Abstract
Introduction
Smoke-free policies are being increasingly promoted and adopted in subsidised multiunit housing to address disparities in residential secondhand smoke exposure. In order to inform the planning and evaluation of these policies, this study examined associations between self-reported in-home smoking and surface nicotine concentrations.
Methods
A face-to-face, cross-sectional survey was conducted from August to October 2011 with leaseholders in a probability sample of private subsidised housing units in Columbus, Ohio, without an existing smoke-free housing policy (n=301, 64% response rate). After the survey, a wipe sample was collected from a wood surface in the living room to measure surface nicotine concentrations (n=279).
Results
In-home smoking was reported by 56.6% of respondents. Geometric mean surface nicotine concentrations differed between non-smoking and smoking homes (11.4 vs 90.9 μg/m2; p<0.001), and between homes with complete, partial and no voluntary home smoking restrictions (8.9 vs 56.3 vs 145.6 μg/m2; p<0.001). Surface nicotine concentrations were moderately correlated (r=.52) with the total number of cigarettes smoked indoors per week. Smoking behaviours of respondents, other household members and visitors, and length of stay were independently associated with surface nicotine concentrations in a multivariable model, explaining 52% of the variance.
Conclusions
Surface nicotine concentrations were significantly associated with a range of self-reported in-home smoking behaviours. This measure should be considered for evaluating changes in in-home smoking behaviours after implementation of smoke-free policies by subsidised housing providers. More research is needed about how surface nicotine concentrations differ over space, time and various indoor surfaces.
INTRODUCTION
Smoke-free policies in publicly subsidised multiunit housing (MUH) are being increasingly promoted as a policy strategy for addressing socioeconomic disparities in secondhand smoke (SHS) exposure in the home.1 About seven million individuals live in MUH units subsidised by the US Department of Housing and Urban Development (HUD) (https://pic.hud.gov/pic/RCRPublic/rcrmain.asp). Documentation that SHS seeps from smoking to non-smoking units in MUH,2,3 and cannot be prevented with building improvements,4 justifies the use of smoke-free housing policies. To date, almost 250 subsidised housing providers in the US have adopted smoke-free policies in one or more buildings (Jim Bergman, JD, written communication, 18 March 2011).
Although it is clear that smoke-free policies can and are being implemented in this setting, it is not yet clear whether they lead to behaviour change among tenants.1 In the only published evaluation of a smoke-free policy in subsidised MUH, smokers reported decreased indoor smoking and cigarette consumption, and increased cessation within 17 months of policy implementation.5 Although these results seem promising, baseline measurement was retrospective self-reporting, and objective measures of in-home smoking were not collected.
Additionally, relatively little is known about in-home smoking behaviours in the absence of smoke-free policies in extremely low-SES populations. Self-reported in-home smoking behaviours have been shown to be reliable and valid in a diverse range of smokers, including low socioeconomic status (SES) populations.2,6–10 However, self-reported in-home smoking among subsidised housing tenants has been validated in only one published study. Kraev et al2 measured air nicotine concentrations in a convenience sample of 49 subsidised housing units occupied by smokers and non-smokers. Nicotine concentrations were higher in homes with smokers, and increased with the number of cigarettes smoked inside the home. However, these results cannot necessarily be generalised to a random sample of subsidised housing tenants because they may not be able11 or willing to report this information. Many housing subsidies are linked to specific housing units rather than households, and demand for subsidies far outpaces supply.12 In this context, social desirability, or intentional misreporting, may be a problem even before a smoke-free policy is implemented.
Although most studies have objectively measured nicotine in SHS using passive diffusion monitors,13 surface nicotine offers an attractive alternative. Almost all nicotine in SHS is deposited and adsorbed onto indoor surfaces, including dust, furnishings, and walls.14–16 Nicotine and other components of residual tobacco smoke that remain after active SHS has dispersed are increasingly referred to as thirdhand smoke (THS).17 Nicotine is slowly re-emitted into the air, but measures longer-term exposure to both SHS and THS (ie, weeks to months) compared with air nicotine.18 Additionally, surface wipe samples may be collected at one point in time, eliminating measurement reactivity and logistical challenges associated with passive monitoring. In several non-probability samples selected to represent strict non-smoking or smoking households, surface nicotine concentrations distinguished well between smoking and non-smoking homes, and were moderately correlated with air nicotine concentrations (r=0.54).19,20
The current study examined associations between self-reported in-home smoking behaviours and indoor surface nicotine concentrations (SurfNicConc) in a population of subsidised housing tenants. The study had three primary aims: (1) determine the extent to which self-reported in-home smoking behaviours were associated with SurfNicConc; (2) identify the SurfNicConc that best distinguished between smoking and non-smoking homes and (3) determine factors that were independently associated with SurfNicConc, including sources of in-home SHS exposure, as well as demographic and building-related characteristics.
