Abstract
Background
The Bernese periacetabular osteotomy (PAO) has entered its fourth decade and is frequently used for corrective osteotomy in patients with acetabular dysplasia. Although our capacity to preserve the joint after corrective osteotomy is excellent, gaining a better understanding on how well patients function after this surgery is important as well.
Questions/purposes
(1) What changes in patient-reported outcomes scores occur in patients treated with PAO for hip dysplasia in the setting of a single-surgeon practice? (2) What are the predictors of clinical function and survivorship?
Methods
All 67 patients presenting to a single surgeon’s clinic with hip dysplasia treated with PAO between October 2005 and January 2013 were prospectively followed. Baseline demographic data as well as pre- and postoperative radiographic and functional measurements were obtained with a minimum of 1-year followup. Radiographic criteria included Tönnis grade, Tönnis angle, minimum joint space width, center-edge angle, presence of crossover sign, medial translation of the hip center, and alpha angle. We also used validated outcome measures including the WOMAC, the UCLA Activity Scale, and the SF-12. Multiple regression analysis was used to determine predictors of functional outcome scores.
Results
There were increases in WOMAC, UCLA, and SF-12 Physical scores. Higher preoperative alpha angle was associated with a lower postoperative WOMAC score (β = −0.47; 95% confidence interval [CI], −0.92 to −0.02; R2 = 0.08; p = 0.04). The 5-year Kaplan-Meier survivorship was 94.1% (95% CI, 90.7–97.5) with reoperation (ie, hip arthroscopy and/or total hip arthroplasty) used as the endpoint for failure. With the limited numbers available, we could not identify any demographic or radiographic factors associated with reoperation.
Conclusions
Overall survivorship for the PAO at our center at 5 years is comparable to other clinical series with overall functional scores improving. A greater alpha angle preoperatively was associated with poorer patient-reported outcome scores. Further research is needed to determine how and when intraarticular cartilage damage associated with dysplasia needs to be addressed.
Level of Evidence
Level IV, therapeutic study.
Introduction
Background
The goal of corrective surgery in the treatment of hip dysplasia is to improve function while relieving pain, delaying and possibly preventing end-stage arthritis [18]. Classically, surgeons performed a variety of osteotomies, proximal femoral, acetabular, or a combination of these [18, 23]. However, with the advent of the Bernese periacetabular osteotomy (PAO) in 1984, a proximal femoral osteotomy has become much less common. PAO allows the surgeon to obtain a large corrective reorientation of the acetabulum with a single incision without the need for external immobilization [8]. This reorientation medializes the joint center and reduces superolateral inclination, thus improving femoral head coverage [7, 14]. Although recent studies have focused on assessing the medium- and long-term outcomes of PAO [10, 11, 15, 24, 27], neither the level of patient function nor the factors that influence clinical and functional outcome are well described [10, 11, 15, 24, 27] for an invasive procedure with a risk of major complications ranging from 6% to 37% [7].
Rationale
Prediction of success with the use of PAO remains difficult because of variations in the definition of success in a joint-preserving procedure of the hip [9]. Further difficulties arise from heterogeneity within the data collection methods used in published studies and the large number of studies that do not attempt to correlate deformity correction with clinical results [7]. Historically, published reports on the PAO have used conversion to THA as the endpoint for failure [7] with proportions ranging from 0% to 17% of cases (Table 1). However, it is not clear if patients without conversion to THA have actually benefitted from PAO surgery; for this, standardized approaches using patient-reported or otherwise validated outcomes tools are needed. In addition, despite the growing use of PAO to treat symptomatic dysplasia of the hip, the optimal selection criteria for surgery and risk factors for clinical failure are still evolving.
Table 1.
