Abstract
Background
The early recovery period after periacetabular osteotomy (PAO) can be limited by pain and activity restrictions. Modifications of the Bernese PAO, including sparing the rectus tendon and discontinuing routine arthrotomy, may accelerate early postoperative recovery compared with the standard approach.
Questions/purposes
Does a modified approach for PAO (1) lead to improved pain control immediately after surgery; (2) lead to improved ambulation during the hospital stay; (3) lead to shorter stays, less blood loss, and shorter surgical times; and (4) compromise acetabular correction?
Methods
We retrospectively reviewed all 75 patients who underwent PAO for developmental dysplasia of the hip between August 2009 and May 2013. The control group included 44 consecutive patients who underwent a standard Bernese PAO with rectus takedown (RT). The study group consisted of 31 consecutive patients who underwent PAO using a modified rectus-sparing (RS) approach without routine arthrotomy. The groups were similar in age, body mass index, and American Society of Anesthesiologists score, but the RT group was comprised of a greater percentage of men than the RS group. Outcome variables were collected from patient charts and included inpatient pain, inpatient ambulation as well as length of stay, estimated blood loss, surgical time, and postoperative radiographic measurements. Cohen’s f2 was used to calculate the effect size in the regression analysis and effects were considered small for values < 0.15, moderate for 0.15 to 0.34, and large for values > 0.35.
Results
Patients who underwent PAO with a RS approach had less overall pain (RT median 4 versus RS median 2); however, the difference may not have been perceptible to the typical patient (p = 0.001, f2 = 0.059). Patients treated with the RS approach ambulated similar distances during the hospital stay with a median 11 feet (interquartile range [IQR], 0–72.5) for the RT group and a median 30 feet (IQR, 0–100) for the RS group (p = 0.215, f2 = 0.095). Patients in the RT group had a median length of stay of 4 days (IQR, 4–5) compared with a median 3 days (IQR, 3–4) in the RS group (p < 0.001). The median estimated blood loss was greater (p = 0.010) in the RT group (median, 500 mL; IQR, 350–700) versus the RS group (median, 300; IQR, 250–500). The median surgical time was longer (p < 0.001) in patients undergoing PAO with the RT approach (median, 159.5 minutes; IQR, 145.5–177) compared with the RS approach (median, 103 minutes; IQR, 75–114). Acetabular reorientation based on postoperative radiographs was not compromised by the modified approach.
Conclusions
The approach modification was straightforward to implement in all patients and did not compromise acetabular fragment mobilization or final positioning. Two of the three key variables that the approach might have influenced–pain and length of stay–were below the minimum clinically important difference and different by only a fraction of a day, respectively. The difference in ambulation was of only modest clinical importance. More definitive evidence for clinical superiority in terms of pain, ambulation, and return of muscle function will likely require more sophisticated instruments such as gait analysis, muscle strength testing, and longer-term outcome studies with sensitive instruments.
Level of Evidence
Level III, therapeutic study. See Instructions for Authors for a complete description of levels of evidence.
Introduction
The Bernese periacetabular osteotomy (PAO) was first described by Ganz et al. [8] in the 1980s and has become the preferred method of surgical treatment of developmental dysplasia of the hip (DDH) in adult patients in North America and Europe [8, 11, 13, 22, 24, 25]. The standard Bernese PAO includes takedown of the direct and indirect heads of the rectus tendon and allows an anterior capsulotomy to address chondrolabral lesions and femoral head-neck offset issues [9, 18]. Although this approach facilitates surgical objectives, early recovery is often limited by pain and symptom-based activity modulation as well as surgeon-based restrictions.
Rationale
Recent studies have described alternative approaches to the Bernese PAO in the hopes of decreasing complications, surgical time, surgical trauma, estimated blood loss, and length of stay (LOS) while maintaining the ability to reorient the acetabulum [2, 14, 19, 23]. Based on these reports, we began modifying the standard Bernese PAO with a rectus femoris-sparing surgical approach without arthrotomy for PAO in 2012. We hypothesized that this approach might improve early recovery.
