Abstract
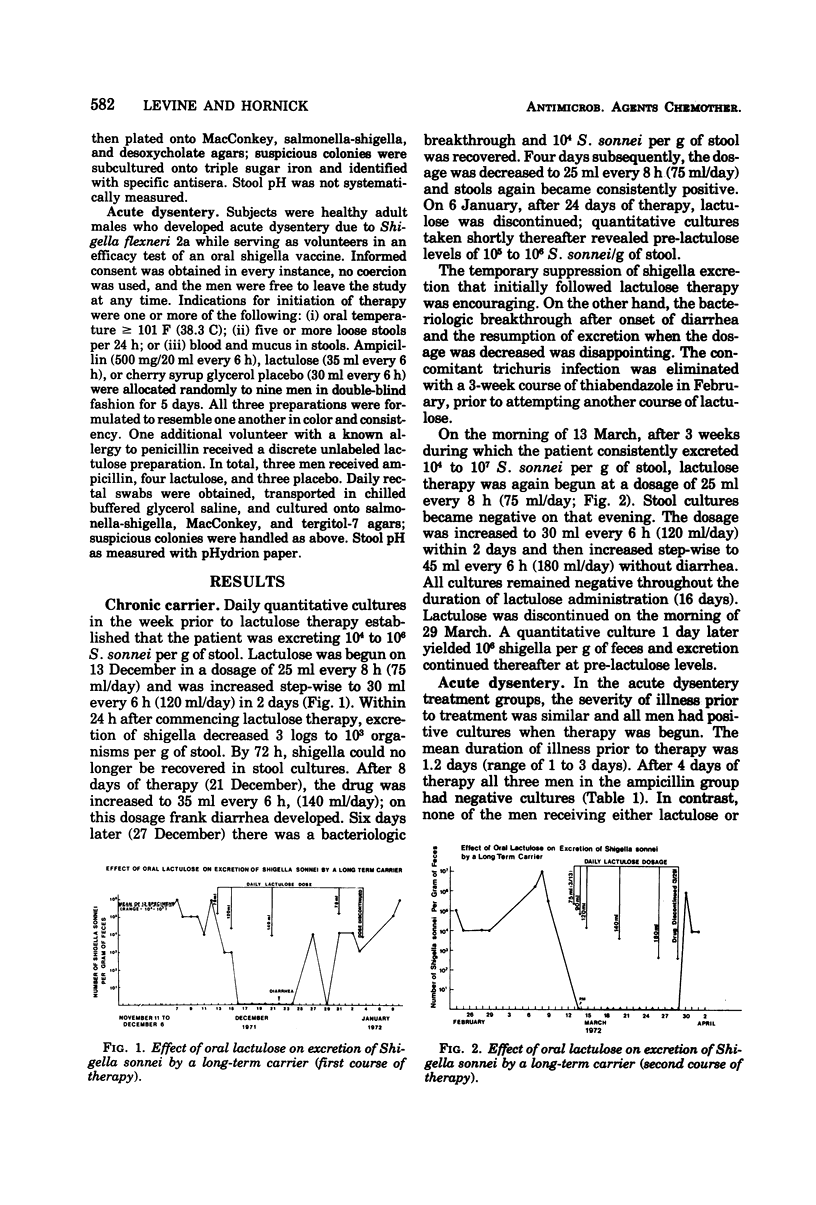
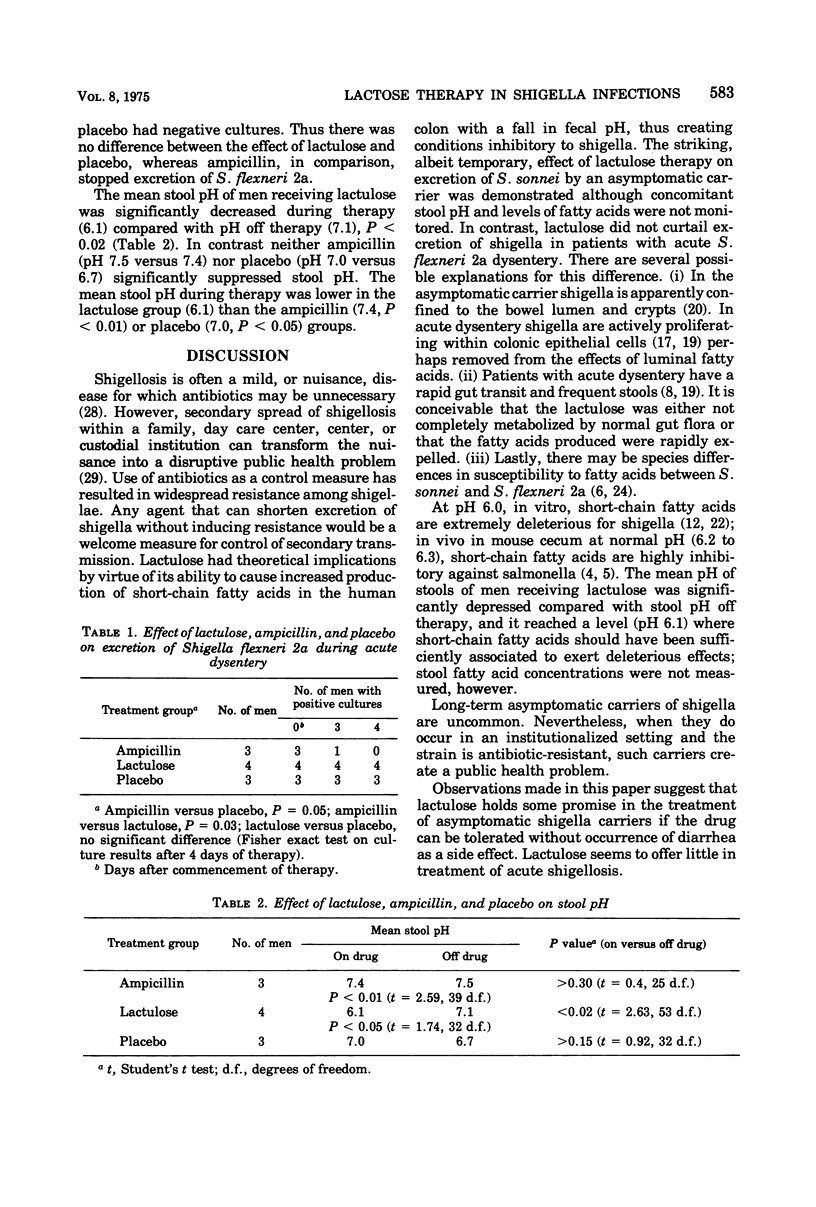
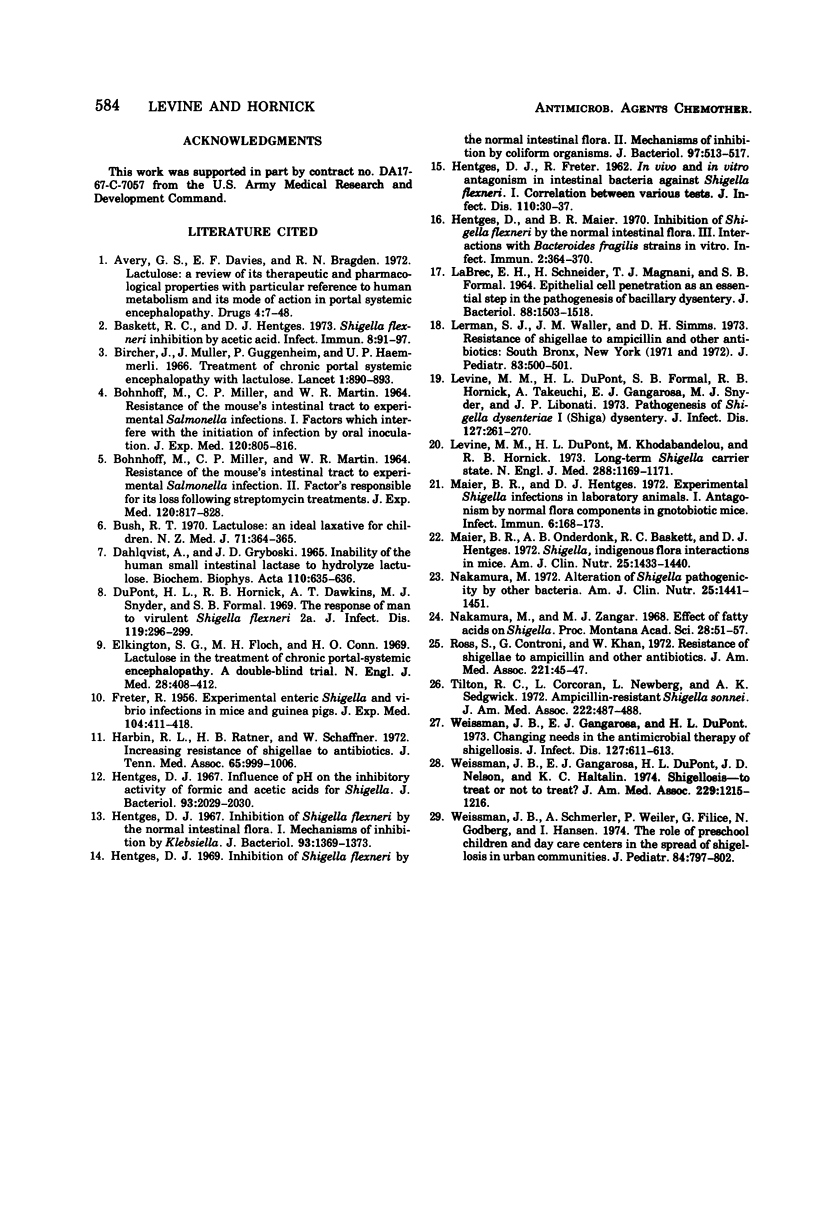
Antibiotic-resistant shigella are increasingly prevalent. Lactulose, a non-absorbable disaccharide, was investigated as an alternative therapy for shigella infection on the hypothesis that the short-chain fatty acids (inhibitory to shigella) resulting from metabolism of lactulose by normal colonic flora would diminish shigella excretion. A long-term antibiotic-refractory carrier (large bowel) excreting 104 to 107Shigella sonnei/g of feces was given two courses of lactulose (of 24 and 16 days duration). During lactulose therapy, excretion of shigella was greatly diminished (24-day course) or suppressed below detectable levels (16-day course), but returned to pretreatment levels upon discontinuation of lactulose. The volunteers who developed induced shigellosis during an efficacy test of oral Shigella flexneri 2a vaccine were randomly given oral ampicillin, lactulose, or placebo in double-blind fashion. Daily rectal cultures were taken. After 4 days of therapy, cultures were still positive in four out of four men on lactulose, three of three on placebo and none of three on ampicillin. Mean stool pH of men receiving lactulose (6.1) was significantly lower than those getting ampicillin (7.4), P < 0.01, or placebo (7.0), P < 0.05. Only in the lactulose group was mean stool pH during therapy significantly decreased compared with the level off therapy (6.1 versus 7.1), P < 0.02. Lactulose shows promise for the treatment of shigella carriers but appears ineffective in treatment of acute shigellosis.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Avery G. S., Davies E. F., Brogden R. N. Lactulose: a review of its therapeutic and pharmacological properties with particular reference to ammonia metabolism and its mode of action of portal systemic encephalopathy. Drugs. 1972;4(1):7–48. doi: 10.2165/00003495-197204010-00003. [DOI] [PubMed] [Google Scholar]