Survivorship of mid- to long-term PAO followup
| Study | Demographics | Mean followup (years) | Survivorship |
|---|---|---|---|
| Garras et al., 2007 [10] | 52 patients (58 hips); mean age: 37.6 years; 42 female; 10 male | 5.5 | None provided; 7.7% conversion rate to THA at 3 years |
| Matheney et al., 2009 [15] | 109 patients (135 hips); mean age: 25.7 years; 95 female; 14 male | 9.0 | 96% at 5 years; 84% at 10 years |
| Troelsen et al., 2009 [27] | 96 patients (116 hips); mean age: 29.9 years; 90 female; 26 male | 6.8 | 90.5% at 5 years; 81.6% at 9.2 years |
| Steppacher et al., 2008 [24] | 58 hips; mean age: 29.4 years; 45 female; 13 male | 20.4 | 93.2% at 5 years; 87.6% at 10 years; 60.0% at 20 years |
| Albers et al., 2013 [1] | 165 hips into 2 groups:mean age: 28 years; one-third male 1) Optimal orientation (43 hips) 2) Impingement: retroversion/aspherical head (122 hips) |
11.1 | 1) 95.2% at 5 years; 90.5% 10 years 2) 86.8% at 5 years; 78.6% at 10 years |
PAO = periacetabular osteotomy.
Study Questions
(1) What changes in patient-reported outcomes scores occur in patients treated with PAO for hip dysplasia in the setting of a single-surgeon practice? (2) What are the predictors of clinical function and survivorship?
Patients and Methods
Study Design and Setting
This is a retrospective study that involved drawing data from a prospectively maintained single-center institutional registry. The setting of this study was the practice of a high-volume surgeon (PEB) who is interested in the study of hip preservation surgery.
Participants/Study Subjects
Between October 2005 and January 2013, one surgeon (PEB) treated 67 patients (72 hips) with PAO for acetabular dysplasia. During that time, patients underwent PAO if they had acetabular dysplasia with a center-edge angle of less than 25°, hip pain for at least 1 year, and failure of nonsurgical management (medications and trial of physiotherapy). Relative exclusion criteria for PAO were (1) Tönnis grade > 2; (2) lack of congruity; and (3) age > 50 years. All patients had followup at a minimum of 1 year (median, 5 years; range, 1–8.3 years) and were considered in this retrospective study. Of 41 eligible patients, 39 had at least 5 years of followup (Table 2). Baseline demographic data as well as pre- and postoperative radiographic and functional measurements were prospectively maintained as part of an institutional registry. Mean age at the time of surgery was 32 years (range, 14–54 years) with 79.1% (53 of 67) of the cohort younger than 40 years of age. Mean body mass index was 26 kg/m2 (range, 17–41 kg/m2). Twenty-one patients were male and 46 patients (69%) were female. Four of the five patients who underwent bilateral procedures were female. Mean time between operations for these patients was 21 months (range, 11–26 months).
Table 2.
Eligible patients for followup at 1, 2, and 5 years
| Most recent followup visit (years) | Number of eligible patients | Number of followups completed |
|---|---|---|
| 5 | 41 | 39 |
| 2 | 22 | 22 |
| 1 | 4 | 4 |
| Total for these intervals | 67 | 65 |
Description of Experiment, Treatment, or Surgery
The diagnosis of hip dysplasia was made based on clinical and radiographic analysis by the lead author (PEB). All patients were treated with PAO at a single center by the lead author using a single-incision technique using the Smith-Petersen interval and sparing of the abductors [19]. All the osteotomy cuts were done using fluoroscopy control with an intraoperative AP radiograph to assess final correction [16]. Osteochondroplasty of the head and neck junction was performed through arthrotomy in 68% of hips (49 of 72) for lack of femoral head/neck concavity (alpha angle > 50.5°) and/or femoral head asphericity predisposing to impingement postsurgical correction. Distal trochanteric transfer was performed in one hip. After surgery all patients were toe-touch weightbearing for 8 weeks and received thromboprophylaxis for 3 weeks using low-molecular-weight heparin. Outpatient physiotherapy was initiated at the 6-week mark.
