Abstract
Encephaloceles, especially in the frontoethmoidal region, are a form of neural tube defect affecting patients in Southeast Asia more commonly than those in western countries, where they are more common in the occipital regions. All patients with classical frontoethmoidal encephalocele had swelling over the bridge of nose or inner canthus of eye since birth, with varying degrees of hypertelorism. This paper emphasizes on the clinical features of this pathology and its surgical management, along with, reviewing the evolution of single-stage correction and fine refinements.
Keywords: Bifida, encephalocele, spina
INTRODUCTION
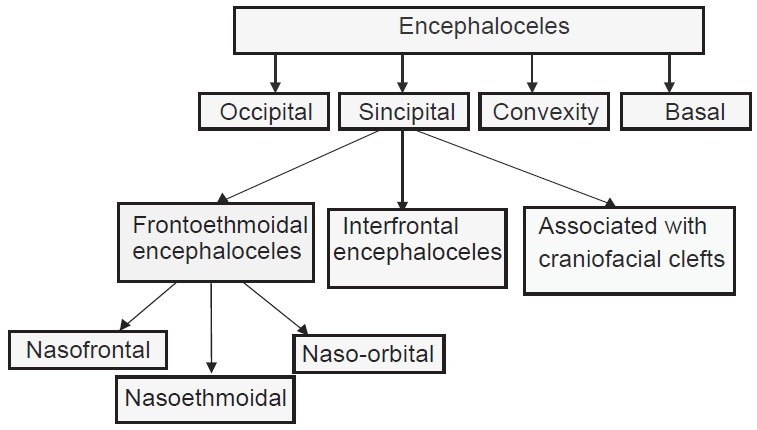
Encephalocele is defined as protrusion of cranial contents beyond the normal confines of the skull. They may contain meninges (meningocele), brain matter and meninges (meningoencephalocele) or they may communicate with the ventricles (meningoencephalocystocele).[1] Nasoethmoidal (sincipital type) is the most common and naso-orbital subtype is least common.[2] Classification of encephalocele is given in Table 1.[3] These swellings are either sessile or pedunculated and on palpation may vary from being solid and firm to soft and cystic type. The skin over the mass may be normal in appearance, thin and shiny or thick and wrinkled. Hyperpigmentation and hypertrichosis may be noted. Visual acuity may be decreased. Strabismus and lacrimal obstructions, resulting in epiphora and/or dacryocystitis can be observed.[4,5]
Table 1.
Suwanwela and Suwanwela classification[3]
CASE REPORT
Indication of surgical repair of the lesion (anterior encephalocele) is usually cosmetic. The goal is to return the cerebral components in to the cranial cavity along with amputation of dysplastic tissue and closure of the bony defect. Computed tomography (CT) scans with appropriate bony and soft tissue brain windows and three-dimensional reconstruction gives the best assessment. Thus, scans are integral to surgical planning.[2]
A 7-year-old boy reported to our department, with an encephalocele since birth that slowly increased in size, causing obvious facial disfigurement [Figure 1]. For the correction, craniofacial approach through a bicoronal scalp flap was taken. The thickened discolored skin over the midlines of tissue deformity was excised. Bifrontal craniotomy was performed. The neck of the meningoencephalocele was isolated by a combined intradural and extradural approach, and then the peduncle stalk was cut and the dural defect repaired [Figure 2]. The excision of the sac, followed by covering with Durapatch with a water-tight closure was done. The osteotomized bone segments were fixed with mini plates or titanium mesh as per requirement [Figure 3]. After 3 months follow-up [Figure 4], the patient is free of any complications and due for further cosmetic corrections. In an adult female 25 years of age, the growth was excised in a similar manner as above and in addition the nasal deformity was also corrected using the cranial graft to provide dorsal nasal support [Figure 5a–c]. Some authors advocated the use of costochondral graft for nasal reconstruction as they thought that the lower alar cartilages could be supported accurately by the chondral element, thereby giving an esthetic nasal tip that is not overly rigid.[6] There was no complication on follow-up visits and the younger patient has been advised to undergo procedures for further staged cosmetic correction.
