Abstract
BACKGROUND
Dyspepsia is a common symptom with an extensive differential diagnosis and a heterogeneous pathophysiology. Many studies have reported that dyspeptic symptoms are associated with ingestion of some foods. Current treatments for functional dyspepsia have generally ignored the potential role of diet.
METHODS
This cross-sectional study was done at the Gastroenterology Department of Shahid Sadoughi Hospital, Yazd, Iran from September 2008 to March 2009. Based on the diagnostic criteria for functional dyspepsia symptoms presented to outpatient gastroenterology clinics, adult patients were invited to participate in this study. Upper GI endoscopy was performed in all the patients so as to rule out any gross pathology. The patients were asked about a list of nutrients including 114 foods which is commonly used in our area. Then, the effects of specific foods were identified on the relief or aggravation of the symptoms with four degrees: low, medium, high, and very high.
RESULTS
Of 384 patients, 152 were men and 231 were women with a mean ± SD age of 39.16±14 years (range: 13-80 years). The foods that caused the highest aggravation of symptoms were sausage and bolognas, pickles vinegar, soft drinks, grain, tea, salt, pizza, watermelon, red pepper, and macaroni. However, the most frequent foods that led to the alleviation of symptoms were apples, rice, rock candy, bread, caraway seed, dates, honey, yogurt, quince, and walnut.
CONCLUSION
This study shows that some foods, especially spicy, pickled, and high-fat foods, strongly induced dyspepsia and aggravated the symptoms in dyspeptic patients.
Keywords: Non-ulcer dyspepsia, Diet, Management
INTRODUCTION
Dyspepsia, defined as “pain or discomfort centered in the upper abdomen”, is a common symptom with an extensive differential diagnosis and a heterogeneous pathophysiology. It occurs in approximately 25% (ranging from 13% to 40%) of the population annually. However, most affected people do not seek medical care. The most important causes are non-ulcer (functional) dyspepsia and peptic ulcer.1,2
There is evidence that people with functional dyspepsia have a reduced quality of life. Many patients report their symptoms are related to food ingestion.3,4 Previous studies have made inconsistent observations with regard to eating patterns in functional dyspepsia. Furthermore, none of these studies has evaluated the relationship between symptoms and eating patterns concurrently.5 Many studies have reported that dyspeptic symptoms are associated with ingestion of some foods such as onions, peppers, fried and fatty foods, alcohol, citrus fruits, and spicy foods.5
Treatment of functional dyspepsia can be frustrating for physicians and patients. This is because few treatment options have proved effective so far. While patients need continued reassurance and support from their physicians, treatment is generally aimed at one of the presumed underlying etiologies of functional dyspepsia.6 Besides, current treatments for functional dyspepsia generally ignore the potential role of diet.
In some studies,7 the effect of fatty foods or carbohydrates has been evaluated on dyspepsia in general, but, in our study, we have evaluated the effect of 114 foods individually on alleviating or aggravating nonulcer dyspepsia. The purpose of this study is to determine specific diets that aggravate the disease and to show that avoidance of certain food items plays an important role in managing functional dyspepsia.
MATERIALS AND METHODS
This cross-sectional study was conducted at the Gastroenterology Department of Shahid Sadoughi Hospital, Yazd, Iran, from September 2008 to March 2009. Based on the diagnostic criteria of functional dyspepsia symptoms set by Rome III and reference to outpatient gastroenterology clinics, adult patients were invited to participate in the study.
The inclusion criteria for patients with functional dyspepsia were symptoms of postprandial fullness, bloating, epigastric pain, nausea, or vomiting of at least a moderate severity for more than 3 months. According to the Rome III criteria, upper GI endoscopy was performed for all the patients so as to rule out any organic cause. Patients with irritable bowel syndrome, previous abdominal surgery, and coronary artery diseases were excluded. Only patients with normal endoscopy or mild gastritis were included in the study, and those with ulcers, erosive gastritis, or cancer were excluded.
