Abstract
Maxillofacial reconstruction on a young child with huge aggressively growing lesion is a tough situation owing to several limiting factors. Besides the other factors, impact of the growing lesion on the psychology of the child also needs to be considered. This manuscript reports a case of an 18-month-old boy with juvenile cemento-ossifying fibroma in whom removal of a large portion of the jaws was required. The regeneration of the jaw bones with the help of protein signal guided reconstruction using bone morphogenetic protein-2 is described. Long-term follow-up of the patient with dental implants placed on the neo-osteogenic bone is reported.
Keywords: Dental implants, maxillofacial reconstruction, protein-signal, recombinant human bone morphogenetic protein-2, total jaw regeneration, total mandibular resection
INTRODUCTION
The clinical, radiological, and histological characteristics of oro-facial fibro-osseous lesions overlap, yet each of them has distinct pathogenesis besides their diverse origins. These rare lesions usually are mono-ostotic except fibrous dysplasia.[1] These lesions besides causing disfigurement could lead to alteration in growth, when occurring during growth. At such times, interfering to maintain normal growth becomes essential.
Recombinant human bone morphogenetic protein-2 (rhBMP-2) is shown to be an effective osteogenic signaling molecule for jaw reconstruction for critical sized defects. There are reports of off label use for immediate reconstruction in segmental reconstruction after tumor reconstruction with a titanium mesh guide.[2] The aim of this report is to present a case of juvenile aggressive cemento-ossifying fibroma (JCOF) in an 18-month-old infant involving both the jaws as well as to describe the successful reconstruction of mandible with rhBMP-2 in conjunction with rib graft.
CASE REPORT
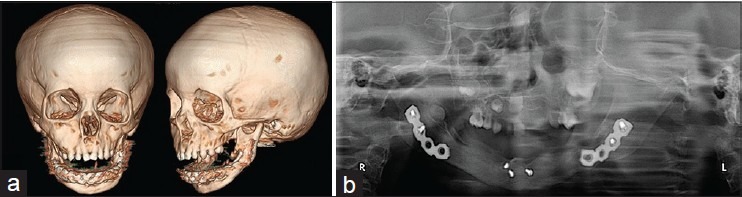
An 18-month-old boy was referred with the complaint of painless, progressive swelling in both the jaws since 6 months of age with gross facial disfigurement and obstruction of vision recently [Figure 1a and b]. Parents were concerned of compromised form, function and psychological impairment. There was a history of malalignment of teeth since eruption leading to difficulty in closing the mouth. There was no history of nasal obstruction, feeding difficulties, and no swelling elsewhere in the body.
Figure 1.
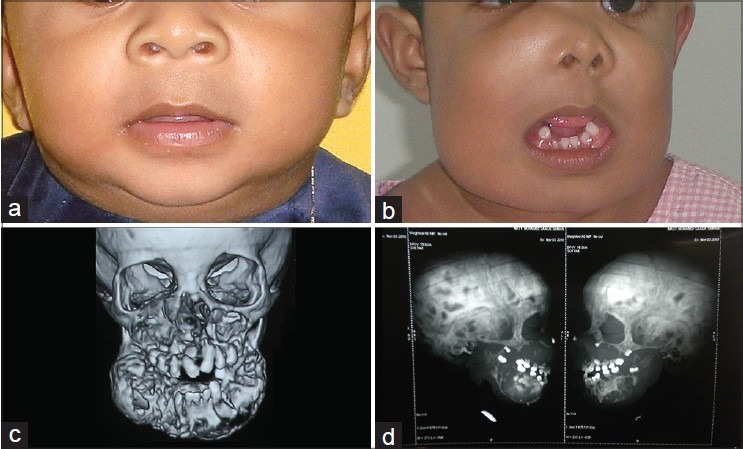
(a) Patient preoperative view at the age of 7 months. (b) Preoperative view at the age of 18 months with the right side facial swelling obliterating the right nasolabial fold, elevating the right lower eyelid. Note the mandibular swelling which is extending from angle to angle. (c and d) Preoperative computed tomography showing the well-defined, multiple solitary radiolucencies with radiopaque sclerotic margin, note the welldefined mandibular radiolucency with radiopaque border sparing bilateral condyle ramal unit and dentoalveolar segment of the anterior mandible
On examination, there was diffuse bony hard nontender swelling involving maxilla and mandible with normal overlying skin. Mandibular swelling involved from angle to angle and a similar swelling was present in the entire maxillae. The swelling also caused elevation of the right lower eyelid, nostril and nasal floor as well as displacement and spacing of teeth. Jaw movements, ophthalmological, and cervical lymph node examination were normal. Intraoral examination revealed multiple regions of asymmetric bony expansion of the buccal and lingual cortex on both right and left side of the mandible from angle to angle resulting in the obliteration of the buccolingual vestibular fold. Similar lesions were seen in maxilla.
