Summary
Background
Cystic thymoma is a rare variant of thymic neoplasm characterized by almost complete cystic degeneration with mixed internal structure. We describe a case of a 60 year-old woman with a cystic thymoma studied with advanced tomographic imaging stydies.
CT, MRI and PET/CT with 18F-FDG were performed; volumetric CT and MRI images provided better anatomic evaluation for pre-operative assessment, while PET/CT was helpful for lesion characterization based on 18F-FDG uptake. Although imaging studies are mandatory for pre-operative evaluation of cystic thymoma, final diagnosis still remains surgical.
Case Report
A 60-year-old woman with recent chest pain and no history of previous disease was admitted to our departement to investigate the result of a previous chest X-ray that showed bilateral mediastinal enlargement; for this purpose, enhanced chest CT scan was performed using a 64-rows scanner (Toshiba, Aquilion 64, Japan) before and after intravenous bolus administration of iodinated non ionic contrast agent; CT images demonstrated the presence of a large mediastinal mass (11×8 cm) located in the anterior mediastinum who extended from the anonymous vein to the cardio-phrenic space, compressing the left atrium and causing medium lobe atelectasis; bilateral pleural effusion was also present.
Conclusions
In conclusion, correlative imaging plays a foundamental role for the diagnostic evaluation of patient with cystic thymoma. In particular, volumetric CT and MRI studies can provide better anatomic informations regarding internal structure and local tumor spread for pre-operative assessment. Conversely, metabolic imaging using 18F-FDG PET/CT is helpful for lesion characterization differentiating benign from malignant lesion on the basis of intense tracer uptake. The role of PET/MRI is still under investigation. However, final diagnosis still remains surgical even though imaging studies are mandatory for pre-operative patient management.
MeSH Keywords: Magnetic Resonance Imaging, Mediastinal Diseases, Multidetector Computed Tomography, Positron-Emission Tomography, Thymoma
Background
Thymic neoplasms constitute less than 1% of all tumors in adults; the most common epithelial thymic neoplasms are thymoma and thymic carcinoma. Nearly all thymomas occur in adults after physiological thymic involution at the age ranging from 40 to 60 years [1]. Most thymomas are solid chest masses that are encapsulated and located in the anterior mediastinum. Approximately one-third of these lesions exhibit necrosis, hemorrhage or cystic components, and similarly one-third of cases show local regional tumor spread, infiltrating the capsule and surrounding anatomical structures [2]. Thus, cystic thymoma is a rare variant of thymic neoplasm and, although cystic regions are present in up to 40% of thymomas, those that are nearly entirely cystic are very rare [3].
About half of the patients suffering from thymic neoplasm are asymptomatic, while the remaining 50% may present thoracic symptoms, such as dyspnea or chest pain; patients with thymoma are often affected by miastenia gravis. Diagnostic imaging techniques are mandatory to assess patients with thymoma; in particular, tomographic studies are requested to evaluate tumor spread into the mediastinum; among these imaging studies, Computed Tomography (CT), Magnetic Resonance Imaging (MRI) and Positron Emission Tomography (PET) represent the state of art for the diagnostic evaluation of such tumor lesions.
In this report, we described a patient with cystic thymoma in whom the results of imaging studies were mainly suggestive of a cystic tumor mass but with capsular partially solid component; thus, imaging findings were suspicious of malignant tumor.
Case Report
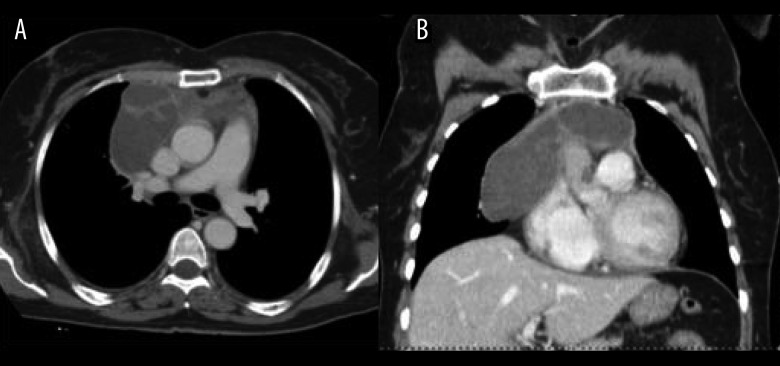
A 60-year-old woman with a recent chest pain and no history of any disease was admitted to our department to follow up the results of a previous chest X-ray that showed bilateral mediastinal enlargement. For that purpose, enhanced chest CT scan was performed using a 64-row scanner (Toshiba, Aquilion 64, Japan) before and after intravenous bolus administration of iodinated non-ionic contrast agent; CT images demonstrated the presence of a large mediastinal mass (11×8 cm) located in the anterior mediastinum which extended from the anonymous vein to the cardiophrenic space, compressing the left atrium and causing medium lobe atelectasis. Bilateral pleural effusion was also present. The lesion was characterized by fluid density, regular margins and internal septa in the upper portion; after contrast injection, only the walls, septa and a capsular nodule showed a significant enhancement (Figure 1).
