Abstract
Background
Modular tapered stems have been suggested as the optimal implants for patients with severe femoral bone loss (Paprosky Type IIIB and IV) undergoing revision total hip arthroplasty (THA); however, there are few data describing survivorship and hip scores associated with this treatment.
Questions/purposes
At minimum 2 years, we sought to determine the (1) survivorship of these implants; (2) radiographic evidence of osseointegration; and (3) the Harris hip scores of patients revised with a modular tapered stem for severe femoral bone loss including the complications associated with their use.
Methods
Between 1999 and 2010, we performed 1124 femoral revisions; of those, 135 (12%) were performed using a modular tapered stem. General indications for use of this device included bone loss, poor quality bone, leg length discrepancy, difficulty adjusting version, proximal femoral remodeling, and ectatic medullary canals in the setting of revision THA. This report reviewed 70 of those that were performed in Type IIIB and IV femurs. Of those 70 patients, 11 had died and one was lost before 2-year followup; the remaining 58 (83%, 33 with a Type IIIB femur and 25 with a Type IV femur) were followed for a minimum of 24 months (average, 67 months; range, 24–151 months). Survivorship free from revision, radiographic analysis for signs of subsidence or stem loosening, and Harris hip scores were tallied.
Results
One patient underwent stem revision for early subsidence followed by failure of ingrowth for a survivorship free from repeat revision of 98% (57 of 58 patients). Five other stems (for a total of six [10%]) subsided early but nonetheless achieved radiographic signs of ingrowth and were not revised again. All other stems demonstrated osseointegration without subsidence and remained radiographically well fixed. In patients with surviving implants, the mean Harris hip score improved from 34 (range, 11–49) preoperatively to 74 (range, 14–100; p < 0.001) postoperatively. Overall, 15 of 58 patients (26%) experienced a complication, of whom 10 (17%) underwent reoperation.
Conclusions
We found that modular tapered stems resulted in 98% survivorship at a mean of 67 months in patients with Type IIIB and IV femurs undergoing femoral revision, although the overall complication rate in this complex subset of patients is high.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Revision THA in the setting of femoral bone loss is a difficult clinical problem with a variety of available treatment options including cemented stems [3, 6, 16], monoblock tapered stems [11, 14, 19], cylindrical stems [1, 2], modular tapered stems, proximal femoral-replacing prostheses, and the use of impaction grafting [15]. In general, cylindrical, nonmodular, fully porous, cobalt-chromium stems have been used as the workhorse of femoral revision surgery in North America with several studies demonstrating excellent results, particularly in Paprosky [23] Type I to IIIA femurs [8, 17, 19, 20, 22]. However, successful revision is more challenging in Paprosky Type IIIB and IV (Fig. 1A–B) femurs, because these patients have severe bone loss with minimal isthmus available for distal fixation of the revision stem. Sporer and Paprosky [26] found that 18% (two of 11) of patients treated with a fully porous-coated stem for revision of Type IIIB defects failed and 37.5% (three of eight patients) failed in Type IV defects. Additionally, there are a number of complications associated with use of these prostheses including thigh pain [14, 19], stress shielding [19], and intraoperative fractures [18, 29].
Fig. 1A–D.
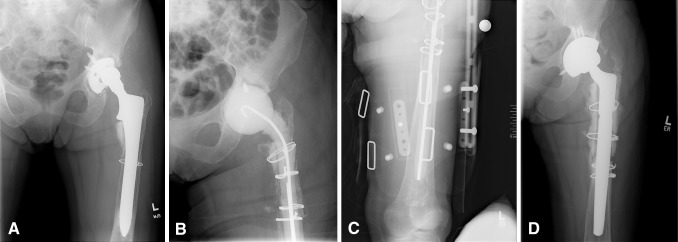
Case example shows a 70-year-old woman demonstrating the original prosthesis (A) that became infected and required treatment with removal and placement of an antibiotic spacer (B–C) with subsequent insertion of a modular tapered prosthesis (D).
