Abstract
Background
Cadaveric and clinical studies have suggested that, despite being touted as muscle-sparing, the direct anterior approach is still associated with muscle damage, particularly to the tensor fascia lata (TFL). Patient body mass index (BMI) and/or sex may also influence this parameter.
Questions/purposes
The purposes of the study were to determine if using a shorter femoral component reduces TFL damage or if patient sex or increasing BMI increases intraoperative TFL damage in direct anterior THA.
Methods
Over a 1-year period, 599 direct anterior THAs were performed by three experienced anterior hip surgeons; of those, 421 direct anterior hips had complete data (70%) and were included in the study. The amount of visible damage to the TFL was recorded before closure. Two stem types were used, a standard-length flat-wedge taper (standard) or a 3-cm shortened version of the same stem (short). Stem selection was based on timeframe of the surgery, surgeon preference, or matching a previous implant type. During the study period, the three surgeons performed an additional 225 primary THAs with other approaches such that the direct anterior approach represented 73% of the THAs performed. A member of the operating team, either a fellow or physician assistant, graded the extent of damage based on a 0 to 3 scale. On this scale, 0 represented no muscle fiber damage, 1 superficial tearing, 2 deep tearing or maceration, and 3 complete tear or severe damage. Patient sex and BMI were recorded and compared with stem type and muscle damage scores. An ordinal logistic regression model was used for statistical analysis.
Results
After controlling for relevant confounding variables using logistic regression, we found that mean muscle damage was associated with male sex (0.93, SD 0.76 versus 0.70, SD 0.68; p < 0.001) and increasing BMI levels (p < 0.001). As BMI increased, more muscle damage also was found in men compared with women (p = 0.05; odds ratio [OR], 1.029; 95% confidence interval [CI], 1.000–1.060). There was no overall difference in mean muscle damage between short and standard-length stems (0.78, SD 0.77 versus 0.85, SD 0.69, p = 0.32); however, as BMI increased, less damage was seen with a short stem (p = 0.04; OR, 0.968; 95% CI, 0.931–0.997).
Conclusions
Visible muscle damage occurred in most hips during anterior supine intermuscular hip arthroplasty. The clinical importance of this muscle damage requires further study, because some evidence suggests earlier restoration of gait and cessation of walking aids with direct anterior THA despite this damage; however, this was not studied here. Surgeons performing this approach can expect more difficulty and as a result possibly more damage to the TFL in patients with male sex and increased BMI. The use of a short stem can be considered for patients with increased BMI to limit damage to the TFL.
Level of Evidence
Level III, therapeutic study.
Introduction
The direct anterior approach for THA is an alternative to traditional surgical approaches that is performed through an internervous and intermuscular plane. This allows the surgeon to approach the hip without splitting or detaching any muscle from the pelvis or femur. The benefits of this approach have been suggested by multiple reports and may include decreased pain, rapid recovery, shorter hospital stay, low risk of dislocation, early cessation of ambulatory aids, and early gait improvement [1, 3, 4, 6–8, 11, 13–15, 17, 18, 21, 23–25, 28–30]. However, some reports have challenged these findings and suggested that the posterior or direct lateral approaches offer comparable results [10, 31, 33], and other studies suggest that the anterior approach is associated with muscle damage, particularly to the tensor fascia lata (TFL), despite it being touted as a muscle-sparing technique [16, 19].
Moreover, body mass index (BMI) and its association with increased surgical difficulty and complications with total joint arthroplasty are well known, and some have suggested that patients with higher muscle mass and BMIs may be at risk for a more difficult or complicated direct anterior procedure [5, 19] and conceivably more muscle damage with this approach. Short hip stems have been developed with the thought of easier insertion in patients with high BMI or in direct anterior or less invasive procedures. These stems have shown in the literature to have stable, dependable fixation and equivalent outcomes to standard-length stems [2, 12, 20, 26]. However, the degree to which they facilitate reduced muscle damage to the TFL in direct anterior hip surgery has not been demonstrated.
