Abstract
Background
Femoral revision using fully coated femoral components offers distinct advantages in patients with notable bone loss. With the increasing concerns being raised about the problems of stem modularity, the results and complications of revision arthroplasty using devices with limited modularity are important.
Questions/purposes
We therefore asked: (1) What is the frequency of infection, aseptic loosening, and reoperations after use of these components? (2) What is the frequency of intraoperative fracture of the femur when using these components and are there any identifiable factors related to these fractures? (3) What is the 10-year survivorship of these components, and are there any identifiable factors related to survival and rerevision?
Methods
We retrospectively reviewed prospectively obtained data on 96 patients undergoing 104 revisions with fully coated components of two different manufacturers; six patients had died (6%) and six were lost to followup (6%) before 2 years. Data on intraoperative fracture, aseptic loosening, and reoperation were analyzed. Ninety-two hips, with a minimum followup of 2 years (mean, 8 years; range, 2–16 years), were evaluated for radiographic evidence of loosening. Intraoperative fracture frequency and Kaplan-Meier survivorship was calculated to 10 years for the entire cohort of 104 hips. Demographic, radiographic, and operative factors associated with implant survival and intraoperative fracture were analyzed using chi-square and Wilcoxon tests.
Results
There were three infections, nine hips (10%) had femoral component loosening (six rerevised), and there were seven other reoperations. Intraoperative complications in 17 hips (17%; 11 diaphyseal fractures, four perforations, two proximal fractures) were treated with allograft strut and cable fixation in 14 hips. Intraoperative femoral complication was more likely with the use of a curved stem [17 of 76, 22% curved; 0 of 28 straight stems (p = 0.005)]. With failure defined as femoral component revision for aseptic loosening or radiographic evidence of loosening, implant survival was 88% at 10 years. Those femurs with Paprosky Grades 3B and 4 defects had a higher risk of loosening (3 of 10 for Grades 3B and 4 versus 6 of 94 hips [6%] for Grades 1, 2, 3A; p = 0.03).
Conclusions
As concerns about stems with more modularity become more prominent, we find the durability of the approach using fully coated femoral components reassuring, but we will continue to follow these patients in the longer term.
Level of Evidence
Level IV, therapeutic study. See Instructions for Authors for a complete description of levels of evidence.
Introduction
A variety of methods of fixation for the femoral component during revision THA have been proposed, including cement, cement with impaction grafting, proximally porous-coated components, distal fixation of extensively coated components, distal fixation of modular body porous or fluted components, and allograft-prosthetic composites [11]. Femoral revision using a nonmodular body extensively coated component offers distinct advantages for both the experienced and occasional revision surgeon in hips with notable bone loss and where the proximal femur is nonsupportive. Surgeons and operating room staff are familiar with the techniques of femoral intramedullary reaming, broaching, and the insertion technique is relatively straightforward.
During the past 5 years, there has been more emphasis on the use of femoral components with modularity of the stem’s body (whether extensively coated or distally tapered and fluted) for revision arthroplasty because of the presumed advantages of modularity [9, 10]. However, these modular components add the complications of difficulty with modular junction engagement and the possibility of modular taper corrosion and fracture [9, 10]. There is a relatively long history of bone ingrowth into a femoral component coated with small beads, and the results of the first decade of use have been favorable [8, 9, 13]. However, there remain concerns about the use of these components in hips with advanced femoral bone loss, late stress shielding, fracture of smaller-sized components with distal fixation, and fracture with insertion [11, 12, 14, 15].
We therefore asked the following questions: (1) What is the frequency of infection, aseptic loosening, and reoperations after use of these components? (2) What is the frequency of intraoperative fracture or perforation of the femur when using these components and are there any identifiable factors related to these fractures? (3) What is the 10-year survivorship of these components, and are there any identifiable factors related to survival and rerevision?
