Abstract
FLAIR vascular hyperintensities (FVH) are frequently encountered in acute ischemic stroke. We report two cases presenting with transient ischemic attack (TIA) with isolated FVH on MRI who went on to have a stroke during hospitalization. Isolated FVH may be an important imaging correlate in acute ischemia, and may suggest proximal occlusion with the presence of slow flow through retrograde leptomeningeal collaterals. Recognition of these subtle correlates may complement clinical predictors of stroke after TIA.
Keywords: FLAIR, MRI, collateral, TIA, stroke
Introduction
The risk of stroke is especially high soon after TIA,(1). FLAIR (FLuid-Attenuated Inversion Recovery) vascular hyperintensities (FVH) are serpentine or linear hyperintensities, best visualized within the Sylvian fissure ipsilateral to acute ischemic stroke. Studies have correlated the presence of FVH with perfusion abnormalities(2), slow flow(3) and presence of leptomeningeal collateral flow.(4) Thus FVH may be of clinical significance in predicting stroke in the setting of TIA, especially when MR-angiography is unavailable or degraded by motion. We present two cases in which FVH were present on MRI in patients experiencing TIA who went on to have ischemic stroke.
Case Report
Case 1
A 79-year-old right-handed woman with a history of Parkinson's disease and multiple vascular risk factors was admitted for workup of an episode of slurred speech, and left-sided weakness lasting approximately 20 minutes with return to baseline.
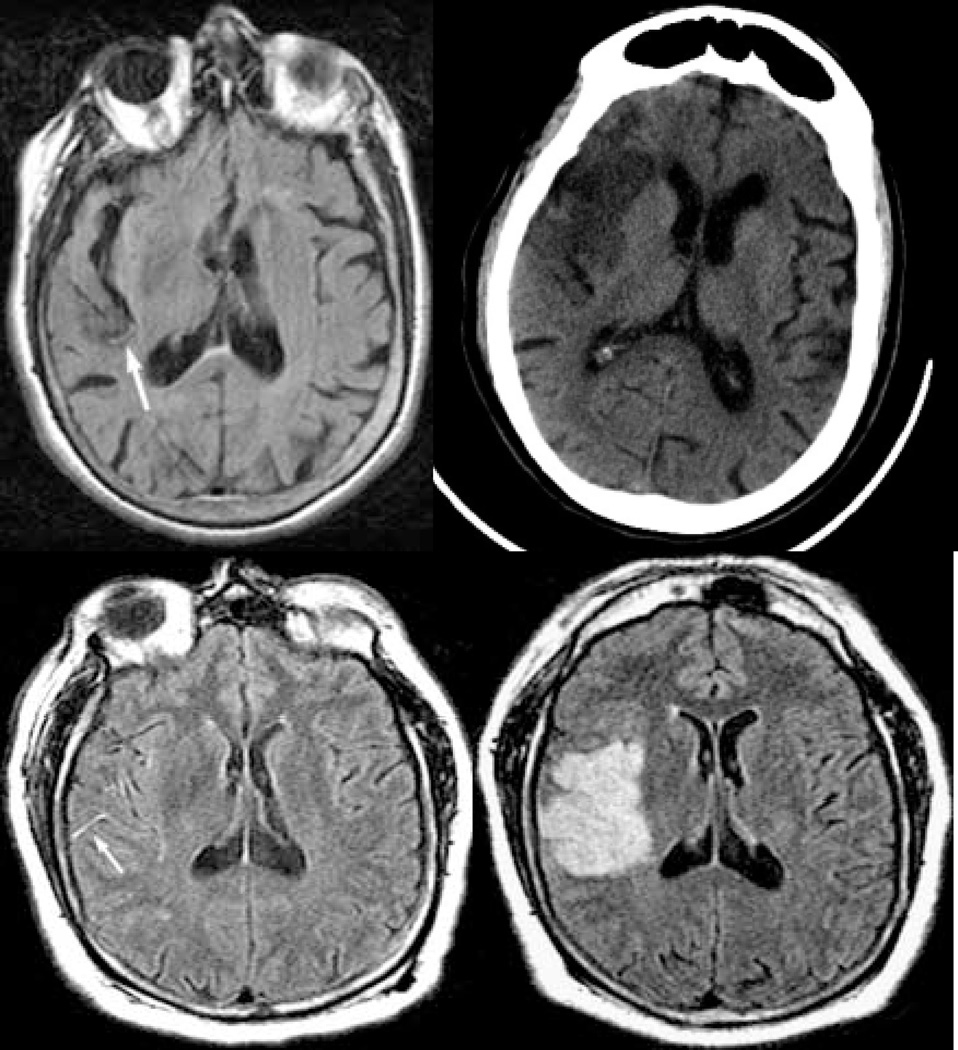
In the emergency room she was evaluated with an MRI study of the brain. There was no evidence of restriction of diffusion to suggest acute ischemic stroke. The FLAIR images demonstrated hyperintensity within the right middle cerebral artery (MCA) distribution (figure 1A). The MR-angiogram was degraded by motion and not interpretable. Further evaluation and consideration of thrombolysis was not undertaken as the patient was clinically asymptomatic. The patient was admitted for observation and further workup.
Figure 1.
Initial FLAIR image of case 1 (A) demonstrating vascular hyperintensity (arrow) in the right MCA and follow-up follow-up CT (B) scan performed 48 hours after presentation. Initial FLAIR image of case 2 (C) at presentation demonstrating FVH in the right Sylvian fissure (arrow) and follow-up FLAIR performed two days after admission (D) demonstrating infarction in the right middle cerebral artery distribution.
At 24 hours after her initial presentation, however, she again acutely developed significant left-sided weakness and a left facial droop. Emergent MRI of the brain at that time revealed acute infarction involving the right inferior frontal lobe corresponding to the MCA territory. MRA demonstrated concomitant occlusion of the proximal right MCA. Continuous cardiac monitoring subsequently revealed atrial fibrillation as the underlying etiology of her stroke. Follow-up CT at 48 hours from admission demonstrated hypodensity consistent with infarction in the right frontal region (Figure 1B).
