Abstract
Schistosomiasis is an endemic disease in Egypt caused by the trematode Schistosoma which has different species. Hepatic schistosomiasis represents the best known form of chronic disease with a wide range of clinical manifestations. The pathogenesis of schistosomiasis is related to the host cellular immune response. This leads to granuloma formation and neo angiogenesis with subsequent periportal fibrosis manifested as portal hypertension, splenomegaly and esophageal varices. Intestinal schistosomiasis is another well identified form of chronic schistosomal affection. Egg deposition and granuloma formation eventually leads to acute then chronic schistosomal colitis and is commonly associated with polyp formation. It frequently presents as abdominal pain, diarrhea, tenesmus and anal pain. Definite diagnosis of schistosomiasis disease depends on microscopy and egg identification. Marked progress regarding serologic diagnosis occurred with development of recent PCR techniques that can confirm schistosomal affection at any stage. Many antischistosomal drugs have been described for treatment, praziquantel being the most safe and efficient drug. Still ongoing studies try to develop effective vaccines with identification of many target antigens. Preventive programs are highly needed to control the disease morbidity and to break the cycle of transmission.
Keywords: Hepatic schistosomiasis, Portal hypertension, Intestinal schistosomiasis, Praziquantel
Introduction
Schistosomiasis is a chronic parasitic disease caused by a trematode blood fluke of the genus Schistosoma that belongs to the Schistosomatidae family [1]. It is a multifactorial disease that includes environmental, behavioral, parasitic, vector and host factors. It continues to be a significant cause of morbidity and mortality [2]. World Health Organization (WHO) considers schistosomiasis as the second only to malaria in socioeconomic importance worldwide and the third more frequent parasitic disease in public health importance [3].
Geographic distribution
There are five species of Schistosoma with a tendency to occur in restricted geographic patterns. S. mansoni is most prevalent in certain tropical and subtropical areas of sub-Saharan Africa, the Middle East, South America and the Caribbean. S. haematobium infection is acquired in North Africa, sub-Saharan Africa, the Middle East and India. S. japonicum occurs only in Asia. S. intercalatum occurs in Central and West Africa while S. mekongi is restricted to Laos and Cambodia [4] (Table 1). Currently, the largest number of cases of schistosomiasis occurs in Egypt, Yemen, and Algeria [5].
Table 1.
Schistosoma species and their geographic distribution.
| Schistosoma name | First intermediate host | Endemic Area |
|---|---|---|
| Schistosoma guineensis | Bulinus forskalii | West Africa |
| Schistosoma intercalatum | Bulinus spp | Africa |
| Schistosoma haematobium | Bulinus spp. | Africa, Middle East |
| Schistosoma japonicun | Oncomelania spp. | China, East Asia, Philippines |
| Schistosoma malayensis | Not known | South East Asia |
| Schistosoma mansoni | Biomphalaria spp. | Africa, South America, Caribbean, Middle East |
| Schistosoma mekongi | Neotricula aperta | South East Asia |
In Egypt, and following construction of the Aswan High Dam in 1960s, a striking change in the geographic distribution of the two species of Schistosoma (S. mansoni and S. haematobium) happened with an increasing prevalence of S. mansoni in the Nile Delta and concomitant decrease of S. haematobium prevalence spreading from the Nile Delta into Upper Egypt. This change was believed to be caused by less silt and by variability in the velocity and volume of water flow with a resultant shift in relative abundance of the corresponding snail vectors [5–9]. The largest and latest epidemiological survey in Egypt mentioned prevalence of S. haematobium in Upper Egypt (where it is endemic) to be around 7.8% while prevalence of S. mansoni in Lower Egypt (where it is endemic) to be around 36.4% [10].
Hepatic schistosomiasis
Hepatic schistosomiasis, or schistosomal hepatopathy, is the most common form of the chronic disease and usually results from heavy S. mansoni infection [11].
Pathogenesis
Hepatic schistosomiasis results from the host’s granulomatous cell-mediated immune response to the soluble egg antigen of S. mansoni, which progresses to irreversible fibrosis and, consequently, severe portal hypertension [12]. Eggs remain viable in the liver for about 3 weeks. Primarily, the eggs cause a moderate type 1 helper (Th1) response to egg antigens. However, this usually evolves to a dominant Th2 immune response to egg-derived antigens with later recruitment of eosinophils, granuloma formation and fibrogenesis of the liver [13,14] Fig. 1.
Fig. 1.
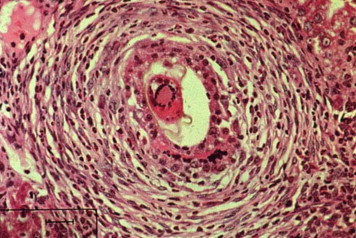
Schistosomal granuloma in liver. Granuloma surrounding schistosomal egg in the liver. (http://www.path.cam.ac.uk/~schisto/schistosoma/schisto_pathology_granuloma).
Although granuloma formation is beneficial for the host because it blocks the hepatotoxic effects of antigen released from parasite eggs, this process may lead to fibrosis with excessive accumulation of collagen and extracellular matrix proteins in the periportal space [15]. Granuloma formation is a helper T cell-mediated delayed hypersensitivity reaction driven by cytokines such as interleukin-4 (IL-4) and IL-13, whereas IL-10, IFN-γ, and a subset of regulatory T cells can limit the schistosomal induced pathology. In addition, a variety of cell types have been implicated, including hepatic stellate cells, activated macrophages, and regulatory T cells [16]. The balance between TH1- and TH2-type cytokines influences the extent of the pathology and the development of fibrosis [17]. Eggs are detectable inside the granulomas with the subsequent formation of marked portal and peri lobular fibrosis, which is most pronounced with S. mansoni and S. japonicum.
