Abstract
Background
Postural orthostatic tachycardia syndrome (POTS) is the most common of several types of dysautonomia, characterized by dysfunction of the autonomic nervous system manifesting with symptoms of orthostatic intolerance with or without associated orthostatic hypotension and excessive autonomic excitation. Given the numerous presenting musculoskeletal symptoms of POTS and its known associations with other clinical entities like Ehlers-Danlos syndrome, POTS constitutes an unusual treatment challenge of which the orthopaedic surgeon and other related healthcare providers should be aware.
Case Description
We describe two patients with a diagnosis of POTS and musculoskeletal manifestations. The first is a 13-year-old boy with a concurrent diagnosis of Ehlers-Danlos syndrome and worsening back pain. The patient had resolution of his musculoskeletal symptoms after treatment with a Boston Overlap LSO brace and physical therapy and resolution of his cardiovascular symptoms after pharmacologic treatment. The second patient is a 17-year-old girl with an L1 vertebral hemangioma and pain of sudden onset radiating to her lower extremities. Her symptoms were controlled with therapy and gabapentin.
Literature Review
POTS is a poorly understood and controversial clinical entity with lack of awareness and knowledge regarding the syndrome by the majority of medical specialists. Its complex and wide range of clinical presentation has led to being commonly mistaken with malingering, depression and anxiety disorders. Review of the literature did not yield any previous studies addressing POTS and the special considerations for the orthopaedic surgeon caring for these patients; previous studies of large patient series focus on investigating the pathologic substrate of POTS and the efficacy of various treatment modalities on the cardiovascular dysregulation.
Clinical Relevance
These two cases show that understanding and knowledge of this syndrome and its comorbidities should guide any diagnostic approach or therapeutic intervention by the orthopaedic surgeon caring for patients with this syndrome. It is important that the surgeon is aware of the benefits of detailed patient education and physical conditioning, the increased perioperative complications, and the need for specialized anesthesia.
Introduction
Postural orthostatic tachycardia syndrome (POTS) is associated with Ehlers-Danlos syndrome Type III, joint hypermobility syndrome, and chronic musculoskeletal pain, complicating the diagnostic approach of the orthopaedic surgeon caring for these patients.
In patients with POTS the postural tachycardia is accompanied by symptoms of cerebral hypoperfusion, sympathetic hyperactivity, and other systemic symptoms (Table 1). The pathophysiologic mechanisms of orthostatic intolerance in POTS are believed to be complex and heterogeneous (Table 1) and include volume dysregulation, hyperadrenergic states, impaired sympathetic vasoconstriction leading to venous pooling in the lower extremities, and physical deconditioning [2, 20]. Patients with POTS are predominantly young (mean age, 30 years) females (87%) with a subacute (1–3 months) onset of lightheadedness, dizziness, and presyncope episodes [20]. Large series have shown that a viral illness or surgical procedure can act as triggering factors [12, 20]. Although in adults it can be an isolated syndrome or associated with porphyria, diabetes mellitus, and paraneoplastic processes, in children it tends to be an isolated syndrome with reports of spontaneous resolution in approximately 75% of the patients by the age of 21 to 25 years [3, 8, 20]. Given the wide range of symptoms and the comorbidities associated with POTS, treatment requires a multidisciplinary approach and involves pharmacologic and nonpharmacologic measures. The four basic principles of POTS management are (1) patient education; (2) nonpharmacologic volume expansion with salt and water replacement; (3) pharmacologic therapy (mineralocorticoids, cholinergics, β-blockers); and (4) physical conditioning/physical countermaneuvers [2, 3, 19].
Table 1.