A questionnaire was prepared to elicit data about the patients’ demographic features, duration of dyspepsia symptoms, precedence of performed endoscopy, as well as a list of 114 commonly used foods and their aggravating or alleviating effect. Also, the relieving or aggravating effects of specific foods were identified in terms of four degrees: low, medium, high, and very high.
Other than 114 choice-controlled items on the questionnaire, there were three open-response questions about the types of food that would trigger symptoms and three types of food that would alleviate symptoms.
The sample size was calculated to be 384 (α=%0.5, p=%0.5, d=%0.5). Also, data were analyzed using Chi-square test and SPSS software, version 11.5.
RESULTS
Of 384 patients, 152 (39.6%) were men and 231 (60.4%) were women with a mean ± SD age of 39.16 ± 14 years (range: 13-80 years). Of these, 296 (77.1%) lived in urban areas and 88 (22.9%) lived in rural areas. With regard to education, 54 (14.1%) patients were illiterate, 105 (27.3%) had primary school degrees, 55 (14.3%) had a postgraduate diploma, and 46 (12%) had a higher education degree.
In this study, the patients with functional dyspepsia were evaluated on 114 nutrients. Thirty nine patients were ulcer-like, 189 were dysmotitlity-like, and the others were in unspecified categories. The patients’ opinions were collected regarding 114 edibles and their influence on dyspepsia and its symptoms.
According to figure 1 and table 1, the foods that aggravated the symptom the most were sausage and bolognas, pickles, foods and fruits, vinegar, soft drinks, grains, tea, salty foods, pizza, watermelon, red pepper, and macaroni (pasta).
Fig. 1 .
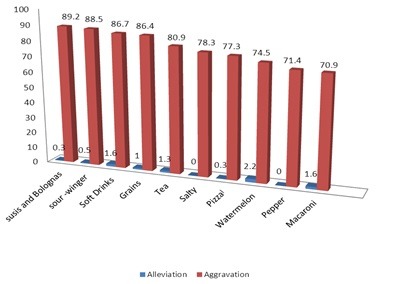
The 10 most common nutrients that aggravate symptoms in dyspeptic patients
Table 1 . Foods that aggravate and alleviate symptoms in dyspeptic patients .
| Food item | N (%) Reporting symptoms | Food item | N (%) Reporting symptoms | ||
| Aggravate | Alleviate | Aggravate | Alleviate | ||
| Carbonated drinks | 325 (86.7) | 6(1.6) | Apple | 74(19.5) | 65(17.2) |
| Legumes | 266(65.1) | 13(3.4) | Beans | 330(86.4) | 4(1) |
| Bell pepper | 240(71.4) | 2(0.5) | Bread | 33(8.6) | 56(14.6) |
| Sausage | 315(89.2) | 1(0.3) | Orange | 153 (48.3) | 2-0/6 |
| Bolognas | 313(89) | (0.1) | Peanut | 82(24.5) | 10(3) |
| Coffee | 125(60.1) | 3(1.4) | Eggs | 93(24.7) | 6(1.6) |
| Red meat | 45(11.8) | 28(7.4) | Cakes | 109(30) | 16(4.3) |
| Beef | 104(32.8) | 8 (2.7) | Yogurt | 59(15.6) | 44(11.6) |
| Pasta | 263(70.9) | 1(0.3) | Honey | 44(11.9) | 30(8.2) |
| Pineapple | 13(4.6) | 25(8.8) | Rock candy | 55(14.7) | 9.6 |
| Milk | 59(15.6} | 13(3.4) | Onions | 141(40.1) | 6(1.7) |
| Cheese | 29(7.6) | 15(3.9) | Mayonnaise | 128(36.3) | 2(0.6) |
| Cucumber | 225 ( 59.7) | 9(2.4) | Watermelon | 281(74.5) | 8(2.2) |
| Sweets | 16(4.3) | 109(30) | Cabbage | 187(54.4) | 6(1.7) |
| Tea | 309(80.9) | 5(1.3) | Grains | 162(44.1) | 5(1.4) |
According to figure 2 and table 2, the foods that alleviated the symptoms the best were apples, rice, rock candy, bread, caraway seeds, dates, honey, yogurt, quinces and walnuts. In this study, the items in the fatty group, especially oily ones, exacerbated the symptoms in 57% of the patients, but walnuts and almonds alleviated them (table 1).
