and no local anaesthesia placed. Fluoride varnish (Duraphat, GABA, Lörrach, Germany) was applied to the cavity. Parents/children were taught toothbrushing using a buccolingual technique for the treated tooth.
All participants were given dietary advice and detailed age-specific toothbrushing instructions following German guidelines (http://www.dgzmk.de). Children from 6 yr of age brushed their teeth twice a day with 1,000- to 1,500-ppm F− toothpaste. Younger children brushed with 500-ppm F− toothpaste.
Participants’ Follow-up
HT and CR participants maintained their dentists’ normal review intervals (twice per year), and those in the NRCT arm had 3 monthly recalls where plaque disclosing and toothbrushing instructions to parents/children for the whole mouth and site specific for the treatment tooth were performed and the information recorded. The study tooth was cleaned and Duraphat applied to active lesions.
After 1 yr, 2 trained examiners (R.M.S., C.H.S.)—experienced pediatric dentists and trained in use of ICDAS—reassessed the teeth. Dentists did not assess their own patients. The oral examination was repeated. Parents/children were asked about pain experience, eating difficulties, and any emergency treatment that was required during the previous year. For further information on study design, see Appendix.
Data Analysis
All analyses were performed with SPSS 17.0 for Windows. Nonparametric Kruskal-Wallis analysis of variance and Bonferroni-corrected Mann-Whitney U test were used for comparisons of clinical outcomes (successful, minor failure, major failure), Gingival Index, Plaque Index, and distribution of ICDAS categories among treatment arms. McNemar’s test was used to compare the Plaque Index scores (baseline vs. 1 yr) for each arm. Age and d3mft comparisons were performed using analysis of variance. The absolute risk reduction (ARR) and numbers needed to treat (NNT) were also calculated. The significance level was set at 5%.
Results
Baseline Characteristics (Participants and Teeth)
Of 169 baseline carious lesions, 138 (82%) were ICDAS code 5 (distinct cavity with visible dentin); 25 (15%), ICDAS 4 (underline dentin shadow), and 6 (3%), ICDAS 3 (localized enamel breakdown)—with no significant differences in distribution among treatment groups (p = .35, 95% confidence interval [CI] = 0.35 to 0.70). The overall baseline d3mft value was 5.59 ± 3.08 with no differences among groups for d3mft (p = .25, 95% CI = 0.25 to 0.27), median plaque scores (p = .29, 95% CI = 0.27 to 0.30), or gingival status (p = .13, 95% CI = 0.13 to 0.14). Sixty-nine percent (n = 116) of the teeth were first primary molars. Additional baseline data are reported in Santamaria et al. (2014).
Treatment Characteristics
For treatment distribution by tooth type and arch, see Table 2. In the CR group, local anaesthesia was administered to 34 participants (52%). In the HT group, orthodontic separators were used in 28 cases (54%), evenly distributed across dentists, with no difference in use between specialists and postgraduate students (p = .41, 95% CI = 0.40 to 0.42). Crown size ranged from size 3 to 7 (mode size, 5; n = 34, 67%).
Table 2.
Distribution of Teeth in the Study and ICDAS Categories According to the Type of Treatment, n (%)
| Hall Technique | Nonrestorative Caries Treatment | Conventional Restoration | Total | |
|---|---|---|---|---|
| Primary molar of treatment | ||||
| Maxillary first | 17 (33) | 22 (42) | 23 (35) | 62 (37) |
| Maxillary second | 7 (13.5) | 8 (15) | 14 (22) | 29 (17) |
| Mandibular first | 21 (40) | 16 (31) | 17 (26) | 54 (32) |
| Mandibular second | 7 (13.5) | 6 (12) | 11 (17) | 24 (14) |
| Total | 52 | 52 | 65 | 169 (100) |
| ICDAS | ||||
| 3 | 3 (6) | 1 (2) | 2 (3) | 6 (3) |
| 4 | 11 (21) | 7 (13) | 7 (11) | 25 (15) |
| 5 | 38 (73) | 44 (85) | 56 (86) | 138 (82) |
| Total | 52 | 52 | 65 | 169 (100) |
ICDAS, International Caries Detection and Assessment System: 3, localized enamel breakdown; 4, underlying dentin shadow; 5, distinct cavity with visible dentin.
