Abstract
Rhinosporidiosis is a chronic granulomatous infective disease caused by fungi, Rhinosporidium seeberi. It can occur universally, is endemic in India, Sri Lanka and in South Asia, mainly reported from Southern India and Sri Lanka. Rhinosporidiosis is a chronic disease classically involving nose and nasopharynx and presents as a localized polypoid mass. Rhinosporidiosis involving parotid duct is rare. We encountered two cases of rhinosporidiosis at extremely unusual extranasal site-parotid duct, presenting as a cyst without nasal manifestations, which was misdiagnosed clinically and on cytological examination.
Keywords: Cyst, nasal polyp, parotid duct, rhinosporidiosis
INTRODUCTION
Rhinosporidiosis is a chronic granulomatous infective disease caused by fungi, Rhinosporidium seeberi. Nose and nasopharynx are the most common sites involved. Ocular lesions particularly of the conjunctiva and lacrimal sac, is second most common site. Rare sites of involvement are lips, palate, uvula, maxillary antrum, epiglottis, larynx, trachea, bronchus, ear, scalp, vulva, penis, rectum and skin. Rarely, disseminated infections are also reported, involving limbs, trunks, viscera and fatal brain involvement.[1] The first case was reported by Guillemo Seeber in 1900 in 19-year-old agricultural laborer suffering from nasal polyp hailing from Buenos Aires. Seeber's teacher Wernicke named it as Coccidium seeberia.[2] In 1923, Ashworth was the first person who described the life cycle of the organism. Recently it has been postulated that the causative organism is not a fungus but a Cyanobacterium, Microcystis aeruginosa.[3] The mode of infection from the natural aquatic habitat is through the traumatized epithelium and can spread by auto-inoculation, hematogenous route or lymphatics. Recurrences can occur due to spillage of endospores into adjacent epithelium.
CASE REPORTS
Case 1
An 18-year-old male residing in the village of Ganjam, Southern Coastal district of Orissa, a field worker by occupation presented to our dental out-patient department with the complaints of a soft painless slow growing swelling of the right cheek with drainage of an unpleasant salty fluid into the right buccal cavity of 1-year duration.
On extraoral examination, a 3 cm × 3 cm soft, nontender, unilocular, mobile, fluctuant swelling was palpable anterior to masseter which was not fixed to the skin or underlying tissue. Intraorally there was an inflammation at the opening of the parotid duct and whitish, thick seromucinous fluid was drained out from opening of the right parotid duct on external pressure on the same side of the cheek. There was no lymphadenopathy or parotid gland enlargement seen. Routine laboratory investigations were within normal limits, HIV antibodies and hepatitis B surface antigen was negative. Clinical diagnosis of sialocele or retention cyst of the parotid duct was made.
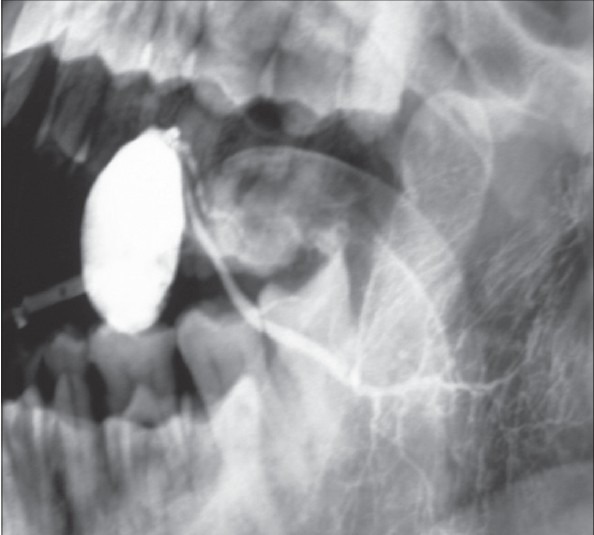
Sialogram revealed an irregular filling defect measuring 2.5 cm × 2 cm anterior to the parotid duct, no calculi were seen [Figure 1]. Diagnosis of sialocele was confirmed on ultrasonography [Figure 2]. On fine needle aspiration about 10 ml of seromucinous fluid was aspirated and cytodiagnosis of the parotid duct retention cyst was made. The cyst was excised under general anesthesia after ligating the parotid the duct. Excised cyst was sent for histopathological examination.
