Abstract
Tension pneumocephalus is a rare but treatable neurosurgical emergency. Prompt and accurate diagnosis of tension pneumocephalus requires a high index of clinical suspicion corroborated by imaging. Herein, we describe a case of extensive tension pneumocephalus in a patient who had undergone transsphenoidal surgery and repair of the sellar floor, with subsequent successful decompression. This case report discusses the pertinent imaging features of tension pneumocephalus and its management.
Keywords: complication, sellar floor repair, tension pneumocephalus
INTRODUCTION
Postsurgical pneumocephalus is often observed in the clinical images of neurosurgical patients during the early postoperative period. The distinction of uncomplicated pneumocephalus from tension pneumocephalus is of vital clinical importance as the latter constitutes a neurosurgical emergency. Appreciation of the imaging features of tension pneumocephalus and a high index of suspicion are required to confidently arrive at an accurate diagnosis.
CASE REPORT
A 69-year-old man who had previously undergone a craniopharyngioma resection presented with signs and symptoms of meningitis. Computed tomography (CT) cisternography performed at another institution had shown a sellar floor defect, and this was repaired electively at that institution. The sellar floor repair was performed with the patient in a supine position. A combination of propofol and fentanyl was given for anaesthetic induction, and subsequent maintenance was achieved using desflurane. The fraction of inspired oxygen was maintained between 0.34 and 0.45, and no positive end expiratory pressure was set during or after the procedure. Postoperative care of the patient was also conducted in the supine position. Subsequent postsurgical CT evaluation showed minimal, expected pneumocephalus in the temporal horns and sellar region (Fig. 1). The patient’s recuperation was complicated by diabetes insipidus. However, after a brief stay in the intensive care unit, the electrolyte imbalance was corrected and steady improvement in the Glasgow Coma Score (GCS) was documented.
Fig. 1.
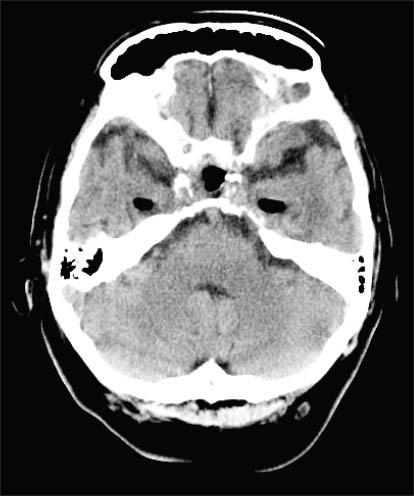
Unenhanced axial CT image through the pons (in soft tissue window) shows expected minimal free air within the sellar region and bilateral temporal horns. No subarachnoid air is visible.
On postoperative Day 6, the patient experienced spikes of fever and a worsening GCS, for which he received an empirical course of antibiotics. A sudden and further drop in the patient’s GCS two days later (from E3V1M5 to E1V2M5) prompted an emergency CT, which showed evidence of tension pneumocephalus, likely due to residual sellar floor defect. Extensive air collections with mass effect were noted in the bilateral subarchnoid spaces, and bilateral dilated frontal and temporal horns (Fig. 2). The patient underwent an emergency burr hole operation and the insertion of a Becker external drainage/monitoring system, with an EDM ventricular catheter (luminal diameter of 1.5 mm), at the right Kocher’s point, upon which air under pressure was detected. The air bubbled out when the dura was opened. The external ventricular catheter was kept in situ and the sellar floor was repaired. The patient’s GCS subsequently improved and postoperative CT imaging showed considerable reduction in the pneumocephalus with relieved mass effect (Fig. 3).
Fig. 2.
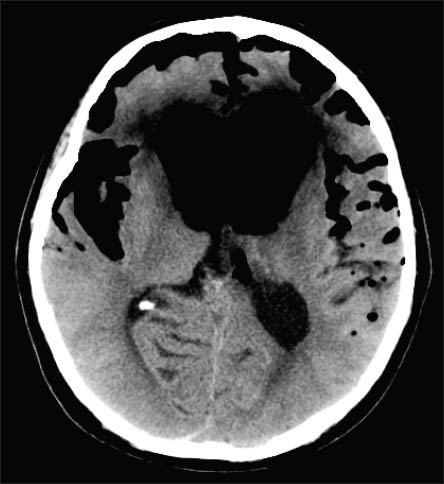
Unenhanced axial CT image through the lateral ventricles shows a large amount of free air in bilateral subarachnoid spaces and dilated, air-filled frontal horns exerting mass effect.
Fig. 3.

Unenhanced axial CT image through the lateral ventricles shows interval insertion of an extraventricular drain, with its tip in the right frontal horn. Considerable interim reduction in the bilateral subarachnoid free air and mass effect were appreciated.