Given these issues, modular tapered titanium stems have been suggested as an alternative solution for these more complex femoral defects. It has been suggested that the tapered distal geometry is better able to engage a short isthmic segment than a stem with a cylindrical distal geometry [24]. Furthermore, the modulus of elasticity of titanium is more similar to bone than other metals, which may decrease thigh pain and stress shielding. Additionally, modularity of the stem allows for impaction of the distal segment until secure axial stability is obtained and then using the varied available modular options in the proximal segment to adjust for leg length, offset, and version. However, there are few data describing survivorship and hip scores associated with this newer stem design in patients with severe femoral bone loss [21, 27, 28].
The purpose of this study was to determine, at minimum 2-year followup, the (1) survivorship of modular tapered implants used in the setting of severe femoral bone loss; (2) radiographic evidence of osseointegration of these stems; and (3) Harris hip scores, complications, and reoperations associated with use of these stems for complex femoral revisions.
Patients and Methods
Between February 1999 and January 2010, three fellowship-trained arthroplasty surgeons (CJDV, WP, SS) at one institution performed 1124 femoral revisions; of those, 135 (12.0%) were performed using a modular tapered stem. General indications for use of this device included bone loss, poor bone quality, leg length discrepancy, difficulty adjusting version, proximal femoral remodeling, and ectatic medullary canals in the setting of revision THA. This institutional review board-approved study reviewed the 70 that were performed in Paprosky Type IIIB and IV femurs. Eleven of 70 patients had died without 2-year followup, and one of 70 patients was lost to followup, leaving 58 patients (83%) for evaluation. The group consisted of 28 men and 30 women out of 58 patients with an average body mass index of 29 kg/m2 (range, 17–49 kg/m2) and age of 66 years (range, 45–89 years) at the time of surgery. Thirty-three patients had a Paprosky Type IIIB femur and 25 patients had a Paprosky Type IV femur (Fig. 1A–D). During this time an additional 39 stems with Type IIIB and IV femurs were revised at this center using other techniques but are not analyzed as part of this report. Nineteen of these were treated with a fully porous coated stem and previously described by Sporer and Paprosky [26].
The reasons for revision included aseptic loosening (37 of 58 patients), periprosthetic joint infection (10 of 58 patients), periprosthetic fracture (nine of 58 patients), and broken implants (two of 58 patients). All patients underwent revision THA with use of a modular tapered femoral prosthesis. Forty-one of 58 patients (71%) had a ZMR stem (Zimmer, Warsaw, IN, USA), 14 of 58 patients (24%) had a Restoration stem (Stryker, Mahwah, NJ, USA), and three of 58 patients (5%) had an MP reconstruction stem (Link, Hamburg, Germany). Minimum followup was 24 months (average, 68 months; range, 24–152 months). An extended trochanteric osteotomy was used as part of the surgical approach in 37 of 58 hips (64%).
Postoperatively, patients were evaluated clinically and radiographically at 3 weeks, 6 weeks, 3 months, 1 year, and annually thereafter. Radiographs at each visit were compared with initial postoperative radiographs to evaluate for femoral component subsidence, osseointegration, and implant failure. Whereas Engh et al. [7] have established radiographic criteria for evaluating cylindrical stems, there is no such established system for tapered stems. However, we used criteria similar to that used by the Revision Total Hip Arthroplasty Study Group [24] such that stems were considered osseointegrated if there was no subsidence, pedestal formation, or periprosthetic fracture. Patients were evaluated clinically using the Harris hip score [12] and were specifically queried regarding thigh pain and assessed for the occurrence of any complications. Descriptive statistics were used to analyze the data set. Student’s t-test was used to compare continuous variables with significance set at p = 0.05. Kaplan-Meier analysis was used to evaluate survivorship [13].