Follow-up: Participants and Teeth
After a minimum of 11 mo, 148 of 169 (87.6%) participants returned for follow-up (CR: n = 56 of 65, 86%; HT: n = 44 of 52, 85%; NRCT: n = 48 of 52, 92%) with no statistical difference among arm allocation (p = .47). Follow-up ranged from 11 to 15 mo (mean, 12.23 ± 0.98). Twenty-one participants did not return for follow-up. Of the 148 returning children, 86 (58%) were boys, with no significant differences among the groups for boys’ ages (mean, 6.67 ± 1.49 yr) or girls’ ages (mean, 6.50 ± 1.48 yr; p > .05). The d3mft was 6.04 ± 2.97, without significant differences among groups (p = .34). Characteristics of nonreturning and followed-up participants were similar.
Minor Failures
There were 20 of 148 minor failures: CR = 7%, NRCT = 5%, HT = 1% (p = .002, 95% CI = 0.001 to 0.003; Table 3). By comparing independently among treatment arms, there were no significant differences between NRCT and CR (p = .79, 95% CI = 0.78 to 0.80). However, there were differences between NRCT and HT (p = .030, 95% CI = 0.026 to 0.033) with an ARR of 0.16 (95% CI = 0.04 to 0.28) and NNT of 7 and between CR and HT (p = .011, 95% CI = 0.009 to 0.013) with an ARR of 0.19 (95% CI = 0.07 to 0.31) and NNT of 6—in both cases in favor of the HT.
Table 3.
Treatment Success Rates after 1-yr Follow-up by Allocated Treatment Group, n (%)
| Type of Treatment |
||||
|---|---|---|---|---|
| Success rate | Hall Technique | Nonrestorative Caries Treatment | Conventional Restoration | Total |
| Successful | 43 (98) | 36 (75 ) | 40 (71) | 119 (80) |
| Minor failure | 1 (2) | 8 (17) | 11 (20) | 20 (14) |
| Major failure | 0 (0) | 4 (8) | 5 (9) | 9 (6) |
| Total | 44 | 48 | 56 | 148 |
Kruskal Wallis test for comparison among the 3 treatment groups (p = .002; confidence interval = 0.001 to 0.003). Bonferroni-corrected Mann-Whitney U test for independent comparisons among nonrestorative caries treatment and conventional restorations (p = .74; confidence interval = 0.73 to 0.75).
In the NRCT group, failure times ranged from 3 to 12 mo (mean, 9.8 ± 2.9). Reasons for failure were caries progression (n = 6) and reversible pulpitis (without requiring pulpotomy; n = 2). In the CR group, failure times ranged from 11 to 13 mo (mean, 11.8 ± 0.7). Reasons for failure were secondary caries (n = 8), restoration fracture (n = 1), and loss (n = 2). In the HT group, new caries around crown margins was detected (12 mo) in 1 case. The majority of minor failures (n = 18 of 20, 90%) were ICDAS 5 teeth and first primary molars (n = 14 of 20, 70%).
Major Failures
From the 148 teeth/participants reviewed, 9 (6%) presented with major failures (NRCT = 4, CR = 5), with no major failures in the HT arm (p = .002, 95% CI = 0.001 to 0.003; Table 3). There were no significant differences when NRCT and CR were compared (p = .75, 95% CI = 0.73 to 0.76). However, differences were observed between NRCT and HT (p = .002, 95% CI = 0.001 to 0.003) with an ARR of 0.1 (95% CI = 0.007 to 0.19) and NNT of 10 and between CR and HT (p = .001, 95% CI = 0.000 to 0.002) with an ARR of 0.11 (95% CI = 0.01 to 0.02) and NNT of 9.