Figure 1.

A 7-year-old boy with frontal encephalocele
Figure 2.
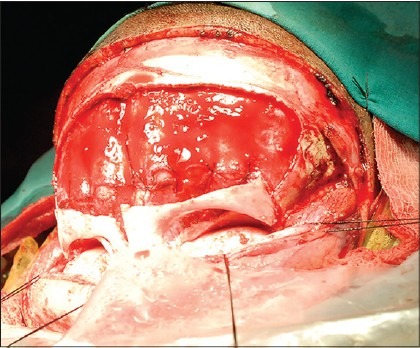
Frontal craniotomy done for access
Figure 3.
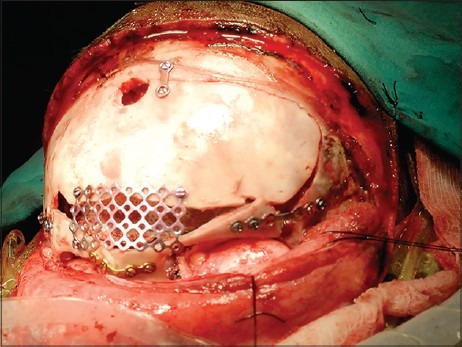
Durapatch used to cover the brain tissue and miniplate and titanium mesh used for fixation of osteotomized bone
Figure 4.

Postoperative picture after 3 months follow-up
Figure 5.
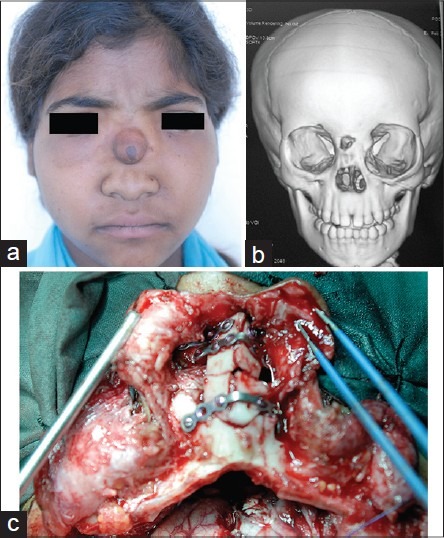
(a) Adult girl patient with naso-ethmoidal encephalocele, (b) three-dimensional computed tomography scan, and (c) nasal dorsum reconstruction with cranial graft
DISCUSSION
Anterior encephaloceles are rare congenital abnormalities characterized by herniation of intracranial components through the cranial and facial bones due to a defect of closure of the anterior neuropore of the neural tube.[7] Frontoethmoidal meningoencephaloceles are common in Southeast Asian countries, with an incidence of 1 in 5000 live births. These lesions affect children from the low socioeconomic class, but its etiology remains poorly understood.[8]
Encephaloceles can be congenital or acquired secondary to tumor, hydrocephalus or other cause.[9] Some suggest that its etiology could be ethnic, genetic, environmental factors, and paternal age. Among environmental factors, fungal and teratogenic agents such as aflatoxin or ochratoxin, found in moldy rice during the wet season, could be involved.[10] Neural tube defects like spina bifida can lead to frontoethmoidal meningoencephaloceles. This suggests a role of folate deficiency, although there is not much documentation on the relationship between maternal folate levels and its incidence.[11]
Theories of development[12]
Many theories have been postulated for the development of an anterior encephalocele:
Primary osseous defect leading to failure of the ethmoidal plate to close around the olfactory nerve. Herniation of the brain then takes place at a later stage
Increased ventricular pressure in the embryo could force the developing brain through the incompletely developed osseous structures
The theory proposed by Jeffrey-Saint-Hillaire (most acceptable): “The skull derives from two portions,” the endochondral cranial floor and the intramembranous cranial vault. At birth the frontal and ethmoidal bones are joined, but when the embryo is 3 months old, they are apart. Therefore, a weak point exists between the frontal and ethmoidal bones and that a congenital defect could result in an encephalocele herniation
A persistent craniopharyngeal canal could explain the rare encephaloceles through the sphenoid bone, but an early protrusion of cranial contents through this canal could lead to its persistence
Developmental failure of the ossification centers in the sphenoid bone could also be considered as a possible cause of encephaloceles in this region.