Patients and Methods
This is a retrospective study of prospectively collected data on 96 patients who had 104 femoral revisions with a nonmodular body fully coated prosthesis, with modularity only of the femoral head-trunnion junction, between July 1996 and July 2010 by the senior author (PFL). During the same time period, 35 other revisions were performed with other techniques: 28 cemented, three cemented with impaction grafting, two cement into cement, one total femur, and one proximally coated component (failed resurfacing). During the period in question, we generally used the fully coated component in younger patients, with varying degrees of bone loss, in which we could template reasonable fixation. Older patients without bone loss were frequently treated with cemented components. No femoral components with modularity other than the head-trunnion junction were implanted.
Six patients (six hips, 6%) had died and six patients (six hips, 6%) were lost or refused to return for followup less than 2 years postoperatively. These 12 hips and their complications were included in the analyses of survivorship and intraoperative femoral complications. After these exclusions, the remaining 84 patients (92 hips) had complete clinical and radiographic data at 2 to 16 years (mean, 8 years). The cohort with at least 2 years’ followup contained 47 male patients (52 hips) and 37 female patients (40 hips) with a mean age of 60 years (range, 30–85 years). The mean patient weight was 81 kg (range, 40–103 kg) and the mean patient BMI was 28 kg/m2 (range, 17–44 kg/m2).
The indication for the revision was painful aseptic loosening in 61 hips (66%), infection in 17 (19%), periprosthetic fracture with loosening in eight (9%), severe polyethylene wear in five (5%), and chronic pain due to presumed fibrous ingrowth in one (1%). The procedure was the first femoral revision in 54 hips (60%), the second revision in 29 (31%), the third revision in four (4%), and the fourth revision in five (5%). The index femoral component was uncemented in 54 hips and cemented in 38 hips. All 17 of the hips treated for infection underwent a two-stage reimplantation, with or without an antibiotic cement spacer. Fifty-one patients (54 hips) were included in a previous study of intraoperative fracture of the femur in revision hip arthroplasty [2]; the mean followup in that series was 3 years (range, 1 to 6 years), while in the current report mean followup of those 51 patients was 8 years (range, 1 to 16 years). In addition, for the current report, we have enlarged the overall study cohort. Data were prospectively collected in an institutional review board-approved practice study incorporating clinical and radiographic data collection.
One surgeon performed all 92 revision hip arthroplasties with use of fully coated cobalt-chrome beaded components, with modularity only of the head-trunnion junction, from two manufacturers: Solution® (Johnson & Johnson DePuy, Warsaw, IN, USA) (n = 51) and Versys® (Zimmer, Inc, Warsaw, IN, USA) (n = 41). Both of these designs are available in 6- and 8-inch straight components, 8- and 10-inch curved components, and 7.5-inch straight and 10-inch curved calcar body components. There are slight differences between the two manufacturers’ components, including a beveled anterior stem tip and 15° neck anteversion for the 8- and 10-inch curved components in the Versys® design. In 41 hips, this was an isolated femoral component revision, and in 41 hips, the acetabular component was also revised. These two stems were performed in consecutive groups, with all the Solution stems performed first, and all the Versys stems thereafter, based upon the hope that the distal stem modification would decrease the frequency of intraoperative femoral complication. The groups of patients receiving each stem were not different in terms of age, sex, BMI, use of curved stem and Paprosky bone defect grade. The femoral head size was 26-mm in 9 hips, 28-mm in 33 hips, 32-mm in 32 hips, 36-mm in 13 hips and 40-mm in 5 hips.
The procedures were performed with use of an extensile posterior approach in 74 hips, extended trochanteric osteotomy in eight, trochanteric slide in eight, and a standard trochanteric osteotomy in two. The techniques for the trochanteric osteotomies and for the prosthesis implantation have been previously described [1, 3, 7]. After removal of the index femoral component and underlying membrane, the femur was prepared with flexible (for all curved stems) and rigid (for straight and occasionally for curved stems) intramedullary reamers and appropriate rasps. Femoral bone loss was classified according to the method of Paprosky et al. [3, 9, 11] on the basis of both preoperative radiographs and intraoperative findings. The bone loss was Paprosky Grade 1 in three hips (3%), Grade 2 in eight (9%), Grade 3A in 71 (77%), Grade 3B in seven (8%), and Grade 4 in three (3%). The femoral component was curved in 68 hips and straight in 24 hips. The size and length of the femoral component was based on preoperative templating (to achieve 4 to 6 cm of “scratch fit”) [9] and intraoperative fit, and ranged from 11-mm to 22.5-mm. Some bone grafting was performed in all hips, with crushed cancellous allograft proximally in all hips and one or two allograft struts in 26 hips. The amount of press-fitting was based on bone quality and surgeon judgment and was line to line in 64 hips, 0.5-mm overreamed in 16, 1-mm overreamed in five, 0.5-mm underreamed in four, 1-mm underreamed in one, 2-mm underreamed in one, and not recorded for one. After placement of the femoral component, routine AP and lateral radiographs, including the tip of the stem, were performed intraoperatively to specifically identify a fracture of the femur. If identified, the fracture or perforation was repaired e with one or two allograft struts and cable fixation. One fracture of the distal femur occurred during exposure of a stiff hip and was treated with a plate and screws.