Postural orthostatic tachycardia syndrome (POTS)
| Diagnostic features/testing | Pathophysiologic mechanisms involved | Symptoms and associated comorbidities | Management principles |
|---|---|---|---|
| Heart rate increase of 30 beats/minute or more for adults and 40 beats/minute or more for individuals 12 to 19 years old, within 10 minutes of standing or head-up tilt in the absence of orthostatic hypotension. Basic diagnostic evaluation includes tests for exclusion of primary cardiac causes (ECG, echocardiogram, Holter monitoring) and head-up tilt test. |
Volume dysregulation Hyperadrenergic states/excessive sympathoexcitatory responses Impaired sympathetic vasoconstriction in the lower extremities Physical deconditioning |
Orthostatic: light-headedness, dizziness, presyncope, palpitations. Ehlers-Danlos syndrome: hypermobility of the small and large joints, recurrent joint subluxations, scoliosis, velvety soft skin, and early onset chronic pain. Visceral pain and dysmotility: nausea, bloating, diarrhea, constipation, early satiety. Fatigue, general sleep disturbances, and myofascial pain. Neurologic: chronic migraines, orthostatic headaches, and so-called “brain fog”. |
Patient education Nonpharmacologic volume expansion with salt and water replacement Pharmacologic therapy (mineralocorticoids, cholinergics, β-blockers) Physical conditioning/physical countermaneuvers |
The purpose of this case report is to describe two patients with POTS who show the broad spectrum of clinical presentation of this syndrome and highlight the necessity for recognition and knowledge of this syndrome by the orthopaedic surgeon.
Case Reports
Patient 1
History
A 13-year-old boy was referred to our orthopaedic department 7 months after his initial diagnosis of POTS and Ehlers-Danlos syndrome for worsening moderate back pain.
Before his initial POTS diagnosis, he had a 2-month-period of fatigue, chest and abdominal pain, dysphagia, and syncopal episodes, and had been evaluated by a gastroenterologist, an endocrinologist, an immunologist, a neurologist, and finally a cardiologist. Otherwise, his medical, surgical, and family history was noncontributory.
Physical Examination
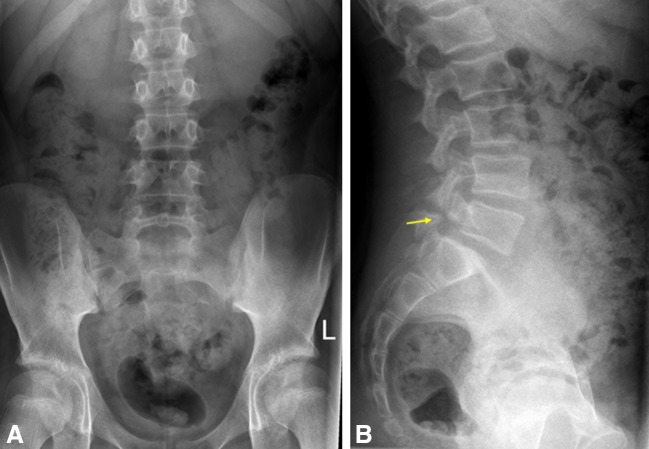
On physical examination, he had tenderness on palpation of the spine in the upper and midthoracic midline and increased pain with hyperextension of the spine. He also had generalized ligamentous laxity (Fig. 1) that was more prominent in the elbows and shoulders bilaterally (Beighton score, 7), tight heel cords, and mild pectus excavatum. He met the heart-rate criterion of a pulse greater than 120 beats per minute during the first 10 minutes of a standing upright test; his heart rate went from 100 beats per minute supine to 140 beats per minute standing. Review of other systems was unremarkable.
Fig. 1A–B.
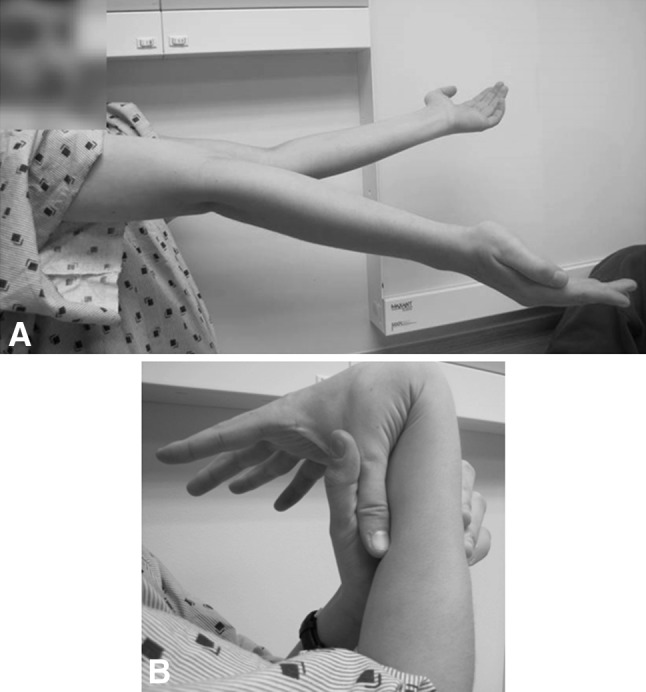
The photographs show (A) apposition of the thumb to the flexor aspect of the forearm and (B) elbow hyperextension of 20°.