Figure 1.
Axial (A) and coronal (B) reformatted CT images obtained after after intravenous contrast agent administration showed a fluid-like mass with multiple enhancing internal septa. Of note, a capsular solid nodule is detectable in the middle of the tumor mass.
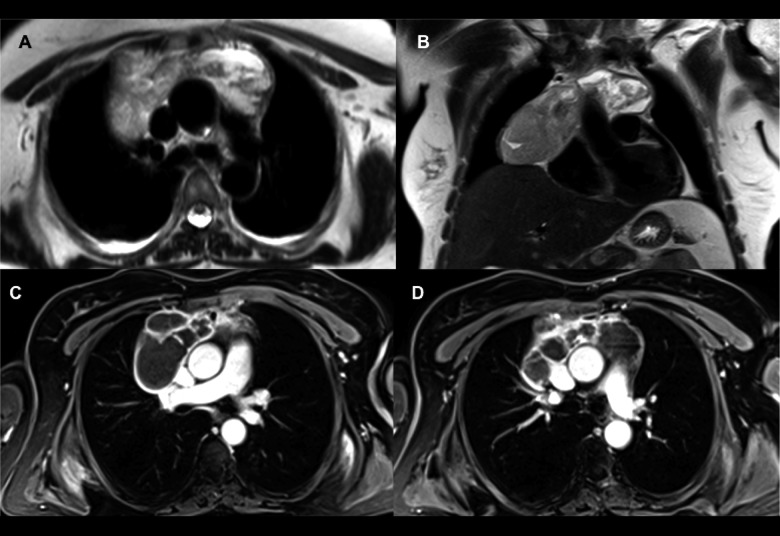
To better characterize the structure of the lesion and to formulate a diagnostic hypothesis, chest MRI with contrast administration was also performed using a 1.5 T MR device (Philips, Achieva, Netherlands) before and after intravenous administration of gadopentetate dimeglumine (120 cc); MRI images confirmed the presence of a voluminous plurilobate cystic mass (14×4.5×7 cm), hypointense on T1 sequence and hyperintense on T2 sequence, with regular margins located in the antero-superior mediastinum (Figure 2). Internal septa appeared slightly irregular with small contextual nodules and showed intense increased signal intensity after gadolinium injection; in particular, intense septal vascularization in the antero-medial portion of the mass was depicted. The patient underwent also a 18F-FDG PET/CT scan. The 18F-FDG PET/CT images were obtained using a combined PET/CT Discovery LS scanner (GE Healthcare). The PET/CT images showed 18F-FDG uptake in the capsular portion of the mass (SUV max 2) and focal intense tracer uptake (SUV max 5.7) was clearly detected in the middle of the lesion (Figure 3). For tumor diagnosis, fine-needle aspiration biopsy was performed.
Figure 2.
T2 TSE axial (A) and coronal (B) MR images: the mass is hyperintense compared to muscular tissues but presents multiple internal septa. T1 VIBE axial MR images after after intravenous contrast agent administration (C, D): the mass shows clear internal fluid content with a significant enhancement of walls and septa, particularly in the anterior portion.
Figure 3.
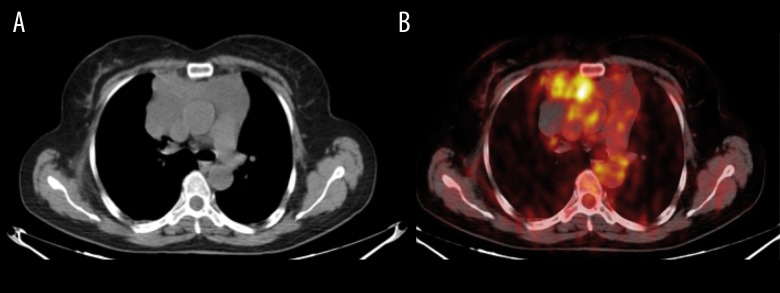
(A, B) Axial 18F-FDG PET/CT shows tracer uptake in the capsular portion of the mass (SUV max 2) and focal intense uptake (SUV max 5.7) was clearly detected in the middle of the lesion.