Case 2
A 48-year-old man was admitted to the internal medicine service following a motor vehicle accident. At the time of initial evaluation in the emergency room he reported transient left-sided sensory loss and weakness lasting 10 minutes in duration. Neurological examination was unrevealing and an MRI of the brain with DWI sequences was reported as unremarkable. No angiographic sequences were obtained with the MRI as cerebral ischemia was not under consideration by the trauma service.
He remained asymptomatic for 36 hours after admission before developing acute leftsided hemiparesis and hemisensory loss. Detailed review of his prior MRI showed no evidence of parenchymal injury, yet isolated FVH were evident in the right Sylvian fissure (figure 1C). A repeat MRI obtained after his recurrent event revealed acute infarction in the territory of the right MCA (figure 1D).
Discussion
These two cases presented to medical attention with transient neurological deficits and were observed to be symptom-free for many hours after their initial events. In both cases, the subsequent strokes manifested identical neurological symptoms with respect to the heralding TIA. The presence of FVH on initial MRI may have been a clue to persistent large-vessel stenosis/occlusion and the possibility of subsequent stroke. In both cases MRA was unavailable to document presence or absence of large-vessel stenosis or occlusion.
The neuroimaging marker of FLAIR vascular hyperintensity has been referred to as hyperintense vessel sign on FLAIR,(5, 6) and early MR imaging vessel sign,(7) in previous publications. The pathophysiologic substrate of FVH has been debated, although many studies have related this finding to slow flow.(3, 6, 8) Of note, studies have found 70% sensitivity and 100% specificity of FVH in relationship to large vessel occlusion (LVO).(8) Another study noted FVH in only 10% of all patients presenting with acute stroke, yet in over 90% of cases presenting with large vessel occlusion or severe stenosis.(6) FVH was found to be more common in symptomatic patients with multiple intracerebral stenoses than in asymptomatic patients without stenosis.(5)
Patients presenting with transient neurological symptoms with evidence of LVO on MRA are at a higher risk of subsequent stroke.(9) Although the overall 90-day risk for recurrent stroke after TIA has been estimated at 11.7%, it may be as high as 32.6% in the setting of LVO. Compared with other stroke subtypes, patients with stroke due to LVO or stenosis are also three times as likely to have recurrence at 7 days. FVH may be a surrogate marker of persistent LVO and thus have predictive value for stroke after TIA.