Frontoethmoidal encephalocele is classified according to the system described by Suwanwela and Suwanwela, based on the work by Mesterton[13] and Von Meyer,[6] dividing the deformity into nasofrontal, nasoethmoidal, and naso-orbital meningoencephalocoeles. Bhagwati and Mahapatra have recently proposed a modified classification of anterior encephaloceles.[12]
In nasofrontal type, defect lies at the junction of the frontal and nasal bones with the nasal bones attached to its inferior margin.[12] In nasoethmoidal type, lie between the nasal bones and the nasal cartilages. The nasal bones are deformed, often broadened with crimped margins. The frontonasal angle is obliterated, producing the appearance of an overhanging ledge. If the facial defect is confined to the nasal pyramid it is small and oval, and the medial walls of the orbit are not involved; if larger, the facial defect extends more laterally, then the anterior margins of the medial orbital walls are eroded and become crescent shaped.[12]
In naso-orbital type, defect is in the medial orbital walls situated in the frontal process of the maxilla and the lacrimal bones.[12] The frontoethmoidal encephalocele, is associated with craniofacial deformity consisting of interorbital hypertelorism (rarely true orbital hypertelorism/telorbitism because, the medial orbital walls are widened but the lateral orbital walls are usually in the normal position). Hence, the term interorbital hypertelorism gives a better description of the skeletal deformity.[6] Other deformities could be secondary trigonocephaly, orbital dystopia, elongation of the face, nasal deformity, and dental malocclusion. Some of the children have neurological complications or associated brain anomalies, although most are mentally normal.
Encephaloceles can cause recurrent meningioencephalitis due to direct communication of the central nervous system with the external environment, facilitating the entry of pathological microorganisms. The bacteria most commonly associated with meningitis in such patients is Steptococcus pneumoniae, followed by Staphylococcus aureus then Neisseria meningitides.[14]
Differential diagnosis of this could be traumatic encephalocele, ethmoid-frontal sinus mucocele, neurinoma, hemangioma (the diagnosis becomes obvious if there is a clinical or palpable cerebral pulsation) and glioma. Traditionally, two-stage correction by preliminary intracranial disconnection and subsequent extracranial correction of the facial deformity was done.[15] This staged method has been employed in our cases too, and the patients are due for further cosmetic corrections. A one-stage operation has been developed. In this a combined nasal-coronal approach with a frontal craniotomy is done. With this method, the frontal bone flap can also be remodeled to eliminate the trigonocephalic bulge, repair any external skull defects, and restore an esthetic appearance such as with nasal augmentation.[16] Mahatumarat et al. have proposed another procedure, the Chula technique, which has substituted a T-shaped osteotomy of the frontonaso-orbital bone, for the formal frontal craniotomy. Compared with previous techniques, this one provides a lower risk of cerebral spinal fluid leakage (2.8%) and meningitis (2.8%). The resected middle portion of the T-shaped osteotomized bone can also be used to augment the nose and decrease the distance between the medial orbital walls.[16] The prognosis depends on site, size, content of encephalocele and any other associated congenital anomaly. Survival rate is higher, nearly 100% in anterior encephalocele compared to posterior encephalocele (55%), where vital structure of brain parenchyma might have herniated to the skull defect.[13]
CONCLUSION
Early surgical intervention is important, so that the deformity does not progress and to prevent infection if an encephalocele has ruptured. Comprehensive surgical treatment of patients with frontoethmoidal meningoencephaloceles should be done by resection of the pathologic tissue, meningoplasty, repair of the osseous defect and reconstruction of the facial deformities (bone and soft tissues).