Added to fibrosis, angiogenesis is an important step in pathogenesis of schistosomal lesions. Its role is evident during periovular granuloma formation as well as in the genesis of schistosomal portal fibrosis [18]. The final result of hepatic schistosomiasis with a heavy S. mansoni burden is severe portal fibrosis and greatly enlarged fibrotic portal tracts, which resemble clay pipe stems thrust through the liver (termed Symmers pipe stem fibrosis) [19].
Interestingly, normal liver architecture is preserved, lobular architecture is retained, nodular regenerative hyperplasia is not observed, and thus the fibrosis could be reversible, at least impart. Moreover, angiogenesis in schistosomiasis seems to have a two-way mode of action, participating both in fibrogenesis and in fibrosis degradation [18]. Evidence from treated schistosomiasis of the mouse showed that hepatic schistosomal lesions can undergo considerable remodeling with time. Obstructive vascular lesions are partially or completely repaired with regression of the excess extracellular matrix [18]. With degradation of the long standing hepatic fibrosis and its removal, the main signs of portal hypertension (as splenomegaly and esophageal varices) can progressively disappear [20]. This dynamic state of equilibrium between forces of synthesis and breakdown with a possibility to cure schistosomiasis and associated hepatosplenic disease doesn’t happen with hepatic cirrhosis [21].
Co-infection with viral hepatitis, either hepatitis B virus (HBV) or hepatitis C virus (HCV) is very common since the regions with a high prevalence of schistosomiasis usually have a high endemicity of chronic viral hepatitis as well. An important cause of the high exposure to HCV was the establishment of a large reservoir of infection as a result of extensive schistosomiasis control programs that used intravenously administered tartar emetic 20–50 years ago [22]. The association between both schistosomiasis and HCV is known to cause earlier liver deterioration and more severe illness. The liver is the principal site for both HCV replication and egg deposition, which down-regulates the local immune responses in the liver [23] and results in suppression of the intrahepatic bystander immune response to HCV. This may also occur during inactive schistosomal infection since the ova remain in the hepatic portal tracts and their soluble antigens could influence the host’s cell-mediated immunity for a considerable time [24]. In addition, this co-infection can also produce a unique clinical, virologic and histologic pattern manifested by viral persistence with high HCV RNA titers, higher necro-inflammatory and fibrosis scores in liver biopsy specimens in addition to poor response to interferon therapy, and accelerated progression of hepatic fibrosis [25].
Clinical manifestations
Clinical presentation of hepatic schistosomiasis markedly differs from that of cirrhosis. Although the symptoms and signs of portal hypertension and hypersplenism are dominant in schistosomiasis, the counter part of hepatocellular failure is absent. However, some patients with schistosomiasis progress to an end stage of the disease by exhibiting muscle wasting, hypoalbuminemia, ascites and coma. These observations led to the concept of compensated and decompensated schistosomiasis to differentiate patients with the sole manifestations of portal hypertension from those who, in addition, presented signs of hepatocellular failure [26].
Intestinal schistosomiasis
Intestinal schistosomiasis represents another form of schistosomal affection. Among spectrum of intestinal lesions, polyps are the commonest [27].
Pathogenesis
Intestinal schistosomiasis is essentially due to S. mansoni infection [28] and it has been reported as well in some S. haematobium cases [29]. Egg-laying worms are present in the intestinal micro-vasculature especially in the distribution of the inferior mesenteric venous plexus. In the large intestine, ova are mainly distributed in the loose submucosa, and to a lesser extent in the subserosa where infrequently multiple granulomas are formed. Subsequently, the muscularis mucosa becomes involved and the overlying mucosa is either denuded forming small superficial ulcers or undergoes hyperplastic changes. Sandy patches develop when the submucosa becomes densely thickened by fibrous tissue containing immense numbers of calcified eggs; the overlying mucosa becomes atrophic and acquires a granular dirty yellowish appearance [30].
The pathogenesis of polyp formation starts by deposition of schistosomal eggs in the superficial layers of submucosa where the connective tissue is loose and not bounded superficially by firmer tissue. This allows the accumulation of large amounts of reactive cellular debris and vascular granulation tissue. In the submucosa, the eggs produce a cell mediated inflammatory response with granuloma formation and necrosis. As necrotic foci heal, fibrous connective tissue is formed and the adjacent muscularis mucosa becomes hypertrophied. The fibrous tissue in the submucosa and the hypertrophied muscularis mucosa form a barrier to the usual route of ova transit from the mesenteric veins to the gut lumen. This entrapment of ova leads to a foreign body reaction with progressive inflammation and fibrosis. As this process continues, a nodule is formed that elevates the hypertrophied muscularis mucosa and mucosa to form the earliest detectable polyp [31]. This mechanism can explain the main concentration of the S. mansoni ova in the polyps than in the adjacent mucosa and submucosa [32] Fig. 2.
Fig. 2.

Schistosomal colonic polyp. Colonic polyp with numerous calcified Schisosome eggs beneath the lamina propria. In (http://www.gastrohep.com/images/image.asp?id=1152).
Colonic mucosa of affected patients is usually edematous and congested with petechial hemorrhage in acute schistosomal colitis cases, while shows confused vascular net with flat or elevated yellow nodules, polyps and intestinal stricture in chronic colitis patients. Acute and chronic inflammation could be observed in colon segments of chronic active schistosomal colitis patients. The most characteristic finding is the grayish yellow or yellowish white schistosomal nodules similar to those of pseudomembranous enterocolitis [32]. Polyps range in size from 2 to 20 mm and may be sessile, pedunculated or showing a cauliflower appearance. They are mainly concentrated in the distal colon, and they count from few to very numerous polyps. The covering mucosa of the polyps is usually redder than the surrounding mucosa due to severe congestion and due to focal hemorrhages. Ulceration is common in rectal polyps, the ulcerated areas appear dusky to blackish gray in color caused by superficial hemorrhage, and are frequently secondarily infected [28,33].