In the 4 NRCT group failures, times to failure were 8 and 10 mo and in 2 cases over 11 mo. Reasons for failures were abscess (n = 3) and irreversible pulpitis (n = 1). In the CR group, failures were recorded at 5, 6, 11, 11, and 12 mo. Reasons for failures were dental abscess (n = 3) and reversible pulpitis (requiring pulpotomy; n = 2). In total, 6 teeth were extracted: NRCT = 3 (2%) and CR = 3 (2%). The rest of the teeth (n = 3, 2%) presenting with major failures were endodontically treated and restored. All major failures were in first primary molars (n = 9), the majority in ICDAS 5 teeth (n = 7 of 9, 78%).
Treatments success/failure were not significantly affected by the dentists’ level of experience (p = .13, 95% CI = 0.12 to 0.14).
Gingival Index and Plaque Index
Overall, the amount of plaque-free children increased after 1 yr (Table 4). There were significant differences by comparing in each arm the Plaque Index status (baseline vs. 1 yr): HT (p = .027), NRCT (p = .003), CR (p < .000). The Gingival Index did not show significant variation in any of the arms during the study period. The majority of patients (n = 24 of 29, 83%) who presented with failures had a Plaque Index > 0 at the time of examination compared to successful cases (n = 28 of 119, 24%; p < .000).
Table 4.
Plaque and Gingival Index Scores at Baseline and after 1 Yr per Treatment Group, n (%)
| 0 |
1 |
2 |
||||
|---|---|---|---|---|---|---|
| Treatment Techniques | Plaque | Gingival | Plaque | Gingival | Plaque | Gingival |
| Conventional restorations | ||||||
| Baseline | 18 (28) | 57 (88) | 43 (66) | 8 (12) | 4 (6) | 0 (0) |
| 1 yr | 33 (59) | 52 (93) | 20 (36) | 4 (7) | 3 (5) | 0 (0) |
| Hall technique | ||||||
| Baseline | 21 (40) | 47 (90) | 27 (52) | 4 (8) | 4 (8) | 1 (2) |
| 1 yr | 28 (64) | 37 (84) | 15 (34) | 7 (16) | 1 (2) | 0 (0) |
| Nonrestorative caries treatment | ||||||
| Baseline | 22 (42) | 40 (77) | 27 (52) | 12 (23) | 3 (6) | 0 (0) |
| 1 yr | 35 (73) | 41 (85) | 11 (23) | 6 (13) | 2 (4) | 1 (2) |
Baseline, n = 169 children; 1 yr, n = 148 children. Plaque Index: 0 = no plaque, 1 = thin visible plaque, 2 = thick visible plaque. Gingival Index: 0 = no swelling, 1 = mild swelling, 2 = moderate to severe gingival swelling.
Discussion
In this 1-yr follow-up comparing the clinical efficacy of CR, HT, and NRCT, the HT outperformed NRCT and CR. The null hypothesis of no difference among any of the 3 arms for the primary outcome of minor failure was rejected. However, NRCT and CR treatment success rates were comparable.
The HT had only 1 minor failure (3%) and no major failures, compared to NRCT (minor = 17%, major = 8%) and CR (minor = 20%, major = 9%). These results were comparable to the 2-yr results of the first trial of CR (minor = 46%, major = 15%) vs. HT (minor = 5%, major = 2%; Innes et al., 2007a). For minor failures, the comparison between NRCT and HT showed an NNT of 7, and for the comparison between CR and HT, the NNT was 6—in both cases in favor of the HT. For major failures, there were no significant differences between NRCT and CR. However, the comparison between NRCT and HT showed an NNT of 10—and between CR and HT, an NNT of 9—in favor of the HT.