Laboratory Tests and Imaging
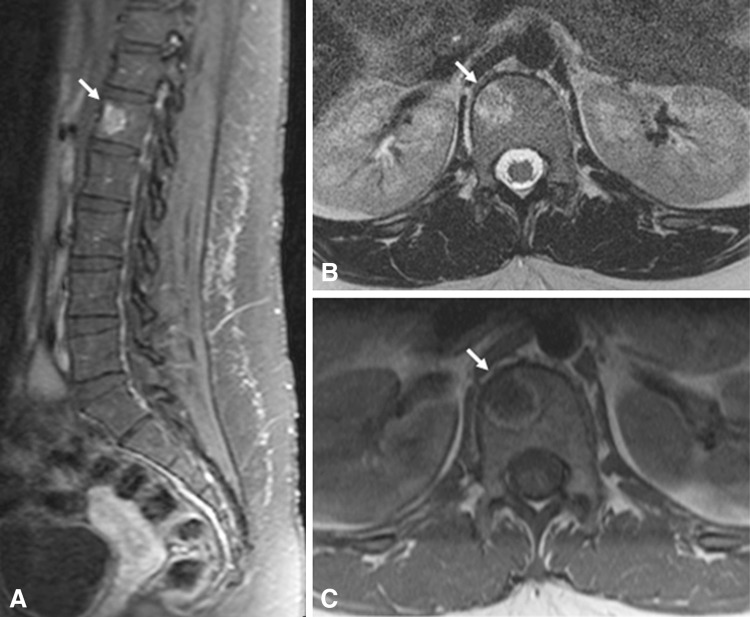
Radiographs of the spine showed a Grade I L5-S1 spondylolisthesis (Fig. 2).
Fig. 2A–B.
(A) AP and (B) lateral radiographs of the lumbar spine show a Grade I spondylolisthesis of L5-S1. The arrow shows the defect in the pars interarticularis (spondylolysis).
Treatment and Followup
Per our institution’s aforementioned four-step treatment approach, the patient and his family were educated in detail regarding the nature of his diagnosis, and the patient was educated regarding nonpharmacologic interventions (60–80 ounces of fluid each day, salty snacks, no caffeine or alcohol, and raising the head of the bed). He also was prescribed physical therapy for conditioning and fludrocortisone, metoprolol, and pyridostigmine. Specifically for his spondylolisthesis, the patient was treated with a Boston Overlap LSO (lumbosacral orthosis) brace and intense and continuous physical and occupational therapy to strengthen and stretch his core and thigh muscles, stabilize the joints, and help with fine motor skills that the patient was lacking. The patient reported that he attended physical therapy regularly and that he wore his brace as recommended. Four months later he had almost complete resolution of his back pain, and 23 months after his initial diagnosis of POTS he was completely asymptomatic from an orthopaedic and cardiovascular standpoint with no orthostatic symptoms and full return to sports and activities. Pharmacologically, he was still taking only metoprolol.
Patient 2
History
A 17-year-old girl with a known history of POTS and localized intermittent back pain from an L1 vertebral intraosseous hemangioma that was being treated nonoperatively with physical therapy, presented to the emergency department with sudden new onset of severe (10/10) back pain radiating to her lower extremities (left worse than right) without associated numbness or tingling. There was no report of loss of bowel or bladder function.
The patient had a long history of palpitations, worsening fatigue, nausea and emesis, insomnia, migraines, diaphoresis, and brief episodes (less than 5 minutes) of numbness and tingling of sudden onset at her lower extremities; these all were attributed to a presumed diagnosis of panic attacks before her official diagnosis of POTS. Her review of symptoms was positive for intermittent moderate back pain and migraines and negative for findings suggestive of Ehlers-Danlos syndrome, weight loss, vision problems, hearing problems, swallowing difficulties, asthma, rashes, seizure disorder, or bleeding dyscrasia. Otherwise, her medical, surgical, and family history was noncontributory.