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Suwanwela C, Suwanwela N. A morphological classification of sincipital encephalomeningoceles. J Neurosurg. 1972;36:201–11. doi: 10.3171/jns.1972.36.2.0201. [DOI] [PubMed] [Google Scholar]
- 2.Mahapatra AK, Agrawal D. Anterior encephaloceles: A series of 103 cases. Journal Of Clinical Neuroscience. 2006;13:536–9. doi: 10.1016/j.jocn.2005.05.016. [DOI] [PubMed] [Google Scholar]
- 3.Diebler C, Dulac O. Cephaloceles: Clinical and neuroradiological appearance. Associated cerebral malformations. Neuroradiology. 1983;25:199–216. doi: 10.1007/BF00540233. [DOI] [PubMed] [Google Scholar]
- 4.Tandon PN. Meningoencephalocoeles. Acta Neurol Scand. 1970;46:369–83. doi: 10.1111/j.1600-0404.1970.tb05801.x. [DOI] [PubMed] [Google Scholar]
- 5.Tebruegge M, Curtis N. Epidemiology, etiology, pathogenesis, and diagnosis of recurrent bacterial meningitis. Clin Microbiol Rev. 2008;21:519–37. doi: 10.1128/CMR.00009-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Von Meyer E. About a basal herniation in the area of lamina cribrosa. Virchows Arch Pathol Anat Physiol Klin Med. 1890;120:309–20. [Google Scholar]
- 7.Hoving EW, Vermeij-Keers C. Frontoethmoidal encephaloceles, a study of their pathogenesis. Pediatr Neurosurg. 1997;27:246–56. doi: 10.1159/000121262. [DOI] [PubMed] [Google Scholar]
- 8.David DJ. Cephaloceles: Classification, pathology, and management - A review. J Craniofac Surg. 1993;4:192–202. [PubMed] [Google Scholar]
- 9.Holmes AD, Meara JG, Kolker AR, Rosenfeld JV, Klug GL. Frontoethmoidal encephaloceles: Reconstruction and refinements. J Craniofac Surg. 2001;12:6–18. doi: 10.1097/00001665-200101000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Dubey D, Pande S, Dubey P, Sawhney A. A case of naso-ethmoidal meningoencephalocele. Int Collab Res Intern Med Public Health. 2011;3:8. [Google Scholar]
- 11.Aung Thu, Hta Kyu. Epidemiology of frontoethmoidal encephalomeningocoele in Burma. J Epidemiol Community Health. 1984;38:89–98. doi: 10.1136/jech.38.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhagwati S, Mahapatra A. Pediatric Neurosurgery. London: Churchill Livingstone; 1999. Encephaloceles and anomalies of the scalp. editors; pp. 101–20. [Google Scholar]
- 13.Mesterton CB. Ommedfödt hjarnbråck [dissertation] Upsala: Upsala University; 1855. [Google Scholar]
- 14.Singh AK, Upadhyaya DN. Sincipital encephaloceles. J Craniofac Surg. 2009;20(Suppl 2):1851–5. doi: 10.1097/SCS.0b013e3181b6c49a. [DOI] [PubMed] [Google Scholar]
- 15.Lello GE, Sparrow OC, Gopal R. The surgical correction of fronto-ethmoidal meningo-encephaloceles. J Craniomaxillofac Surg. 1989;17:293–8. doi: 10.1016/s1010-5182(89)80056-3. [DOI] [PubMed] [Google Scholar]
- 16.Mahatumarat C, Rojvachiranonda N, Taecholarn C. Frontoethmoidal encephalomeningocele: Surgical correction by the Chula technique. Plast Reconstr Surg. 2003;111:556–65. doi: 10.1097/01.PRS.0000040523.57406.94. [DOI] [PubMed] [Google Scholar]