Study Questions
We sought to answer the following questions: does this modified approach for PAO (1) lead to improved pain control immediately after surgery; (2) lead to improved ambulation during the hospital stay; (3) lead to shorter stays, less blood loss, and shorter surgical times; and (4) compromise acetabular correction as judged by radiographic measurements?
Patients and Methods
Study Design and Setting
After receiving an exemption from our institutional review board, we performed a retrospective comparative analysis on all 75 patients who underwent PAO for DDH at a major academic medical center from August 2009 to May 2013.
Participants/Study Subjects
Patients were included in this study if they had undergone surgery with either a standard Bernese PAO with rectus takedown (RT) or a modified rectus-sparing (RS) approach without routine arthrotomy. There were no exclusions. The RT group consisted of 44 consecutive patients from August 2009 to May 2012 who underwent standard Bernese PAO with rectus takedown. In June 2012, a modification of the standard approach was incorporated into the surgical protocol and consisted of sparing the rectus tendon and the discontinuation of routine arthrotomy. The RS group consisted of 31 consecutive patients and included all hips that underwent a modified RS PAO from June 2012 to May 2013. General indications for PAO were similar in both groups and included failure of conservative management with radiographic evidence of dysplasia (lateral center-edge angle < 20°) without significant osteoarthritis (Tönnis grade < 2) and physical examination findings consistent with diagnosis.
Description of Experiment, Treatment, or Surgery
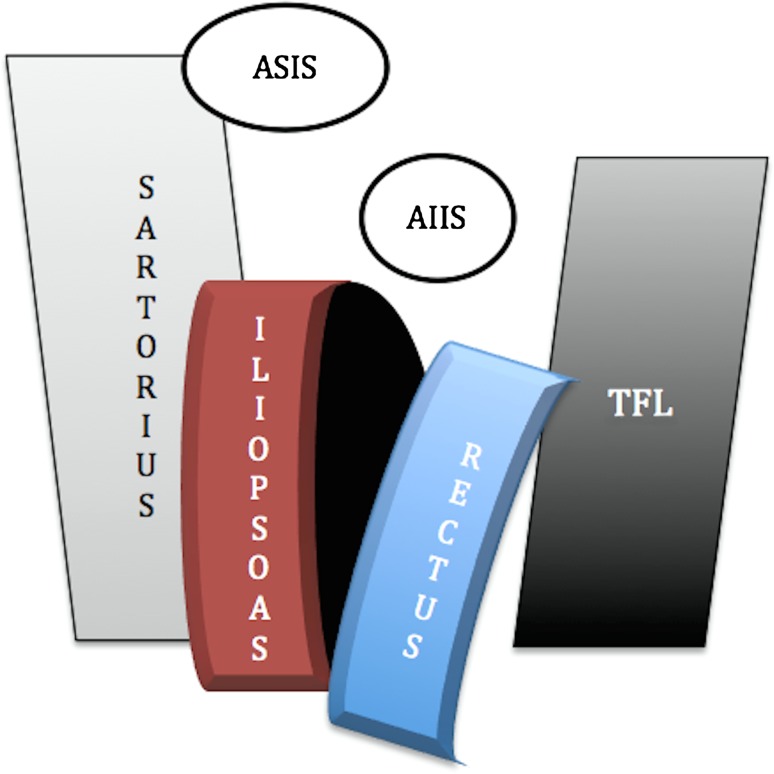
The standard RT approach was performed following previously described techniques [5, 8, 16]. After performing an osteotomy of the anterosuperior iliac spine (ASIS) with the sartorius and abdominal muscles attached, it is retracted medially and then the approach is extended distally between the tensor fascia latae and sartorius. Once down on the AIIS, the direct head of the rectus is elevated from the AIIS with electrocautery and tagged with a nonabsorbable suture; traction on the rectus tendon and cautery are used to completely remove both the direct and indirect heads of the rectus from the anterior hip capsule (Fig. 1). A second suture is placed in the indirect head for later repair. After rotation and fixation of the PAO fragment, a T-shaped anterior arthrotomy is made allowing intraarticular inspection and treatment of pathology. Thereafter, the capsule is closed with absorbable suture. With the hip flexed 45°, the direct and indirect heads of the rectus tendon are repaired to bone through a drill hole in the AIIS.