Although not high quality (Innes et al., 2007b), there is consistent evidence of conventional stainless steel crowns outperforming other restorations for multisurface carious primary teeth—with failure rates of 11.6% for stainless steel crowns and 88.7% for amalgam (Randall et al., 2000), as well as 8%, 21%, and 30% for stainless steel crowns, amalgam, and composite, respectively (Tate et al., 2002). Despite recommendations for conventional stainless steel crowns (Attari and Roberts, 2006; Kindelan et al., 2008), their use is mainly limited to paediatric specialists, with general dentists considering stainless steel crowns too complex, time-consuming, expensive, and not cosmetically acceptable (Threlfall et al., 2005). The HT, however, makes relatively few demands on the child or the dentist, even compared with the technique-sensitive CR. The use of the HT could be advantageous for practitioners in terms of technique complexity and time saving. The higher success rate for the HT may be attributable to crown durability giving complete isolation of the plaque biofilm from the oral environment, slowing or arresting the lesion progression. Also, glass ionomer cement with the HT may have offered additional benefit in lesion remineralization (Salas et al., 2011). While a stainless steel crown with full coronal coverage effectively isolates the tooth from dietary challenges and brushing habits of the child and parent, the use of NRCT relies for its success on the same people responsible for the original lesion.
We found no significant differences in efficacy between NRCT and CR (p > .05). There is very limited NRCT research. An observational study on mesial slicing in approximal carious lesions and fluoride application, which included parental advice on diet and oral hygiene, found 90% of lesions arrested after 1 yr and only 10% requiring restorations (Peretz and Gluck, 2006). Negative outcomes were associated with insufficient oral hygiene. Similarly, in our study, the oral health status in children with NRCT failures was significantly lower than successful cases. Additionally, more than 70% of NRCT-allocated children with treatment failures failed to attend the regular 3-mo follow-ups. A recent trial comparing 3.5-yr survival rates of primary molars treated with CR (n = 341), atraumatic restorative treatment (n = 244), or ultraconservative caries treatment (n = 281: ART = 109, NRCT = 166, atraumatic restorative treatment–NRCT combination = 6; Mijan et al., 2013) showed no significant differences in the survival rates (p = .13), with ultraconservative caries treatment major failures (fistula, abscess, etc.) proportionally lower than in our study (9.25%). However, the ultraconservative caries treatment group also received supervised daily toothbrushing, positively influencing the clinical outcomes and unrealistic in most settings.
NRCT should not be confused with “no caries treatment.” The controversy continues unresolved between studies where untreated carious primary teeth exfoliate physiologically and asymptomatically (Levine et al., 2002; Tickle et al., 2002; Hu et al., 2013) and those where this is associated with higher risk of new caries lesions, space loss, pain, and so on (for a review of these, see Finucane, 2012). However, NRCT must be part of a comprehensive caries control program (training in plaque control, diet instructions, fluoride application, etc.), including recall visits allowing lesion activity to be monitored. Treatment success depends on parental cooperation, as parents are responsible for toothbrushing the affected lesion surfaces with fluoride toothpaste (Kidd, 2012). Monitoring allows nonsuccessful cases to be picked up and, if necessary, another treatment approach to be carried out.
There was a high failure rate for the control restorations (19%). Although occlusoproximal restorations usually have higher failure rates than single-surface restorations (dos Santos et al., 2009), choice of material can influence restoration longevity (Qvist et al., 2004b). Compomers have shown adequate survival rates in occlusoproximal cavities comparable with amalgam (Marks et al., 2010; Qvist et al., 2010). Four practice-based longitudinal studies (Qvist et al., 2010) comparing various filling materials reported an annual failure rate of approximately 10% for class II cavities restored with compomer. However, the study population had low caries activity and relatively low restorative need. In this study, the most frequent reason for failure was restoration associated secondary caries. Radiographs were not an inclusion requirement, and in Germany, bitewings are not routinely taken where pulpal involvement is considered unlikely. Therefore, one-third of participants had no baseline radiographs. This is unlikely to have contributed to inaccurate baseline diagnosis of pulpal status as randomization ensured an equal chance of distribution across arms; HT teeth suffered no irreversible pulpal involvement. Another hypothesis that we generated to explain failure rates in the CR group was the non-uniform use of local anesthesia (administrated to 52% participants); however, local anaesthesia use did not explain the CR failure rates, as its use did not influence restoration failure rate either (p = .73, 95% CI = 0.72 to 0.75). Furthermore, although a rubber dam was not used during the filling procedure, Carvalho et al. (2010) and Brunthaler et al. (2003) found that its use did not influence failure in primary teeth and permanent teeth, respectively.