Variables, Patient-reported Outcome Measures, Data Sources, and Bias
An independent observer (CD) performed radiographic measurements using standard AP, false profile, and Dunn views obtained during clinical follow up [17]. These included Tönnis angle (median, 15.3°; range, 0°–55°), minimum joint space width (median, 5 mm; range, 1–45 mm), center-edge angle [30] (median, 16.5°; range, −24° to 28°), presence of crossover sign (32.4%), and alpha angle [21, 25] (median, 52.8°; range, 29°–82°), with 57% of hips (41 of 72) having an alpha angle greater than 50.5°. Medial translation of the hip center was measured based on methods described previously by Clohisy et al. [6] and Troelsen et al. [27] as the difference between the horizontal distance from the most medial aspect of the femoral head to the ipsilateral ilioischial line measured on AP radiograph pre and post-PAO (median, 1.4 mm; range −4.5 to 8.7 mm).
Presence of osteoarthritis was assessed by the Tönnis grade [26]: no osteoarthritis (Grade 0); increased sclerosis of the head and acetabulum (Grade 1); small cysts in the femoral head or acetabulum, increased narrowing of joint space, and moderate loss of femoral head sphericity (Grade 2); large cysts in the head or acetabulum, severe joint space narrowing or obliteration, severe deformity of the femoral head; and or evidence of necrosis (Grade 3). Median Tönnis grade was 0 (range, 0–2).
Patient-reported outcome scores were collected preoperatively and at a minimum of 1 year postoperatively. These include the WOMAC [5], the UCLA Activity Scale [2], and the SF-12 [29]. Furthermore, using the previously published results of Garbuz et al. [9], we divided WOMAC outcome scores into three clinically relevant categories: poor (< 65), good (65–75), and very good (> 75).
Statistical Analysis, Study Size
Comparison of mean values for pre- and postoperative radiographic and questionnaire measurements was done using either paired t-test or Wilcoxon test. Multiple regression was used to determine which variables were a predictor of functional outcome scores. Basic patient demographic information (age, body mass index, and gender) as well as radiographic measurements (presence of crossover sign, Tönnis angle, minimum joint space, medial translation of the hip center) were included in the regression analysis. Kaplan-Meier analysis was conducted to calculate survivorship. An alpha value of 0.05 was used to determine a statistical difference. A power analysis was not done. All statistical analyses were performed using SPSS 22 (IBM, Armonk, NY, USA).
Results
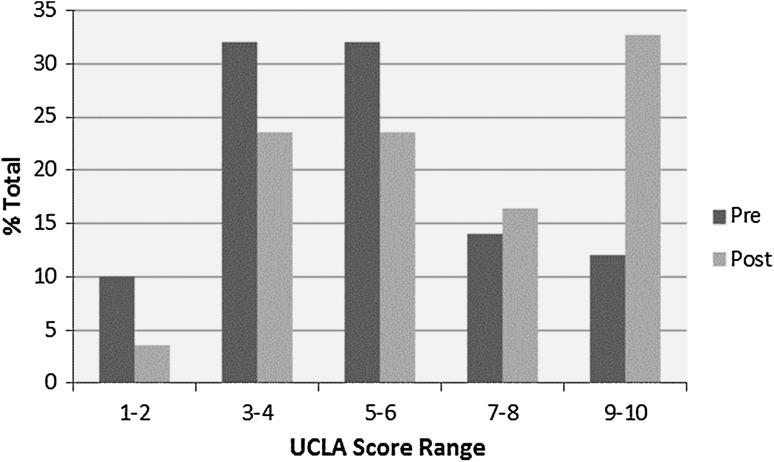
Most functional outcome scores consistently improved in this group of patients (Table 3). The overall WOMAC score improved from 54 to 74 (p < 0.001). The number of patients with “good” to “very good” [9] WOMAC scores (> 65) increased from 30% to 70% postoperatively (p < 0.001) (Table 4). SF-12 Physical Component score improved from 37 to 45 (p < 0.001), although the mental component scores showed no change (45–48, p = 0.207). UCLA activity score improved from 5 to 7 (p < 0.001) (Fig. 1). Radiographic comparison found improvements in median center-edge angle from 16.5° to 31.0° (range, 10.7°–49.0°; p < 0.001) as well as the Tönnis angle from 15.3° to 8.0° (range, −5° to 19°; p < 0.001). The median alpha angle fell from 52.8° to 45° (range, 31°–60°; p < 0.001). The median medial translation was 1.4 mm (range, −4.5 mm to 8.7 mm). Only 7% (five of 72) of hips had an alpha angle greater than 51° postsurgery, down from 57% (41) (Figs. 2, 3). Among demographic and radiographic measures, only center-edge angle after surgery and body mass index showed significant gender-related differences (Table 5).