We therefore sought to determine whether stem style (3-cm shortened), sex, or BMI was associated with increasing amounts of muscle damage during direct anterior THA.
Patients and Methods
A series of 599 primary THAs were performed through the anterior approach by three experienced anterior hip surgeons (KRB, AVL, MJM) between October 2012 and September 2013. Of those, 421 direct anterior hips had complete data (70%) and were included in the study. There were also 225 primary THAs performed through the direct lateral approach during the study period; thus, 73% of hip surgeries were performed through the direct anterior approach. There were 225 female and 196 male patients included in the study. All devices used have been approved by the US Food and Drug Administration. The standard stem studied was the Taperloc® Complete (Biomet, Inc, Warsaw, IN, USA) and the shortened stem was the Taperloc® Complete Microplasty (Biomet, Inc), which is shortened 3 cm compared with the standard stem but maintains the same flat, tapered wedge proximal geometry (Fig. 1). The stem choice was made according to surgeon preference, preoperative templating, or matching a previous implant on the contralateral side. In general, one of the surgeons (AVL) prefers the shortened stem routinely for all hips, and the others (KRB, MJM) would consider the shortened stem for proximal femoral deformities or proximal-distal mismatches or perceived difficulty with exposure. Patients with large muscular hips, limited ROM, and femurs with short, varus necks tend to have more difficulties during exposure of the femur, and so patients with these characteristics may have been more likely to receive short stems during the study period. Two hundred fourteen standard-length stems and 207 shortened stems were used during the study.
Fig. 1A–B.

(A) The standard stem used was the Taperloc® Complete (Biomet, Inc, Warsaw, IN, USA), a flat, tapered, wedge titanium design with a porous plasma-sprayed coating applied proximally. (B) The shortened stem used was the Taperloc® Complete Microplasty (Biomet, Inc), which is shortened 3 cm compared with the standard stem but maintains the same flat, tapered, wedge proximal geometry. (Photographs reproduced courtesy of Biomet, Inc.)
All surgeries were performed with the anterior supine intermuscular approach on a standard radiolucent operating table using a table-mounted femoral elevator during femoral preparation. This technique has been described by the senior authors (KRB, AVL, MJM) in previous reports [5, 6, 30] and includes strict avoidance of posterior capsule, piriformis, or external rotator release to limit the risk of posterior dislocation. Prospective data were collected at the time of surgery including sex, BMI, and whether a standard-length stem or shortened stem was used, but this was a retrospective study.
An experienced member of the surgical team, either a fellow or physician assistant, then graded the presence and severity of TFL muscle damage to the anterior, medial, and deep surfaces after final implants were in position. A standardized grading system was used in all hips. A grade of 0 was given for completely intact muscle fibers without visible damage, 1 for small tearing in the superficial muscle fibers, 2 deep laceration or maceration of muscle fibers, and 3 for severe damage involving more than 50% of the muscle belly (Fig. 2).
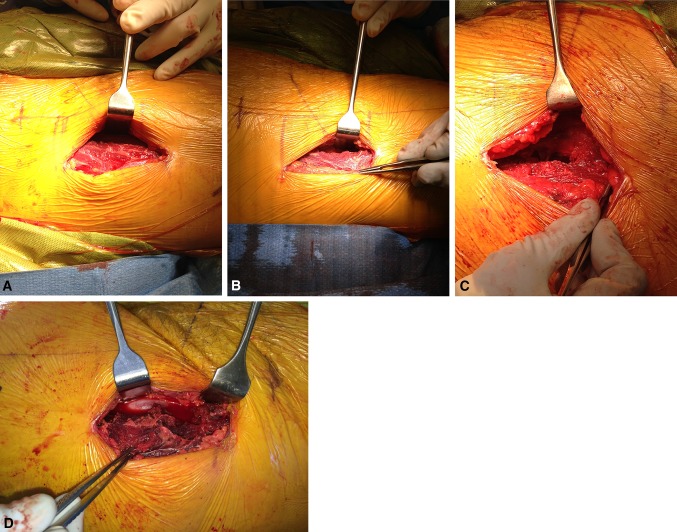
Fig. 2A–D.