Figure 1.
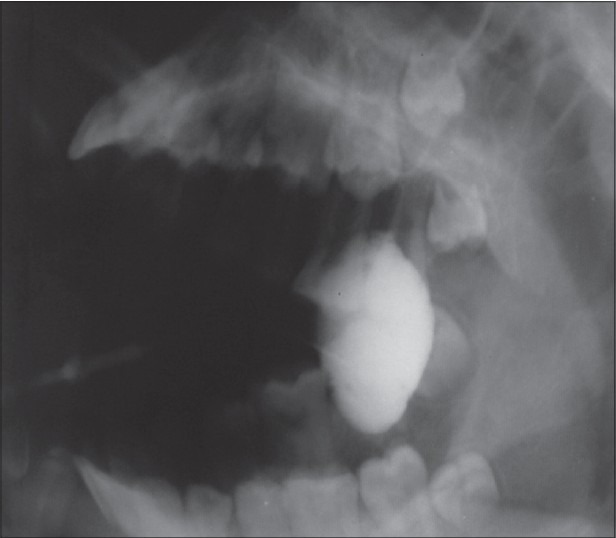
Sialogram of patient (case 1) showing filling defect in parotid duct
Figure 2.
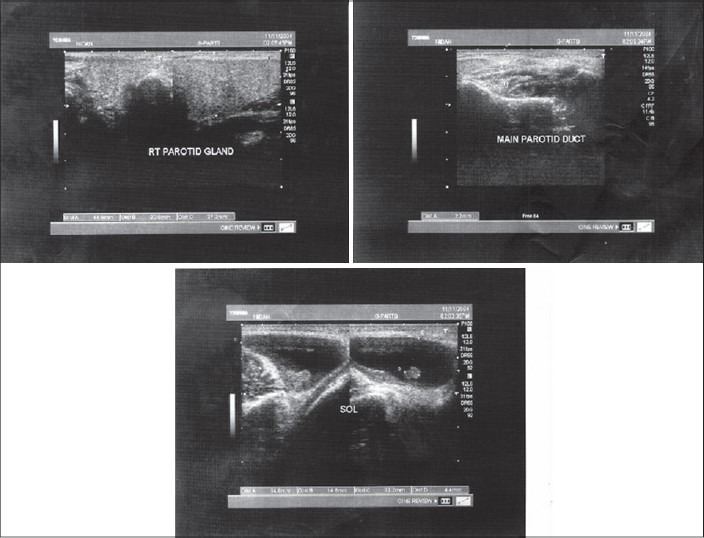
Ultrasonography of patient (case 1) showing right parotid gland with space occupying lesion and parotid duct
Grossly uniloculated cyst measured 4 cm in diameter and cut section showed hemorrhagic fluid [Figure 3]. Microscopically cyst was lined by columnar epithelium with subepithelial tissue showing sporangia of varying stages of maturation containing numerous and large spores surrounded by dense stroma infiltrated by chronic inflammatory infiltrate and giant cells [Figure 4]. No eosinophils/splendore hoeppli phenomenon were noted. Histopathological diagnosis of rhinosporidiosis of the parotid duct was made.
Figure 3.
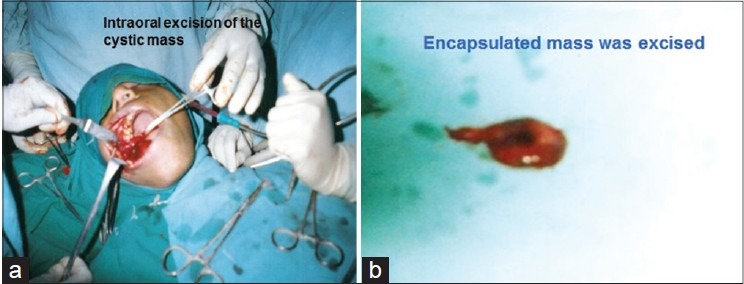
Operative field during intraoral excision (a) of cyst (case 1) and the excised cyst (b)
Figure 4.