Table 3.
Patient-reported outcome scores at pre- and postoperation
| Score | Mean preoperative (SD) | Mean postoperative (SD) | 95% CI of difference | p value |
|---|---|---|---|---|
| WOMAC | ||||
| Pain | 51.9 (21.9) | 75.3 (24.4) | 15.8–30.9 | < 0.001 |
| Stiffness | 47.6 (26.5) | 68.2 (18.8) | 13.0–28.2 | < 0.001 |
| Function | 59.8 (20.8) | 76.9 (23.4) | 10.2–24.1 | < 0.001 |
| Total | 53.9 (20.8) | 74.4 (21.6) | 14.1–26.9 | < 0.001 |
| UCLA | 5.3 (2.2) | 6.6 (2.6) | 0.5–2.1 | 0.002 |
| SF-12 | ||||
| Mental | 45.3 (11.5) | 48.0 (13.7) | −1.5 to 6.8 | 0.207 |
| Physical | 37.2 (9.5) | 44.9 (12.6) | 4.8–10.6 | < 0.001 |
CI = confidence interval.
Table 4.
Demographic breakdown based on WOMAC total outcome scores
| Demographic | Poor (< 65) | Good (65–75) | Very good (> 75) |
|---|---|---|---|
| Percent of total | 30.4 | 8.9 | 60.7 |
| Mean age (years) | 33.9 (11.3) | 33.2 (7.8) | 29.8 (7.8) |
| Mean body mass index (kg/m2) | 27.0 (6.3) | 28.1 (5.9) | 24.7 (4.8) |
| Gender (male/female) | 41.2%/58.8% | 40.0%/60.0% | 20.6%/79.4% |
Values in parentheses are SD.
Fig. 1.
The graph shows distribution of UCLA scores pre- and postoperation.
Fig. 2.

Radiographs from a 29-year-old woman with bilateral symptomatic hip dysplasia are shown. Inset shows preserved concavity at the anterior femoral head/neck junction. Alpha angle was 47° in the left hip and 55° in the right hip. WOMAC pain score was 65; WOMAC total score was 68.3.
Fig. 3.

Radiographs taken at 6 years postbilateral PAOs are shown. The patients has had two children by normal vaginal delivery. Alpha angle was 43° in the left hip and 34.3° in the right hip. WOMAC pain score has improved to 80; WOMAC total score has improved to 85.3.
Table 5.
Radiographic and demographic information broken down by gender
| Variable | Whole group | Female | Male | p value |
|---|---|---|---|---|
| CE angle | ||||
| Preoperative | 16.5 (−24.0 to −28.0) | 17.4 (−8.1 to 28.0) | 8.3 (−24.0 to 25.0) | 0.081 |
| Postoperative | 31.0 (10.7–49.0) | 32.7 (21.0–45.1) | 25.0 (10.7–49.0) | 0.015 |
| Tönnis angle | ||||
| Preoperative | 15.3 (0–55.0) | 14.0 (0–55.0) | 20.2 (9.0–33.0) | 0.062 |
| Postoperative | 8.0 (−5.0 to 19.4) | 6.8 (−5.0 to 19.0) | 9.0 (0–19.4) | 0.134 |
| Percent crossover | ||||
| Preoperative | 32.4 | 26.0 | 47.6 | 0.076 |
| Postoperative | 43.3 | 37.0 | 57.1 | 0.122 |
| Alpha angle | ||||
| Preoperative | 52.8 (29.0–82.0) | 48.0 (29.0–82.0) | 55.2 (36.1–80.0) | 0.427 |
| Postoperative | 45.0 (31.0–60.0) | 45.0 (34.0–55.0) | 45.0 (31.0–60.0) | 0.379 |
| Medial | ||||
| Translation (mm) | 1.4 (−4.5 to 8.7) | 1.3 (−2.6 to 7.7) | 1.9 (−4.5 to 8.7) | 0.723 |
| Mean age (years) (SD) | 31.2 (8.5) | 30.8 (8.1) | 32.2 (9.6) | 0.111 |
| BMI (kg/m2) | 24.6 (17.3–40.8) | 23.4 (17.3–40.8) | 26.6 (21.3–40.0) | 0.003 |
Unless otherwise indicated, median along with minimum and maximum values are presented. Probability value indicates the significance of gender-related differences; CE = center-edge; BMI = body mass index.