Grading of tensor fascia lata muscle damage is shown: (A) 0, no damage, (B) 1, small superficial tearing, (C) 2, deep laceration, (D) 3, severe laceration involving 50% of muscle.
Statistical analysis was performed using an ordinal logistic regression model to determine whether controlling for other major variables affected the significance for stem size, BMI, and sex.
Results
Overall, we found no difference between the short and standard-length stems in terms of TFL damage (p = 0.32). The mean TFL damage score for the standard stem was 0.83 (SD 0.69) with a maximum score of 3 in five (2%), 2 in 39 (18%), and 1 in 108 of 214 THA (51%). The mean TFL damage score for the shortened stem was 0.78 (SD 0.77) with a maximum score of 2 in 25 (12%) and 1 in 89 of 207 THA (43%) (Table 1). However, when evaluating BMI and stem type, we found that as BMI increased, muscle damage was less when a short stem was used (p = 0.04; Table 1; odds ratio [OR], 0.968; 95% confidence interval [CI], 0.931–0.997). The overall mean damage score in this series was 0.81 (SD 0.73).
Table 1.
Tensor fascia lata (TFL) damage scores by sex and stem type
| Characteristic | Mean TFL score | 0 score (no damage) | 1 score (small superficial tear) | 2 score (deep laceration) | 3 score (severe > 50% of muscle) | p value |
|---|---|---|---|---|---|---|
| Sex | < 0.001 | |||||
| Males | 0.93 | 57/196 (29%) | 98/196 (50%) | 36/196 (18%) | 5/196 (3%) | |
| Females | 0.70 | 98/225 (44%) | 99/225 (44%) | 28/225 (12%) | 0/225 (0%) | |
| Stem type | 0.32 | |||||
| Standard stem | 0.83 | 62/214 (29%) | 108/214 (51%) | 39/214 (18%) | 5/214 (2%) | |
| Short stem | 0.78 | 93/207 (45%) | 89/207 (43%) | 25/207 (12%) | 0/207 (0%) | |
TFL damage was more prominent in males than it was in females (p < 0.001; OR, 0.869; 95% CI, 0.831–0.955). The mean TFL damage in female patients was 0.70 (SD 0.68) with the highest score of 2 in 28 of 225 (12%) and a score of 1 in 99 of 225 hips (44%). The mean TFL damage score in males was 0.93 (SD 0.76) with the highest score of 3 in five (3%), 2 in 36 (18%), and 1 in 98 of 196 hips (50%; Table 1).
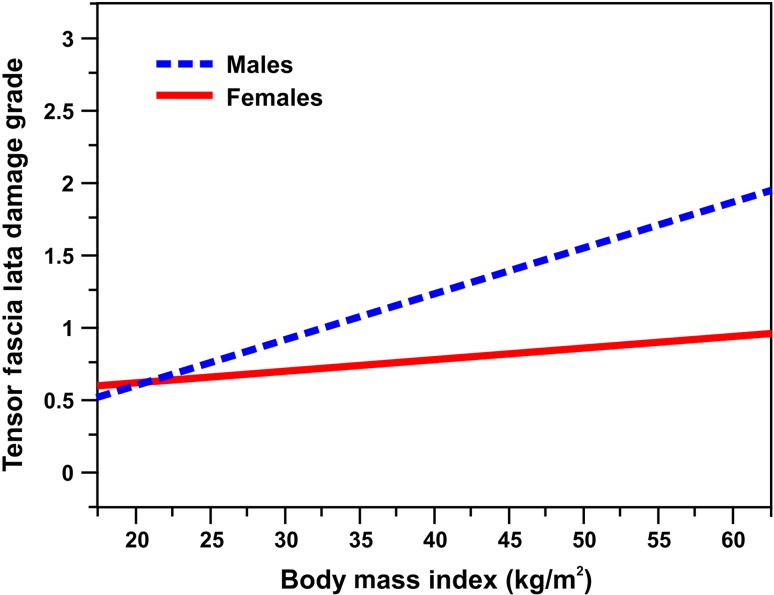
Using BMI as a continuous variable, we found that TFL damage increased directly as BMI increased (p < 0.001; OR, 1.019; 95% CI, 1.018–1.020), and higher muscle damage occurred in men as BMI increased compared with women (p = 0.049; OR, 1.029; 95% CI, 1.000–1.060) (Fig. 3).