The patients started ambulation, partial weightbearing, with a walker on the first postoperative day. The patients continued use of a walker or two crutches for 6 weeks and then progressed to a single cane, which was recommended for an additional 6 weeks. Those patients who had a standard or extended trochanteric osteotomy were advised a walker or two crutches for 12 weeks and then a cane for an additional 6 weeks. All patients received supervised physical therapy twice daily while in the hospital. Formal physical therapy was usually not prescribed after discharge.
Patients were requested to return for examination and radiographs at 6 weeks, 12 weeks, 6 months, 1 year, and annually (or biannually) thereafter. Patients who were not seen within 1 year were recalled for examination and radiographs. For the purposes of this study, we defined adverse clinical outcomes as deep infection, implant loosening requiring rerevision, reoperation for any other reason (polyethylene wear, acetabular component loosening, recurrent dislocation, or periprosthetic fracture), and intraoperative fracture of the femur. Infection was a clinical diagnosis based on a combination of hip aspiration and intraoperative culture in addition to laboratory tests (erythrocyte sedimentation rate, C-reactive protein). Standardized supine AP radiographs of the pelvis and entire femur and frog leg lateral radiographs were made by technicians specifically trained in making these radiographs and with similar patient and tube positioning. Both authors reviewed the radiographs at the same time for radiolucent lines and subsidence (defined as > 3-mm difference). Any differences between observers were resolved by consensus. Any component that subsided or had “fibrous fixation” was considered radiographically loose.
We collected and analyzed the following descriptive variables: Patient sex, age, BMI, surgical approach (posterior compared with any trochanteric osteotomy), type of femoral component (curved compared with straight stem, standard tip compared with beveled tip), Paprosky grade (Grades 1, 2, and 3A compared with Grades 3B and 4), and occurrence of an intraoperative fracture of the femur. Survival analysis using Kaplan-Meier analysis was performed at 10 years. For one curve, we defined failure as revision of the femoral component for aseptic loosening or definite radiographic loosening. For the second curve, we defined failure as reoperation for any reason (including femoral revision, polyethylene wear, acetabular component loosening, recurrent dislocation, and internal fixation of a femur fracture). Patients were censored at the time of death or at 15 years of followup. For each definition of failure, bivariate survival comparisons were made for each of the three dichotomized variables listed above using the nonparametric Wilcoxon test. The association of each of the seven variables listed above with intraoperative fracture or perforation of the femur was analyzed with the chi-square test for dichotomized variables (with Fisher’s exact test being used for small group sizes) and the nonparametric Wilcoxon rank-sum test for continuous variables.
Results
There were no early infections and three late hematogenous infections. Two of these were treated with débridement, liner and head exchange, and antibiotic therapy. One late infection occurred in a patient with hemophilia and was treated with a resection arthroplasty. Nine patients had aseptic loosening of the femoral component (10%) and six had rerevision. In three patients, symptoms were considered mild and the patients declined revision. There were seven other patients who had reoperations: Two had liner-head exchange for recurrent dislocation, three had revision of a loose acetabular component, and two had late fixation of a periprosthetic fracture of the femur distal to the implant tip. Overall, there were six dislocations in the entire cohort of 104 hips.