We found that among the factors we considered, only preoperative alpha angle was associated with lower WOMAC scores. No other demographic (age, gender, body mass index) or radiographic factors (presence of crossover sign, medial translation, Tönnis and center-edge angles) were found to be associated wither with lower scores. A higher alpha angle was found to be associated with lower WOMAC scores (β = −0.47; 95% confidence interval [CI], −0.92 to −0.02; R2 = 0.08; p = 0.04). When the WOMAC score was analyzed by subscales, higher alpha angle was a predictor of lower function (β = −0.59; 95% CI of β, −1.05 to −0.12; R2 = 0.12; p = 0.015) but was not correlated with pain or stiffness scores. No other demographic or radiographic factors were predictive of outcome scores. There was one conversion to THA at 86 months postoperatively. Additional reoperations include three hip arthroscopies (2.3, 2.5, and 4.9 years postoperatively). With reoperation (ie, hip arthroscopy and/or THA) used as the endpoint for failure, Kaplan-Meier survivorship at 5 years was 94.1% (95% CI, 90.7–97.5) and 86.3% (95% CI, 78.2%–94.4%) at 8 years. In terms of complications, there was one reoperation for excision of heterotopic ossification at 2 years and one patient had a femoral nerve palsy that fully recovered at 1 year.
Discussion
Hip dysplasia is a common pathology that causes substantial morbidity in the young adult population [12]. The Bernese PAO has become one of the most commonly used corrective osteotomy for treatment of this condition, but because this surgery can carry substantial risks [7], there is need for effective patient selection criteria. The purpose of this study was to determine the outcome of patients undergoing PAO for hip dysplasia at our center and to determine which factors were predictive for poor outcome. We found that patients undergoing PAO at our center have good midterm survivorship and improvements in functional scores. A higher alpha angle was found to be associated with lower WOMAC scores; no other demographic or radiographic variables were identified that were associated with lower patient-reported outcomes scores or reoperations.
This study has some limitations. First, all operations were performed in a single center by a single surgeon, which may affect the generalizability of our results. However, given that our surgical protocol and study population are similar to others found in the literature [15, 24, 27], our results may be representative, at least for high-volume subspecialty hip-preservation practices. Second, our study was a retrospective case series with no control. This type of study is inherently open to a variety of sources of bias, including selection bias, assessor bias, and transfer bias (loss to followup). We have tried to define the indications for PAO, which should mitigate the issue of selection bias. Assessor bias was limited by using self-reported outcome measures as well as independent assessor of radiographs. We note that two of 39 patients were lost to followup at 5 or more years. It is conceivable that these patients have had reoperations or conversions to THA done elsewhere. Third, this is a short-term followup study and does not give any information regarding medium- to long-term results. Again there are few long-term followup studies in the literature [1, 24] and short-term predictors of success have not been well described. Nonetheless, by categorizing our results into three groups, we were able to provide a better sense of the quality of outcomes after PAO and, more importantly, some further insight into predictors of outcome with poor femoral head sphericity leading to poorer functional outcome. However, our analysis is somewhat limited as a result of the limited number of negative outcomes (ie, low outcome scores or failure defined by reoperation). It is probable that our study is underpowered to detect less common sequelae.