Histologically, the typical polyp is composed of a stalk of fibrous connective tissue projecting from the sub mucosa into the lumen and partially covered with mucosa. The overlying mucosa consists of distorted glands with varied degrees of mucoid activity, mucinous degeneration, and adenomatous hyperplasia. Focal areas of ulceration frequently interrupt the surrounding mucosa. Larger areas of ulceration may be replaced by granulation tissue. Mononuclear cells, eosinophils, and few polymorphonuclear leukocytes infiltrate the mucosa. The supporting tissue is composed of fibrous connective tissue and muscle derived from the muscularis mucosa. Blood vessels may be present in large numbers but diminish as fibrosis progresses. Viable and nonviable eggs are present in all polyps [34].
Clinical manifestations
Schistosomal colonic polyposis affects mainly adult males. This male predominance is related to greater employment in agricultural work and higher rates of contact with water [35]. The primary presenting symptoms are usually tenesmus and the rectal passage of blood and mucous. Diarrhea, abdominal pain, dyspepsia, and irreducible schistosomal papilloma protruding from the anus occur in some patients [34,36]. Malnutrition, weight loss, nail clubbing, pitting peripheral edema, and pericolic masses may also be present [29,36,37]. Other manifestations include iron deficiency anemia, hypoalbuminemia, protein-losing enteropathy, and rectal prolapse [37,38]. The presence of polyposis does not appear to predispose patients to the development of large bowel cancer [39,40] and many investigators even have rejected any relationship between schistosomiasis and colorectal carcinoma, although this view is debatable if we consider S. japonicum [41–43]. However, there is a report on a patient with sigmoid cancer coexisting with schistosomiasis and the authors entailed a possible but inconclusive role for chronic schistosomiasis mansoni in promoting carcinogenesis of colorectal neoplasms [44].
Schistosomal appendicitis is a rare complication that can occur in 0.02–6.3% in endemic areas (representing 28.6% of chronic appendicitis in such region) and 0.32% in developed countries. Its main mechanism depends on mechanical appendiceal lumen obstruction by adult worms rather than being a complication from egg deposition [45].
Diagnosis
Definite diagnosis of the disease depends on certain tools as microscopy and egg identification, serology and radiologic findings. Other non-specific findings include eosinophilia (in relation to stage, intensity and duration of infection), thrombocytopenia (from splenic sequestration) and anemia (from chronic blood loss). Liver biochemical profile is usually normal [46]. Demonstration of parasite eggs in stool is the most common method used for making the diagnosis of schistosomiasis and species identification. To assess intensity of infection, quantitative sampling of defined amounts of stools (Kato Katz technique) is applied. Concentration techniques improve the sensitivity of egg detection. Moreover, further slide readings from the same stool sample using the Kato Katz technique associated with a serological test (three slides reading and the IgG anti-Schistosoma mansoni-ELISA technique) proved to be a useful procedure for increasing the diagnostic sensitivity [47]. Schistosomiasis can be diagnosed also by finding eggs in tissue biopsy specimens from rectal, intestinal and liver biopsies [48]. However, the sensitivity of these procedures is variable due to fluctuation of egg shedding [49].
Serologic tests can detect antischistosomal antibodies in serum samples. The main drawback is their inability to distinguish between past and current active infection. However, a negative test can rule out infection in endemic population. Another drawback is that they remain positive for prolonged periods following therapy making them unreliable for post treatment follow up [46]. To solve these defects, techniques to detect parasite antigens, in sera and stools, have recently been developed and can identify current infection and its intensity [50]. Urine dipstick diagnostic tests can detect schistosome circulating cathodic antigen (CCA). They were tested in field-based surveys, certainly for preschool children due to the difficulty to obtain consecutive stool samples, and provided a more sensitive and rapid testing for intestinal schistosomiasis. This may help in future epidemiological screening studies [51].
Sensitive and specific diagnostic methods of schistosomiasis at an early stage of infection are important to avoid egg-induced irreversible pathological reactions. Detection of free circulating DNA by PCR can be used as a valuable test for early diagnosis of prepatent schistosomiasis infection [52]. Several studies have developed polymerase chain reaction (PCR) methods to improve the direct detection of Schistosoma antigens. These tests are done on urine, stool, or organ biopsy samples, and involve the preparation of DNA from eggs prior to PCR amplification [53]. Only a small volume of sample can be used for DNA extraction, and it is dependent on chance whether the processed sample contains ova or not. Similarly, PCR has the same limitations as microscopy and does not provide a significant clinical benefit [49]. Another study detected S. haematobium-specific DNA in urine with similar specificity to detection of parasite eggs but with improved sensitivity [54]. Hopefully, an updated PCR assay has been available for the detection of Schistosoma mansoni DNA in human stool samples using QIAamp® DNA Stool Mini Kit. It allows the heating of the sample (until 95 °C) to facilitate the rupture of the egg and cellular lysis. It also includes Inhibitex, which adsorbs DNA damaging substances and PCR inhibitors present in the fecal material. For amplification, the DNA samples are diluted only 5-fold with good reproducibility and the study can provide high sensitivity and specificity results [55]. Another novel diagnostic strategy is developed, following the rationale that Schistosoma DNA may be liberated as a result of parasite turnover and reaches the blood. Cell-free parasite DNA (CFPD) can be detected in plasma by PCR for any stage of schistosomiasis [49].