METHODS
Sample
The study population comprised tenants in subsidised housing units located in 184 buildings across five urban neighbourhoods and managed by a private company in Columbus, Ohio. No buildings or units were covered by a smoke-free housing policy. Using units that were occupied as of July 2011 (n=914), a stratified random sample (n=475) was selected using proportional allocation; administrative data from the property management company were used to stratify units by the age of the youngest child, because this variable has been associated with home smoking restrictions.21,22 The primary leaseholder in selected units was eligible to participate.
Data collection
A face-to-face, interviewer-administered survey was conducted in tenants’ homes from August to October 2011. Each interviewer completed 6 h of training about interview techniques and data collection protocols. A personalised letter was sent to leaseholders in selected units 1 week prior to the first in-person visit. Teams of two interviewers (one community resident and one graduate student) made at least five attempts to contact leaseholders at different days and times. Surface wipe samples were collected at the end of the survey.
Using methods developed by researchers at San Diego State University (SDSU) ( Joy Zakarian, MPH, written communication, 14 April 2011; Dale Chatfield, PhD, written communication, 7 April 2011),19,20 a small round 100% cotton wipe was wetted with 2 ml of freshly prepared 1% ascorbic acid solution using a sterile pipette. Wearing gloves, the interviewer wiped the area within a 10×10 cm template taped on a vertical wooden surface in the living room, and placed the wipe in a precleaned 20 ml amber bottle with Teflon cap seal. Samples were chilled during transport and frozen (−20°C) until analysis. Blank wipes were prepared and bottled before collecting the samples in each unit; 10% of blank wipes were randomly selected for analysis.
Visits took an average of 27.0 min to complete, and respondents were given a US$5 grocery store gift card. Completed surveys were obtained for 301 units (63.8% response rate; three vacant units were removed from the denominator); the cooperation rate was 74.1% among units where someone was reached. Surface wipe samples were obtained for 279 units (92.7% of survey respondents); 19 did not give permission, two did not have an appropriate surface, and one was discarded due to contamination. The study was approved by the university's institutional review board, and participants provided informed consent.
Measurement
Surface nicotine concentration (SurfNicConc)
Surface wipe samples were analysed by Dale Chatfield at SDSU using similar methods as previous studies.19,20 Briefly, analysis procedures used 100 ng nicotine-d4 followed by 10 ml 0.1 M KOH (aqueous) added to the stored cotton wipes, and the bottles were vortexed periodically for 30 min. The wipes were removed, squeezing out excess liquid. Four millilitres of methylene chloride was added, and the sample was placed on a rocking table for 30 min. Next, 1.5 ml was transferred to an amber autosampler vial and 25 μl buffer (90% methanol/10% 0.1 M propionic acid) was added. After samples were evaporated to dryness in a vacuum manifold, 500 μl mobile phase solution (acetonitrile: pH4 20 mM acetate buffer of 70:30 (v/v)) HPLC was added, capped and stored at −10°C in the dark until analysis (Dale Chatfield, PhD, written communication, 9 January 2012).
Smoking status
All participants were asked whether they had smoked at least 100 cigarettes in their lifetime, and how many days per week they smoked presently. Participants were instructed to include small cigars in their responses because there was not a separate question about small cigar use. Participants were categorised as never, former and current smokers. Never-smokers had never smoked 100 cigarettes, and smoked zero days per week now. Former smokers had smoked 100 cigarettes in their lifetime, but smoked zero days now. Current smokers smoked 1–7 days per week now regardless of whether they had smoked 100 cigarettes in their lifetime.
Sources and quantity of in-home smoking
Current smokers reported how many cigarettes they usually smoke on days they smoke, and how many they usually smoke inside the home. Responses to the latter question were assigned proportions (none=0.0; a few=0.25; about half=0.5; most=0.75; all=1.0) and used to calculate the number of cigarettes smoked indoors per week. The number of days per week other household members and visitors smoked inside the respondent's home was multiplied by the number of cigarettes usually smoked indoors each day. Totals from all sources were summed (weekly total) and divided by seven (average daily).
Outdoor smoking by others
Respondents reported how many days per week other household members or visitors smoked cigarettes outdoors but still on the property. Responses were dichotomised as none versus any outdoor smoking.
Voluntary home smoking restrictions (HSRs)
Respondents were asked, ‘Which of the following best describes smoking inside your home? Do not include decks or porches.’, with responses for ‘not allowed anywhere’, ‘allowed in some places or at some times’, or ‘allowed anywhere inside the home’. Those who reported no smoking anywhere were asked if there were any exceptions to the rule. Complete HSRs were defined as no smoking allowed anywhere in the home with no exceptions. Partial HSRs allowed smoking in some places or at some times, including having exceptions to complete restrictions.