Fig. 1.
Diagram illustrates the standard Bernese PAO approach with the takedown of the rectus tendon from the AIIS followed by exposure (area in black) of the anterior hip capsule. TFL = tensor fascia latae.
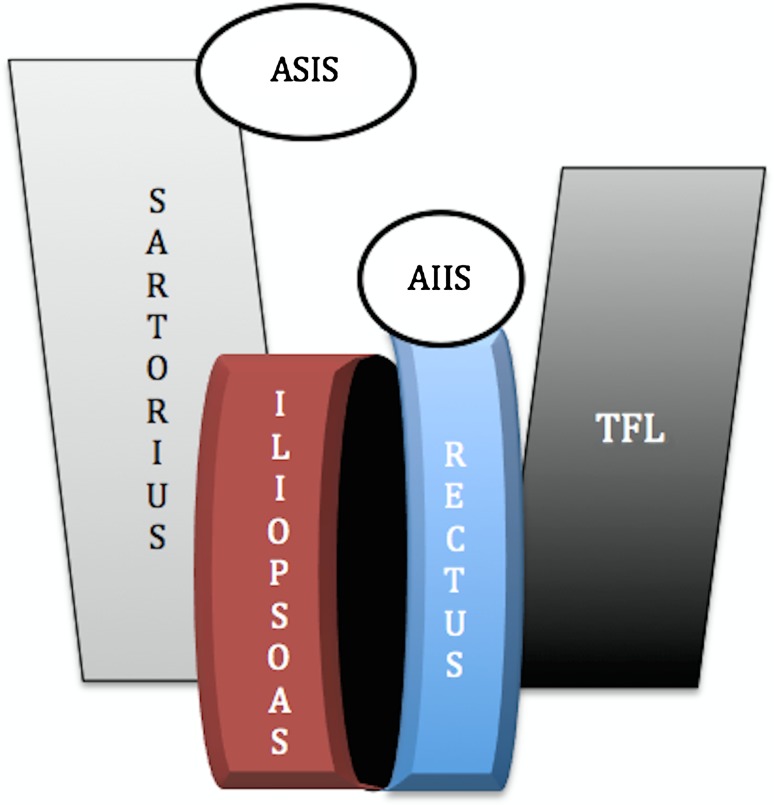
The RS approach without routine arthrotomy, not previously described, was performed according to the following. After the previously described ASIS osteotomy and tensor fascia latae/sartorius interval is developed, exposure is then continued medial to the rectus; the interval between the rectus and iliacus is developed followed by retracting the iliopsoas tendon medially for exposure of the medial hip capsule, ischium, and the superior pubic ramus (Fig. 2). Then the interval between the inferomedial capsule and iliopsoas is bluntly developed to allow placement of the angled osteotome for the ischial osteotomy. If arthrotomy is warranted for chondrolabral pathology or to improve head-neck offset, the interval can be developed between the lateral side of the rectus and tensor fascia latae.
Fig. 2.
Diagram illustrates the modified approach sparing the rectus tendon by developing a smaller window (area in black) between the iliopsoas and the rectus muscles. TFL = tensor fascia latae.