FVH may be an important neuroimaging marker and clinicians as well as radiologists should be trained to look for their presence. The finding of FVH in patients with TIA may be associated with subsequent ischemic stroke in the corresponding vascular distribution or arterial territory. Prospective studies are warranted to systematically evaluate the relative incidence of FVH in patients presenting with TIA and the association of FVH with early subsequent stroke. Presence of FVH may be especially important in instances where MRA or perfusion MRI is unavailable or degraded by artifact.
Acknowledgments
Acknowledgements and other support: none
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Johnston SC, Gress DR, Browner WS, Sidney S. Short-term Prognosis After Emergency Department Diagnosis of TIA. JAMA. 2000;284(22):2901–2906. doi: 10.1001/jama.284.22.2901. [DOI] [PubMed] [Google Scholar]
- 2.Liebeskind DS, Cucchiara BL, Kasner SE, et al. FLAIR MRI vascular hyperintensity reflects perfusion status in cerebral ischemia. Presented at the 53rd Annual Meeting of the American Academy of Neurology; Philadelphia, PA. 2001. [Google Scholar]
- 3.Sanossian N, Saver JL, Alger JR, et al. Angiography reveals that FLAIR Vascular Hyperintensities are due to Slow Flow, Not Thrombus (Abs.) Stroke. 2006;37(2):651. doi: 10.3174/ajnr.A1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liebeskind DS, Bemporad JA, Melhem ER. FLAIR vascular hyperintensity as a marker of leptomeningeal collaterals in subacute stroke. Presented at the ASNR 41st Annual Meeting; Washington, D.C.. 2003. [Google Scholar]
- 5.Iancu-Gontard D, Oppenheim C, Touze E, et al. Evaluation of Hyperintense Vessels on FLAIR MRI for the Diagnosis of Multiple Intracerebral Arterial Stenoses. Stroke. 2003;34(8):1886–1891. doi: 10.1161/01.STR.0000080382.61984.FE. [DOI] [PubMed] [Google Scholar]
- 6.Kamran S, Bates V, Bakshi R, et al. Significance of hyperintense vessels on FLAIR MRI in acute stroke. Neurology. 2000;55(2):265–269. doi: 10.1212/wnl.55.2.265. [DOI] [PubMed] [Google Scholar]
- 7.Schellinger PD, Chalela JA, Kang D-W, Latour LL, Warach S. Diagnostic and Prognostic Value of Early MR Imaging Vessel Signs in Hyperacute Stroke Patients Imaged <3 Hours and Treated with Recombinant Tissue Plasminogen Activator. Am J Neuroradiol. 2005;26(3):618–624. [PMC free article] [PubMed] [Google Scholar]
- 8.Schellinger PD, Chalela JA, Kang D-W, Latour LL, Warach S. Diagnostic and Prognostic Value of Early MR Imaging Vessel Signs in Hyperacute Stroke Patients Imaged <3 Hours and Treated with Recombinant Tissue Plasminogen Activator. AJNR Am J Neuroradiol. 2005;26(3):618–624. [PMC free article] [PubMed] [Google Scholar]
- 9.Coutts SB, Simon JE, Eliasziw M, et al. Triaging transient ischemic attack and minor stroke patients using acute magnetic resonance imaging. Annals of Neurology. 2005;57(6):848–854. doi: 10.1002/ana.20497. [DOI] [PubMed] [Google Scholar]