SHS incursion
Respondents were asked, ‘How often do you smell cigarette smoke in your apartment that came from other apartments or the hallway?’ Responses were categorised into never, infrequently (few times per year/month) or frequently (few times per week/everyday).
Building characteristics
Length of stay was a proxy for the time since indoor surfaces were replaced, cleaned and/or painted, and was calculated using the self-reported move-in date. However, complete physical renovations were conducted on all units between 2004 and 2009, which would have substantively affected SurfNicConc. Therefore, length of stay was truncated to the date of renovation completion (obtained from administrative data) if the respondent lived in the same unit prior to renovation. Data collectors recorded unit location (upper vs ground floor) and the number of units in the building. Number of units was dichotomised into four units or less versus more than four units. Square footage of units was obtained from administrative data and dichotomised based on median size (820 square feet).
Demographic and household characteristics
Age (in years); race (African–American or other); gender (male or female); age of youngest child under 18 years living in household (none, <5 years, 5–17 years); presence of a child with asthma diagnosis (yes or no); educational attainment (high school graduate or not); and employment status (full-time/part-time or not employed).
Data analysis
Laboratory analyses
Analysts at SDSU used liquid chromatography tandem mass spectrometry (LC-MS-MS) using electrospray ionisation (Finnigan TSQ Quantum Ultra; Thermo Fisher Scientific, Waltham, Massachusetts, USA). Nicotine was quantified against the internal standard, nicotine-d4 (CDN Isotopes Inc, Pointe-Claire, Quebec, Canada). Aliquots were injected onto a 2.1 mm×50 mm, 5 μm particle diameter LC silica column (Hypersil, Thermo Fisher Scientific, Waltham, Massachusetts, USA) at 150 μl/min. Selected reaction monitoring of the MS-MS transitions at 24 V collision-induced dissociation (CID) of m/z 163.2 to m/z 117.1 and 130.1, and m/z 167.1 to m/z 121.1 and 134.1 was used for nicotine and nicotine-d4, respectively. The amount of nicotine in the sample was determined by the ratio of peak areas of nicotine to nicotine-d4 in the sample. The limit of detection (LOD) was approximately 0.5 μg nicotine/m2. Lab blanks were run between each sample; if they were above the LOD, another blank was run. Standard calibration curves were linear from 5 to 8000 ng/ml with R2=0.998; samples with values greater than 8000 ng/ml were diluted and reanalysed. (Dale Chatfield, PhD, written communication, 9 January, 26 March and 25 May 2012).
Statistical analyses
One surface wipe sample had a nicotine concentration below the LOD and was assigned a value of LOD/2 (0.25 μg/m2). SurfNicConc and number of cigarettes smoked indoors per week were natural log-transformed to address positively skewed distributions; geometric means are reported for SurfNicConc. χ2 tests were used to compare categorical variables, and linear regressions were used to compare means across groups for all analyses unless otherwise noted, with adjustments for stratification. Bonferroni adjustments were used for multiple post-hoc comparisons with α=0.05.
‘Smoking homes’ were defined as those in which the respondent was a current smoker and reported smoking cigarettes inside the home, or other household members or visitors smoked inside the home at least once per week. ‘Non-smoking homes’ did not meet either of these criteria. Demographic characteristics and mean SurfNicConc were compared between smoking and non-smoking homes, and across homes with complete, partial and no HSRs. Consistent with a recent study,19 the optimum value that distinguished between smoking and non-smoking homes was determined using a receiver operator characteristic (ROC) curve. Pearson's correlation coefficients were calculated between SurfNicConc and total weekly cigarettes smoked inside in smoking homes.
Independent associations between potential sources of indoor SHS exposure and SurfNicConc were also examined. Multiple linear regression adjusted for stratification was used to measure adjusted associations between each source and SurfNicConc. A purposeful forward selection approach to model building was used, and diagnostics were conducted using non-survey regression to examine assumptions of normality and homoscedasticity of error terms, linearity for continuous dependent variables, multicollinearity and overly influential observations.23 Analyses were conducted using SAS 9.2 (SAS Institute, Inc, Cary, North Carolina, USA) and STATA V.10.1 (StataCorp, College Station, Texas, USA).
RESULTS
Sample characteristics
Based on administrative data, non-respondents did not differ from respondents in leaseholder age (p=0.29), age of youngest child (p=0.82), or neighbourhood of residence (p=0.50). Demographic characteristics did not differ between respondents with and without surface wipe samples (data not shown), but the smoking rate was higher among those without samples (68.2% vs 45.9%; p=0.04). The overall geometric mean SurfNicConc was 37.0 μg/m2; actual values ranged from 0.5 to 6377 μg/m2. Blank wipes (n=28) ranged from 0.0 to 1.6 μg/m2 with an arithmetic mean of 0.4 (0.4) μg/m2.