Fig. 3.
Graph demonstrating relationship of TFL damage to BMI and sex.
Discussion
The internervous and intermuscular plane used in the direct anterior approach allows for THA to be performed without splitting or detaching muscles from the femur or pelvis. This procedure has shown improved gait patterns and rehabilitation, faster recovery, less pain, shorter hospital stay, and quicker cessation of ambulatory aids compared with other traditional approaches in some studies [1, 3, 4, 6, 7, 13–15, 21, 23–25], although other studies have questioned these findings, because most of the studies claiming benefits were not well controlled or randomized [10, 31, 33]. Moreover, others have raised concerns about whether this approach results in damage to the TFL [19], and some have suggested that particular patients such as muscular patients, those with higher BMI, and male patients may be at increased risk for muscle damage with this approach [6, 19]. For that reason, we sought to determine whether a shorter stem (designed with less invasive approaches in mind), patient sex, or BMI was associated with differences in muscle damage to the TFL in patients undergoing THA through the direct anterior approach. We found that increased TFL damage occurred with male patients and those with a higher BMI. This increased damage was more pronounced in male patients with high BMIs than their female counterparts. We also found that less damage occurred in patients with higher BMIs when a short stem was used.
There are limitations to this study. First, there was no initial power analysis performed. Also, the grading system used an estimation of the amount of damage to the TFL as opposed to a truly objective measurement of muscle quantity, and the assessment was made by members of the surgical team, leaving open the possibility of assessor bias and concerns about repeatability and validity of this classification. The true volume of muscle damage would be difficult to quantify in vivo as a result of limited exposure of the true muscle volume during actual surgery. The size of the TFL would also vary between patients making any method of measurement difficult. Another limitation is the number of team members grading each hip. Two fellows and three physician assistants participated in the study. There may have been inconsistency in grading between each person and intraobserver and interobserver reliability was not tested. Each member, however, was instructed on the appropriate grading method by the senior authors during the study. Also, the stem choice was not randomized. Stems were chosen according to surgeon preference, time of implantation, or stem style on a contralateral hip arthroplasty (Table 2). This could have allowed for bias in stem selection using a shortened stem for more difficult procedures. The incision length was not studied, because this could affect the amount of retraction needed on the TFL, thus affecting muscle damage. The surgeons participating in this study are all fellowship-trained hip surgeons with experience with the direct anterior approach and short stems who had completed their learning curves before this study (Table 2). The surgeons also operate with a team of experienced fellows and assistants. This may limit the generalizability to the community surgeon or hip surgeon without experience in this surgical approach going through the learning curve. MRI and enzyme markers were not used in this study nor were patient-reported outcome measures used to correlate with muscle damage scores. These measures could answer if various levels of TFL damage affect clinical recovery. Finally, this study does not report damage to other muscles including the rectus femoris. These data are being collected and will require future study.
Table 2.