Physical Examination
The patient had poor motor examination at the lower extremities bilaterally (3/5 at the right hip, knee and ankle and 2/5 at the left hip, knee and ankle) because of limitation from pain. Sensation was noted to be intact in the lower extremities. The neurologic examination revealed normal tone, normal and symmetric deep tendon reflexes, and no spasticity or clonus in the extremities. The patient had met the heart-rate criterion for POTS of a pulse greater than 120 beats per minute during the first 10 minutes of a standing upright test; her heart rate went from 85 beats per minute supine to 130 beats per minute standing at her initial POTS diagnosis.
Laboratory Tests and Imaging
During her emergency department admission, because radiographs of her spine did not show any changes, she underwent emergent MRI of the spine. The images showed no lumbar spinal canal stenosis or pathologic enhancement and no interval changes of the L1 hemangioma (Fig. 3).
Fig. 3A–C.
(A) Patient 2 had an L1 hemangioma. (B) A heterogeneous hyperintense signal was seen on a T2-weighted image and (C) peripheral hyperintensity and central hypointensity on a T1-weighted image.
Treatment and Followup
Previous to her latest emergency department admission, per our institution’s aforementioned four-step treatment approach, the family was educated in detail regarding the nature of her diagnosis and were given information on support groups, and the patient was educated regarding nonpharmacologic interventions (60–80 ounces of fluid each day and salty snacks, no caffeine or alcohol, raising the head of the bed) and was prescribed physical therapy for conditioning. She was prescribed methylphenidate for its vasoconstrictive properties owing to its action as a dopamine and norepinephrine reuptake inhibitor and meclizine and ondansetron for her reported nausea and emesis. During her emergency department visit, after evaluation by a multidisciplinary team (orthopaedic surgeon, cardiologist, pain medicine specialist, physical medicine and rehabilitation) and concluding that the pain was neuropathic and associated with her POTS diagnosis, the patient was prescribed gabapentin for her neuropathic pain, tizanidine as a muscle relaxant, and intensive physical therapy. Physical therapy consisted of very gradually increasing aerobic exercise using a recumbent bicycle, rowing machine, or swimming, and exercises focused on strengthening of the legs mainly, and core secondarily. At latest followup, 10 months after the emergency department episode (3.5 years after her initial diagnosis of POTS), the patient’s symptoms are stable and adequately controlled with the neuropathic pain being intermittent and mild to moderate (2/10–4/10) with use of pregabalin, and only occasional orthostatic symptoms of daytime dizziness and nighttime palpitations from a cardiovascular standpoint.
Discussion
These two cases show the orthopaedic implications of this clinical entity and the importance of establishing a correct diagnosis of POTS to improve treatment outcomes by avoiding unnecessary diagnostic studies and treatments. Overall, the absence of previous reports regarding POTS in the orthopaedic literature and the aforementioned associated musculoskeletal comorbidities underline the need for increased awareness of this syndrome by the orthopaedic community.
POTS is a newly recognized [6] and poorly understood [2, 6] clinical entity evidenced by the exposure it received in 2011 from the media after cases being misdiagnosed by medical specialists as malingering, “laziness” and “panic attacks” [4]. Although “orthostatic hypotension” was defined in 1996 by the American Academy of Neurology, it was only in 2011 that the American Autonomic Society and the Autonomic Disorders section of the American Academy of Neurology issued a consensus statement defining POTS [6]. POTS is defined as a heart rate increase of 30 beats per minute or more for adults and 40 beats per minute or more for individuals 12 to 19 years old, within 10 minutes of standing or head-up tilt in the absence of orthostatic hypotension; the standing heart rate is often 120 beats per minute or greater [6].