Radiologically, abdominal ultrasonography plays an integral role in the diagnosis of hepatosplenic schistosomiasis. Imaging can show periportal fibrosis, splenomegaly, portal vein dimensions and the presence of collateral vessels. In addition, ultrasonography helps to assess degree of periportal fibrosis by measuring portal tract thickness: Grade I if thickness is 3–5 mm, Grade II if it is 5–7 mm and Grade III if it is more than 7 mm. This method reflects the hemodynamic changes and provides a good estimate of the clinical status of patients who have periportal fibrosis [56]. Portal hypertension is suspected when dilatation of one or more of the portal, mesenteric and splenic veins is detected. For the collateral vessels, the most commonly described are the left and right gastric, the short gastric, the par umbilical and the splenorenal veins [57,58] Fig. 3.
Fig. 3.

Periportal fibrosis detected by ultrasonography. Thickened portal tracts seen in the liver by abdominal ultrasonography [58].
Lastly, the hepatic veins in schistosomiasis can be assessed ultrasonographically. They remain patent with normal phasic flow as the disease evolves, which is different from liver cirrhosis. In advanced cirrhosis, hepatic venous outflow becomes monophasic [57]. Colonic affection can be diagnosed by endoscopy and biopsy from the abnormally apparent mucosa. Also, barium enema and double contrast enema may provide a diagnostic tool for colonic polyps [28].
Treatment
Interventions for the control of schistosome infections involve Mass Drug Administration (MDA) and/or chemotherapy of individuals, as well as improved sanitation, environmental modifications to reduce exposure to the snail intermediate hosts and to cercariae that have been shed by snails, and education to reduce unsafe water contact [59].
Praziquantel (PZQ) is the mainstay of chronic schistosomiasis treatment. It is quite safe and effective with a single oral dose of 40–60 mg/kg bodyweight producing cure rates ranging between 60% and 90%. Even those individuals who are not completely cured have drastic reductions in the number of excreted schistosome eggs which in turn greatly reduces the likelihood of long-term sequelae. Moreover, PZQ is active against all schistosome species infecting humans, an important feature, especially in those areas where more than a single species is present, typically in Africa where S. mansoni and S. haematobium are often co-endemic [60]. Looking for better coverage and aiming to improve compliance of preschool children (aged ⩽ 5 years) during mass treatment campaigns targeting schistosomiasis, the WHO provided certain areas with a syrup formulation of PZQ. This syrup form gave very similar efficacies to crushed PZQ tablets in the treatment of this special age group [61].
However, with just one drug used for individual patient management and community-based morbidity control, resistance to praziquantel may emerge and spread [62]. The second shortcoming of PZQ is the fact that it is not active against juvenile schistosomes [63]. When administered in the first few days after infection, PZQ is apparently effective, but activity rapidly drops until it reaches insignificant levels around the fourth week and then starts rising again to attain maximal efficacy around the seventh week. The practical consequence of this phenomenon is that, in areas of very active transmission of infection, many people are likely to harbor immature worms at the time of treatment, with the result of correspondingly low cure rates [64].
Some antimalarial drugs were found to have some antischistosomal properties, such as the artemisinin, synthetic trioxolanes, and mefloquine [62]. They are effective against the juvenile stages of schistosome species but are less effective against adult worms. From systematic review and meta-analysis, the combination of an artemisinin derivatives plus praziquantel showed a higher cure rate than praziquantel monotherapy. This confirms that artemisinin derivatives used in combination with praziquantel have the potential to increase the cure rates in schistosomiasis treatment, but not artesunate alone. However, the incorporation of artemisinin derivatives in mass praziquantel administration has some limitations such as the higher cost-effectiveness implications, the required repeated treatments and most importantly the possibility of emergence of artemisinin-resistant malaria [64].
As treatment depends on the stage of infection and the clinical presentation, Deng et al. recommended a new clinical classification after reviewing the medical records of 11 092 cases of advanced schistosomiasis. Based on the new classification method, there were eight types: huge splenomegaly, ascites, colon proliferative, dwarf, universal, bleeding, hepatic coma, and miscellaneous. The aim of this new classification method was to present a more comprehensive picture for clinical features, severe complications and prognosis of advanced schistosomiasis [65]. The effect of antischistosomal treatment on disease manifestations varies by stage. Early hepatomegaly is known to resolve after specific anti schistosomal chemotherapy. Late manifestations, such as fibrosis, do not change. Additional management modalities are necessary for patients with combined infection (e.g. schistosomiasis and HCV), such as hepatocellular failure with ascites and encephalopathy which need diuretics and anticoma measures [66].
For primary prophylaxis of variceal bleeding; beta-blockers or endoscopic therapy could be used. For the control of acute variceal bleeding, endoscopic therapy is effective. Ligation is the recommended form; although sclerotherapy may be used in the acute setting if ligation is technically difficult. Endoscopic therapy with tissue adhesive (e.g., N-butyl-cyanoacrylate) is recommended for acute gastric variceal bleeding. Interventional therapy such as TIPS, shunt surgery and decompressive surgery should only be considered for patients with failure of endoscopic therapy [67].
Colonoscopic polypectomy is safe and effective and may be required along with medical therapy to achieve complete symptom relief and prevent complications. All symptomatic or large polyps should be removed after pharmacologic treatment even before waiting for complete parasitological cure because they will not resolve with medical treatment alone [33,34,68,69].
Vaccination
Clinical trials to develop an antischistosomal vaccine are still in progress. A recent study identified certain issues to facilitate its development and licensure as follows: Identification of the human immunoprotective antigens and mechanisms, induction of the appropriate responses by adjuvant vaccines, understanding the effect of immunization on immunopathology, development of an improved serologic assay to determine worm burden, and generation of a fund to apply it primarily through a project [70]. More than 10 antigens with strong potential as vaccines candidates were tried; most of them failed to move forward [71]. The most eligible candidates are egg antigens and the schistosomular tegument membrane antigens (Sm 23, SmTSP-2 and Sm29) [72]. From proteomic analysis, the most important target of the schistosome was found to be the tegument. Sm-TSP-2 is thought to play a critical role in tegument development and maturation [73]. Another newer chimeric form (Sm-TSP-2/5B) showed significant reductions in adult worm and liver egg burdens in two separate murine schistosomiasis challenge studies. Enhanced protection was obtained with the chimeric fusion protein and was associated with increased production of anti-Sm-TSP-2 antibodies as well as IL-4, IL-10 and IFN-γ in vaccinated animals [74].