Smoking versus non-smoking homes
Overall, 56.6% of respondents reported any indoor smoking in their homes; these respondents differed from those in non-smoking homes by education level and employment status (table 1). Mean SurfNicConc were significantly different between smoking and non-smoking homes and across types of HSRs (table 2). Concentrations were significantly lower among those with complete versus partial HSRs (p<0.001), and partial versus no HSRs (p<0.001). The SurfNicConc that best distinguished between self-reported home smoking status was 16.8 μg/m2 with a sensitivity of 88.6% and specificity of 71.1% (figure 1).
Table 1.
Demographic characteristics by home smoking status
| Smoking homes* (n=158) | Non-smoking homes* (n=121) | p Value | |||
|---|---|---|---|---|---|
| Age, median (years) | 25.0 | – | 24.4 | – | 0.83 |
| Female (%) | 138 | 87.3 | 104 | 86.0 | 0.74 |
| African–American (%) | 136 | 86.1 | 97 | 80.2 | 0.19 |
| Age of youngest child (%) | 0.50 | ||||
| No children | 47 | 29.7 | 29 | 24.0 | |
| <5 years | 85 | 53.8 | 73 | 60.3 | |
| 5–17 years | 26 | 16.5 | 19 | 15.7 | |
| Has child with asthma (%) | 33 | 20.9 | 31 | 25.6 | 0.35 |
| Less than high school graduate (%) | 55 | 34.8 | 28 | 23.1 | 0.03 |
| Employed full-time or part-time (%) | 42 | 26.6 | 48 | 39.7 | 0.02 |
‘Smoking homes’ were those in which either the respondent reported smoking any cigarettes inside the home, or other household members or visitors smoked inside the home at least once per week. ‘Non-smoking homes’ did not meet either of these criteria.
Table 2.
Geometric mean surface nicotine concentrations (μg/m2) by self-reported home smoking status and voluntary home smoking restrictions (n=279)
| 95% CI |
||||||
|---|---|---|---|---|---|---|
| n | % | Mean | Lower | Upper | p value | |
| Home smoking status* | <0.001 | |||||
| Non-smoking | 121 | 43.4 | 11.4 | 8.9 | 14.7 | |
| Smoking | 158 | 56.6 | 90.9 | 71.5 | 115.6 | |
| Voluntary HSRs | <0.001 | |||||
| Complete | 86 | 30.8 | 8.9 | 6.7 | 11.9 | |
| Partial | 150 | 53.8 | 56.3 | 43.2 | 73.4 | |
| None | 43 | 15.4 | 145.6 | 94.8 | 223.6 | |
HSRs, home smoking restrictions.
‘Smoking homes’ were those in which either the respondent reported smoking any cigarettes inside the home, or other household members or visitors smoked inside the home at least once per week. ‘Non-smoking homes’ did not meet either of these criteria.
Figure 1.
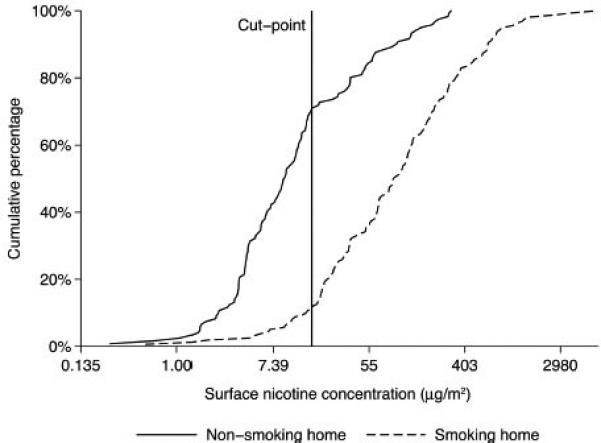
Cumulative distributions of surface nicotine concentrations (μg/m2) by home smoking status with cut-point that maximises sensitivity and specificity.
Amount of indoor smoking
Among smoking homes, a median of 3.0 cigarettes (mean=5.9 cigarettes) were smoked indoors per day by all sources (range 0.1–65.7). Number of cigarettes and SurfNicConc were moderately correlated (r=0.52, p<0.001). Similarly, mean SurfNicConc varied by number of cigarettes smoked indoors per day (table 3). Differences were statistically significant between all categories except the highest two.
Table 3.