- BOHNHOFF M., MILLER C. P., MARTIN W. R. RESISTANCE OF THE MOUSE'S INTESTINAL TRACT TO EXPERIMENTAL SALMONELLA INFECTION. I. FACTORS WHICH INTERFERE WITH THE INITIATION OF INFECTION BY ORAL INOCULATION. J Exp Med. 1964 Nov 1;120:805–816. doi: 10.1084/jem.120.5.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BOHNHOFF M., MILLER C. P., MARTIN W. R. RESISTANCE OF THE MOUSE'S INTESTINAL TRACT TO EXPERIMENTAL SALMONELLA INFECTION. II. FACTORS RESPONSIBLE FOR ITS LOSS FOLLOWING STREPTOMYCIN TREATMENT. J Exp Med. 1964 Nov 1;120:817–828. doi: 10.1084/jem.120.5.817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baskett R. C., Hentges D. J. Shigella flexneri inhibition by acetic acid. Infect Immun. 1973 Jul;8(1):91–97. doi: 10.1128/iai.8.1.91-97.1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bircher J., Müller J., Guggenheim P., Haemmerli U. P. Treatment of chronic portal-systemic encephalopathy with lactulose. Lancet. 1966 Apr 23;1(7443):890–892. doi: 10.1016/s0140-6736(66)91573-x. [DOI] [PubMed] [Google Scholar]
- Bush R. T. Lactulose: an ideal laxative for children. N Z Med J. 1970 Jun;71(457):364–365. [PubMed] [Google Scholar]
- DuPont H. L., Hornick R. B., Dawkins A. T., Snyder M. J., Formal S. B. The response of man to virulent Shigella flexneri 2a. J Infect Dis. 1969 Mar;119(3):296–299. doi: 10.1093/infdis/119.3.296. [DOI] [PubMed] [Google Scholar]
- Elkington S. G., Floch M. H., Conn H. O. Lactulose in the treatment of chronic portal-systemic encephalopathy. A double-blind clinical trial. N Engl J Med. 1969 Aug 21;281(8):408–412. doi: 10.1056/NEJM196908212810803. [DOI] [PubMed] [Google Scholar]
- FRETER R. Experimental enteric Shigella and Vibrio infections in mice and guinea pigs. J Exp Med. 1956 Sep 1;104(3):411–418. doi: 10.1084/jem.104.3.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HENTGES D. J., FRETER R. In vivo and in vitro antagonism of intestinal bacteria against Shigella flexneri. I. Correlation between various tests. J Infect Dis. 1962 Jan-Feb;110:30–37. doi: 10.1093/infdis/110.1.30. [DOI] [PubMed] [Google Scholar]