The management of multisurface carious primary molars in children is challenging. In contrast to treatment in adults, pediatric dentistry has to consider factors such as age, cognitive development, pain perception, type of treatment, and so on. These play important roles in selection and provision of dental treatment (Goumans et al., 2004; van Bochove and van Amerongen, 2006). An early report from our study (Santamaria et al., 2014) compared children’s behavior and pain perception at treatment and techniques’ acceptability to parents and dentists. Children treated with NRCT and the HT presented less negative behavior compared to those treated with CR. However, when children themselves were asked about comfort of the procedure, they rated all 3 treatments similarly.
The HT and NRCT are still regarded as unreliable caries treatment approaches for many dentists. However, the results of this study found the HT to give encouraging results in sealing carious lesions without caries removal. The risk difference between CR and HT resulted in 19% fewer cases of minor failures and an NNT of 6 for the HT—meaning that 6 children had to be treated with the HT rather than a CR to avoid 1 minor failure—and 11% fewer major failures with an NNT of 9. Similarly, also favoring the HT, the risk difference between NRCT and HT was a decrease in minor (16%) and major failures (10%). Furthermore, 75% of lesions in the NRCT arm did not give signs/symptoms of pulp damage during the study period: results comparable to the CR arm.
Interpreting these findings for generalizability to their own practice, clinicians should particularly consider the following: (1) participants were treated by specialists or trainee specialists; (2) all had high caries risk, which may have adversely affected the clinical outcomes for CR and NRCT; and (3) children’s treatment should be tailored to their individual circumstances. Although participants/parents received toothbrushing instructions and dietary guidance, individual procedures relied on parental compliance with advice to different extents. The HT took lesion control out of parents’ hands by sealing the lesion, whereas NRCT relied on child/parental fulfilment of brushing and diet advice for caries control.
Although the HT considerably reduces the complexity of placing preformed metal crowns, their poor aesthetics can still be a barrier for more aesthetic-oriented patients, parents, and dentists.
Overall, these results support the concept of caries control by managing the activity of the biofilm. Children require individual treatment plans, and keeping in mind that there is not one single treatment choice for caries control, clinicians should consider the HT and NRCT as treatment options with positive results for children’s pain perception and parents’ acceptability of techniques (Santamaria et al., 2014). Relative clinical outcomes show the HT to be significantly more successful than NRCT and CR after 1 yr, while NRCT and CR treatment success rates were comparable.
Supplementary Material
Acknowledgments
We thank the children, their parents, and dentists who took part in this study. Preliminary data from this study were presented at the 2014 EAPD and ORCA meetings.
Footnotes
A supplemental appendix to this article is published electronically only at http://jdr.sagepub.com/supplemental.
This study has been supported by the Paediatric Dentistry Department of Greifswald University, Germany.
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
References
- Attari N, Roberts JF. (2006). Restoration of primary teeth with crowns: a systematic review of the literature. Eur Arch Paediatr Dent 7:58-63. [DOI] [PubMed] [Google Scholar]
- Brunthaler A, König F, Lucas T, Sperr W, Schedle A. (2003). Longevity of direct resin composite restorations in posterior teeth. Clin Oral Investig 7:63-70. [DOI] [PubMed] [Google Scholar]