Geometric means for indoor surface nicotine concentrations (μg/m2) by amount and sources of in-home SHS and building-related characteristics (n=279)
| 95% CI |
||||||
|---|---|---|---|---|---|---|
| n | % | Mean | Lower | Upper | p value | |
| Amount of indoor SHS | ||||||
| Average daily cigarettes smoked indoors | <0.001 | |||||
| None | 121 | 43.5 | 11.4 | 8.9 | 14.7 | |
| ≤1 | 43 | 15.5 | 26.1 | 17.4 | 39.4 | |
| >1 and ≤3 | 36 | 12.9 | 83.1 | 50.7 | 136.1 | |
| >3 and ≤7 | 34 | 12.2 | 182.8 | 120.3 | 277.8 | |
| >7 | 44 | 15.8 | 197.2 | 131.5 | 295.8 | |
| Sources of SHS | ||||||
| Respondent smoking status | ||||||
| Current | 128 | 45.9 | 113.4 | 87.9 | 146.2 | <0.001 |
| Former | 36 | 12.9 | 18.3 | 10.5 | 31.9 | |
| Never | 115 | 41.2 | 13.3 | 10.2 | 17.3 | |
| Respondent smokes indoors | ||||||
| Yes | 110 | 39.4 | 131.9 | 99.9 | 174.3 | <0.001 |
| No | 169 | 60.6 | 16.2 | 12.9 | 20.3 | |
| Other HH smoker | ||||||
| Yes | 44 | 15.9 | 87.4 | 54.6 | 139.9 | <0.001 |
| No | 233 | 84.1 | 31.8 | 25.2 | 40.0 | |
| Other HH member smokes indoors | ||||||
| Yes | 33 | 11.9 | 115.6 | 72.6 | 184.2 | <0.001 |
| No | 244 | 88.1 | 32.0 | 25.5 | 40.2 | |
| Visitors smoke indoors | ||||||
| Yes | 110 | 39.4 | 87.1 | 65.7 | 115.3 | <0.001 |
| No | 169 | 60.6 | 21.2 | 16.3 | 27.6 | |
| Other HH member or visitors smoke outdoors | ||||||
| Yes | 151 | 54.1 | 43.3 | 32.7 | 57.5 | 0.11 |
| No | 128 | 45.9 | 30.7 | 22.3 | 42.1 | |
| SHS incursion* | 0.03 | |||||
| Never | 102 | 68.0 | 14.8 | 11.1 | 19.9 | |
| Infrequent | 20 | 13.3 | 7.4 | 4.1 | 13.3 | |
| Frequent | 28 | 18.7 | 20.7 | 11.8 | 36.3 | |
| Building-related characteristics | ||||||
| Length of stay | <0.001 | |||||
| ≤2 months | 17 | 6.1 | 8.6 | 5.2 | 14.2 | |
| 3–6 months | 33 | 11.8 | 20.3 | 11.8 | 35.0 | |
| >6 months | 229 | 82.1 | 44.9 | 35.4 | 56.9 | |
| Unit location | ||||||
| Upper floor | 57 | 20.5 | 46.3 | 28.5 | 75.1 | 0.29 |
| Ground floor | 221 | 79.5 | 34.9 | 27.5 | 44.3 | |
| Units in building | ||||||
| ≤4 units | 120 | 44.8 | 40.0 | 29.6 | 54.0 | 0.35 |
| >4 units | 148 | 55.2 | 32.5 | 24.0 | 44.0 | |
| Size of unit | ||||||
| <820 sq. ft. | 139 | 49.8 | 37.7 | 27.7 | 51.3 | 0.86 |
| ≥820 sq. ft. | 140 | 50.2 | 36.3 | 27.0 | 48.6 | |
Among non-smokers only. Infrequent=a few times a year or month; frequent=a few times per week or everyday.
SHS, secondhand smoke; HH, household.
Factors associated with SurfNicConc
In bivariate associations, each potential source of indoor SHS was significantly associated with higher SurfNicConc except outdoor smoking (table 3). Concentrations were higher for current compared with former (p<0.001) smokers, but did not differ between former and never-smokers (p=0.28); former and never-smokers were combined (ie, non-smokers) in the multivariable model. Interestingly, SurfNicConc were higher among respondents who never had SHS incursions compared with those with infrequent incursions (p=0.04), but were also higher among those with frequent, compared with infrequent incursions (p=0.01). The only building-related characteristic associated with SurfNicConc was length of stay (table 3).
Two influential cases and two cases with missing data were removed from the final regression model. Indoor smoking by respondents and visitors, as well as smoking status of respondents and other household members, contributed significantly to predicting SurfNicConc (table 4). Additionally, SurfNicConc increased as length of stay (continuous) increased. Predictors explained about half the variance in SurfNicConc (R2=0.52).
Table 4.
Multiple linear regression model of associations between sources of secondhand smoke and log-transformed surface nicotine concentrations (n=275)
| 95% CI |
||||
|---|---|---|---|---|
| Variables | Coefficient | Lower | Upper | p value |
| Intercept | 0.9 | 0.5 | 1.2 | <0.001 |
| Sources of SHS | ||||
| Respondent is a current smoker | 1.1 | 0.6 | 1.6 | <0.001 |
| Respondent smokes indoors | 0.8 | 0.2 | 1.3 | 0.01 |
| Other household member smokes | 0.5 | 0.1 | 1.0 | 0.02 |
| Visitors smoke indoors | 0.6 | 0.3 | 1.0 | <0.001 |
| Building-related characteristics | ||||
| Length of stay, log months | 0.5 | 0.4 | 0.6 | <0.001 |
SHS, secondhand smoke.