Fig. 2 .
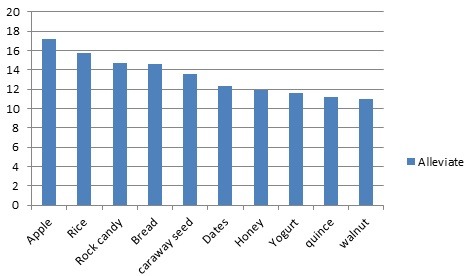
The 10 most common nutrients that alleviate symptoms in dyspeptic patients
Table 2 . Alleviating and aggravating nutrients .
| Nutrients | Alleviation | Aggravation |
| Sausage and Bolognas | 0.3 | 89.2 |
| Pickles -Vinegar | 0.5 | 88.5 |
| Soft Drinks | 1.6 | 86.7 |
| Grains | 1 | 86.4 |
| Tea | 1.3 | 80.9 |
| Salty foods | 0 | 78.3 |
| Pizza | 0.3 | 77.3 |
| Watermelon | 2.2 | 74.5 |
| Pepper | 0 | 71.4 |
| Macaroni | 1.6 | 70.9 |
In the fruit group, watermelon was the most aggravating food and aggravated the symptoms in 74.5% of the patients, followed by cucumber (59.7%), orange (48.3%), and citrus juice (42%). However, some fruits also had some relieving effects (figures 3 and 4).
Fig. 3 .
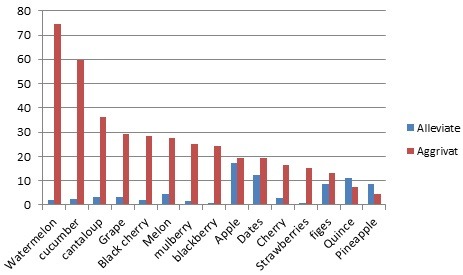
The 10 most common fruits that aggravate symptoms in dyspeptic patients
Fig. 4 .
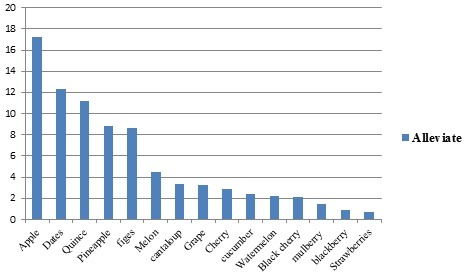
The most common fruits that alleviate symptoms in dyspeptic patients
In the beverage group, citrus juice had the most adverse effect on non-ulcer dyspepsia. It could especially exacerbate the symptoms in 42% of the patients. Also, carbonated drinks induced symptoms in 86.7% of the patients. As shown in table 1, coffee aggravated the symptoms in 60% of the patients, but it was had no effect in 38% of the patients. The studied participants rarely drank alcohol because of the strict religious beliefs in our country.
Sedative effects were reported by the patients. Rice had a good effect in 15.7% of the patients but had no effect on dyspepsia in 60% of the patients. Other nutrients like rock candy, bread, caraway seeds, dates, honey, yogurt, quinces, and walnuts were the most common foods having alleviating effects in this study (table 3).