- Carvalho TS, Sampaio FC, Diniz A, Bönecker M, Van Amerongen WE. (2010). Two years survival rate of class II ART restorations in primary molars using two ways to avoid saliva contamination. Int J Paediatr Dent 20:419-425. [DOI] [PubMed] [Google Scholar]
- dos Santos MP, Passos M, Luiz RR, Maia LC. (2009). A randomized trial of resin-based restorations in class I and class II beveled preparations in primary molars: 24-month results. J Am Dent Assoc 140:156-166. [DOI] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang AG, Buchner A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39:175-191. [DOI] [PubMed] [Google Scholar]
- Finucane D. (2012). Rationale for restoration of carious primary teeth: a review. Eur Arch Paediatr Dent 13:281-292. [DOI] [PubMed] [Google Scholar]
- Goumans C, Veerkamp JS, Aartman IH. (2004). Dental anxiety and behavioural problems: what is their influence on the treatment plan? Eur J Paediatr Dent 5:15-18. [PubMed] [Google Scholar]
- Griffin SO, Oong E, Kohn W, Vidakovic B, Gooch BF; CDC Dental Sealant Systematic Review Work Group: Bader J, Clarkson J, Fontana MR, Meyer DM, Rozier RG, Weintraub JA, et al. (2008). The effectiveness of sealants in managing caries lesions. J Dent Res 87:169-174. [DOI] [PubMed] [Google Scholar]
- Gruythuysen RJ, van Strijp AJ, van Palestein Helderman WH, Frankenmolen FW. (2011). Non-restorative treatment of cavities in temporary dentition: effective and child-friendly. Ned Tijdschr Geneeskd 155:A3489. [PubMed] [Google Scholar]
- Hu X, Chen X, Fan M, Mulder J, Frencken JE. (2013). What happens to cavitated primary teeth over time? A 3.5-year prospective cohort study in China. Int Dent J 63:183-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Innes NP, Stirrups DR, Evans DJ, Hall N, Leggate M. (2006). A novel technique using preformed metal crowns for managing carious primary molars in general practice: a retrospective analysis. Br Dent J 22:451-454. [DOI] [PubMed] [Google Scholar]
- Innes NP, Evans DJ, Stirrups DR. (2007a). The Hall technique: a randomized controlled clinical trial of a novel method of managing carious primary molars in general dental practice. Acceptability of the technique and outcomes at 23 months. BMC Oral Health 7:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Innes NP, Ricketts DN, Evans DJ. (2007b). Preformed metal crowns for decayed primary molar teeth. Cochrane Database Syst Rev 1:CD005512. [DOI] [PubMed] [Google Scholar]
- Innes NP, Evans DJ, Stirrups DR. (2011). Sealing caries in primary molars: randomized control trial, 5-year results. J Dent Res 90:1405-1410. [DOI] [PubMed] [Google Scholar]
- Kandiah T, Johnson J, Fayle SA. (2010). British Society of Paediatric Dentistry: a policy document on management of caries in the primary dentition. Int J Paediatr Dent 20(Suppl 1):5. [DOI] [PubMed] [Google Scholar]
- Kidd E. (2012). Should deciduous teeth be restored? Reflections of a cariologist. Dent Update 39:159-162, 165-166. [DOI] [PubMed] [Google Scholar]
- Kindelan SA, Day P, Nichol R, Willmott N, Fayle SA. (2008). British Society of Paediatric Dentistry: UK national clinical guidelines in paediatric dentistry. Stainless steel preformed crowns for primary molars. Int J Paediatr Dent 18(Suppl 1):20-28. [DOI] [PubMed] [Google Scholar]
- Levine RS, Pitts NB, Nugent ZJ. (2002). The fate of 1,587 unrestored carious deciduous teeth: a retrospective general dental practice based study from northern England. Br Dent J 193:99-103. [DOI] [PubMed] [Google Scholar]
- Löe H. (1967). The Gingival Index, the Plaque Index and the Retention Index systems. J Periodontol 38(Suppl):610-616. [DOI] [PubMed] [Google Scholar]
- Löe H, von der Fehr FR, Schiött CR. (1972). Inhibition of experimental caries by plaque prevention: the effect of clorhexidine mouthrinses. Scand J Dent Res 80:1-9. [DOI] [PubMed] [Google Scholar]