The biopsy specimen included fibroadipose tissue and a large necrotic component with an internal lymphoid population; the finding was not conclusive because of large necrosis but all findings were suggestive of T-cell lymphoproliferative disease with possible lymphoblastic nature. So that, a new immunohistochemical analysis was performed and, despite the necrotic component, diagnostic hypotesis of thymoma was made because of the presence of a large T TDT+ cell population. Thus, the patient received a course of steroid therapy and then a post-therapeutic CT scan was performed. CT images demonstrated a significant size reduction of the mass with no detectable cardiac or pulmonary compression and no pleural effusion (Figure 4). Five months after the first clinical investigation, the patient underwent surgical resection of the mass. Hystological analysis revealed a B1 thymoma, stage I, according to the Masaoka-Koga classification.
Figure 4.
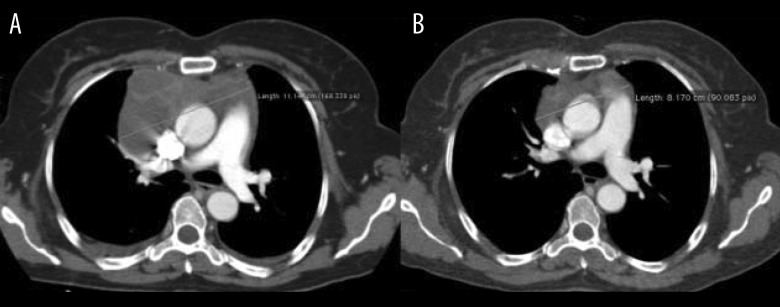
Axial CT images at the level of the pulmonary artery bifurcation obtained after after intravenous contrast agent administration before (A) and after (B) a cicle of steroid therapy: there is a significant size reduction of the mass suggestive of disease regression.
Discussion
Thymoma is the most common primary anterior mediastinal tumor, with an overall incidence of 0.13 cases per 100,000 person years [4]. Many tumors, including thymomas, may present cystic degeneration developing mixed structure with solid and cystic components and, when degeneration is extensive, they may be almost entirely cystic [5]. About 40% of thymomas can undergo cystic degeneration. This secondary event may vary from inconspicuous spaces that contain clear fluid to occasional larger cavities that are occupied by blood or yellow-brown grumose material. Occasionally cystic changes result in a unilocular or multilocular cystic mass that has only a few recognizable small tumor nodules attached to its walls [6].
In this report, we described a patient with an anterior mediastinal mass that appeared almost entirely cystic with multiple internal septa but regular margins on both CT and MRI; those findings were suggestive of a benign cystic mediastinal mass, such as cystic lymphangioma, even if the internal septa with intense contrast enhancement were suspicious for other type of lesions. For that reason, 18F-FDG PET/CT scan was performed showing abnormal tracer uptake suggestive of a partially solid component. The histopathology demonstrated cystic thymoma.
CT is a routine imaging modality for evaluating thymomas being homogeneous solid masses with soft tissue attenuation and well-demarcated margins [7]. However, large thymomas may also have areas of cystic or necrotic degeneration. On MRI, thymoma appears as homogeneous or heterogeneous mass with low signal intensity on T1-weighted images and high signal intensity on T2-weighted images; cystic thymoma, instead, is mostly fluid, due to internal necrosis and cystic degeneration, with solid intramural nodules; foci of hemorrhage can also be present [2]. The 18F-FDG PET can be useful in case of overlapping findings at CT or MRI, providing metabolic information; it may also have predictive significance for patient’s prognosis depending on the degree of 18F-FDG uptake.
When an anterior mediastinal mass is detected, the diagnosis of thymoma must always be formulated as the most probable one, but in our patient the large area of tumor mass necrosis was misinterpreted as fluid, and the presence of small mural nodules on CT and MRI suggested to further investigate the lesion for tissue characterization. For that purpose, 18F-FDG PET/CT was performed and showed a significant tracer uptake in the middle cranial portion of the mass, corresponding to capsular profile, mural nodules and internal septa. That finding clearly suggested a malignant lesional nature; in fact, pathological specimen after surgical resection presented as cystic thymoma.