Results
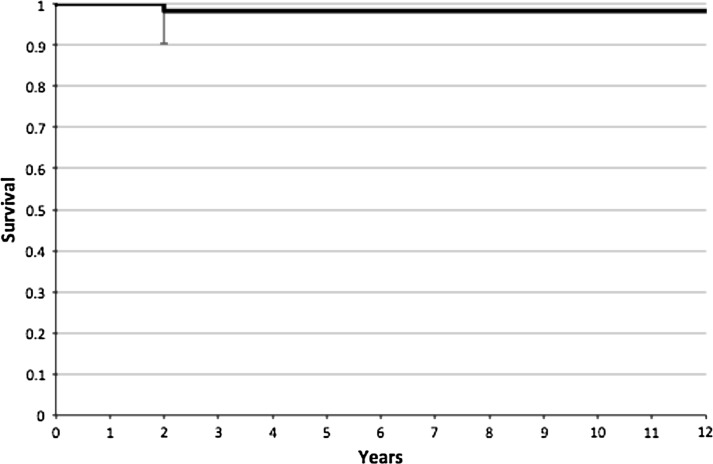
Kaplan-Meier survivorship (Fig. 2) was 98% at 12 years (95% confidence interval, 89.5%–99.5%). At the time of the most recent evaluation, one stem in one patient was considered a clinical failure. The stem in this patient failed to osseointegrate; the patient had persistent pain, leg length discrepancy, and poor ambulatory ability; and ultimately underwent a total femoral arthroplasty at an outside hospital 18 months postoperatively. No other stems were rerevised, and none of the 12 patients who had died or were lost to followup before 2 years were known to have had their stems revised.
Fig. 2.
Kaplan-Meier survival curve uses femoral stem revision as the endpoint.
Six of 58 stems (10%) subsided more than 4 mm within the first 3 months; however, the only stem that did not osseointegrate was in the patient who underwent revision surgery. The other five prostheses were clinically and radiographically stable at the latest examination. Of the stems with early subsidence, four were in Type IIIB femurs and two were in Type IV femurs. Additionally, three of 14 (28.6%) were Stryker Restoration stems and three of 41 (7.3%) were Zimmer ZMR stems (p = 0.17). The mean amount of subsidence in this group was 23 mm (range, 7–34 mm). Five of 37 (13.5%) femurs that were treated using an extended trochanteric osteotomy and one of 21 (5%) femurs revised without an extended osteotomy subsided more than 4 mm (p = 0.4).
The mean Harris hip score (HHS) improved from a mean preoperative value of 34 (range, 0–92) to a mean postoperative value of 74 (range, 5–100; p < 0.001). Eleven of 58 patients (19%) reported experiencing at least some thigh pain at their most recent postoperative visit.
Overall, 10 of 58 patients (17%) required reoperation including five exchanges of the modular head and liner for recurrent instability, two open reduction and internal fixation of postoperative periprosthetic supracondylar femur fractures, one acetabular revision for aseptic loosening, one irrigation and débridement of a superficial hematoma, and the one stem that was loose. Of the patients who had recurrent instability, none had stems that had subsided. Four of 58 patients (7%) had intraoperative femur fractures. One fracture occurred in the patient whose stem did not osseointegrate and required revision to a total femur, but the other three patients had no further issues. Additionally, there was one patient who dislocated but has not required revision and one nondisplaced periprosthetic fracture treated nonoperatively. Overall, 15 of 58 patients (26%) experienced a complication (Table 1). With the numbers available, there was no association between frequency of complications and stem type.
Table 1.
Summary of complications
| Complication | Number of patients |
|---|---|
| Head liner exchange for recurrent instability | 5 |
| Intraoperative fracture | 3 |
| ORIF supracondylar femur fracture | 2 |
| I&D of superficial hematoma | 1 |
| Dislocation not requiring revision | 1 |
| Nonoperatively treated periprosthetic fracture | 1 |
| Persistent femoral loosening, intraoperative fracture | 1 |
| Acetabular revision for aseptic loosening | 1 |
| Total | 15 |
ORIF = open reduction and internal fixation; I&D = irrigation and débridement.