Many patients, however, have symptoms that cannot be explained by their postural intolerance and their tachycardia. These symptoms are associated with known comorbidities and are classified as follows: (1) Ehlers-Danlos syndrome/joint hypermobility syndrome. Although the association between POTS and joint hypermobility syndrome or Ehlers-Danlos syndrome Type III (hypermobile type) is not completely explained, it has been well documented [7, 10, 18]. In a study by Gazit et al. [7], 80% of patients with joint hypermobility syndrome displayed symptoms of dysautonomia with orthostatic hypotension or POTS. Ehlers-Danlos syndrome Type III is characterized by recurrent joint subluxations and early-onset chronic pain that can further complicate the chronic fatigue, weakness, and neuropathic pain associated with POTS. (2) Visceral pain and dysmotility. Patients with POTS present with nausea (39%), bloating (24%) and diarrhea (18%), constipation, and early satiety. Their clinical picture can be similar to that of patients with functional motility disorders like irritable bowel syndrome and functional dyspepsia [20], although they also can have true slow motility, or even gastroparesis. (3) Fatigue, insomnia, and fibromyalgia. Weakness, fatigue, and low energy levels have been reported to be present in as much as 50% of patients with POTS, general sleep disturbances in 32% of patients, and myofascial pain in 16% of patients [20]. (4) Neurologic comorbidities. The most common neurologic symptoms observed in patients with POTS are chronic migraines and orthostatic headaches [20]. Although sensory examination usually is normal, symptoms of neuropathic pain (2%) and signs consistent with peripheral neuropathy (1.4%) also have been reported [20]. Finally, cognitive dysfunction (so-called “brain fog”) also has been reported [3, 11]. The main principle of POTS management is patient education. As with any chronic disease, patients should be educated in detail regarding their disease [3]. Education should not be limited to symptoms, precipitating factors, and natural history; most importantly the orthopaedic surgeon should be able to inform the patient and/or family about the associated musculoskeletal symptoms of this syndrome and reassure them that they are not related to any underlying musculoskeletal anomaly once appropriately cleared.
In terms of medical treatment, since the etiology is not clear, treatment is directed mostly toward addressing and treating the symptoms until spontaneous remission, or resolution in younger patients, occurs [3, 20]. Although pharmacotherapy and intravascular volume expansion measures typically are beyond the realm of an orthopaedic surgeon, these patients can require polypharmacy to control their symptoms. Fludrocortisone, a mainstay salt-sparing corticosteroid used in these patients, can cause, in higher doses, significant hypokalemia and hypomagnesemia complicating the interpretation of laboratory values and increasing the risk for nontraumatic avascular necrosis. Chronic neuropathic pain usually is addressed with duloxetine, pregabalin, or gabapentin with minimal musculoskeletal adverse effects [3]. Chronic pain also can be improved with physical therapy and exercise to strengthen the leg and core muscles. Aerobic exercises also are crucial but at the beginning, duration and intensity should be limited [20].
A multidisciplinary evaluation for patients with POTS (with or without concurrent Ehlers-Danlos syndrome) is imperative before any surgical procedure. It has been reported that surgery, illness, or trauma may worsen or cause additional symptoms [2, 15, 20]. Although little is known regarding the anesthetic implications in POTS, there have been reports of complications regarding the type of anesthesia, intubation, and intraoperative blood pressure [13, 16]. Because patients are not allowed food or drink before operative procedures and owing to the aforementioned tendency for volume dysregulation and impaired sympathetic vasoconstriction, we routinely recommend preoperative intravenous hydration before administration of sedative or anesthetic agents to help to stabilize their vasculature. Preoperatively, specifically for patients with concurrent Ehlers-Danlos syndrome, it is important that they are evaluated by an experienced cardiologist for aortic aneurysms, valvular heart disease (mainly mitral valve prolapse), and possible need for preoperative antibiotics or ß-blockers, and by an experienced anesthesiologist because of reported concerns regarding the efficacy and safety of epidurals in these patients [5].
Intraoperatively, in addition to the complex anesthetic requirements in these patients [16] that are beyond the realm of our study, for the patient with POTS with associated Ehlers-Danlos syndrome, the main concerns during preparation of the patient are careful positioning to avoid joint subluxations and minimizing needle sticks and monitor device placement (eg, neuromonitoring probes) because of concerns with skin fragility [9]. Furthermore, meticulous hemostasis is needed in these patients [1]. Characteristically, posterior spinal fusion for scoliosis has been associated with excessive bleeding [14, 17], leading to death in a patient with postoperative intraabdominal bleeding [17]. Although surgical closure might be complicated by tearing of the skin edges by the sutures, careful multilayered closure with nylon sutures and wound closure strips instead of staples can prevent possible future wound hematoma, wound dehiscence, and resulting infections [21].