Another recently identified and promising antigen is Sm 14, a 14 kDa fatty acid binding protein, which provokes protection against S. mansoni. It appears to be a viable and stable vaccine candidate for clinical testing [75]. Finally, tetraspanins were evaluated as vaccine candidates: Sj23 is a tegument tetraspanin used in DNA vaccine for water buffaloes, an important reservoir for S. japonicum in China [76].
Another potential strategy that could accelerate the achievement of an effective vaccine would be the association of different recombinant antigens that previously resulted in partial protection or the use of pools of antigens known as multivalent or multiepitope vaccines [14].
Footnotes
Peer review under responsibility of Cairo University.
References
- 1.Badr M. Detection of bladder cancer. In: El-Bolkany, Chu, editors. Bladder cancer. Al-Ahram Press; 1981. p. 1. [Google Scholar]
- 2.Burke M.L., Jones M.K., Gobert G.N., Li Y.S., Ellis M.K., McManus D.P. Immunopathogenesis of human schistosomiasis. Parasite Immunol. 2009;31:163–176. doi: 10.1111/j.1365-3024.2009.01098.x. [DOI] [PubMed] [Google Scholar]
- 3.Sarvel A.K., Oliveira A.A., Silva A.R., Lima A.C., Katz N. Evaluation of a 25-year-program for the control of schistosomiasis mansoni in an endemic area in Brazil. PLoS Negl Trop Dis. 2011;5:e990. doi: 10.1371/journal.pntd.0000990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hagan P., Gryseels B. Schistosomiasis research and the European community. Trop Geogr Med. 1994;46:259–268. [PubMed] [Google Scholar]
- 5.Hotez P.J., Savioli L., Fenwick A. Neglected tropical diseases of the middle East and North Africa: review of their prevalence, distribution, and opportunities for control. PLoS Negl Trop Dis. 2012;6(2):e1475. doi: 10.1371/journal.pntd.0001475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abdel-Wahab M.F., Strickland G.T., El-Sahly A., El-Kady N., Zakaria S., Ahmed L. Changing pattern of schistosomiasis in Egypt, 1935–1979. Lancet. 1979;2:242–244. doi: 10.1016/s0140-6736(79)90249-6. [DOI] [PubMed] [Google Scholar]
- 7.Abdel-Wahab M.F., Yosery A., Narooz S., Esmat G., el Hak S., Nasif S. Is Schistosoma mansoni replacing Schistosoma haematobium in the Fayoum? Am J Trop Med Hyg. 1993;49:697–700. doi: 10.4269/ajtmh.1993.49.697. [DOI] [PubMed] [Google Scholar]
- 8.Cline B.L., Richards F.O., El Alamy M.A., El Hak S., Ruiz-Tiben E., Hughes J.M. 1983 Nile Delta schistosomiasis survey: 48 years after Scott. Am J Trop Med Hyg. 1989;41:56–62. [PubMed] [Google Scholar]
- 9.Michelson M.K., Aziz F.A., Gamil F.M., Wahid A.A., Richards F.O., Juranek D.D. Recent trends in the prevalence and distribution of schistosomiasis in the Nile delta region. Am J Trop Med Hyg. 1993;49:76–87. doi: 10.4269/ajtmh.1993.49.76. [DOI] [PubMed] [Google Scholar]
- 10.El-Khoby T., Galal N., Fenwick A., Barakat R., El-Hawey A., Nooman Z. The epidemiology of schistosomiasis in Egypt: summary findings in nine governorates. Am J Trop Med Hyg. 2000;62:88–99. doi: 10.4269/ajtmh.2000.62.88. [DOI] [PubMed] [Google Scholar]
- 11.Lambertucci J.R., Cota G.F., Pinto-Silva R.A., Serufo J.C., Gerspacher-Lara R., Costa Drummond S. Hepatosplenic schistosomiasis in field-based studies: a combined clinical and sonographic definition. Mem Inst Oswaldo Cruz. 2001;96:147–150. doi: 10.1590/s0074-02762001000900022. [DOI] [PubMed] [Google Scholar]
- 12.Van der Kleij D., Latz E., Brouwers J.F., Kruize Y.C., Schmitz M., Kurt-Jones E.A. A novel host parasite lipid cross-talk. Schistosomal lyso-phosphatidylserine activates toll-like receptor 2 and affects immune polarization. J Biol Chem. 2002;277:48122–48129. doi: 10.1074/jbc.M206941200. [DOI] [PubMed] [Google Scholar]
- 13.Wynn T.A., Thompson R.W., Cheever A.W., Mentink-Kane M.M. Immunopathogenesis of schistosomiasis. Immunol Rev. 2004;201:156–167. doi: 10.1111/j.0105-2896.2004.00176.x. [DOI] [PubMed] [Google Scholar]
- 14.Wilson M.S., Mentink-Kane M.M., Pesce J.T., Ramalingam T.R., Thompson R., Wynn T.A. Immunopathology of schistosomiasis. Immunol Cell Biol. 2007;85(2):148–154. doi: 10.1038/sj.icb.7100014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morais C.N., Souza J.R., Melo W.G., Aroucha M.L., Miranda P., Domingues A.L. Cytokine profile associated with chronic and acute human schistosomiasis mansoni. Mem Inst Oswaldo Cruz. 2008;103:561–568. doi: 10.1590/s0074-02762008000600009. [DOI] [PubMed] [Google Scholar]