Previous studies have shown that improvements in radiographic parameters such as acetabular inclination and center-edge angle are achieved consistently and reliably with the PAO [7]. This is consistent with our results, which show an improvement in postoperative center-edge angle, Tönnis angle, and alpha angle. The most commonly reported clinical outcome scores for PAO are the Harris hip score and the Merle D’Aubigné score [7]. In these studies the majority of patients had decreased pain and increased function at short- to midterm followup [7]. Our patients had improvements in self-reported outcome scores as measured by the WOMAC, UCLA, and SF-12 physical surveys. In 2008 Garbuz et al. [9] analyzed quality-of-life parameters after PAO and THA by breaking the WOMAC down into good/very good scores and poor scores. They found that 73% of patients rated good/very good on the WOMAC pain scale and 64% on the WOMAC function scale. In our study the percentage of patients with good to excellent WOMAC scores improved substantially postoperatively (70% versus 30%). This suggests that a majority of patients have good quality of life after PAO and that this represents a major change from preoperative status. Finally, the majority of studies have used THA as their endpoint and show a 5-year survivorship between 90% and 95%, which drops to 81% to 88% at 10 years (Table 1). In our cohort, there was only one conversion to THA. Given this low conversion rate to THA, a more meaningful measure of survivorship could count any reoperation as a failure. In 1995 Trousdale et al. [28] found a 21% failure rate using subsequent major surgery as their definition of failure. With this expanded definition, our failure rate is 5.6% (three arthroscopies and one THA).
Despite the evidence that suggests PAO can achieve reliable deformity correction and improved functional outcome measures, little is known about which patients stand to benefit the most predictably from this procedure. The majority of studies involving radiographic measures have not attempted to correlate these factors with clinical outcome [7]. Previous studies have identified several predictors of conversion to THA, including age older than 30 years and poor congruency (Table 6). In our study, we found that a higher alpha angle predicted lower postoperative WOMAC score. Although it is known that younger patients with no or mild preoperative arthritis have better functional outcome [7], this is the first radiographic predictor of postoperative function to our knowledge. Higher alpha angles have been shown to be associated with cam-type femoroacetabular impingement (FAI) [3, 4, 13, 20]. A recent study by Albers et al. [1] found that patients with residual bony deformities associated with FAI after PAO had decreased survivorship compared with those without impingement (87% versus 95%). These results suggest that outcome of PAO is affected by the presence of bony deformities associated with FAI both pre- and postoperatively. Furthermore, there is an established relationship between the presence of a cam deformity and the severity of cartilage damage [4], pointing to intraarticular cartilage pathology as a possible cause of poor outcome with PAO. In our study 68% of the hips received a concurrent osteochondroplasty. However, this procedure does not address pathology of the acetabular cartilage. Given that 60% of patients undergoing PAO have evidence of cartilage damage on arthroscopy [22], there may be a role for perioperative hip arthroscopy to address intraarticular pathology, particularly in patients with higher preoperative alpha angles.
Table 6.
Failure of PAO at mid- to long-term followup
| Study | Predictors of failure |
|---|---|
| Garras et al., 2007 [10] | None identified |
| Matheney et al., 2009 [15] | Age > 35 years at the time of surgery; poor or fair preoperative congruency; probability of failure was: 14% if none were present; 36% if one was present; 95% if the 2 were present; |
| Troelsen et al., 2009 [27] | CEA < 0°; postoperative sourcil width < 2.5 cm; presence of os acetabuli; postoperative distance to ilioischial line ≥ 2.0 cm |
| Steppacher et al., 2008 [24] | Age > 30 years; preoperative Merle d’Aubigne < 14; Tönnis grade ≥ 2; postoperative extrusion index of 20% or more |
| Albers et al., 2013 [1] | Age > 30 years; preoperative Merle d’Aubigne < 15; preoperative positive Trendelenburg sign; nonspherical head; preoperative OA Grade 1; Severin > Grade 3; excessive acetabular anteversion; acetabular retroversion; LCE > 22° (undercoverage); no offset correction in a nonspherical femoral head |
PAO = periacetabular osteotomy; CEA = center-edge angle; OA = osteoarthritis; LCE = lateral center-edge.