Proportion of cases performed with the anterior supine approach, stem use, and muscle damage scores by individual surgeon
| Characteristic | Surgeon 1 | Surgeon 2 | Surgeon 3 | p value |
|---|---|---|---|---|
| Anterior approach cases before study period | 16 | 1630 | 259 | |
| Approach type during study period | < 0.001 | |||
| Anterior | 51/259 (20%) | 376/382 (98%) | 172/183 (94%) | |
| MIS direct lateral | 178/259 (69%) | 4/382 (1%) | 8/183 (4%) | |
| Direct lateral | 30/259 (12%) | 2/382 (<1%) | 3/183 (2%) | |
| Stem type | < 0.001 | |||
| Short | 3/183 (2%) | 155/304 (51%) | 26/90 (29%) | |
| Standard | 0/27 (0%) | 155/304 (51%) | 64/90 (71%) | |
| Tensor fascia lata damage score | ||||
| 0 | 7/27 (26%) | 117/304 (39%) | 30/90 (33%) | 0.322 |
| 1 | 14/27 (52%) | 135/304 (44%) | 48/90 (53%) | 0.284 |
| 2 | 4/27 (15%) | 48/304 (16%) | 12/90 (13%) | 0.849 |
| 3 | 2/27 (7%) | 3/304 (1%) | 0/90 (0%) | 0.007 |
MIS = minimally invasive surgery.
This is the first study we are aware of that specifically evaluates sex, BMI, stem type, and their relationships with muscle damage in direct anterior THA. However, other studies have been published examining muscle damage in various approaches to THA. One paper compared muscle damage between the direct anterior approach and the miniposterior approach [19]. This study found similar amounts of damage to the gluteus medius between the two approaches but found more damage to the gluteus minimus with the miniposterior approach. The authors noted that 50% of the anterior approach cadavers required complete release of the piriformis or conjoined external rotator tendon to mobilize the femur. This study showed damage to the TFL in every anterior approach cadaver with a mean of 31% of its muscular area and rectus femoris damage in some cadavers. Another study used cadaver specimens to compare muscle damage among a minimally invasive surgical (MIS) anterior, MIS anterolateral, MIS two-incision, MIS posterior, and traditional transgluteal approaches [32]. The authors found similar amounts of gluteus medius damage in all approaches except for the anterior approach, which completely spared the medius in four of five hips. This study found a similar surface area (35%) of the TFL damaged as found in the previously described study. The authors of these studies cited small numbers and different muscle consistency between cadaveric specimens and live patients as weaknesses of the studies.
Two papers used MRI to assess fatty atrophy in hip musculature after THA as a means to assess muscle damage. One study showed increased fatty atrophy of the gluteus medius with a modified Hardinge approach compared with a modified Watson-Jones approach where no muscle was detached from the femur [22]. This study also showed that no atrophy occurred in the TFL with the Watson-Jones approach and actually showed compensatory hypertrophy with the Hardinge approach. Another study showed increased fatty atrophy along with partial detachments of the gluteus medius and minimus with a transgluteal approach compared with a direct anterior approach [9]. Interestingly, this study showed that fatty atrophy of the TFL was no different in the direct anterior approach compared with transgluteal. A recent paper used inflammatory and muscle damage markers to evaluate muscle damage after direct anterior and miniposterior approaches for THA [7]. The authors concluded that the minor differences they observed in inflammatory markers may have been the result of the fact that bone preparation is similar between the groups and may be primarily responsible for their levels; however, the anterior approach group showed significantly less muscle damage than the posterior group as evidenced by the creatine kinase levels.
Men in our series had higher damage scores than women and more damage occurred in men with high BMIs than their female counterparts. This may correlate with BMI through higher muscle mass in men. This is consistent with another study showing equal relative hip muscle distribution in women and men but higher absolute muscle volumes and more muscle relative to BMI in men compared with women [27]. When controlling for other variables like sex and BMI, this study showed no overall differences in muscle damage when using a short versus standard length stem. However, the short stem did decrease the amount of damage seen in patients with high BMIs. The clinical importance of the muscle damage found in our study is unknown. Although the majority of hips demonstrated some form of visible muscle damage, this may not correlate with changes on MRI or serum markers as shown in other studies. Further study should be considered regarding the addition of posterior releases and their effects on damage scores, outcomes, and dislocation.