Discussion
Revision THA in the setting of severe bone loss remains a challenge. Given the failures of monoblock cylindrical stems in patients with the most severe defects (Paprosky Type IIIB/IV) [26], it has been suggested that these patients may be best treated with a modular tapered stem; however, few studies have specifically studied this issue [21, 27, 28]. Stems with a tapered distal geometry may be able to gain stability in a shorter isthmic segment than a cylindrical stem, whereas their modularity allows the surgeon to adjust length, offset, and version. Furthermore, a titanium stem may decrease thigh pain and proximal stress shielding. The purpose of our study was to evaluate the survivorship free from repeat revision, radiographic signs of osseointegration, hip scores, and complications in a population of patients with severe bone loss whose femoral revisions were performed with a modular tapered stem.
One limitation to this study is the relatively high percentage of patients who had died or were lost to followup (12 of 70 [17%]). Although this does diminish our results to some degree, to our knowledge, none of the patients who had died or were lost to followup had undergone revision as of our last evaluation. Another limitation is that the data, although collected prospectively, were reviewed retrospectively. Every attempt was made to review patient records rigorously and objectively; however, the nature of retrospective review is such that bias can be introduced in the review and the data are not always accurate. Furthermore, our study was noncomparative and thus it is unknown if alternative treatment options would have led to similar outcomes. Similarly, selection bias may have been introduced because the most severe femoral defects may require more extensive treatment in the form of allograft-prosthetic composites, impaction grafting, or tumor prostheses. It is likely that patients selected for modular tapered implants were slightly healthier and had bone with sufficient quality to support distal fixation. Additionally, three different stems with varying design characteristics were used, but the relatively low numbers rendered it difficult to make any meaningful comparisons. Furthermore, our functional outcomes were only measured by HHS because this was the only outcomes tool consistently available during our retrospective review. A final limitation is the wide range of duration of patient followup. Although we had an average of followup time of over 5 years, the wide range (24–152 months) undermines the interpretation of longer-term survivorship. This is notable given that 10% of the radiographs demonstrated early subsidence. Whereas these patients clinically and radiographically appeared to subsequently osseointegrate, this group of patients is being followed closely.
The proportion of patients undergoing repeat revision after revision with a modular tapered stem was similar to previously published reports in which this stem type was used for revision surgery in the setting of Paprosky Type IIIB/IV bone loss. The authors of this paper [27] had previously reported on 16 patients treated in this manner and had only one failure, but this was with followup limited to a mean of 2 years. Palumbo et al. [21] reported on 18 patients with Paprosky Type IIIB/IV femurs treated with the Stryker Restoration modular tapered stems at a mean followup of 4.5 years. HHS increased from mean 56 to 79, and overall implant survival rate was 94% (17 of 18 patients). Van Houwelingen et al. [28] reported on 48 patients with Type 3B and 4 defects at a mean of 84 months followup. The implant survivorship in that series was 90% (43 of 48 patients) with several failures being the result of implant breakage.
Osseointegration of the implant is inherently associated with patient outcomes and survivorship because failure to achieve stable fixation often leads to pain and eventual revision. As noted by the results of our study as well as others [21, 28], early subsidence is relatively common with implants of this design. Although most of these stems stabilize and osseointegrate, leg length discrepancies can and do occur. Van Houwelingen et al. reported that all of the seven of 48 (15%) patients in their study who had early subsidence eventually achieved stability. In our study the average leg length discrepancy at most recent followup in patients with early subsidence was 25 mm. This is an important point because leg length discrepancy after THA has been associated with back pain [9], problems with gait [25], and dislocation [34] . However, other studies have found no correlation with outcomes [32, 33]. Comparisons to other studies are difficult, because most do not report leg length discrepancy. Weiss et al. [30] reported that only two of 63 patients (3%) had > 3 cm discrepancy and 30 of 63 patients (48%) had no discrepancy with the use of the Link MP prosthesis; however, the patient population in this study substantially differed from ours such that the bone loss was less severe in the majority of patients. Although design features of the implant (such as the degree of the taper, curvature of stem, and surface coating) may affect the frequency of this complication, we did not have large enough numbers to identify definitively which stem design characteristics were most advantageous. Future studies involving more hips might evaluate the association of the angle of the taper (an element of stem design) and the use of extended trochanteric osteotomy (a factor related to surgical approach) with subsidence. We do believe that care with surgical technique is also critical. Specifically, the surgeon should ensure that reaming is performed until cortical contact is achieved and the liberal use of intraoperative radiographs is suggested. Furthermore, the distal segment of the stem must be fully impacted until axial stability is achieved with the modular proximal body being used to restore appropriate leg length.