DISCUSSION
This is the first study of associations between self-reported in-home smoking behaviours, and an objective measure of in-home smoking in a probability sample of subsidised MUH tenants. Across almost all self-reported in-home smoking behaviours, differences in SurfNicConc were large in magnitude and statistically significant. Smoking by tenants, other household members and visitors all contributed significantly to SurfNicConc. These findings are consistent with a previous study that measured air nicotine concentrations and self-reported in-home smoking in a small convenience sample of subsidised housing tenants.2 Taken together, and in the absence of a smoke-free policy, these findings suggest that tenants were willing and able to accurately report in-home smoking-related behaviours.
SurfNicConc did not distinguish between higher levels of in-home smoking (ie, above three cigarettes per day). Proxy reporting of cigarette consumption has been shown to be less accurate than a self-report,7 but homes with smokers other than the respondent were not more common among higher levels of in-home smoking (data not shown). Alternatively, the measure itself may be less precise at higher levels of smoking. For example, surfaces may become saturated with nicotine at a certain threshold. Future studies conducted in controlled environments should test this hypothesis.
SurfNicConc were relatively high in non-smoking homes. In a previous study, Matt et al19 measured SurfNicConc in purposively selected non-smoking homes (ie, no smokers had lived and no visitors had smoked indoors for the past 6 months, n=50). Compared with this previous study, mean SurfNicConc were more than seven times higher among non-smoking homes in the current study. There are several possible reasons for these findings. In the current study, tenants only reported the number of cigarettes usually smoked inside their homes each week, while the previous study considered all smoking in the past 6 months. Additionally, homes in the current study may have been contaminated by smoking behaviours of previous tenants19 because 18% of respondents had been in their homes 6 months or less, whereas, 6-month residency was an eligibility criterion for the previous study. Finally, non-smoking units in the current study may have been contaminated from SHS incursions because SHS transfers between units in MUH.2,3 However, nicotine transfers less than other SHS components due to its high rate of sorption.3,4 One previous study did not find significant associations between self-reported SHS incursions and air nicotine concentrations.2,19 Results in the current study were mixed, with inexplicably higher SurfNicConc in units reporting no incursions despite limiting this analysis to non-smokers. These leaseholders may have been concerned about reporting negative behaviours of their neighbours. SurfNicConc were higher in units with frequent, compared with infrequent incursions, but sample sizes were limited in these two groups.
Regardless of the reason for relatively high SurfNicConc in non-smoking homes, the cut-point for smoking versus non-smoking homes should not be used to evaluate individual-level compliance with smoke-free housing policies. Instead, mean SurfNicConc could be compared between units in buildings with and without smoke-free policies, or before and after policy implementation. A previous study found that SurfNicConc decreased significantly, but remained detectable several months after smokers moved out of their homes.19 Future studies should examine whether SurfNicConc are sensitive to less dramatic changes in in-home smoking behaviours (eg, implementation of complete home smoking restrictions) to better inform the appropriateness of this measure for evaluating smoke-free housing policies.
If SurfNicConc are higher among non-smoking homes in subsidised MUH compared with other populations, these households are also exposed to higher levels of THS. Nicotine from household surfaces may be inhaled or ingested through dust or dermal contact, especially among young children.24 Indoor SurfNicConc have been independently associated with urine cotinine concentration in children even after controlling for air and/or dust nicotine concentrations.19,20 Additionally, sorbed nicotine has been shown to create potentially harmful secondary indoor pollutants that cause eye, skin and upper respiratory tract irritations, and exacerbate asthma symptoms.17 Although independent health effects of THS beyond those associated with SHS have not yet been documented in human beings, higher rates of exposure to THS among non-smokers in subsidised MUH could be a concern if such evidence emerges.
Limitations
The presence of surface nicotine means that smoke from a tobacco product was present at some time in the past, but little is known about chronological or spatial patterns of surface nicotine concentrations. In the current study, results may have been different if samples were collected from different surface types or areas of the home. Sampled surfaces could have been painted or cleaned since the tenant moved in (or the unit was renovated), and it is not known how these activities affect surface nicotine. Measurable surface nicotine does not necessarily mean that active smoking occurred in the home or among current tenants. However, tobacco smoking in the home may have been under-reported due to a lack of biomeasures and specific questions about tobacco products other than cigarettes, and tenant concerns about the housing provider discovering adults in the home who were not identified on the lease. This subsidised housing population was from a single city, and included predominantly young African–American females with children. Therefore, findings may not generalise to subsidised housing populations in other types of cities, or those that are predominantly seniors, or people with disabilities, but may generalise to other low-SES populations living in MUH. Because buildings typically had four to eight units with few units on an upper floor, results may not generalise to higher-density MUH.