Our study found that some amount of visible TFL muscle injury occurs, although low, with the anterior approach with an overall average damage score of 0.81 and that increasing BMI was associated with increasing muscle damage. Unlike other authors who describe selective releases of the piriformis and external rotators [13, 17, 29], our technique strictly avoided their release to limit the risk of posterior dislocation. This may have contributed to higher amounts of retraction of the TFL in more difficult hips with higher BMI.
In summary, most patients who underwent the direct anterior approach experienced some amount of visible muscle damage although very mild. Future studies will need to determine what the clinical implications of this muscle damage might be, if any. A surgeon can expect increased difficulty and likely more muscle damage when operating on male and obese patients. The use of a shorter stem may help decrease muscle damage in these more difficult hips. Although surgeons earlier in their learning curves might find the shorter stem facilitates the direct anterior procedure for all patients, we found that in this small group of experienced surgeons, there was no discernible difference in muscle damage with the use of a shortened stem except in patients with high BMIs. Caution should be taken in changing both a surgical approach and stem at the same time. A surgeon considering adopting the direct anterior approach with a short stem should become comfortable with a short stem through his or her standard approach before changing approaches.
Acknowledgments
We thank Gerald Hobbs PhD, for his assistance in performing statistical analysis for this study.
Footnotes
One of the authors (KRB) certifies that he has or may receive payments or benefits, in any one year, an amount in excess of USD 1,000,000 from Biomet, Inc (Warsaw, IN, USA). One of the authors (AVL) certifies that he has or may receive payments or benefits, in any one year, an amount in excess of USD 1,000,000, from Biomet, Inc and Innomed, Inc (Savannah, GA, USA). The institution of the authors has received institutional research support from Biomet, Inc, Stryker (Mahwah, NJ, USA), and a grant from the Piedmont Orthopaedic Society (Durham, NC, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Joint Implant Surgeons, Inc, New Albany, OH, USA.
References
- 1.Alecci V, Valente M, Crucil M, Minerva M, Pellegrino CM, Sabbadini DD. Comparison of primary total hip replacements performed with a direct anterior approach versus the standard lateral approach: perioperative findings. J Orthop Traumatol. 2011;12:123–129. doi: 10.1007/s10195-011-0144-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Banerjee S, Pivec R, Issa K, Harwin SF, Mont MA, Khanuja HS. Outcomes of short stems in total hip arthroplasty. Orthopedics. 2013;36:700–707. doi: 10.3928/01477447-20130821-06. [DOI] [PubMed] [Google Scholar]
- 3.Barrett WP, Turner SE, Leopold JP. Prospective randomized study of direct anterior vs postero-lateral approach for total hip arthroplasty. J Arthroplasty. 2013;28:1634–1638. doi: 10.1016/j.arth.2013.01.034. [DOI] [PubMed] [Google Scholar]
- 4.Bender B, Nogler M, Hozack WJ. Direct anterior approach for total hip arthroplasty. Orthop Clin North Am. 2009;40:321–328. doi: 10.1016/j.ocl.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 5.Berend KR, Kavolus JJ, Morris MJ, Lombardi AV., Jr Primary and revision anterior supine total hip arthroplasty: an analysis of complications and reoperations. Instr Course Lect. 2013;62:251–263. [PubMed] [Google Scholar]