DISCUSSION
Tension pneumocephalus is an indication of clinical deterioration due to increased intracranial pressure secondary to pneumocephalus.(1) It occurs when air that enters through a dural defect is unable to escape, akin to a ball-valve mechanism.(2) The initial presence of pneumocephalus and its subsequent gradual resolution after a craniotomy or craniectomy are universal.(3) The risk of tension pneumocephalus developing after the evacuation of a chronic subdural haematoma has been cited as 2.5%.(4)
Distinguishing tension pneumocephalus, a neurosurgical emergency, from the expected benign variety of postsurgical pneumocephalus is difficult. It can only be achieved with a high recording of intracranial pressure on intracranial measuring devices or a documented resonant air sprouting from the dura through a burr hole at the time of emergency reoperation.(4,5)
Tension pneumocephalus may manifest with a wide range of clinical presentations, including severe restlessness, deteriorating consciousness, focal neurological deficits, and even cardiac arrest.(6) The causes of tension pneumocephalus are also varied. Trauma, previous surgery, tumours of the paranasal sinuses and infections are some of the recognised causes.(1) In neurosurgical anaesthesia, nitrous oxide as an anaesthetic agent has been implicated in iatrogenic tension pneumocephalus. Nitrous oxide dissolves into the blood and enters the closed subdural space at a rate that is faster than the rate at which nitrogen is vented, thus increasing the amount of postsurgical pneumocephalus.(7,8) The use of hyperbaric oxygen treatment (HBOT) and continuous positive airway pressure (CPAP) ventilation have also been implicated in tension pneumocephalus.(9,10) In CPAP ventilation, a postulated mechanism of increased intrathoracic pressure with subsequent decreased venous return, leading to increased intracranial pressures, has been suggested.(10) With HBOT, however, the postulated mechanism is that air is sucked in through the dural defect due to the compression and consequent negative pressure within the cranium during therapy in the hyperbaric oxygen chamber; the negative pressure within the cranium results in the subsequent expansion of the intracranial air after decompression (i.e. after HBOT).(9) Detection of pneumocephalus with evidence of mass effect upon the underlying structures is the key feature in differentiating tension pneumocephalus from benign pneumocephalus. The radiological sign that is most widely reported as specific to tension pneumocephalus is the ‘Mount Fuji’ sign, which is observed when the presence of subdural free air causes the compression and separation of the frontal lobes.(2,4) The displaced frontal lobes and the widening of the interhemispheric fissure simulates the silhouette of Mount Fuji. Although this sign is specific in describing the mass effect of subdural air, a large volume of free air may also accumulate in other intracranial compartments (e.g. the intraventricular and subarchnoid spaces) and cause similar pressure effects, as was illustrated in the present case.
Management of tension pneumocephalus involves the urgent relief of the intracranial pressure. This is achieved with urgent neurosurgical interventions such as craniotomy, drilling of burr holes, needle aspiration, ventriculostomy placement and closure of the dural defects.
In conclusion, tension pneumocephalus is a neurosurgical emergency that requires prompt surgical intervention. The diagnosis of tension pneumocephalus requires a high index of suspicion and careful clinical correlation. Differentiating normal postneurosurgical benign pneumocephalus from tension pneumocephalus is critical for accurate diagnosis and successful management.
REFERENCES
- 1.Lin MB, Cheah FK, Ng SE, Yeo TT. Tension pneumocephalus and pneumorachis secondary to subarachnoid pleural fistula. Br J Radiol. 2000;73:325–7. doi: 10.1259/bjr.73.867.10817052. [DOI] [PubMed] [Google Scholar]
- 2.Michel SJ. The Mount Fuji sign. Radiology. 2004;232:449–50. doi: 10.1148/radiol.2322021556. [DOI] [PubMed] [Google Scholar]
- 3.Reasoner DK, Todd MM, Scamman FL, Warner DS. The incidence of pneumocephalus after supratentorial craniotomy. Observations on the disappearance of intracranial air. Anesthesiology. 1994;80:1008–12. doi: 10.1097/00000542-199405000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Ishiwata Y, Fujitsu K, Sekino T, et al. Subdural tension pneumocephalus following surgery for chronic subdural hematoma. J Neurosurg. 1988;68:58–61. doi: 10.3171/jns.1988.68.1.0058. [DOI] [PubMed] [Google Scholar]
- 5.Shaikh N, Masood I, Hanssens Y, Louon A, Hafiz A. Tension pneumocephalus as complication of burr-hole drainage of chronic subdural hematoma: A case report. Surg Neurol Int. 2010;6:1. doi: 10.4103/2152-7806.65185. pii: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Satapathy GC, Dash HH. Tension pneumocephalus after neurosurgery in the supine position. Br J Anaesth. 2000;84:115–7. doi: 10.1093/oxfordjournals.bja.a013368. [DOI] [PubMed] [Google Scholar]
- 7.Artru AA. Nitrous oxide plays a direct role in the development of tension pneumocephalus intraoperatively. Anesthesiology. 1982;57:59–61. doi: 10.1097/00000542-198207000-00019. [DOI] [PubMed] [Google Scholar]
- 8.Raggio JF, Fleischer AS, Sung YF, Hoffman JC. Expanding pneumocephalus due to nitrous oxide anesthesia: case report. Neurosurgery. 1979;4:261–3. doi: 10.1227/00006123-197903000-00014. [DOI] [PubMed] [Google Scholar]
- 9.Lee LC, Lieu FK, Chen YH, Hung TH, Chen SF. Tension pneumocephalus as a complication of hyperbaric oxygen therapy in a patient with chronic traumatic brain injury. Am J Phys Med Rehabil. 2012;91:528–32. doi: 10.1097/PHM.0b013e31824ad556. [DOI] [PubMed] [Google Scholar]
- 10.Klopfenstein CE, Forster A, Suter PM. Pneumocephalus. A complication of continuous positive airway pressure after trauma. Chest. 1980;78:656–7. doi: 10.1378/chest.78.4.656. [DOI] [PubMed] [Google Scholar]