Patients who underwent PAO for hip dysplasia in this high-volume subspecialty setting had excellent survivorship and improvements in functional scores; this is consistent with other studies that evaluated some of those same endpoints [1, 15, 27]. PAO can be used to perform reliable correction of deformity with predictable improvements in center-edge angle, Tönnis angle, and alpha angle. These results are consistent with the other studies in which the consensus is that PAO is a reliable technique for correction of adult hip dysplasia [16, 27]. Interestingly, we found a higher alpha angle to be associated with a lower postoperative WOMAC score. Not only does this suggest that patients with a CAM deformity may have poorer outcomes with PAO, but it supports the role for addressing intraarticular hip pathology concurrently. Further research is needed to determine if preoperative alpha angle can reliably predict functional outcome and to clarify the role for adjunct hip arthroscopy with PAO.
Acknowledgments
We thank Drs Joel Matta and Jeffrey Mast for teaching the principles of joint-preserving surgery of the hip.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Albers CE, Steppacher SD, Ganz R, Tannast M, Siebenrock KA. Impingement adversely affects 10-year survivorship after periacetabular osteotomy for DDH. Clin Orthop Relat Res. 2013;471:1602–1614. doi: 10.1007/s11999-013-2799-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amstutz HC, Thomas BJ, Jinnah R, Kim W, Grogan T, Yale C. Treatment of primary osteoarthritis of the hip. A comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am. 1984;66:228–241. [PubMed] [Google Scholar]
- 3.Anderson LA, Peters CL, Park BB, Stoddard GJ, Erickson JA, Crim JR. Acetabular cartilage delamination in femoroacetabular impingement. Risk factors and magnetic resonance imaging diagnosis. J Bone Joint Surg Am. 2009;91:305–313. doi: 10.2106/JBJS.G.01198. [DOI] [PubMed] [Google Scholar]
- 4.Beaulé PE, Hynes K, Parker G, Kemp KA. Can the alpha angle assessment of cam impingement predict acetabular cartilage delamination? Clin Orthop Relat Res. 2012;470:3361–3367. doi: 10.1007/s11999-012-2601-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bellamy N, Wilson C, Hendrikz J. Population-based normative values for the Western Ontario and McMaster (WOMAC) Osteoarthritis Index: part I. Semin Arthritis Rheum. 2011;41:139–148. doi: 10.1016/j.semarthrit.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 6.Clohisy JC, Barrett SE, Gordon JE, Delgado ED, Schoenecker PL. Medial translation of the hip joint center associated with the Bernese periacetabular osteotomy. Iowa Orthop J. 2004;24:43–48. [PMC free article] [PubMed] [Google Scholar]
- 7.Clohisy JC, Schutz AL, St John L, Schoenecker PL, Wright RW. Periacetabular osteotomy: a systematic literature review. Clin Orthop Relat Res. 2009;467:2041–2052. doi: 10.1007/s11999-009-0842-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res. 1988;232:26–36. [PubMed] [Google Scholar]
- 9.Garbuz DS, Awwad MA, Duncan CP. Periacetabular osteotomy and total hip arthroplasty in patients older than 40 years. J Arthroplasty. 2008;23:960–963. doi: 10.1016/j.arth.2007.08.015. [DOI] [PubMed] [Google Scholar]
- 10.Garras D, Crowder T, Olson SA. Medium-term results of the Bernese periacetabular osteotomy in the treatment of symptomatic developmental dysplasia of the hip. J Bone Joint Surg Br. 2007;89:721–724. doi: 10.1302/0301-620X.89B6.18805. [DOI] [PubMed] [Google Scholar]