- 6.Berend KR, Lombardi AV, Jr, Seng BE, Adams JB. Enhanced early outcomes with the anterior supine intermuscular approach in primary total hip arthroplasty. J Bone Joint Surg Am. 2009;91(Suppl 6):107–120. doi: 10.2106/JBJS.I.00525. [DOI] [PubMed] [Google Scholar]
- 7.Bergin PF, Doppelt JD, Kephart CJ, Benke MT, Graeter JH, Holmes AS, Haleem-Smith H, Tuan RS, Unger AS. Comparison of minimally invasive direct anterior versus poster total hip arthroplasty based on inflammation and muscle damage markers. J Bone Joint Surg Am. 2011;93:1392–1398. doi: 10.2106/JBJS.J.00557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bhandari M, Matta JM, Dodgin D, Clark C, Kregor P, Bradley G, Little L. Outcomes following the single-incision anterior approach to total hip arthroplasty: a multicenter observational study. Orthop Clin North Am. 2009;40:329–342. doi: 10.1016/j.ocl.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 9.Bremer AK, Kalberer F, Pfirrmann CW, Dora C. Soft tissue changes in hip abductor muscles and tendons after total hip replacement: comparison between the direct anterior and the transgluteal approaches. J Bone Joint Surg Br. 2011;93:886–889. doi: 10.1302/0301-620X.93B7.25058. [DOI] [PubMed] [Google Scholar]
- 10.Duwelius PJ, Dorr LD. Minimally invasive total hip arthroplasty: an overview of the results. Instr Course Lect. 2008;57:215–222. [PubMed] [Google Scholar]
- 11.Goebel S, Steinert AF, Schillinger J, Eulert J, Broscheit J, Rudert M, Noth U. Reduced postoperative pain in total hip arthroplasty after minimal-invasive anterior approach. Int Orthop. 2012;36:492–498. doi: 10.1007/s00264-011-1280-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gustke K. Short stems for total hip arthroplasty: initial experience with the Fitmore stem. J Bone Joint Surg Br. 2012;94(Suppl A):47–51. doi: 10.1302/0301-620X.94B11.30677. [DOI] [PubMed] [Google Scholar]
- 13.Kennon RE, Keggi JM, Wetmore RS, Zatorski LE, Huo MH, Keggi KJ. Total hip arthroplasty through a minimally invasive anterior surgical approach. J Bone Joint Surg Am. 2003;85(Suppl 4):39–48. doi: 10.2106/00004623-200300004-00005. [DOI] [PubMed] [Google Scholar]
- 14.Klausmeier V, Lugade V, Jewett BA, Collis DK, Chou LS. Is there faster recovery with an anterior or anterolateral THA? A pilot study. Clin Orthop Relat Res. 2010;468:533–541. doi: 10.1007/s11999-009-1075-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lugade V, Wu A, Jewett B, Collis D, Chou LS. Gait asymmetry following an anterior and anterolateral approach to total hip arthroplasty. Clin Biomech. 2010;25:675–680. doi: 10.1016/j.clinbiomech.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 16.Mardones R, Pagnano MW, Nemanich JP, Trousdale RT. The Frank Stinchfield Award: Muscle damage after total hip arthroplasty done with the two-incision and mini-posterior techniques. Clin Orthop Relat Res. 2005;441:63–67. doi: 10.1097/01.blo.0000194727.55372.04. [DOI] [PubMed] [Google Scholar]
- 17.Matta JM, Shahrdar C, Ferguson T. Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop Relat Res. 2005;441:115–124. doi: 10.1097/01.blo.0000194309.70518.cb. [DOI] [PubMed] [Google Scholar]
- 18.Mayr E, Nogler M, Benedetti MG, Kessler O, Reinthaler A, Krismer M, Leardini A. A prospective randomized assessment of earlier functional recovery in THA patients treated by minimally invasive direct anterior approach: a gait analysis study. Clin Biomech. 2009;24:812–818. doi: 10.1016/j.clinbiomech.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 19.Meneghini RM, Pagnano MW, Trousdale RT, Hozack WJ. Muscle damage during MIS total hip arthroplasty: Smith-Peterson versus posterior approach. Clin Orthop Relat Res. 2006;453:293–298. doi: 10.1097/01.blo.0000238859.46615.34. [DOI] [PubMed] [Google Scholar]