- Harbin R. L., Ratner H. B., Schaffner W. Topics in infectious diseases. Increasing resistance of Shigellae to antibiotics. J Tenn Med Assoc. 1972 Nov;65(11):999–1000. [PubMed] [Google Scholar]
- Hentges D. J. Influence of pH on the inhibitory activity of formic and acetic acids for Shigella. J Bacteriol. 1967 Jun;93(6):2029–2030. doi: 10.1128/jb.93.6.2029-2030.1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hentges D. J. Inhibition of Shigella flexneri by the normal intestinal flora. I. Mechanisms of inhibition by Klebsiella. J Bacteriol. 1967 Apr;93(4):1369–1373. doi: 10.1128/jb.93.4.1369-1373.1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hentges D. J. Inhibition of Shigella flexneri by the normal intestinal flora. II. Mechanisms of inhibition by coliform organisms. J Bacteriol. 1969 Feb;97(2):513–517. doi: 10.1128/jb.97.2.513-517.1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hentges D. J., Maier B. R. Inhibition of Shigella flexneri by the Normal Intestinal Flora III. Interactions with Bacteroides fragilis Strains in Vitro. Infect Immun. 1970 Oct;2(4):364–370. doi: 10.1128/iai.2.4.364-370.1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labrec E. H., Schneider H., Magnani T. J., Formal S. B. EPITHELIAL CELL PENETRATION AS AN ESSENTIAL STEP IN THE PATHOGENESIS OF BACILLARY DYSENTERY. J Bacteriol. 1964 Nov;88(5):1503–1518. doi: 10.1128/jb.88.5.1503-1518.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lerman S. J., Waller J. M., Simms D. H. Resistance of shigellae to ampicillin and other antibiotics: South Bronx New York (1971 and 1972). J Pediatr. 1973 Sep;83(3):500–501. doi: 10.1016/s0022-3476(73)80286-0. [DOI] [PubMed] [Google Scholar]
- Levine M. M., DuPont H. L., Formal S. B., Hornick R. B., Takeuchi A., Gangarosa E. J., Snyder M. J., Libonati J. P. Pathogenesis of Shigella dysenteriae 1 (Shiga) dysentery. J Infect Dis. 1973 Mar;127(3):261–270. doi: 10.1093/infdis/127.3.261. [DOI] [PubMed] [Google Scholar]