- 11.Hartig-Andreasen C, Troelsen A, Thillemann TM, Soballe K. What factors predict failure 4 to 12 years after periacetabular osteotomy? Clin Orthop Relat Res. 2012;470:2978–2987. doi: 10.1007/s11999-012-2386-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hickman JM, Peters CL. Hip pain in the young adult: diagnosis and treatment of disorders of the acetabular labrum and acetabular dysplasia. Am J Orthop. 2001;30:459–467. [PubMed] [Google Scholar]
- 13.Johnston TL, Schenker ML, Briggs KK, Philippon MJ. Relationship between offset angle alpha and hip chondral injury in femoroacetabular impingement. Arthroscopy. 2008;24:669–675. doi: 10.1016/j.arthro.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 14.Leunig M, Siebenrock KA, Ganz R. Rationale of periacetabular osteotomy and background work. J Bone Joint Surg Am. 2001;83:438–448. [PubMed] [Google Scholar]
- 15.Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am. 2009;91:2113–2123. doi: 10.2106/JBJS.G.00143. [DOI] [PubMed] [Google Scholar]
- 16.Matta JM, Stover MD, Siebenrock KA. Periacetabular osteotomy through the Smith-Petersen approach. Clin Orthop Relat Res. 1999;363:21–32. [PubMed] [Google Scholar]
- 17.Meyer DC, Beck M, Ellis T, Ganz R, Leunig M. Comparision of six radiographic projections to assess femoral head/asphericity. Clin Orthop Relat Res. 2006;445:181–185. doi: 10.1097/01.blo.0000201168.72388.24. [DOI] [PubMed] [Google Scholar]
- 18.Millis MB, Murphy SB, Poss R. Osteotomies of the hip joint for the prevention and treatment of osteoarthritis. Instr Course Lect. 1996;45:209–226. [PubMed] [Google Scholar]
- 19.Murphy SB, Millis MB. Periacetabular osteotomy without abductor dissection using direct anterior exposure. Clin Orthop Relat Res. 1999;364:92–98. doi: 10.1097/00003086-199907000-00013. [DOI] [PubMed] [Google Scholar]
- 20.Nepple JJ, Carlisle JC, Nunley RM, Clohisy JC. Clinical and radiographic predictors of intra-articular hip disease in arthroscopy. Am J Sports Med. 2011;39:296–303. doi: 10.1177/0363546510384787. [DOI] [PubMed] [Google Scholar]
- 21.Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 22.Ross JR, Zaltz I, Nepple JJ, Schoenecker PE, Clohisy JC. Arthroscopic disease classification and interventions as an adjunct in the treatment of acetabular dysplasia. Am J Sports Med. 2011;39:72s–78s. doi: 10.1177/0363546511412320. [DOI] [PubMed] [Google Scholar]
- 23.Santore RF, Dabezies EJJ. Femoral osteotomy for secondary arthritis of the hip in young adults. Can J Surg. 1995;38(Suppl 1):S33–S38. [PubMed] [Google Scholar]
- 24.Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633–1644. doi: 10.1007/s11999-008-0242-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tannast M, Siebenrock KA, Anderson S. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 26.Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. doi: 10.2106/00004623-199912000-00014. [DOI] [PubMed] [Google Scholar]
- 27.Troelsen A, Elmengaard B, Soballe K. Medium-term outcome of periacetabular osteotomy and predictors of conversion to total hip replacement. J Bone Joint Surg Am. 2009;91:2179. doi: 10.2106/JBJS.H.00994. [DOI] [PubMed] [Google Scholar]
- 28.Trousdale RT, Ekkernkamp A, Ganz R, Wallrichs SL. Periacetabular and intertrochanteric osteotomy for the treatment of osteoarthrosis in dysplastic hips. J Bone Joint Surg Am. 1995;77:73–85. doi: 10.2106/00004623-199501000-00010. [DOI] [PubMed] [Google Scholar]
- 29.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 30.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteoarthritis. Acta Chir Scand. 1939;83(Suppl 58):S2–S7. [Google Scholar]