The overall proportion of patients experiencing complications (15 of 58 patients [26%]) and reoperation rate (10 of 58 patients [17%]) was relatively high; however, this is not unexpected given the complexity of the reconstructions and the poor medical condition of many of these patients. Furthermore, this complication rate is comparable to that found by Van Houwelingen et al. [28] who reported a 17% rate of intraoperative fracture (eight of 48 patients) and 10% dislocation rate (five of 48 patients) in addition to having five of 27 (19%) of the standard ZMR stems fracture. The most common reason for reoperation was instability, which in a recent large series [31] of revisions was seen in 10% with earlier papers showing even higher rates of dislocation in the revision population [4, 30]. Given the high risk, great care must be taken with trialing and we recommend the use of large-diameter femoral heads routinely [10]. However, this decision must take into consideration the possible risk of increased trunnion corrosion with larger head size [5]. Intra- and postoperative periprosthetic fractures were also seen commonly, which again is not surprising given the severe bone loss seen in this series. To prevent these fractures, we recommend that reaming be initiated by hand to ensure the reamer is centralized within the canal and the reamer should not be pushed deeper than the desired length of the revision stem to avoid the femoral bow. Furthermore, we routinely prophylactically place a cerclage wire just beyond the distal extent of the extended trochanteric osteotomy when used to protect the intact remaining femoral canal. Finally, we have seen these fractures occur during trialing or attempted reduction of the hip and the assistant must be warned that great care is required during this portion of the procedure.
In conclusion, modular tapered stems provided a low likelihood of revision at a minimum followup of 2 years, reliable osseointegration, and improvements in hip scores particularly when compared with an earlier report in which a cylindrical cobalt-chrome alloy stem was used in patients with Paprosky Type IIIB and IV femoral defects [26]. However, the overall rate of complications and reoperations in this complex patient population was substantial with dislocation and periprosthetic fractures being the most common complications observed. Although larger scale and longer-term studies are needed to better evaluate the survivorship and optimal design characteristics of these implants, based on these results, we continue to use modular tapered stems for the treatment of severe femoral bone loss.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Rush University Medical Center, Chicago, IL, USA.