- Levine M. M., DuPont H. L., Khodabandelou M., Hornick R. B. Long-term Shigella-carrier state. N Engl J Med. 1973 May 31;288(22):1169–1171. doi: 10.1056/NEJM197305312882207. [DOI] [PubMed] [Google Scholar]
- Maier B. R., Hentges D. J. Experimental Shigella infections in laboratory animals. I. Antagonism by human normal flora components in gnotobiotic mice. Infect Immun. 1972 Aug;6(2):168–173. doi: 10.1128/iai.6.2.168-173.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maier B. R., Onderdonk A. B., Baskett R. C., Hentges D. J. Shigella, indigenous flora interactions in mice. Am J Clin Nutr. 1972 Dec;25(12):1433–1440. doi: 10.1093/ajcn/25.12.1433. [DOI] [PubMed] [Google Scholar]
- Nakamura M. Alteration of Shigella pathogenicity by other bacteria. Am J Clin Nutr. 1972 Dec;25(12):1441–1451. doi: 10.1093/ajcn/25.12.1441. [DOI] [PubMed] [Google Scholar]
- Ross S., Controni G., Khan W. Resistance of shigellae to ampicillin and other antibiotics. Its clinical and epidemiological implications. JAMA. 1972 Jul 3;221(1):45–47. [PubMed] [Google Scholar]
- Tilton R. C., Corcoran L., Newberg L., Sedgwick A. K. Ampicillin-resistant Shigella sonnei. JAMA. 1972 Oct;222(4):487–488. [PubMed] [Google Scholar]
- Weissman J. B., Gangarosa E. J., Dupont H. L., Nelson J. D., Haltalin K. C. Shigellosis. To treat or not to treat? JAMA. 1974 Aug 26;229(9):1215–1216. doi: 10.1001/jama.229.9.1215. [DOI] [PubMed] [Google Scholar]
- Weissman J. B., Schmerler A., Weiler P., Filice G., Godbey N., Hansen I. The role of preschool children and day-care centers in the spread of shigellosis in urban communities. J Pediatr. 1974 Jun;84(6):797–802. doi: 10.1016/s0022-3476(74)80750-x. [DOI] [PubMed] [Google Scholar]
- Weissman J. P., Gangarosa E. J., Dupont H. L. Changing needs in the antimicrobial therapy of shigellosis. J Infect Dis. 1973 May;127(5):611–613. doi: 10.1093/infdis/127.5.611. [DOI] [PubMed] [Google Scholar]