Intraoperative complications related to the femur occurred in 17 of 104 hips (16.7%). There were 11 femoral shaft fractures at or distal to the tip, four perforations of the femoral canal, and two fractures of the proximal femur. In 14 hips, one or two allograft struts and cables were placed, and the two proximal fractures had cerclage wire or cable fixation. One of these patients also had a late additional fracture between a 10-inch curved stem and the femoral stem of a constrained-condylar knee prosthesis and was treated with a custom intercalated intramedullary device. All fractures occurred with the use of curved stems. Curved stems were associated with a greater likelihood of intraoperative fracture of the femur or perforation [17 of 76, 22% curved; 0 of 28 straight]; (p = 0.005). There were no differences between the stems in terms of the frequency of intraoperative femoral complication (Solution® stem 24% [13 of 54], Versys® beveled tip stem 8% [4 of 50]; [p = 0.24]). With the numbers available, there was no association between patient age (p = 0.96), sex (p = 0.43), preoperative Paprosky grade (p = 0.31), femoral stem diameter (p = 0.13), or femoral head size (p = 0.49) and intraoperative fracture or perforation of the femur.
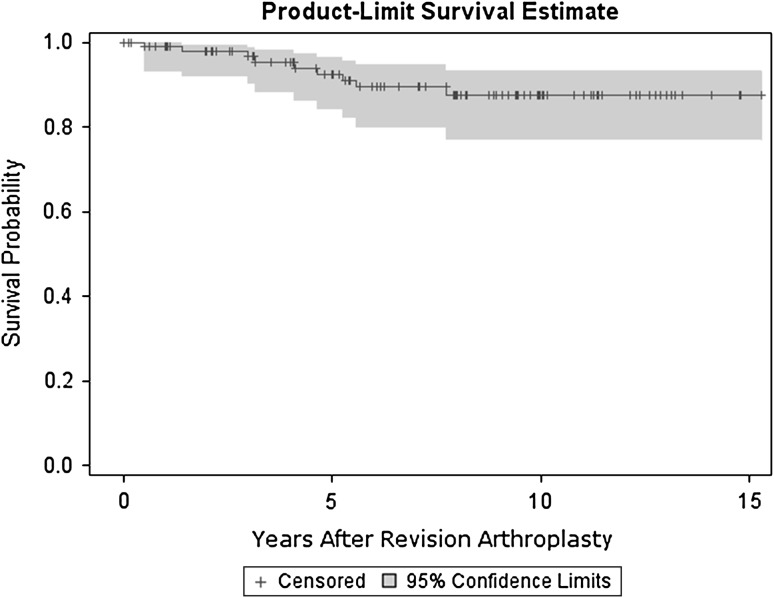
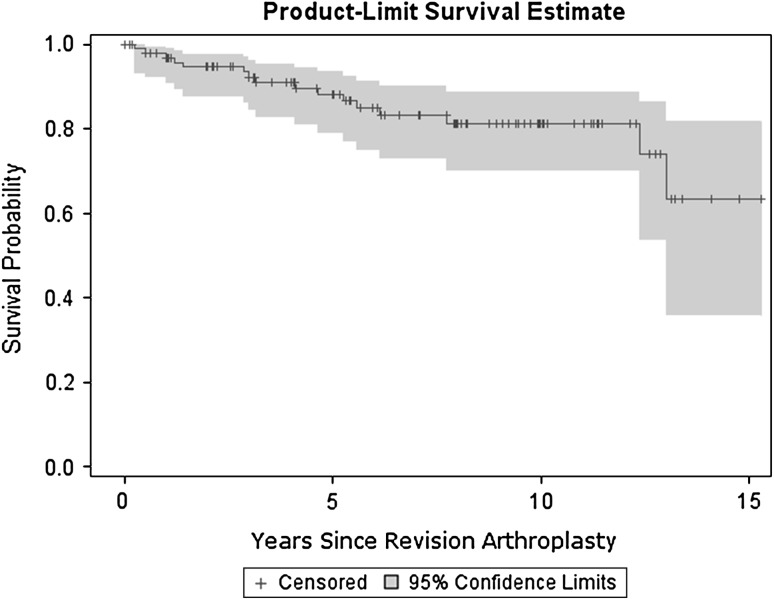
With failure defined as either femoral component revision for aseptic loosening or definite radiographic evidence of loosening (Fig. 1), the 10-year survival rate was 88% (95% CI, 77%–93%). With failure defined as any reoperation involving the hip (Fig. 2), the 10-year survival rate was 81% (95% CI, 70%–89%). With the numbers available, there was no association between patient age (p = 0.50), sex (p = 0.45), BMI (p = 0.92), head size (p = 0.49) or curved versus straight component (p = 0.97), standard versus modified tip component (p = 0.28), component diameter (p = 0.73), intraoperative fracture (p = 0.67) and femoral component loosening. There was an association between preoperative Paprosky grade (3 of 10 [30%] Grades 3B and 4 versus 6 of 94 [6%] Grades 1, 2, and 3A) and femoral component radiographic loosening (p = 0.03; hazard ratio 1.56).