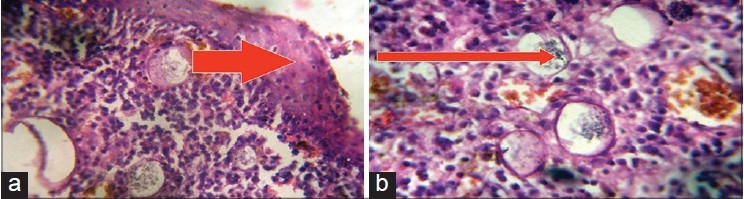
Photomicrography (×10) H and E, showing (a) metaplastic squamous epithelium with sub-epithelial dense stroma surrounding the sporangia. (b) Sporangia are seen in various stages of maturation with few collapsed cyst wall
Patient was followed-up for 1-year and there was no recurrence of the swelling and salivary outflow was normal.
Case 2
A 72-year-old male residing in the village of Ganjam, presented to our Dental out-patient department with complaints of a soft painless slow growing swelling of the left cheek with drainage of an unpleasant salty fluid into the left buccal cavity of 1-year 6 months duration. Patient was a known diabetic on treatment.
On extraoral examination, 2 × 2.5 cm soft, nontender, unilocular, mobile, fluctuant swelling was palpable anterior to masseter, which was not fixed to the skin or underlying tissue. Intraorally there was an inflammation at the opening of the parotid duct and whitish, thick seromucinous fluid was drained out from opening of the right parotid duct on external pressure on the same side of the cheek. There was no lymphadenopathy or parotid gland enlargement seen. Routine laboratory investigations, fasting and postprandial blood sugar levels were within normal limits, HIV antibodies and hepatitis B surface antigen was negative. Clinical diagnosis of sialocele of parotid duct was made. Sialogram showed cystic dilatation of the parotid duct near the opening of left parotid duct into the oral cavity [Figure 5]. On percutaneous fine-needle aspiration about 7.8 ml thick mucopurulent fluid was aspirated, and cytological diagnosis of possible retention cyst of the parotid duct was given. The cyst was excised under general anesthesia after ligating the parotid duct. Excised cyst was sent for histopathological examination.
Figure 5.
Sialogram of patient (case 2) showing cystic lesion with left parotid duct
Grossly uniloculated cyst measured 2 × 1.5 × 1.5 cm in size. Microscopically cyst was lined by columnar epithelium with subepithelial tissue showing sporangia of varying stages of maturation containing numerous and large spores surrounded by dense stroma infiltrated by chronic inflammatory infiltrate and giant cells [Figure 6]. No eosinophils/splendore hoeppli phenomenon was noted. Histopathological diagnosis of rhinosporidiosis of the parotid duct was made.
Figure 6.
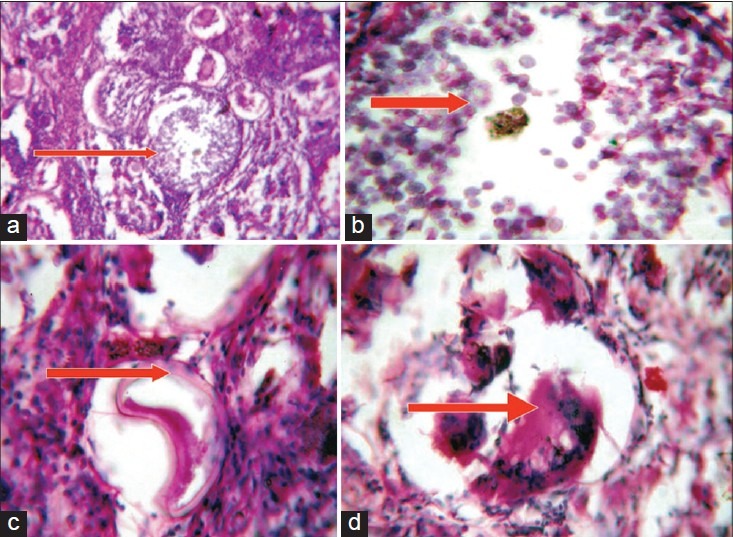
Photomicrographs [×10 (a, b), ×40 (c, d) H and E], showing mature sporangium (a) surrounded by dense stroma infiltrated by inflammatory cells, endospores (b), collapsed cyst (c) and foreign body giant cell reaction (d)
Post biopsy screening was done in both the cases to rule out involvement of other sites by rhinosporidiosis. There was no evidence of extra-parotid duct involvement.