- Lula EC, Monteiro-Neto V, Alves CM, Ribeiro CC. (2009). Microbiological analysis after complete or partial removal of carious dentin in primary teeth: a randomized clinical trial. Caries Res 43:354-358. [DOI] [PubMed] [Google Scholar]
- Marks LA, Faict N, Welbury RR. (2010). Literature review: restorations of class II cavities in the primary dentition with compomers. Eur Arch Paediatr Dent 11:109-114. [DOI] [PubMed] [Google Scholar]
- Martignon S, Tellez M, Santamaría RM, Gomez J, Ekstrand KR. (2010). Sealing distal proximal caries lesions in first primary molars: efficacy after 2.5 years. Caries Res 44:562-570. [DOI] [PubMed] [Google Scholar]
- Mijan M, de Amorim RG, Leal SC, Mulder J, Oliveira L, Creugers NH, et al. (2014). The 3.5-year survival rates of primary molars treated according to three treatment protocols: a controlled clinical trial. Clin Oral Investig 18:1061-1069. [DOI] [PubMed] [Google Scholar]
- Peretz B, Gluck G. (2006). Early childhood caries (ECC): a preventive-conservative treatment mode during a 12-month period. J Clin Pediatr Dent 30:191-194. [DOI] [PubMed] [Google Scholar]
- Qvist V, Manscher E, Teglers PT. (2004a). Resin-modified and conventional glass ionomer restorations in primary teeth: 8-year results. J Dent 32:285-294. [DOI] [PubMed] [Google Scholar]
- Qvist V, Laurberg L, Poulsen A, Teglers PT. (2004b). Class II restorations in primary teeth: 7-year study on three resin-modified glass ionomer cements and a compomer. Eur J Oral Sci 112:188-196. [DOI] [PubMed] [Google Scholar]
- Qvist V, Poulsen A, Teglers PT, Mjör IA. (2010). The longevity of different restorations in primary teeth. Int J Paediatr Dent 20:1-7. [DOI] [PubMed] [Google Scholar]
- Randall RC, Vrijhoef MM, Wilson NH. (2000). Efficacy of preformed metal crowns vs. amalgam restorations in primary molars: a systematic review. J Am Dent Assoc 131:337-343. [DOI] [PubMed] [Google Scholar]
- Ricketts D, Lamont T, Innes NP, Kidd E, Clarkson JE. (2013). Operative caries management in adults and children. Cochrane Database Syst Rev 3:CD003808. [DOI] [PubMed] [Google Scholar]
- Ricketts DN, Pitts NB. (2009). Traditional operative treatment options. Monogr Oral Sci 21:164-173. [DOI] [PubMed] [Google Scholar]
- Salas CF, Guglielmi CA, Raggio DP, Mendes FM. (2011). Mineral loss on adjacent enamel glass ionomer cements restorations after cariogenic and erosive challenges. Arch Oral Biol 56:1014-1019. [DOI] [PubMed] [Google Scholar]
- Santamaria RM, Innes NP, Machiulskiene V, Evans DJ, Alkilzy M, Splieth CH. (2014). Acceptability of different caries management methods for primary molars in a RCT. Int J Paediatr Dent [E-pub ahead of print March 7, 2014] in press. [DOI] [PubMed] [Google Scholar]
- Schulz KF, Altman DG, Moher D; CONSORT Group (2010). CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol 63:834-840. [DOI] [PubMed] [Google Scholar]
- Schwendicke F, Meyer-Lueckel H, Dörfer C, Paris S. (2013). Failure of incompletely excavated teeth: a systematic review. J Dent 41:569-580. [DOI] [PubMed] [Google Scholar]
- Tate AR, Ng MW, Needleman HL, Acs G. (2002). Failure rates of restorative procedures following dental rehabilitation under general anesthesia. Pediatr Dent 24:69-71. [PubMed] [Google Scholar]
- Threlfall AG, Pilkington L, Milsom KM, Blinkhorn AS, Tickle M. (2005). General dental practitioners’ views on the use of stainless steel crowns to restore primary molars. Br Dent J 199:453-455. [DOI] [PubMed] [Google Scholar]
- Tickle M, Milsom K, King D, Kearney-Mitchell P, Blinkhorn A. (2002). The fate of the carious primary teeth of children who regularly attend the general dental service. Br Dent J 192:219-223. [DOI] [PubMed] [Google Scholar]
- van Bochove JA, van Amerongen WE. (2006). The influence of restorative treatment approaches and the use of local analgesia, on the children’s discomfort. Eur Arch Paediatr Dent 7:11-16. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.