Fig. 1.
A Kaplan-Meier survival curve with failure defined as femoral component revision for aseptic loosening or definite radiographic loosening shows a 10-year survival rate of 88% (95% CI, 77%–93%).
Fig. 2.
A Kaplan-Meier survival curve with failure defined as any reoperation involving the hip shows a 10-year survival rate of 81% (95% CI, 70%–89%).
Discussion
The best method of fixation for the femoral component in revision THA remains somewhat controversial. After initial enthusiasm with the early results of cemented and proximally coated femoral components in revision hip arthroplasty, most surgeons moved to the use of nonmodular body extensively coated components [10]. During the past 5 years, there has been more emphasis on the use of modular body femoral components (whether extensively coated or distally tapered and fluted), for revision arthroplasty because of the presumed advantages of modularity, such as both proximal and distal implant fit and fill and the ability to adjust femoral anteversion [9, 10]. However, these modular components add the complications of difficulty with modular junction engagement and the possibility of modular taper corrosion and fracture [9, 10]. Thus, there is a renewed interest in nonmodular body, fully coated or tapered fluted femoral components. There have been reports of the success of nonmodular body fully coated components in the first decade after implantation [6, 8, 9, 14], but only two studies report survivorship data longer than 10 years [5, 13]. There has also been a slight modification to the distal end of the curved component to ease insertion, with the intention of lowering the risk of intraoperative fracture. Thus, we asked the following questions: (1) What is the frequency of infection, aseptic loosening, and reoperations with nonmodular body fully coated components? (2) What is the frequency of intraoperative fracture of the femur and are there any factors related to these fractures? (3) What is the 10-year survivorship of these components, and are there any identifiable factors related to survival and rerevision?
This study has several limitations. First, the patient cohort was relatively small, as it was a single-surgeon study, but similar to other studies of revision femoral components [6, 8, 9, 13]. Second, this was not a randomized study comparing these fully coated femoral components to components with additional modularity or other methods of fixation, and we did not use this approach for all revisions during the period in question. However, our indications during the period were relatively standard, including all young patients and those with notable femoral bone deficiency and so the proportion of patients to whom this technique applies can be readily discerned. Third, this study involved one experienced revision hip surgeon using two components, and the results may not be applicable to other surgeons and implant systems. Fourth, there were six patients who died and six patients who refused to return for complete evaluation before the minimum 2-year followup. However, these hips were functioning well at the time of last followup. Fifth, these procedures were performed during many years and there might have been some subtle changes in techniques through the years. Finally, there were no dual-energy x-ray absorptiometry scans or other advanced imaging performed to quantitate the loss of proximal bone structure due to stress shielding, but this was not a major focus of the study.