- 20.Molli RG, Lombardi AV, Jr, Berend KR, Adams JB, Sneller MA. A short tapered stem reduces intraoperative complications in primary total hip arthroplasty. Clin Orthop Relat Res. 2012;470:450–461. doi: 10.1007/s11999-011-2068-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moskal JT. Anterior approach in THA improve outcomes: affirms. Orthopedics. 2011;34:e456–e458. doi: 10.3928/01477447-20110427-20. [DOI] [PubMed] [Google Scholar]
- 22.Muller M, Tohtz S, Dewey M, Springer I, Perka C. Evidence of reduced muscle trauma through a minimally invasive anterolateral approach by means of MRI. Clin Orthop Relat Res. 2010;468:3192–3200. doi: 10.1007/s11999-010-1378-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Muller M, Tohtz S, Dewey M, Springer I, Perka C. Age-related appearance of muscle trauma in primary total hip arthroplasty and the benefit of a minimally invasive approach for patients older than 70 years. Int Orthop. 2011;35:165–171. doi: 10.1007/s00264-010-1166-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nakata K, Nishikawa M, Yamamoto K, Hirota S, Yoshikawa H. A clinical comparative study of the direct anterior with mini-posterior approach: two consecutive series. J Arthroplasty. 2009;24:698–704. doi: 10.1016/j.arth.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 25.Palieri G, Vetrano M, Mangone M, Cereti M, Bemporad J, Roselli G, D’Arrigo C, Speranza A, Vulpiani MC, Ferretti A. Surgical access and damage extent after total hip arthroplasty influence early gait pattern and guide rehabilitation treatment. Eur J Phys Rehabil Med. 2011;47:9–17. [PubMed] [Google Scholar]
- 26.Patel RM, Lo WM, Cayo MA, Dolan MM, Stulberg SD. Stable, dependable fixation of short-stem femoral implants at 5 years. Orthopedics. 2013;36:e301–e307. doi: 10.3928/01477447-20130222-18. [DOI] [PubMed] [Google Scholar]
- 27.Preininger B, Schmorl K, von Roth P, Winkler T, Matziolis G, Perka C, Tohtz S. The sex specificity of hip-joint muscles offers an explanation for better results in men after total hip arthroplasty. Int Orthop. 2012;36:1143–1148. doi: 10.1007/s00264-011-1411-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Restrepo C, Mortazavi SM, Brothers J, Parvizi J, Rothman RH. Hip dislocation: are hip precautions necessary in anterior approaches? Clin Orthop Relat Res. 2011;469:417–422. doi: 10.1007/s11999-010-1668-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Restrepo C, Parvizi J, Pour AE, Hozack WJ. Prospective randomized study of two surgical approaches for total hip arthroplasty. J Arthroplasty. 2010;25:671–679. doi: 10.1016/j.arth.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 30.Seng BE, Berend KR, Ajluni AF, Lombardi AV., Jr Anterior-supine minimally invasive total hip arthroplasty: defining the learning curve. Orthop Clin North Am. 2009;40:343–350. doi: 10.1016/j.ocl.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 31.Sculco TP. Anterior approach in THA improves outcomes: opposes. Orthopedics. 2011;34:e459–e461. doi: 10.3928/01477447-20110714-29. [DOI] [PubMed] [Google Scholar]
- 32.Van Oldenrjk J, Hoogland PV, Tuijthof GJ, Corveleijn R, Noordenbos TW, Schafroth MU. Soft tissue damage after minimally invasive THA: a comparison of 5 approaches. Acta Orthop. 2010;81:696–702. doi: 10.3109/17453674.2010.537804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ward SR, Jones RE, Long WT, Thomas DJ, Dorr LD. Functional recovery of muscles after minimally invasive total hip arthroplasty. Instr Course Lect. 2008;57:249–254. [PubMed] [Google Scholar]