- 16.Gryseels B., Polman K., Clerinx J., Kestens L. Human schistosomiasis. Lancet. 2006;368:1106–1118. doi: 10.1016/S0140-6736(06)69440-3. [DOI] [PubMed] [Google Scholar]
- 17.Stadecker M.J., Asahi H., Finger E., Hernandez H.J., Rutitzky L.I., Sun J. The immunobiology of Th1 polarization in high pathology schistosomiasis. Immunol Rev. 2004;201:168–179. doi: 10.1111/j.0105-2896.2004.00197.x. [DOI] [PubMed] [Google Scholar]
- 18.Andrade Z.A., Santana T.S. Angiogenesis and schistosomiasis. Mem Inst Oswaldo Cruz. 2010;105:436–439. doi: 10.1590/s0074-02762010000400013. [DOI] [PubMed] [Google Scholar]
- 19.Symmers W.S.C. Note on a new form of liver cirrhosis due to the presence of ova of Bilharzia haematobilium. J Pathol Bacteriol. 1904;9:237–239. [Google Scholar]
- 20.Andrade Z.A., Baptista A.P., Santana T.S. Remodeling of hepatic vascular changes after specific chemotherapy of schistosomal periportal fibrosis. Mem Inst Oswaldo Cruz. 2006;101:267–272. doi: 10.1590/s0074-02762006000900041. [DOI] [PubMed] [Google Scholar]
- 21.Andrade Z.A. Extracellular matrix degradation in parasitic diseases. Br J Med Biol Res. 1994;27:2273–2281. [PubMed] [Google Scholar]
- 22.Frank C., Mohamed M.K., Strickland G.T., Lavanchy D., Arthur R.R., Magder L.S. The role of parenteral antischistosomal therapy in the spread of hepatitis C virus in Egypt. Lancet. 2000;355:887–891. doi: 10.1016/s0140-6736(99)06527-7. [DOI] [PubMed] [Google Scholar]
- 23.Lundy S.K., Lerman S.P., Boros D.L. Soluble egg antigen stimulated T-helper lymphocyte apoptosis and evidence for cell death mediated by FasL + T and B cells during murine Schistosoma mansoni infection. Infect Immun. 2001;69:271–280. doi: 10.1128/IAI.69.1.271-280.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Farid A., Al-Sherbiny M., Osman A., Mohamed N., Saad A., Shata M.T. Schistosoma infection inhibits cellular immune responses to core HCV peptides. Parasite Immunol. 2005;27:89–96. doi: 10.1111/j.1365-3024.2005.00762.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kamal S.M., Turner B., He Q., Rasenack J., Bianchi L., Al Tawil A. Progression of fibrosis in hepatitis C with and without schistosomiasis: correlation with serum markers of fibrosis. Hepatology. 2006;43:771–779. doi: 10.1002/hep.21117. [DOI] [PubMed] [Google Scholar]
- 26.Andrade Z.A. Schistosomal hepatopathy. Mem Inst Oswaldo Cruz. 2004;99:51–57. doi: 10.1590/s0074-02762004000900009. [DOI] [PubMed] [Google Scholar]
- 27.Ismail M.M., Attia M.M., El-Badawy A.A., Farghaly A.M., Husein M.H., Metwally A. Treatment of schistosomiasis with Praziquantel among school children. J Egypt Soc Parasitol. 1994;24:487–494. [PubMed] [Google Scholar]
- 28.El-Garem A.A. Schistosomiasis. Digestion. 1998;59:589–605. doi: 10.1159/000007534. [DOI] [PubMed] [Google Scholar]
- 29.Ata A.A., Raziky S.H., El-Hawey A.M., Rafla H. A clinicopathological study of schistosomal colonic polyposis and their pathogenesis. J Egypt Med Assoc. 1970;53:767–772. [PubMed] [Google Scholar]
- 30.Strickland G.T. Leading article: tropical infections of the gastrointestinal tract and liver series. Gastrointestinal manifestations of schistosomiasis. Gut. 1994;35:1334–1337. doi: 10.1136/gut.35.10.1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mostafa I. Schistosomal colonic polyposis. Gastrointest Endosc. 1997;46:584–587. [PubMed] [Google Scholar]
- 32.Cao J., Liu W.J., Xu X.Y., Zou X.P. Endoscopic findings and clinicopathologic characteristics of colonic schistosomiasis: a report of 46 cases. World J Gastroenterol. 2010;16:723–727. doi: 10.3748/wjg.v16.i6.723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thakeb F., El-Kalouby A.H., Ibrahim I.M., Hunter S., Zakaria S. Colonoscopic polypectomy in management of schistosomal colonic polyposis. Egypt J Bilh. 1980;7:49–56. [Google Scholar]
- 34.Mostafa IM, Zakaria S, Khalil A, El-Kaluoby A. The effect of medical treatment and endoscopic polypectomy on clinicopathological, immunological and endoscopic aspects of schistosomal colonic polyposis in Egypt. In: Proceedings of the world congresses of gastroenterology 1990; Sydney, Australia; 1260.