Computed tomography (CT) revealed well-defined, multiple solitary radiolucencies with radiopaque sclerotic margin. In mandible, a well-defined radiolucency with radiopaque border sparing bilateral condyle ramal unit and the dentoalveolar segment of the anterior mandible was seen [Figure 1c and d]. There was thinning out of the inferior cortex of the mandible from angle to angle. An incisional biopsy from both the lesions confirmed it to be JCOF [Figure 2a–d].
Figure 2.
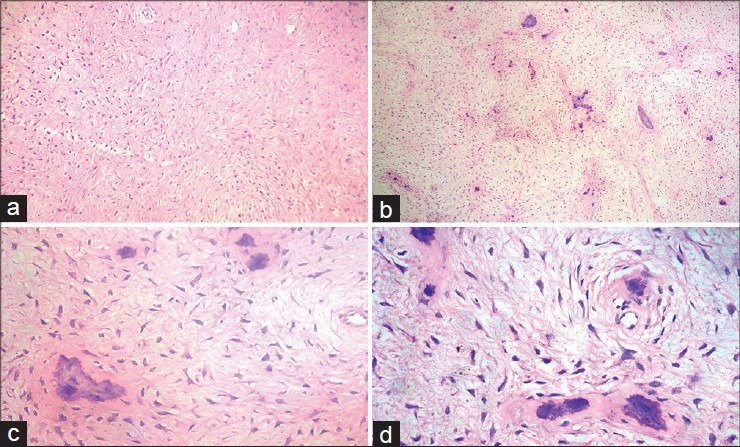
(a-d) Histopathological investigation showing the features of juvenile cemento-ossifying fibroma
After diagnosis, surgical en bloc removal and immediate reconstruction using rhBMP-2 with bone graft was planned for the mandible. For maxillary lesion, total enucleation was planned. Elective tracheostomy was done anticipating airway compromise from rhBMP-2 associated inflammatory swelling.
Under general anesthesia, mandibular degloving with subperiosteal dissection was done through crevicular incision with distal release incisions extending from the angle to angle, thus to expose the mandibular lesion. The periosteum was lifted, stripped taking adequate care not to injure or tear the periosteum. The lesion was removed as a single mass [Figure 3a and b]. The surrounding area was cauterized thoroughly. Fresh bleeding was induced. A titanium reconstruction plate was adapted and fixed to the residual mandible using the resected specimen as guide [Figure 3c]. Bone graft was harvested from the right 5th, 7th and 8th, ribs. The rib graft was osteotomied according to the need and secured to the reconstruction plate and host bone with titanium screws. Inside the periosteum, rhBMP-2 was supplemented to the surgical site using absorbable collagen sponge (ACS) as a carrier as indicated by the manufacturer [Figure 3d]. Layer wise primary closure was done thereby creating surgical bed enriched with rhBMP-2 enclosing the grafts. The maxillary lesion was approached via the transoral route. Subperiosteal dissection was performed exposing the entire maxillary lesion [Figure 4a and b]. The lesion was enucleated enmass, and the layers were closed using 3-0 silk. Postoperative recovery was uneventful.
Figure 3.
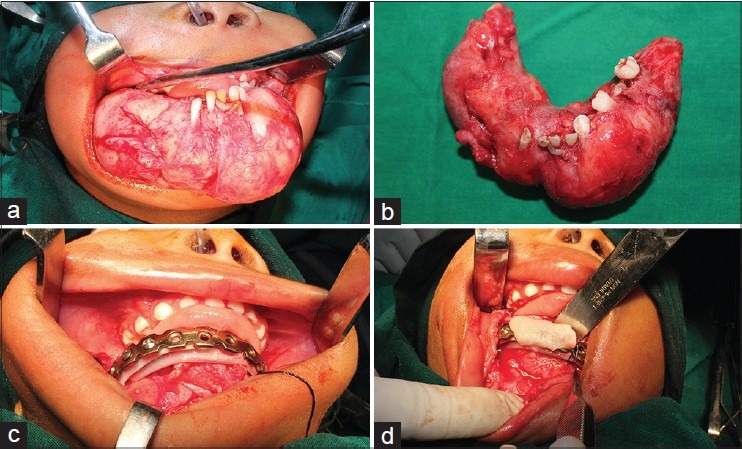
(a) Surgical enbloc removal of the mandibular lesion. (b) Resected specimen. (c and d) Immediate reconstruction of the mandible using recombinant human bone morphogenetic protein-2 with bone graft
Figure 4.
(a) Total nucleation of the maxillary lesion. (b) Resected specimen
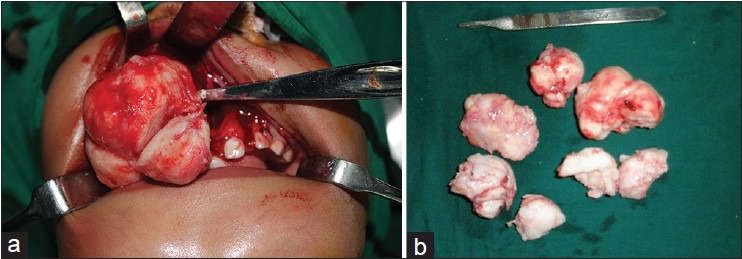
On the 3rd postoperative day, a large scale postoperative inflammatory response was observed [Figure 5]. This was attributed to the use of rhBMP-2. There were no associated complications. The tracheostomy tube was maintained in place for 5 days, after which it was removed when there was no threat of compression of the trachea from the inflammatory swelling.