CONCLUSIONS
In a probability sample of subsidised housing tenants, indoor SurfNicConc were strongly associated with a range of self-reported in-home smoking behaviours. Thus, self-reported in-home smoking behaviours obtained from subsidised housing tenants in the absence of a smoke-free housing policy can be used to inform interventions to address residential SHS exposure. Surface nicotine should also be considered as an objective measure to evaluate the effectiveness of smoke-free policies in subsidised housing. Relatively high SurfNicConcs in non-smoking homes should be revisited if more conclusive evidence emerges about independent health effects of THS.
What this study adds
▶ Smoke-free policies in subsidised multiunit housing (MUH) are increasingly common but their effectiveness has not yet been rigorously evaluated. Indoor surface nicotine offers a feasible alternative for objectively measuring in-home smoking that could inform the planning and evaluation of such policies.
▶ This is the first study to examine associations between self-reported in-home smoking behaviours and indoor surface nicotine concentrations in a probability sample, and among subsidised housing tenants.
▶ Results showed that subsidised housing tenants without an existing smoke-free policy were willing and able to accurately report in-home smoking behaviours. In addition, surface nicotine concentrations were strongly associated with a range of self-reported in-home smoking behaviours.
▶ Future studies should continue to examine surface nicotine as an objective measure of in-home smoking.
Acknowledgements
The authors would like to acknowledge Community Properties of Ohio staff for partnering on this study, and the tenants for graciously sharing their time and opinions. We also sincerely thank Anna Borsick, Amber Broadus, Danyelle Heard, Katy Meeker and Meaghan Novi for their commitment to and enthusiasm for collecting data. Finally, we gratefully acknowledge Dale Chatfield, PhD, at San Diego State University, for analysing the surface wipe samples.
Funding Prepared under Grant Number H-21629SG from the Department of Housing and Urban Development, Office of University Partnerships. Points of view, or opinions in this document, are those of the author and do not necessarily represent the official position or policies of the Department of Housing and Urban Development. One student data collector (K Meeker) was supported through a grant from the National Cancer Institute (P50CA105632). This work was also supported by Community Properties of Ohio (CPO). CPO staff provided a list of tenants for the sampling frame and reviewed drafts of the survey and preliminary study results. No other funders were involved in any study-related activities.
Footnotes
Competing interests None.
Provenance and peer review Not commissioned; externally peer reviewed.
Contributors All authors made substantial contributions to the conception and design of the study, and to the interpretation of data. NEH also collected and analysed the data. NEH drafted the article, and all coauthors contributed to revising it substantively based on intellectual content. Finally, all authors approved the final version of the article to be published.
REFERENCES
- 1.Winickoff JP, Gottlieb M, Mello MM. Regulation of smoking in public housing. N Engl J Med. 2010;362:2319–25. doi: 10.1056/NEJMhle1000941. doi:10.1056/NEJMhle1000941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kraev TA, Adamkiewicz G, Hammond SK, et al. Indoor concentrations of nicotine in low-income, multi-unit housing: associations with smoking behaviours and housing characteristics. Tob Control. 2009;18:438–44. doi: 10.1136/tc.2009.029728. doi:10.1136/tc.2009.029728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.King BA, Travers MJ, Cummings KM, et al. Secondhand smoke transfer in multiunit housing. Nicotine Tob Res. 2010;12:1133–41. doi: 10.1093/ntr/ntq162. doi:10.1093/ntr/ntq162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bohac D, Hewett M, Hammond S, et al. Secondhand smoke transfer and reductions by air sealing and ventilation in multiunit buildings: PFT and nicotine verification. Indoor Air. 2011;21:36–44. doi: 10.1111/j.1600-0668.2010.00680.x. doi:10.1111/j.1600-0668.2010.00680.x. [DOI] [PubMed] [Google Scholar]
- 5.Pizacani BA, Maher JE, Rohde K, et al. Implementation of a smoke-free policy in subsidized multiunit housing: effects on smoking cessation and secondhand smoke exposure. Nicotine Tob Res. 2012;14:1027–34. doi: 10.1093/ntr/ntr334. [DOI] [PubMed] [Google Scholar]