Table 3 . : Food items that alleviate symptoms .
| Food item | Alleviate | Aggravate |
| Apple | 17.2 | 19.5 |
| Rice | 15.7 | 23.8 |
| Rock candy | 14.7 | 9.6 |
| Bread | 14.6 | 8.6 |
| Caraway seeds | 13.6 | 4.2 |
| Dates | 12.3 | 19.4 |
| Honey | 11.9 | 8.2 |
| Yogurt | 11.6 | 15.6 |
| Quince | 11.2 | 7.2 |
| Walnut | 11 | 10.5 |
The patients were also asked three open questions about aggravating and alleviating effects of specific food items that may not have been mentioned in the forum. Many of their answers were correlated with the answers mentioned in the forum.
DISCUSSION
Questions regarding diets are common questions a physician encounters in managing patients with dyspepsia, and every physician recommends a certain diet or avoidance of certain foods. Over the past years, internists have recommended to avoid raw fruits. Patients also say their symptoms are related to ingestion of a variety of food items and food groups, including fatty foods, carbohydrates, certain fruits and vegetables, coffee, and carbonated drinks. In gastroenterology textbooks and articles, the role of diet in these patients is questioned, and they recommend larger studies in this area. The exact mechanism by which diet induces dyspepsia symptoms has not been clarified yet. However, Feinle-Bisset et al.7 have suggested a few probable factors including gastric acid hypersecretion, alterations in the secretion of gastrointestinal hormones, gastric or small intestinal hypersensitivity, gastric emptying, and intragastric meal distribution.
The present study evaluated the opinion of patients regarding aggravating and alleviating effects of specific foods on their symptoms. These opinions can help physicians manage the disease better. In this study, the patients with functional dyspepsia were evaluated on 114 nutrients. The data analysis revealed a significant exacerbation of symptoms particularly by fats and oils.
The foods that caused the highest aggravation of the symptoms were sausage and bolognas, sour foods, vinegar, soft drinks, grains, tea, salty foods, pizza, watermelon, red pepper, and macaroni. This finding agrees with the limited amount of research ever done. The list of the food articles is almost the same as the one studied in Brazil, where it was found that foods strongly associated with dyspepsia were carbonated drink, pepper, fried foods, red meat, sausage, coffee, and pasta.7
As compared to the research reported in the literature, our study was conducted on a larger group (384 patients) and more diverse food items (114 items). These foods had either an effect or no effect or a bad effect. In case there were effects, they were grouped into mild, moderate, and severe. The sedative effects reported by the patients were not significant except for walnuts and almonds. The intensifying effect of beverage was significant. This finding is in agreement with Feinl et al.’s study which showed that people with functional dyspepsia have the ability to handle less volume of liquids and beverages.7 In our study, however, beverages, especially citrus juice and fuzzy beverage, induced symptoms in many patients. Coffee worsened the symptoms in many of our patients. In one study, coffee was found to promote reflux but did not affect dyspepsia.8 Coffee may aggravate dyspepsia symptoms in some cases9 and, if implicated, should be avoided.8-9
Tea, one of the most commonly used beverages in the world, aggravated the symptoms in over 80% of the patients in this study, but Chen et al. and Mahadva et al. showed that tea had an alleviating effect on dyspepsia. They reported that tea users suffer from dyspepsia less frequently.10-11 In contrast; our patients said that tea aggravated their symptoms. One reason for this discrepancy is that many patients with dyspepsia automatically learn to omit nutrients that do not suit them.
Pepper is one the items that mostly aggravated the symptoms in many patients. Pepper and pickles serve as a base for many nutrients. They are considered as one of the top10 stimulating nutrients that adversely affect dyspepsia.