DISCUSSION
Rhinosporidiosis involving parotid duct is a rare finding, with only few cases reported in the literature.[4] Mandalik observed that contact with infected water during bathing and swimming is the possible mode for nasal rhinosporidiosis.[5] Present two cases of the parotid duct rhinosporidiosis may be due to washing mouth with infected water. The natural patulous and everted anatomy of the orifice of the parotid duct in the buccal cavity could have promoted a quick passage of the spores into the duct resulting in the development of the disease.[6] Both the cases were missed on cytological examination due to the presentation at a rare site and lesion was localized only to the parotid duct without any other manifestations. Diagnosis was established by histopathology. Though, histopathological features are classical sometimes it can be confused with myospherulosis and Coccidioides immitis. Myospherulosis is an iatrogenically induced reactive process caused by the interaction of red blood cells with petrolatum, lanolin, or traumatized human adipose tissue in the nose, paranasal sinuses and sub-cutaneous tissue.[7]
Coccidioides immitis has similar mature stages represented by large, thick-walled, spherical structures containing endospores, but the spherules are smaller and contain small endospores and does not stain with mucicarmine.[8] The patients of present two cases did not give any history of injury or received any petrolatum based injections and on histopathology showed classical large sporangia with numerous large endospores without eosinophilic infiltrate. So diagnosis could be established by hematoxylin and eosin stain. Meticulous excision of the base is the treatment of choice. Both patients were followed-up for 1-year without any recurrence. Recurrence could be due to spillage of endospores into the adjacent mucosa.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Arseculeratne SN. Recent advances in rhinosporidiosis and Rhinosporidium seeberi. Indian J Med Microbiol. 2002;20:119–31. [PubMed] [Google Scholar]
- 2.Karunaratne WA. The pathology of rhinosporidiosis. J Path Bact. 1936;42:193–202. [Google Scholar]
- 3.Ahluwalia KB, Maheshwari N, Deka RC. Rhinosporidiosis: A study that resolves etiologic controversies. Am J Rhinol. 1997;11:479–83. doi: 10.2500/105065897780914938. [DOI] [PubMed] [Google Scholar]
- 4.Sivapathasundharam B, Saraswathi TR, Manjunath K, Sriram G. Rhinosporidiosis of parotid duct. Indian J Dent Res. 2009;20:388–9. doi: 10.4103/0970-9290.57362. [DOI] [PubMed] [Google Scholar]
- 5.Mandalik GS. A record of rhinosporidial polyp: With some observation on mode of infection. Ind Med Gaz. 1937;72:143–7. [PMC free article] [PubMed] [Google Scholar]
- 6.Kini U, Amirtham U, Shetty SC, Balasubramanya AM. Rhinosporidiosis of the parotid duct cyst: Cytomorphological diagnosis of an unusual extranasal presentation. Diagn Cytopathol. 2001;25:244–7. doi: 10.1002/dc.2047. [DOI] [PubMed] [Google Scholar]
- 7.Kyriakos M. Myospherulosis of the paranasal sinuses, nose and middle ear. A possible iatrogenic disease. Am J Clin Pathol. 1977;67:118–30. doi: 10.1093/ajcp/67.2.118. [DOI] [PubMed] [Google Scholar]
- 8.Morelli L, Polce M, Piscioli F, Del Nonno F, Covello R, Brenna A, et al. Human nasal rhinosporidiosis: an Italian case report. Diagn Pathol. 2006;1:25. doi: 10.1186/1746-1596-1-25. [DOI] [PMC free article] [PubMed] [Google Scholar]