- 6.Hovell M, Zakarian J, Matt G, et al. Counseling to reduce children's secondhand smoke exposure and help parents quit smoking: a controlled trial. Nicotine Tob Res. 2009;11:1383–94. doi: 10.1093/ntr/ntp148. doi:doi:10.1093/ntr/ntp148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matt GE, Hovell MF, Zakarian JM, et al. Measuring secondhand smoke exposure in babies: the reliability and validity of mother reports in a sample of low-income families. Health Psychol. 2000;19:232–41. doi: 10.1037//0278-6133.19.3.232. doi:10.1037//0278-6133.19.3.232. [DOI] [PubMed] [Google Scholar]
- 8.Berman BA, Wong GC, Bastani R, et al. Household smoking behavior and ETS exposure among children with asthma in low-income, minority households. Addict Behav. 2003;28:111–28. doi: 10.1016/s0306-4603(01)00221-0. doi:10.1016/S0306-4603(01)00221-0. [DOI] [PubMed] [Google Scholar]
- 9.Gehring U, Leaderer BP, Heinrich J, et al. Comparison of parental reports of smoking and residential air nicotine concentrations in children. Occup Environ Med. 2006;63:766–72. doi: 10.1136/oem.2006.027151. doi:10.1136/oem.2006.027151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brunekreef B, Leaderer B, van Strien R, et al. Using nicotine measurements and parental reports to assess indoor air: The PIAMA birth cohort study. Epidemiology. 2000;11:350–2. doi: 10.1097/00001648-200005000-00023. doi:10.1097/00001648-200005000-00023. [DOI] [PubMed] [Google Scholar]
- 11.Streiner DL, Norman GR. Health measurement scales: a practical guide to their development and use. 2nd edn. Oxford University Press; New York, NY: 1995. [Google Scholar]
- 12.Turner MA, Kingsley GT. Federal programs for addressing low-income housing needs: a policy primer. Urban Institute; Washington, DC: 2008. [Google Scholar]
- 13.Hammond SK, Leaderer BP. A diffusion monitor to measure exposure to passive smoking. Environ Sci Technol. 1987;21:494–7. doi: 10.1021/es00159a012. doi:10.1021/es00159a012. [DOI] [PubMed] [Google Scholar]
- 14.Daisey JM. Tracers for assessing exposure to environmental tobacco smoke: what are they tracing? Environ Health Perspect. 1999;107(Suppl 2):319–27. doi: 10.1289/ehp.99107s2319. doi:10.2307/3434424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singer B, Revzan K, Hotchi T, et al. Sorption of organic gases in a furnished room. Atmos Environ. 2004;38:2483–94. doi:10.1016/j.atmosenv.2004.02.003. [Google Scholar]
- 16.Kim S, Aung T, Berkeley E, et al. Measurement of nicotine in household dust. Environ Res. 2008;108:289–93. doi: 10.1016/j.envres.2008.07.004. doi:10.1016/j.envres.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 17.Matt GE, Quintana PJE, Destaillats H, et al. Thirdhand tobacco smoke: emerging evidence and arguments for a multidisciplinary research agenda. Environ Health Perspect. 2011;119:1218–26. doi: 10.1289/ehp.1103500. doi:10.1289/ehp.1103500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singer B, Hodgson A, Nazaroff W. Gas-phase organics in environmental tobacco smoke: 2. Exposure-relevant emission factors and indirect exposures from habitual smoking. Atmos Environ. 2003;37:5551–61. doi:10.1016/j.atmosenv.2003.07.015. [Google Scholar]
- 19.Matt G, Quintana P, Zakarian J, et al. When smokers move out and non-smokers move in: residential thirdhand smoke pollution and exposure. Tob Control. 2011;20:e1–8. doi: 10.1136/tc.2010.037382. doi:10.1136/tc.2010.037382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Matt GE, Quintana PJ, Hovell MF, et al. Households contaminated by environmental tobacco smoke: sources of infant exposures. Tob Control. 2004;13:29–37. doi: 10.1136/tc.2003.003889. doi:10.1136/tc.2003.003889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Borland R, Yong HH, Cummings KM, et al. Determinants and consequences of smoke-free homes: findings from the International Tobacco Control (ITC) four country survey. Tob Control. 2006;15(Suppl 3):S42–50. doi: 10.1136/tc.2005.012492. doi:10.1136/tc.2005.012492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.King B, Cummings K, Mahoney M, et al. Multiunit housing residents’ experiences and attitudes toward smoke-free policies. Nicotine Tob Res. 2010;12:598–605. doi: 10.1093/ntr/ntq053. doi:10.1093/ntr/ntq053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hosmer DW, Lemeshow S. Applied logistic regression. 2nd edn. John Wiley & Sons, Inc; Hoboken, NJ: 2000. [Google Scholar]
- 24.Matt GE, Bernert JT, Hovell MF. Measuring secondhand smoke exposure in children: an ecological measurement approach. J Pediatr Psychol. 2008;33:156–75. doi: 10.1093/jpepsy/jsm123. doi:10.1093/jpepsy/jsm123. [DOI] [PubMed] [Google Scholar]