Previous studies have demonstrated that red pepper consumed in diets taken not chronically stimulates the TRPV1 receptor, which increases the sensitivity of the patient. Capsaicin can mediate a painful, burning sensation in the human gut via the transient receptor potential vanilloid-1 (TRPV1). Chronic consumption of red pepper diets via TRPV1 receptors can decrease dyspeptic symptoms.12
Another question that is very common is ‘what food is good for dyspepsia? Alleviating effects of the above-mentioned foods are not as prominent as their aggravating effects, but many patients agree that rice, apple, caraway seeds, quince and rock candy had alleviating effects on dyspepsia. Other studies also show that rice is well tolerated and should be recommended, as a source of carbohydrate for patients with dyspepsia.12-13
In this study, the fatty group of nutrients proved to have significant aggravating effects on the symptoms in dyspeptic patients. The results of some other studies agree with ours.7,14-18 They all point out that the detriment may come through altered secretion of cholecystokinin (CCK), peptide-YY (PYY), and ghrelin and via the increased size of the antrum. Because the presence of lipid in the duodenum causes gastric sensitivity, avoidance of high-fat meals is advisable.18,19 This is of more relevance to dysmotitlity like dyspepsia that causes bloating. Alleviating effect of this group is not significant, expect for walnuts and almonds.
This study had several strengths. First of all, the number of patients included in the study was rather great. Secondly, the food items that were investigated constituted a wide variety of commonly used food items. Thirdly, the questions that the patients were asked were inclusive in that they seem to have covered all the important aspects of the research; they bore upon such matters as whether each and every of those specific foods was effective or not, the effect was favorable or adverse, and to what extent. The limitation of the study is that the patients’ opinions are largely influenced and preconditioned by their culture. Another limitation was that we could not exclude the cases with GERD which may have overlapped with functional dyspepsia.
This study shows that some foods can strongly increase dyspepsia symptoms. One may especially refer to spicy, pickles, and high-fat foods. In order for patients to realize whether or not dietary changes are effective in reducing dyspepsia symptoms, they can eliminate specific foods and then resume using those eliminated items. But because of induction symptoms, many patients avoid of certain edibles especially fruit. Many patients also omit some food items because of fear or cultural preconditions. So, further research is needed to establish the role of diet therapy in functional dyspepsia and logical use of diets.
CONFLICT OF INTEREST
The authors declare no conflict of interest related to this work.
Please cite this paper as:
Akhondi-Meybodi M, Aghaei MA, Hashemian Z. The Role of Diet in the Management of Non-Ulcer Dyspepsia. Middle East J Dig Dis 2015;7:19-24.
References
- 1.Tack J, Talley NJ, Camilleri M, Holtmann G, Hu P, Malagelada JR. et al. Functional gastroduodenal disorders. Gastroenterology. 2006;130:1466–79. doi: 10.1053/j.gastro.2005.11.059. [DOI] [PubMed] [Google Scholar]
- 2.Agréus L, Talley NJ. Dyspepsia: current understanding and management. Annu Rev Med. 1998;49:475–93. doi: 10.1146/annurev.med.49.1.475. [DOI] [PubMed] [Google Scholar]
- 3.Haug TT, Svebak S, Wilhelmsen I, Berstad A, Ursin H. Psychological factors and somatic symptoms in functional dyspepsiaA comparison with duodenal ulcer and healthycontrols. J Psychosom Res. 1994;38:281–91. doi: 10.1016/0022-3999(94)90033-7. [DOI] [PubMed] [Google Scholar]