The success of fixation and the rate of loosening of these revisions performed with a nonmodular body fully coated femoral component are difficult to compare to other series of nonmodular body full coat femoral components due to the variables of stem lengths, use of allograft struts, and length of followup (Table 1). Lawrence et al. [8] first reported the results of fully coated stems for revision arthroplasty. Using predominantly straight components in 174 revisions, 10 hips (5.7%) were rerevised for aseptic loosening in six, broken stem in two, and infection in two. The highest rate of failure was in the “severely deficient femur,” with eight failures in 39 hips, and another 18 hips (11%) were classified as having only “fibrous fixation” [8]. Kim and Kim [6] described a series of 54 hip revisions in which both a fully coated stem and two or three allograft struts were routinely used. Twenty of these hips were Paprosky Grade 3B, but only two femoral components were loose and were rerevised at a minimum followup of 10 years [6]. Weeden and Paprosky [13] reported on 170 revisions using fully coated components followed for 11 to 16 years. Bone ingrowth was seen in 139 hips (82%), fibrous fixation was seen in 24 hips (14%), and seven hips (4%) were considered loose, with six rerevised. Patients with Paprosky Grade 3B femurs had a failure rate of 21% (four of 19 hips). In the present study, there were nine femoral components (10%) with aseptic loosening and six were rerevised. Similar to the studies of Lawrence et al. [7] and Weeden and Paprosky [14], there was an association between aseptic loosening and severe bone loss, defined as Paprosky Grades 3B and 4. However, Thomsen et al. reported no stem rerevision in 30 hips described as Paprosky Grades 3B and 4, but only 36 of 93 hips had followup times greater than 10 years [13].
Table 1.
Results of nonmodular body fully coated femoral revisions
| Study | Number of hips | Paprosky Grade 3B (severe bone loss) (number of hips) | Mean followup (years) | Failure (number of hips) | Comment |
|---|---|---|---|---|---|
| Lawrence et al. [8] (1993) | 174 | 39 (22%) | 9 | 10 (6.9%) | Survival only 76.9% at 9 years with “severe bone loss” |
| Weeden and Paprosky [14] (2002) | 170 | 19 (11%) | 14 | 6 (4.1%) | 21% failure in Grade 3B femurs |
| Kim and Kim [6] (2005) | 54 | 20 (37%) | 10 | 2 (4%) | All had 2–3 allograft struts |
| Hamilton et al. [5] (2007) | 905 | Not stated | 6 | 20 (2.2%) | 143 hips with 10 year followup; 75 hips with 15 year followup |
| Thomsen et al. [13] (2013) | 93 (36 hips with 10–18 year followup) | 30 (32%) | 14 (for 36 hips only) | 4 (4.3%) | No stem rerevision in Grade 3B + 4 femurs |
| Present study | 92 | 10 (11%) | 8 | 9 (10.2%) | Higher failure with Grade 3B and 4 femurs |
Intraoperative fracture or perforation of the femur is the most frequent complication of uncemented femoral revisions, with the prevalence ranging from 9% to 46% [2, 4, 9, 14]. Egan and DiCesare [4] reported 27 fractures in 135 hips (20%) revised with a fully coated straight stem. However, Paprosky et al. [9] reported only 15 fractures in 170 hips (9%) revised with a fully coated straight stem. In the present study, intraoperative radiographs were always performed after insertion of the component, and there were 11 distal shaft fractures, two proximal fractures, and four perforations. There was an association between the use of a curved stem and intraoperative fracture and perforation of the femur. We wondered whether modification of the anterior tip of the component would decrease the frequency of fracture, but with the numbers available, we did not observe this to be the case. A power analysis showed we would need 180 stems in each group to find a statistically significant difference.
In conclusion, this study suggests that femoral revision with a nonmodular body fully coated component has a high rate of survival at a mean of 8 years. However, the overall frequency of reoperation for any reason, especially acetabular loosening, continues to increase as we follow the patients during a longer period of time [8], and so we will continue to follow these patients during the longer term. The senior author continues to use a nonmodular body, fully coated component for most femoral revisions. However, for certain hips with Paprosky Grades 3B and 4 femoral defects, a nonmodular body fluted tapered femoral component is being investigated. Because of the risk of intraoperative fractures, we routinely perform intraoperative radiographs during femoral component revisions to detect subtle fractures, and we perform fixation of any fracture or defect with allograft struts and cables.
Acknowledgments
We thank Richard Sloane, MPH for the statistical analyses and Mr Stephen Perlman, MLS for assistance with the literature search.
Footnotes
The institution of the authors (PFL, ESS) has received funding, during the study period, from Zimmer, Inc (Warsaw, IN, USA).
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
This project was performed at Chapel Hill Orthopedics Surgery & Sports Medicine (Chapel Hill, NC, USA) and Duke University Medical Center (Durham, NC, USA).