Postoperatively, patients with POTS usually require not only prolonged hospital stay until they are stable for discharge, but also rehabilitation time. As mentioned previously, prolonged postoperative immobilization can further decondition these patients, leading to destabilization of their orthostatic symptoms and a challenging rehabilitation. Patients with POTS rapidly become symptomatic during exercise (53% of patients) [20] and require the guidance of an experienced physical therapist to start slowly with small amounts of exercise and use suitable equipment, like a recumbent cycle [2]. In addition, resistance exercises for the major muscle groups can help by improving venous return. In a large series of 152 patients, after volume expansion measures (92.5%) and β-blockers (76.7%), resistance training was the third most common treatment modality selected by the patients because of its positive effects [20]. Another way to improve venous return in these patients is with the use of support garments like waist-high compression stockings and abdominal binders, but their efficacy has been questioned [3, 20]. Finally, given the association with Ehlers-Danlos syndrome, continuous and appropriate physical therapy has an added benefit to these patients by improving proprioception, muscle strength, balance, and protecting the joints from damage [22].
Musculoskeletal pain, extremity numbness and weakness, and joint laxity are commonly seen by orthopaedic surgeons. With an established diagnosis of POTS, coexistent understanding and knowledge of this syndrome and its comorbidities should guide any diagnostic approach, patient education, or therapeutic intervention. For this reason, POTS constitutes an unusual treatment challenge of which the orthopaedic surgeon and other related healthcare providers should be aware.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the reporting of this case report, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Anstey A, Mayne K, Winter M, Van de Pette J, Pope FM. Platelet and coagulation studies in Ehlers-Danlos syndrome. Br J Dermatol. 1991;125:155–163. doi: 10.1111/j.1365-2133.1991.tb06063.x. [DOI] [PubMed] [Google Scholar]
- 2.Benarroch EE. Postural tachycardia syndrome: a heterogeneous and multifactorial disorder. Mayo Clin Proc. 2012;87:1214–1225. doi: 10.1016/j.mayocp.2012.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boris JR. The role of the cardiologist in the evaluation of dysautonomia. Cardiol Young. 2010;20(Suppl 3):135–139. doi: 10.1017/S1047951110001198. [DOI] [PubMed] [Google Scholar]
- 4.Brody JE. Ailment Can Steal Youth From the Young. 2011. The New York Times. Available at: http://www.nytimes.com/2011/10/18/health/18brody.html?_r=4&ref=science&. Accessed August 6, 2014.
- 5.Dolan P, Sisko F, Riley E. Anesthetic considerations for Ehlers-Danlos syndrome. Anesthesiology. 1980;52:266–269. doi: 10.1097/00000542-198003000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Freeman R, Wieling W, Axelrod FB, Benditt DG, Benarroch E, Biaggioni I, Cheshire WP, Chelimsky T, Cortelli P, Gibbons CH, Goldstein DS, Hainsworth R, Hilz MJ, Jacob G, Kaufmann H, Jordan J, Lipsitz LA, Levine BD, Low PA, Mathias C, Raj SR, Robertson D, Sandroni P, Schatz I, Schondorff R, Stewart JM, van Dijk JG. Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Clin Auton Res. 2011;21:69–72. doi: 10.1007/s10286-011-0119-5. [DOI] [PubMed] [Google Scholar]
- 7.Gazit Y, Nahir AM, Grahame R, Jacob G. Dysautonomia in the joint hypermobility syndrome. Am J Med. 2003;115:33–40. doi: 10.1016/S0002-9343(03)00235-3. [DOI] [PubMed] [Google Scholar]
