Abstract
Hypertension is the most common chronic condition seen in primary care. It is a potentially modifiable risk factor for cardiovascular and renal complications. The latest Joint National Committee recommendations in 2014 address common clinical questions from the best available science with regard to managing patients with hypertension. We review some of these recommendations and discuss how they may be applied in our practice.
Keywords: blood pressure, hypertension, Joint National Committee
Mr and Mrs Wolfgang had been recommended to your clinic for a second opinion concerning their blood pressure targets. The memo from your fellow family physician noted a trend of systolic blood pressure readings of 131–139 mmHg and diastolic blood pressure readings of 81–88 mmHg for both patients in the last four visits over the past 12 months. Mr Wolfgang had well-controlled diabetes mellitus, while Mrs Wolfgang did not have any chronic medical condition. The couple felt that their pressure readings were tolerable for people in their seventies and was not keen to start on any antihypertensive medications.
WHAT IS HYPERTENSION?
Hypertension, also known as high or raised blood pressure, is a global health issue with potential risk for long-term cardiovascular and renal complications.(1) Patients rarely experience symptoms in the early stages of hypertension and many go undiagnosed. The majority of patients with hypertension are treated by primary care physicians.
Blood pressure is measured in millimetres of mercury (mmHg) and recorded as the upper number or systolic (highest pressure in blood vessels when the heart squeezes) over the lower number or diastolic (lowest blood pressure in blood vessels when the heart relaxes). As there can be large spontaneous variations in blood pressure, hypertension is diagnosed based on multiple systolic blood pressure readings above 140 mmHg or diastolic blood pressure readings above 90 mmHg taken on several separate occasions.(2)
HOW RELEVANT IS THIS TO MY PRACTICE?
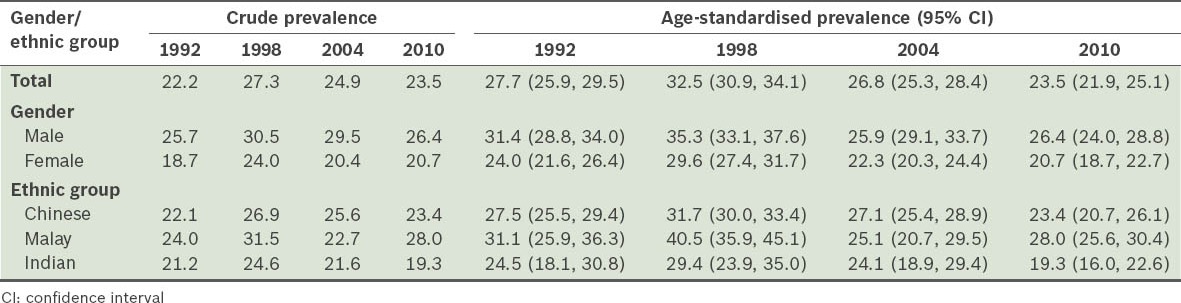
In Singapore, the 2010 National Health Survey showed a slight decrease in crude prevalence of hypertension, from 27.3% in 1998 to 24.9% in 2004 and 23.5% in 2010 (Table I).(3) In 2014, the Joint National Committee (JNC) published the latest guideline for high blood pressure management, providing a summary of the current available evidence-based recommendations for our practising reference, in the absence of any local guidelines (the withdrawn Ministry of Health clinical practice guidelines for hypertension was dated 2005).
Table I.
Prevalence (%) of hypertension by gender and ethnic group in 1992, 1998, 2004 and 2010.(3)
CLINICAL APPROACH TO HYPERTENSION
Differences in approach to the current available evidence between JNC 7 and JNC 8
The JNC 8(4) approached the medical literature with a limited number of questions judged to be of the highest priority and restricted the initial systematic review to only randomised controlled trials (Table II). The JNC 7, on the other hand, addressed multiple issues and reviewed a range of study designs.
Table II.
The nine key recommendations of Joint National Committee (JNC) 8.(4)

TAKE HOME MESSAGES
Hypertension, also known as high or raised blood pressure, is a global health issue with a potential risk for long-term cardiovascular and renal complications.
For adults aged < 60 years, hypertension medications should be recommended when systolic and diastolic blood pressures are > 140 mmHg and > 90 mmHg, respectively.
For adults aged ≥ 60 years, hypertension medications should be recommended when systolic and diastolic blood pressures are > 150 mmHg and > 90 mmHg, respectively.
For patients with diabetes mellitus, our latest local clinical guidelines state that target blood pressure is < 140/80 mmHG, while JNC 8 uses the threshold of < 140/90 mmHg, i.e. both guidelines agree on the target systolic blood pressure of < 140/80 mmHg, but differ slightly in the target diastolic blood pressure.
For patients with chronic kidney disease or diabetes mellitus (regardless of age), the target systolic and diastolic blood pressures should be < 140 mmHg and < 90 mmHg, respectively.
If the target blood pressure is not reached within a month of treatment, the dosage of the initial drug should be increased, or a second drug from one of the recommended classes should be added.
Our local clinical practice guidelines recommend an angiotensin-converting-enzyme inhibitor (ACEI) or angiotensin receptor blocker (ARB) to be included as part of the antihypertensive regimen for people with type 2 diabetes mellitus requiring pharmacotherapy for hypertension, unless it is not well tolerated.
It is not advisable to use an ACEI and ARB together in the same patient.
You explained to the patients the recent international review of clinical evidence and current local guidelines. The target blood pressure for Mr Wolfgang, who has uncomplicated diabetes mellitus, should be below 140/80 mmHg, while that for Mrs Wolfgang should be below 150/90 mmHg. As the trend of Mr Wolfgang’s diastolic blood pressure had been above 80 mmHg, he could benefit from starting on either an angiotensin-converting-enzyme inhibitor or angiotensin receptor blocker class of medication, according to our local guidelines. Mrs Wolfgang’s blood pressure is, however, tolerable for her age. You wrote a short memo to your colleague with reference to the recommendations of the Joint National Committee 8 and Ministry of Health Clinical Practice Guidelines on Diabetes Mellitus (March 2014).
REFERENCES
- 1.Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 3.Epidemiology and Disease Control Division, Ministry of Health, Singapore. National Health Survey 2010 Report [online] [Accessed August 1 2014]. Available at: http://www.moh.gov.sg/content/dam/moh_web/Publications/Reports/2011/NHS2010%20-%20low%20res.pdf .
- 4.James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311:507–20. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 5.Ministry of Health, Singapore. Clinical Practice Guidelines 1/2014 Diabetes Mellitus [online] [Accessed August 1, 2014]. Available at: http://www.moh.gov.sg/content/dam/moh_web/HPP/Doctors/cpg_medical/current/2014/diabetes_mellitus/cpg_Diabetes%20Mellitus%20Booklet%20-%20Mar%202014.pdf .