- 35.El Malatatwy A., El Habashy A., Lechine N., Dixon H., Davis A., Mott K.E. Selective population chemotherapy among school children in Beheira Governate: the UNICEF/Arab Republic of Egypt/WHO Schistosomiasis Contrl Project. Bull World Health Organization. 1992;70:47–56. [PMC free article] [PubMed] [Google Scholar]
- 36.Abaza H., Asser L., Mostafa S., El Mallah S. Management of schistosomal colonic polyposis. J Egypt Med Assoc. 1986;69:101–110. [Google Scholar]
- 37.Dimmette R.M., Sproat H.F. Recto-sigmoid polyps in schistosomiasis. General clinical and pathological considerations. Am J Trop Med Hyg. 1955;4:1057–1067. doi: 10.4269/ajtmh.1955.4.1057. [DOI] [PubMed] [Google Scholar]
- 38.Farid Z., Bassily S., Lehman J.S., Jr., Kent D.C., Haxton J., Patwardhan V.N. Iron loss and reabsorption in Ancylostoma duodenale infection and bilharzial colonic polyposis. Trans R Soc Trop Med Hyg. 1970;64:881–884. doi: 10.1016/0035-9203(70)90106-9. [DOI] [PubMed] [Google Scholar]
- 39.Nebel O.T., El Masry N.A., Castell D.O., Farid Z., Fornes M.F., Sparks H.A. Schistosomal disease of the colon. A reversible form of polyposis. Gastroenterology. 1974;67:939–949. [PubMed] [Google Scholar]
- 40.Barsoum H. Cancer in Egypt: its incidence and clinical forms. Acta Uni Intern ConCan. 1953;9:241–250. [PubMed] [Google Scholar]
- 41.El-Rooby A. The gastroenterology of schistosomiasis in complied review of bilharziasis. The national information and documentation center (NIDOC) Cairo. 1991:137–143. [Google Scholar]
- 42.Mohamed A.R., Al Karawi M., Yasawy M.I. Schistosomal colonic disease. Gut. 1990;31:439–442. doi: 10.1136/gut.31.4.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Xu Z., Su D.L. Schistosoma Japonicum and colorectal cancer: an epidemiological study in the People’s Republic of China. Int J Cancer. 1984;34:315–318. doi: 10.1002/ijc.2910340305. [DOI] [PubMed] [Google Scholar]
- 44.Salim H.O., Hamid H.K., Mekki S.O., Suleiman S.H., Ibrahim S.Z. Colorectal carcinoma associated with schistosomiasis: a possible causal relationship. World J Surg Oncol. 2010;8:68. doi: 10.1186/1477-7819-8-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.López de Cenarruzabeitia I., Landolfi S., Armengol Carrasco M. Intestinal schistosomiasis as unusual aetiology for acute appendicitis, nowadays a rising disease in Western countries. Case Rep Infect Dis. 2012;2012:896820. doi: 10.1155/2012/896820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Leder K, Weller PF. Diagnosis and treatment of schistosomiasis. Version 14.3UpToDate 2005. <http//:www.uptodate.com>.
- 47.Carneiro T.R., Pinheiro M.C., Oliveira S.M., Hanemann A.L., Queiroz J.A., Bezerra F.S. Increased detection of schistosomiasis with Kato-Katz and SWAP-IgG-ELISA in a Northeastern Brazil low-intensity transmission area. Rev Soc Bras Med Trop. 2012;45(4):510–513. doi: 10.1590/s0037-86822012000400019. [DOI] [PubMed] [Google Scholar]
- 48.Elliott D.E. Schistosomiasis. Pathophysiology, diagnosis, and treatment. Gastroenterol Clin North Am. 1996;25:599–625. doi: 10.1016/s0889-8553(05)70265-x. [DOI] [PubMed] [Google Scholar]
- 49.Wichmann D., Panning M., Quack T., Kramme S., Burchard G.D., Grevelding C. Diagnosing schistosomiasis by detection of cell-free parasite DNA in human plasma. PLoS Negl Trop Dis. 2009;3:e422. doi: 10.1371/journal.pntd.0000422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Deelder A.M., Qian Z.L., Kremsner P.G., Acosta L., Rabello A.L., Enyong P. Quantitative diagnosis of Schistosoma infections by measurement of circulating antigens in serum and urine. Trop GeogrMed. 1994;46:233–238. [PubMed] [Google Scholar]
- 51.Navaratnam A.M., Mutumba-Nakalembe M.J., Stothard J.R., Kabatereine N.B., Fenwick A., Sousa-Figueiredo J.C. Notes on the use of urine-CCA dipsticks for detection of intestinal schistosomiasis in preschool children. Trans R Soc Trop Med Hyg. 2012;106(10):619–622. doi: 10.1016/j.trstmh.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 52.Hussein H.M., El-Tonsy M.M., Tawfik R.A., Ahmed S.A. Experimental study for early diagnosis of prepatent schistosomiasis mansoni by detection of free circulating DNA in serum. Parasitol Res. 2012;111(1):475–478. doi: 10.1007/s00436-012-2822-0. [DOI] [PubMed] [Google Scholar]
- 53.Pontes L.A., Oliveira M.C., Katz N., Dias-Neto E., Rabello A. Comparison of a polymerase chain reaction and the Kato-Katz technique for diagnosing infection with Schistosoma mansoni. Am J Trop Med Hyg. 2003;68:652–656. [PubMed] [Google Scholar]
- 54.Shiff C. The importance of definitive diagnosis in chronic schistosomiasis, with reference to Schistosoma haematobium. J Parasitol Res. 2012;2012:761269. doi: 10.1155/2012/761269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gomes L.I., Marques L.H., Enk M.J., Coelho P.M., Rabello A. Further evaluation of an updated PCR assay for the detection of Schistosoma mansoni DNA in human stool samples. Mem Inst Oswaldo Cruz. 2009;104:1194–1196. doi: 10.1590/s0074-02762009000800021. [DOI] [PubMed] [Google Scholar]
- 56.Abdel-Wahab M.F., Esmat G., Farrag A., El-Boraey Y.A., Strickland G.T. Grading of hepatic schistosomiasis by the use of ultrasonography. Am J Trop Med Hyg. 1992;46:403–408. doi: 10.4269/ajtmh.1992.46.403. [DOI] [PubMed] [Google Scholar]