- 8.Grubb BP, Kanjwal Y, Kosinski DJ. The postural tachycardia syndrome: a concise guide to diagnosis and management. J Cardiovasc Electrophysiol. 2006;17:108–112. doi: 10.1111/j.1540-8167.2006.00575.x. [DOI] [PubMed] [Google Scholar]
- 9.Johnston BA, Occhipinti KE, Baluch A, Kaye AD. Ehlers-Danlos syndrome: complications and solutions concerning anesthetic management. Middle East J Anesthesiol. 2006;18:1171–1184. [PubMed] [Google Scholar]
- 10.Kanjwal K, Saeed B, Karabin B, Kanjwal Y, Grubb BP. Comparative clinical profile of postural orthostatic tachycardia patients with and without joint hypermobility syndrome. Indian Pacing Electrophysiol J. 2010;10:173–178. [PMC free article] [PubMed] [Google Scholar]
- 11.Karas B, Grubb BP, Boehm K, Kip K. The postural orthostatic tachycardia syndrome: a potentially treatable cause of chronic fatigue, exercise intolerance, and cognitive impairment in adolescents. Pacing Clin Electrophysiol. 2000;23:344–351. doi: 10.1111/j.1540-8159.2000.tb06760.x. [DOI] [PubMed] [Google Scholar]
- 12.Low PA, Opfer-Gehrking TL, Textor SC, Benarroch EE, Shen WK, Schondorf R, Suarez GA, Rummans TA. Postural tachycardia syndrome (POTS) Neurology. 1995;45(4 suppl 5):S19–S25. [PubMed] [Google Scholar]
- 13.McEvoy MD, Low PA, Hebbar L. Postural orthostatic tachycardia syndrome: anesthetic implications in the obstetric patient. Anesth Analg. 2007;104:166–167. doi: 10.1213/01.ane.0000246815.39197.2b. [DOI] [PubMed] [Google Scholar]
- 14.McMaster MJ. Spinal deformity in Ehlers-Danlos syndrome: five patients treated by spinal fusion. J Bone Joint Surg Br. 1994;76:773–777. [PubMed] [Google Scholar]
- 15.Medow MS, Stewart JM. The postural tachycardia syndrome. Cardiol Rev. 2007;15:67–75. doi: 10.1097/01.crd.0000233768.68421.40. [DOI] [PubMed] [Google Scholar]
- 16.Rabbitts JA, Groenewald CB, Jacob AK, Low PA, Curry TB. Postural orthostatic tachycardia syndrome and general anesthesia: a series of 13 cases. J Clin Anesth. 2011;23:384–392. doi: 10.1016/j.jclinane.2010.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rabenhorst BM, Garg S, Herring JA. Posterior spinal fusion in patients with Ehlers-Danlos syndrome: a report of six cases. J Child Orthop. 2012;6:131–136. doi: 10.1007/s11832-012-0393-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rowe PC, Barron DF, Calkins H, Maumenee IH, Tong PY, Geraghty MT. Orthostatic intolerance and chronic fatigue syndrome associated with Ehlers-Danlos syndrome. J Pediatr. 1999;135:494–499. doi: 10.1016/S0022-3476(99)70173-3. [DOI] [PubMed] [Google Scholar]
- 19.Shibata S, Fu Q, Bivens TB, Hastings JL, Wang W, Levine BD. Short-term exercise training improves the cardiovascular response to exercise in the postural orthostatic tachycardia syndrome. J Physiol. 2012;590:3495–3505. doi: 10.1113/jphysiol.2012.233858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thieben MJ, Sandroni P, Sletten DM, Benrud-Larson LM, Fealey RD, Vernino S, Lennon VA, Shen WK, Low PA. Postural orthostatic tachycardia syndrome: the Mayo clinic experience. Mayo Clin Proc. 2007;82:308–313. doi: 10.1016/S0025-6196(11)61027-6. [DOI] [PubMed] [Google Scholar]
- 21.Weinberg J, Doering C, McFarland EG. Joint surgery in Ehlers-Danlos patients: results of a survey. Am J Orthop (Belle Mead NJ). 1999;28:406–409. [PubMed] [Google Scholar]
- 22.Wolf JM, Cameron KL, Owens BD. Impact of joint laxity and hypermobility on the musculoskeletal system. J Am Acad Orthop Surg. 2011;19:463–471. doi: 10.5435/00124635-201108000-00002. [DOI] [PubMed] [Google Scholar]