References
- 1.Bohm P, Bischel O. Femoral revision with the Wagner SL revision stem: evaluation of one hundred and twenty-nine revisions followed for a mean of 4.8 years. J Bone Joint Surg Am. 2001;7:1023–1031. [PubMed] [Google Scholar]
- 2.Bohm P, Bischel O. The use of tapered stems for femoral revision surgery. Clin Orthop Relat Res. 2004;420:148–159. doi: 10.1097/00003086-200403000-00021. [DOI] [PubMed] [Google Scholar]
- 3.Cabanela ME, Trousdale RT, Berry DJ. Impacted cancellous graft plus cement in hip revision. Clin Orthop Relat Res. 2003;417:175–182. doi: 10.1097/01.blo.0000096817.78689.ac. [DOI] [PubMed] [Google Scholar]
- 4.Carter AH, Sheehan EC, Mortazavi SM, Purtill JJ, Sharkey PF, Parvizi J. Revision for recurrent instability: what are the predictors of failure? J Arthroplasty. 2011;6(Suppl):46–52. doi: 10.1016/j.arth.2011.03.021. [DOI] [PubMed] [Google Scholar]
- 5.Elkins JM, Callaghan JJ, Brown TD. Stability and trunnion wear potential in large-diameter metal-on-metal total hips: a finite element analysis. Clin Orthop Relat Res. 2014;472:529–542. doi: 10.1007/s11999-013-3244-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Engh CA, Glassman AH, Griffin WL, Mayer JG. Results of cementless revision for failed cemented total hip arthroplasty. Clin Orthop Relat Res. 1988;235:91–110. [PubMed] [Google Scholar]
- 7.Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990;257:107–128. [PubMed] [Google Scholar]
- 8.Engh CA, Jr, Ellis TJ, Koralewicz LM, McAuley JP, Engh CA., Sr Extensively porous-coated femoral revision for severe femoral bone loss: minimum 10-year follow-up. J Arthroplasty. 2002;8:955–960. doi: 10.1054/arth.2002.35794. [DOI] [PubMed] [Google Scholar]
- 9.Friberg O. Clinical symptoms and biomechanics of lumbar spine and hip joint in leg length inequality. Spine (Phila Pa 1976). 1983;6:643–651. [DOI] [PubMed]
- 10.Garbuz DS, Masri BA, Duncan CP, Greidanus NV, Bohm ER, Petrak MJ, Della Valle CJ, Gross AE. The Frank Stinchfield Award: Dislocation in revision THA: do large heads (36 and 40 mm) result in reduced dislocation rates in a randomized clinical trial? Clin Orthop Relat Res. 2012;470:351–356. doi: 10.1007/s11999-011-2146-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hamilton WG, Cashen DV, Ho H, Hopper RH, Jr, Engh CA. Extensively porous-coated stems for femoral revision: a choice for all seasons. J Arthroplasty. 2007;4(Suppl 1):106–110. doi: 10.1016/j.arth.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 12.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;4:737–755. [PubMed] [Google Scholar]
- 13.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. doi: 10.1080/01621459.1958.10501452. [DOI] [Google Scholar]
- 14.Krishnamurthy AB, MacDonald SJ, Paprosky WG. 5- to 13-year follow-up study on cementless femoral components in revision surgery. J Arthroplasty. 1997;8:839–847. doi: 10.1016/S0883-5403(97)90152-2. [DOI] [PubMed] [Google Scholar]
- 15.Lamberton TD, Kenny PJ, Whitehouse SL, Timperley AJ, Gie GA. Femoral impaction grafting in revision total hip arthroplasty: a follow-up of 540 hips. J Arthroplasty. 2011;8:1154–1160. doi: 10.1016/j.arth.2011.03.028. [DOI] [PubMed] [Google Scholar]
- 16.Lawrence JM, Engh CA, Macalino GE, Lauro GR. Outcome of revision hip arthroplasty done without cement. J Bone Joint Surg Am. 1994;7:965–973. doi: 10.2106/00004623-199407000-00002. [DOI] [PubMed] [Google Scholar]
- 17.McAuley JP, Engh CA., Jr Femoral fixation in the face of considerable bone loss: cylindrical and extensively coated femoral components. Clin Orthop Relat Res. 2004;429:215–221. doi: 10.1097/01.blo.0000150274.21573.f4. [DOI] [PubMed] [Google Scholar]