- 57.Pinto-Silva R.A., Queiroz L.C., Azeredo L.M., Silva L.C., Lambertucci J.R. Ultrasound in schistosomiasis mansoni. Mem Inst Oswaldo Cruz. 2010;105:479–484. doi: 10.1590/s0074-02762010000400021. [DOI] [PubMed] [Google Scholar]
- 58.Wilson S., Vennervald B.J., Dunne D.W. Chronic hepatosplenomegally in African school children: a common but neglected morbidity associated with schistosomiasis and malaria. PLoS Negl Trop Dis. 2011;5(8):e1149. doi: 10.1371/journal.pntd.0001149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Prichard R.K., Basáñez M.G., Boatin B.A., McCarthy J.S., García H.H., Yang G.J. A research agenda for Helminth diseases of humans: intervention for control and elimination. PLoS Negl Trop Dis. 2012;6(4):e1549. doi: 10.1371/journal.pntd.0001549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cioli D., Basso A., Valle C., Pica-Mattoccia L. Decades down the line: the viability of praziquantel for future schistosomiasis treatment. Expert Rev Anti Infect Ther. 2012;10(8):835–837. doi: 10.1586/eri.12.70. [DOI] [PubMed] [Google Scholar]
- 61.Navaratnam A.M., Sousa-Figueiredo J.C., Stothard J.R., Kabatereine N.B., Fenwick A., Mutumba-Nakalembe M.J. Efficacy of praziquantel syrup versus crushed praziquantel tablets in the treatment of intestinal schistosomiasis in Ugandan preschool children, with observation on compliance and safety. Trans R Soc Trop Med Hyg. 2012;106(7):400–407. doi: 10.1016/j.trstmh.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 62.Keiser J., Utzinger J. Antimalarials in the treatment of schistosomiasis. Curr Pharm Des. 2012;18(24):3531–3538. [PubMed] [Google Scholar]
- 63.Pavlin BI, Kozarsky P, Cetron MS. Acute pulmonary schistosomiasis in travelers: case report and review of the literature. Travel Med Infect Dis 2012 S pii: S1477-8939(12)00084-1. doi: http://dx.doi.org/10.1016/j.tmaid.2012.06.001. [DOI] [PubMed]
- 64.del Villar L.P., Burguillo F.J., López-Abán J., Muro A. Systematic review and meta-analysis of artemisinin based therapies for the treatment and prevention of schistosomiasis. PLoS One. 2012;7(9):e45867. doi: 10.1371/journal.pone.0045867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Deng W.C., Li J.X., Pan K., Kong G.Q., He Y.K., Li Y.S. Recommendation of a new clinical classification of advanced schistosomiasis. Zhongguo Xue Xi Chong Bing Fang Zhi Za Zhi. 2012;24(2):235–236. [PubMed] [Google Scholar]
- 66.Mahmoud A.A.F.M. Schistosomiasis. In: Pasvol G., Hoffman S., editors. Tropical medicine: science and practice. Imperial College Press; London: 2001. pp. 1–510. [Google Scholar]
- 67.De Franchis R. Evolving consensus in portal hypertension report of the baveno IV consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. 2005;43:167–176. doi: 10.1016/j.jhep.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 68.Hussein A.M., Medany S., Abou El-Magd A.M., Sherif S.M., Williams C.B. Multiple endoscopic polypectomies for schistosomal polyposis of the colon. Lancet. 1983;1:673–674. doi: 10.1016/s0140-6736(83)91969-4. [DOI] [PubMed] [Google Scholar]
- 69.Williams C.B., Hunt R.H., Loose H., Ridel R.H., Skai Y., Swarbrick E.T. Colonoscopy in the management of colon polyps. Br J Surg. 1974;61:673–682. doi: 10.1002/bjs.1800610902. [DOI] [PubMed] [Google Scholar]
- 70.Todd C.W., Colley D.G. Practical and ethical issues in the development of a vaccine against schistosomiasis mansoni. Am J Trop Med Hyg. 2002;66:348–358. doi: 10.4269/ajtmh.2002.66.348. [DOI] [PubMed] [Google Scholar]
- 71.McManus D.P., Loukas A. Current status of vaccines for schistosomiasis. Clin Microbiol Rev. 2008;21:225–242. doi: 10.1128/CMR.00046-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wilson R.A., Coulson P.S. Immune effector mechanisms against schistosomiasis: looking for a chink in the parasite’s armour. Trends Parasitol. 2009;25:423–431. doi: 10.1016/j.pt.2009.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tran M.H., Freitas T.C., Cooper L., Gaze S., Gatton M.L., Jones M.K. Suppression of mRNAs encoding tegument tetraspanins from Schistosoma mansoni results in impaired tegument turnover. PLoS Pathog. 2010;6:e1000840. doi: 10.1371/journal.ppat.1000840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pearson M.S., Pickering D.A., McSorley H.J., Bethony J.M., Tribolet L., Dougall A.M. Enhanced protective efficacy of a chimeric form of the schistosomiasis vaccine antigen Sm-TSP-2. PLoS Negl Trop Dis. 2012;6(3):e1564. doi: 10.1371/journal.pntd.0001564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ramos C.R., Spisni A., Oyama S., Jr., Sforça M.L., Ramos H.R., Vilar M.M. Stability improvement of the fatty acid binding protein Sm14 from S. mansoni by Cys replacement: structural and functional characterization of a vaccine candidate. Biochim Biophys Acta. 2009;1794:655–662. doi: 10.1016/j.bbapap.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 76.Da’dara A.A., Li Y.S., Xiong T., Zhou J., Williams G.M., McManus D.P. DNA-based vaccines protect against zoonotic schistosomiasis in water buffalo. Vaccine. 2008;26:3617–3625. doi: 10.1016/j.vaccine.2008.04.080. [DOI] [PMC free article] [PubMed] [Google Scholar]