References
- 1.Archibeck MJ, Rosenberg AG, Berger RA, Silverton CD. Trochanteric osteotomy and fixation during total hip arthroplasty. J Am Acad Orthop Surg. 2003;11:163–173. doi: 10.5435/00124635-200305000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Chappell JD, Lachiewicz PF. Fracture of the femur in revision hip arthroplasty with a fully porous-coated component. J Arthroplasty. 2005;20:234–238. doi: 10.1016/j.arth.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 3.Della Valle CJ, Paprosky WG. The femur in revision total hip arthroplasty evaluation and classification. Clin Orthop Relat Res. 2004;420:55–62. doi: 10.1097/00003086-200403000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Egan KJ, DiCesare PE. Intra-operative complications of revision hip arthroplasty using fully porous coated straight cobalt-chrome femoral stem. J Arthroplasty. 1995;10(suppl):45–50. doi: 10.1016/S0883-5403(05)80230-X. [DOI] [PubMed] [Google Scholar]
- 5.Hamilton WG, Cashen DV, Ho H, Hopper RH, Engh CA. Extensively porous-coated stems for femoral revision. A choice for all seasons. J Arthroplasty. 2007;22(suppl 1):106–110. doi: 10.1016/j.arth.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 6.Kim YH, Kim JS. Revision hip arthroplasty using strut allografts and fully porous-coated stems. J Arthroplasty. 2005;20:454–459. doi: 10.1016/j.arth.2004.09.054. [DOI] [PubMed] [Google Scholar]
- 7.Lachiewicz PF, Soileau ES. Fixation, survival, and dislocation of jumbo acetabular components in revision hip arthroplasty. J Bone Joint Surg Am. 2013;95:543–548. doi: 10.2106/JBJS.L.00758. [DOI] [PubMed] [Google Scholar]
- 8.Lawrence JM, Engh CA, Macalino GE. Revision total hip arthroplasty: long-term results without cement. Orthop Clin North Am. 1993;24:635–644. [PubMed] [Google Scholar]
- 9.Paprosky WG, Greidanus NV, Antoniou J. Minimum 10-year-results of extensively porous-coated stems in revision hip arthroplasty. Clin Orthop Relat Res. 1999;369:230–242. doi: 10.1097/00003086-199912000-00024. [DOI] [PubMed] [Google Scholar]
- 10.Richards CJ, Duncan CP, Masri BA, Garbuz DS. Femoral revision hip arthroplasty: a comparison of two stem designs. Clin Orthop Relat Res. 2010;468:491–496. doi: 10.1007/s11999-009-1145-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sheth NP, Nelson CL, Paprosky WG. Femoral bone loss in revision total hip arthroplasty: evaluation and management. J Am Acad Orthop Surg. 2013;21:601–612. doi: 10.5435/JAAOS-21-10-601. [DOI] [PubMed] [Google Scholar]
- 12.Sporer SM, Paprosky WG. Revision total hip arthroplasty: the limits of fully coated stems. Clin Orthop Relat Res. 2003;417:203–209. doi: 10.1097/01.blo.0000096803.78689.0c. [DOI] [PubMed] [Google Scholar]
- 13.Thomsen PB, Jensen NJF, Kampmann J, Hansen TB. Revision hip arthroplasty with an extensively porous-coated stem-excellent long-term results also in severe bone stock loss. Hip Int. 2013;23:353–358. doi: 10.5301/hipint.5000032. [DOI] [PubMed] [Google Scholar]
- 14.Weeden SH, Paprosky WG. Minimal 11-year follow-up of extensively porous-coated stems in femoral revision total hip arthroplasty. J Arthroplasty. 2002;17(suppl 1):134–137. doi: 10.1054/arth.2002.32461. [DOI] [PubMed] [Google Scholar]
- 15.Zalzal R, Gandi R, Petrucelli D, Winemaker MJ, deBeer J. Fractures at the tip of long-stem prostheses used for revision hip arthroplasty. J Arthroplasty. 2003;18:741–745. doi: 10.1016/S0883-5403(03)00258-4. [DOI] [PubMed] [Google Scholar]