- 18.Meek RM, Garbuz DS, Masri BA, Greidanus NV, Duncan CP. Intraoperative fracture of the femur in revision total hip arthroplasty with a diaphyseal fitting stem. J Bone Joint Surg Am. 2004;3:480–485. doi: 10.2106/00004623-200403000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Moreland JR, Bernstein ML. Femoral revision hip arthroplasty with uncemented, porous-coated stems. Clin Orthop Relat Res. 1995;319:141–150. [PubMed] [Google Scholar]
- 20.Nadaud MC, Griffin WL, Fehring TK, Mason JB, Tabor OB, Jr, Odum S, Nussman DS. Cementless revision total hip arthroplasty without allograft in severe proximal femoral defects. J Arthroplasty. 2005;6:738–744. doi: 10.1016/j.arth.2004.12.053. [DOI] [PubMed] [Google Scholar]
- 21.Palumbo BT, Morrison KL, Baumgarten AS, Stein MI, Haidukewych GJ, Bernasek TL. Results of revision total hip arthroplasty with modular, titanium-tapered femoral stems in severe proximal metaphyseal and diaphyseal bone loss. J Arthroplasty. 2013;4:690–694. doi: 10.1016/j.arth.2012.08.019. [DOI] [PubMed] [Google Scholar]
- 22.Paprosky WG, Greidanus NV, Antoniou J. Minimum 10-year-results of extensively porous-coated stems in revision hip arthroplasty. Clin Orthop Relat Res. 1999;369:230–242. doi: 10.1097/00003086-199912000-00024. [DOI] [PubMed] [Google Scholar]
- 23.Paprosky WG, Lawrence JM, Cameron HU. Femoral defect classification: clinical application. Orthop Rev. 1990;9:33–44. [Google Scholar]
- 24.Revision Total Hip Arthroplasty Study Group A comparison of modular tapered versus modular cylindrical stems for complex femoral revisions. J Arthroplasty. 2013;8(Suppl):71–73. doi: 10.1016/j.arth.2013.04.052. [DOI] [PubMed] [Google Scholar]
- 25.Rosler J, Perka C. The effect of anatomical positional relationships on kinetic parameters after total hip replacement. Int Orthop. 2000;1:23–27. doi: 10.1007/s002640050006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sporer SM, Paprosky WG. Revision total hip arthroplasty: the limits of fully coated stems. Clin Orthop Relat Res. 2003;417:203–209. doi: 10.1097/01.blo.0000096803.78689.0c. [DOI] [PubMed] [Google Scholar]
- 27.Sporer SM, Paprosky WG. Femoral fixation in the face of considerable bone loss: the use of modular stems. Clin Orthop Relat Res. 2004;429:227–231. doi: 10.1097/01.blo.0000150120.80409.0d. [DOI] [PubMed] [Google Scholar]
- 28.Van Houwelingen AP, Duncan CP, Masri BA, Greidanus NV, Garbuz DS. High survival of modular tapered stems for proximal femoral bone defects at 5 to 10 years followup. Clin Orthop Relat Res. 2013;471:454–462. doi: 10.1007/s11999-012-2552-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Weeden SH, Paprosky WG. Minimal 11-year follow-up of extensively porous-coated stems in femoral revision total hip arthroplasty. J Arthroplasty. 2002;4(Suppl 1):134–137. doi: 10.1054/arth.2002.32461. [DOI] [PubMed] [Google Scholar]
- 30.Weiss RJ, Beckman MO, Enocson A, Schmalholz A, Stark A. Minimum 5-year follow-up of a cementless, modular, tapered stem in hip revision arthroplasty. J Arthroplasty. 2011;1:16–23. doi: 10.1016/j.arth.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 31.Wetters NG, Murray TG, Moric M, Sporer SM, Paprosky WG, Della Valle CJ. Risk factors for dislocation after revision total hip arthroplasty. Clin Orthop Relat Res. 2013;471:410–416. doi: 10.1007/s11999-012-2561-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.White TO, Dougall TW. Arthroplasty of the hip. Leg length is not important. J Bone Joint Surg Br. 2002;3:335–338. doi: 10.1302/0301-620X.84B3.12460. [DOI] [PubMed] [Google Scholar]
- 33.Whitehouse MR, Stefanovich-Lawbuary NS, Brunton LR, Blom AW. The impact of leg length discrepancy on patient satisfaction and functional outcome following total hip arthroplasty. J Arthroplasty. 2013;8:1408–1414. doi: 10.1016/j.arth.2012.12.009. [DOI] [PubMed] [Google Scholar]
- 34.Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982;9:1295–1306. [PubMed] [Google Scholar]