Figure 5.

Postoperative inflammatory swelling attributed to the use of recombinant human bone morphogenetic protein-2. Note the tracheostomy tube in place
Periodical follow-up was ensured. At 6 months of follow-up, radiologic evidence of mandibular continuity was observed, and sufficient healing of maxilla was also visualized [Figure 6a and b]. No recurrence was noted in a year follow-up and dental implants were placed for functional rehabilitation. Bone retrieved during placement was of normal quality. At 36 months of age, patient had excellent form, function and social skills. Dental implants were later placed, and patient is under continuous follow-up with no evidence of recurrence of the lesion [Figure 7a–d].
Figure 6.
(a) Postoperative computed tomography showing the completely reconstructed mandible. (b) Postoperative orthopantomograph after removal of the reconstruction plate
Figure 7.
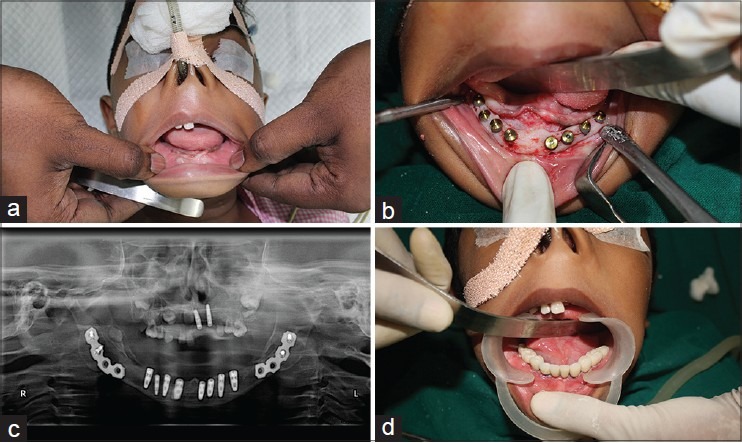
(a and b) Postoperative view at the age of 3 years showing the well-developed mandibular ridge with implant placement. (c and d) Orthopantomograph showing the implant abutment in mandible and the clinical image of implant prosthetic replacement
DISCUSSION
Losing large portion of the face at very young age causes morbidity in terms of growth, function and proper psychological well-being. Hence, in the present case, immediate reconstruction simulating the lost structure in terms of form and function including the growth was essential. Hence, with earlier reported experience from literature, use of rhBMP-2 was planned for the current case.[2,3] Anticipating the huge postoperative inflammation, elective tracheostomy was planned.
The rationale of using rhBMP-2 in this condition was two-following: (1) The lesional tissue was removed in-toto by en bloc resection with sufficient margins. Usually, the lesion by nature is confined within the capsule. (2) Periosteum provided much guidance for the remodeling of the rhBMP-2. The costochondral graft (rich in progenitor cells) and the plates provided the framework and stability, the ACS acted as carrier and rhBMP-2 acted as a signal that inducted the stimulus.[4] This combination has been very effective in previous experience.[5] After a year, the patient remained tumor-free, and implants have been placed on the newly formed alveolar ridge to stimulate the natural jaw function and esthetic rehabilitation. As the bone growth was normal, there was no psychological impairment or compromise of social skills indicating complete success of treatment.
CONCLUSION
The use of rhBMP-2 in immediate reconstruction at tumor site has been questioned. Though this could be off-label use of rhBMP-2, the option was exercised in this case as there was no other better alternative for the 20-month-old boy. An effective solution to the problem has been provided by the use of the treatment modality that has been debated.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Nwizu NN, Aguirre A, Chen F. Diagnostic challenges of benign fibro-osseous lesions and psammomatous meningiomas of the craniofacial region: A comparative review of their clinico-pathological features. N Am J Med Sci. 2010;3:17–23. [Google Scholar]
- 2.Cicciù M, Herford AS, Stoffella E, Cervino G, Cicciù D. Protein-signaled guided bone regeneration using titanium mesh and Rh-BMP2 in oral surgery: A case report involving left mandibular reconstruction after tumor resection. Open Dent J. 2012;6:51–5. doi: 10.2174/1874210601206010051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Balaji SM. Use of rhBMP2 with bone grafts in pediatric jaw resection cases. Int J Oral Maxillofac Surg. 2011;40:1096. [Google Scholar]
- 4.Balaji SM. Mandibular cystic defect: A composite approach with rhBMP-2 and rib graft. J Maxillofac Oral Surg. 2009;8:27–30. doi: 10.1007/s12663-009-0007-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Balaji SM. The efficacy of recombinant human bone morphogenetic protein-2 in alveolar cleft and mandibular reconstruction. Int J Oral Maxillofac Oral Surg. 2009;38:511. doi: 10.1007/s12663-009-0052-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