According to the diagnostic imaging protocol, to investigate a suspected thymoma, volumetric CT and MRI with multiplanar tridimentional reconstruction are useful in evaluating the morphological appearance of mediastinal masses. However, imaging findings may be insufficient for appropriate lesion characterization. In fact, cystic thymoma should be differentiated from other cystic mediastinal masses, such as cystic lymphangioma, cystic theratoma, that may also present a more complex internal structure with multiple septa, and from simple cystic masses such as congenital, thymic and pericardial cysts [8]. Hydatid cyst and chronic ematoma may be discriminated from cystic thymoma owing to, respectively: the presence of mural calcifications, better depicted on CT, and internal hyperdensity or variable signal intensity on CT or MRI. Moreover, the 18F-FDG PET/CT can be very helpful in evaluating metabolic activity in such degenerated malignant mediastinal lesions that may often appear as cystic. In our case, 18F-FDG PET/CT evaluation ultimately suggested the malignant nature of the mass, due to the presence of internal septa, capsular profile and mural nodule showing increased abnormal tracer uptake. As reported in literature, 18F-FDG PET/CT is effective for estimating histopathological malignancy and staging of thymic epithelial tumors and may be an important imaging test with high relevance to patient’s prognosis depending on the degree of 18F-FDG uptake [9]. However, SUVmax cut off for differentiating between low- and high-risk thymoma is still not well defined, ranging approximately from 4.5 to 6.3 with different sensitivity and specificity values [10]. In our case, a SUV max of 5.7 detected in the middle of the lesion corresponded to a low-grade thymoma demonstrated by pathology. In such patients, MRI/PET could also be useful, providing higher soft-tissue contrast than CT, assessing additional parameters as tumor vascularization and, with Diffusion Weighted Imaging (DWI), giving important information on tumor biology [11,12].
Conclusions
In conclusion, correlative imaging plays a fundamental role in the diagnostic evaluation of patients with cystic thymoma. In particular, volumetric CT and MRI studies can provide better anatomic informations regarding the internal structure and local tumor spread for pre-operative assessment. Conversely, metabolic imaging using 18F-FDG PET/CT is helpful for lesion characterization differentiating benign from malignant lesions on the basis of intense tracer uptake. The role of PET/MRI is still under investigation. However, the final diagnosis still remains surgical even though imaging studies are mandatory for pre-operative patient management.
References
- 1.Raad RA, Suh J, Ko JP. Case of the season: cystic thymoma. Semin Roentgenol. 2013;48(4):290–94. doi: 10.1053/j.ro.2013.03.016. [DOI] [PubMed] [Google Scholar]
- 2.Benveniste MF, Rosado-de-Christenson ML, Sabloff BS. Role of imaging in the diagnosis, staging, and treatment of thymoma. Radiographics. 2011;31(7):1847–61. doi: 10.1148/rg.317115505. discussion 1861–63. [DOI] [PubMed] [Google Scholar]
- 3.Takahashi K, Al-Janabi NJ. Computed tomography and magnetic resonance imaging of mediastinal tumors. J Magn reson Imaging. 2010;32(6):1325–39. doi: 10.1002/jmri.22377. [DOI] [PubMed] [Google Scholar]
- 4.Engels EA. Epidemiology of thymoma and associated malignancies. J Thorac Oncol. 2010;5:S260–65. doi: 10.1097/JTO.0b013e3181f1f62d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Suster S, Rosai J. Cystic thymomas: a clinicopathologic study of ten cases. Cancer. 1992;69:92–97. doi: 10.1002/1097-0142(19920101)69:1<92::aid-cncr2820690117>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 6.Jeung MY, Gasser B, Gangi A. Imaging of cystic masses of the mediastinum. Radiographics. 2002;22(Spec No):S79–93. doi: 10.1148/radiographics.22.suppl_1.g02oc09s79. [DOI] [PubMed] [Google Scholar]
- 7.Nasseri F, Eftekhari F. Clinical and radiologic review of the normal and abnormal thymus: pearls and pitfalls. Radiographics. 2010;30(2):413–28. doi: 10.1148/rg.302095131. [DOI] [PubMed] [Google Scholar]
- 8.Odev K, Aribas BK, Nayman A. Imaging of Cystic and Cyst-like Lesions of the Mediastinum with Pathologic Correlation. J clin Imaging Sci. 2012;22:33. doi: 10.4103/2156-7514.97750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Otsuka H. The utility of FDG-PET in the diagnosis of thymic epithelial tumors. J Med Invest. 2012;59(3–4):225–34. doi: 10.2152/jmi.59.225. [DOI] [PubMed] [Google Scholar]
- 10.Kaira K, Sunaga N, Ishizuka T. The role of [18F]fluorodeoxyglucose positron emission tomography in thymic epithelial tumors. Cancer Imaging. 2011;11:195–201. doi: 10.1102/1470-7330.2011.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Werner MK, Schmidt H, Schwenzer NF. MR/PET: a new challenge in hybrid imaging. Am J Roentgenol. 2012;199(2):272–77. doi: 10.2214/AJR.12.8724. [DOI] [PubMed] [Google Scholar]
- 12.Schiepers C, Dahlbom M. Molecular imaging in oncology: the acceptance of PET/CT and the emergence of MR/PET imaging. Eur Radiol. 2011;21(3):548–54. doi: 10.1007/s00330-010-2033-y. [DOI] [PMC free article] [PubMed] [Google Scholar]