- 4.Gutiérrez A, Rodrigo L, Riestra S, Fernández E, Cadahia V, Tojo R. et al. Quality of life in patients with functional dyspepsia:A prospective 1-year follow-up study in Spanish patients. Eur J Gastroen Hepat. 2003;15:1175–81. doi: 10.1097/00042737-200311000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Pilichiewicz AN, Horowitz M, Holtmann GJ, Talley NJ, Feinle-Bisset C. Relationship between symptoms and dietary patterns in patients with functional dyspepsia. Clin Gastroenterol Hepatol. 2009;7:317–22. doi: 10.1016/j.cgh.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 6.Ryan A, Loyd MD, David A. Update on the Evaluation and Management of Functional Dyspepsia. American Family Physician. 2011;83:547–52. [PubMed] [Google Scholar]
- 7.Feinle-Bisset C, Vozzo R, Horowitz M, Talley NJ. Diet, food intake, and disturbed physiology in the pathogenesis of symptoms in functional dyspepsia. Am J Gastroenterol. 2004;99:170–81. doi: 10.1111/j.1572-0241.2004.04003.x. [DOI] [PubMed] [Google Scholar]
- 8.Boekema PJ, Samsom M, van Berge Henegouwen GP, Smout AJ. Coffee and gastrointestinal function: facts and fition A review. Scand J Gastroenterol Suppl. 1999;230:35–9. doi: 10.1080/003655299750025525. [DOI] [PubMed] [Google Scholar]
- 9.Elta GH, Behler EM, Colturi TJ. Comparison of coffee intake and coffee-induced symptoms in patients with duodenal ulcer, nonulcer dyspepsia and normal controls. Am J Gastroenterol. 1990;85:1339–42. [PubMed] [Google Scholar]
- 10.Mahadeva S, Yadav H, Rampal S, Goh KL. Risk factors associated with dyspepsia in a rural Asian population and its impact on quality of life. Am J Gastroenterol. 2010;105:904–12. doi: 10.1038/ajg.2010.26. [DOI] [PubMed] [Google Scholar]
- 11.Chen TS, Luo JC, Chang FY. Psychosocial-spiritual factors in patients with functional dyspepsia: a comparative study with normal individuals having the same endoscopic features. Eur J Gastroenterol Hepatol. 2010;22:75–80. doi: 10.1097/MEG.0b013e32832937ad. [DOI] [PubMed] [Google Scholar]
- 12.Gonlachanvit S. Are rice and spicy diet good for functional gastrointestinal disorders? J Neurogastroenterol Motil. 2010;16:131–8. doi: 10.5056/jnm.2010.16.2.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miwa H, Ghoshal UC, Fock KM, Gonlachanvit S, Gwee KA, Ang TL. et al. Asian consensus report on functional dyspepsia. J Gastroenterol Hepatol. 2012;27:626–41. doi: 10.1111/j.1440-1746.2011.07037.x. [DOI] [PubMed] [Google Scholar]
- 14.Lacy BE, Talley NJ, Locke GR 3rd, Bouras EP, DiBaise JK, El-Serag HB. et al. Review Article: Current Treatment Options and Management of Functional Dyspepsia. Aliment Pharmacol Ther. 2012;36:3–15. doi: 10.1111/j.1365-2036.2012.05128.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Feinle-Bisset C, Horowitz M. Dietary factors in functional dyspepsia. Neurogastroenterol Motil. 2006;18:608–18. doi: 10.1111/j.1365-2982.2006.00790.x. [DOI] [PubMed] [Google Scholar]
- 16.Carvalho RV, Lorena SL, Almeida JR, Mesquita MA. Food intolerance, diet composition, and eating patterns in functional dyspepsia patients. Dig Dis Sci. 2010;55:60–5. doi: 10.1007/s10620-008-0698-8. [DOI] [PubMed] [Google Scholar]
- 17.Pilichiewicz AN, Feltrin KL, Horowitz M, Holtmann G, Wishart JM, Jones KL. et al. Functional dyspepsia is associated with a greater symptomatic response to fat but notcarbohydrate, increased fasting and postprandial CCK, and diminished PYY. Am J Gastroenterol. 2008;103:2613–23. doi: 10.1111/j.1572-0241.2008.02041.x. [DOI] [PubMed] [Google Scholar]
- 18.Feinle C, D’Amato M, Read NW. Cholecystokinin-A receptors modulate gastric sensory and motor responses to gastric distension and duodenal lipid. Gastroenterology. 1996;110:1379–85. doi: 10.1053/gast.1996.v110.pm8613041. [DOI] [PubMed] [Google Scholar]
- 19.Feinle C, Rades T, Otto B, Fried M. Fat digestion modulates gastrointestinal sensations induced by gastric distention and duodenal lipid in humans. Gastroenterology. 2001;120:1100–7. doi: 10.1053/gast.2001.23232. [DOI] [PubMed] [Google Scholar]