Description of Followup Routine
As part of our multimodal pain management pathway, we used an epidural placed preoperatively, which remained in place until the morning of the second postoperative day. Our standard multimodal oral medication regimen consisted of celecoxib, oxycontin, and pregabalin along with parenteral narcotics for breakthrough pain. All patients were mobilized with experienced musculoskeletal physical therapists beginning on postoperative day 1. There were no changes in the inpatient physical therapy protocol between the RT and RS groups, and in general, therapists were unaware of the change in surgical approach. However, anecdotally the therapists reported improved inpatient pain and ambulation after the modified approach was initiated.
Variables, Outcome Measures, Data Sources, and Bias
We reviewed the patient charts for outcome variables including pain scores, 0 to 10 numeric pain scale measured by the physical therapists, and distance walked in feet with physical therapy during postoperative days (POD) 1 through 3, LOS, estimated blood loss (EBL), and surgical time in minutes. Radiographically, the use of the center-edge angle with at least one other measurement, including the acetabular index, has been recommended to accurately assess dysplasia in young adults [15]. Thus, pre- and postoperative radiographs were measured as previously described [1, 6, 16] for the acetabular index, lateral center-edge angle (LCEA), anterior center-edge angle (ACEA), and Tönnis Grade of Osteoarthritis by an experienced clinician other than the operating surgeon (JAE). The reproducibility of these measures has been demonstrated as adequate to excellent in the literature [1, 3, 4, 10, 12, 21]. The postoperative correction goals were defined as an acetabular index of 0° to 10° and center-edge angles (lateral and anterior) of 20° to 35° and remained consistent throughout the study.
Statistical Analysis and Study Size
Demographics and clinical variables were analyzed using the Wilcoxon Mann-Whitney test between the groups (RT versus RS) as a result of the nonparametric nature of the data. The effect size for the Wilcoxon Mann-Whitney test was calculated using the formula r = z/sqrt(N) [7]. Values less than 0.1 were considered small, 0.1 to 0.49 medium, and ≥ 0.50 were considered large. Binary data were analyzed using chi square analysis or Fisher’s exact test when appropriate. A multivariable mixed effects regression analysis was used to compare distance walked and pain scores between the groups on POD 1 to 3 while controlling for age and sex. Cohen’s f2 was used to calculate the effect size in the regression analysis and effects were considered small for values < 0.15, moderate for 0.15 to 0.34, and large for values > 0.35 [17]. Simple logistic regression was used to allow for the reporting of odds ratios. Values less than or equal to p = 0.05 were considered statistically significant. Data are presented as median and interquartile ranges (IQRs) for continuous data and proportions for binary data.
Demographics and Description of Study Population
The groups consisted of two separate and successive series of patients who were similar in age, body mass index, and American Society of Anesthesiologists score; however, there were more men in the RT group despite no specific selection process (Table 1). The preoperative radiographs revealed a lesser degree of dysplasia (p = 0.001, r = 0.37) as measured by the LCEA in the RT group (median, 16°; IQR, 11.5°–21°) compared with the RS group (median, 10°; IQR, 3°–15°). This is likely the result of the presence of 11 retroverted hips in the RT group compared with zero retroverted hips in the RS group (p = 0.012). The RT group had a lower rate (p < 0.001, r = −0.45) of preoperative osteoarthritis changes with a median Tönnis grade of 0 (IQR, 0–0) compared with a median of 1 (IQR, 0–1) in the RT group.
Table 1.
Patient and preoperative radiographic characteristics
| Patient characteristics | Rectus takedown (n = 44) | Rectus sparing (n = 31) | p value |
|---|---|---|---|
| Age (years), median (IQR) | 23 (18.5–30) | 25 (18–31) | 0.775 |
| Sex, number (%) | |||
| Male | 16 (36) | 4 (13) | 0.033 |
| Female | 28 (64) | 27 (87) | |
| BMI (kg/m2), median (IQR) | 23.9 (21.6–27.3) | 23.0 (20.1–26.8) | 0.186 |
| ASA, median (IQR) | 1 (1–2) | 1 (1–2) | 0.881 |
IQR = interquartile range; BMI = body mass index; ASA = American Society of Anesthesiologists.
Results
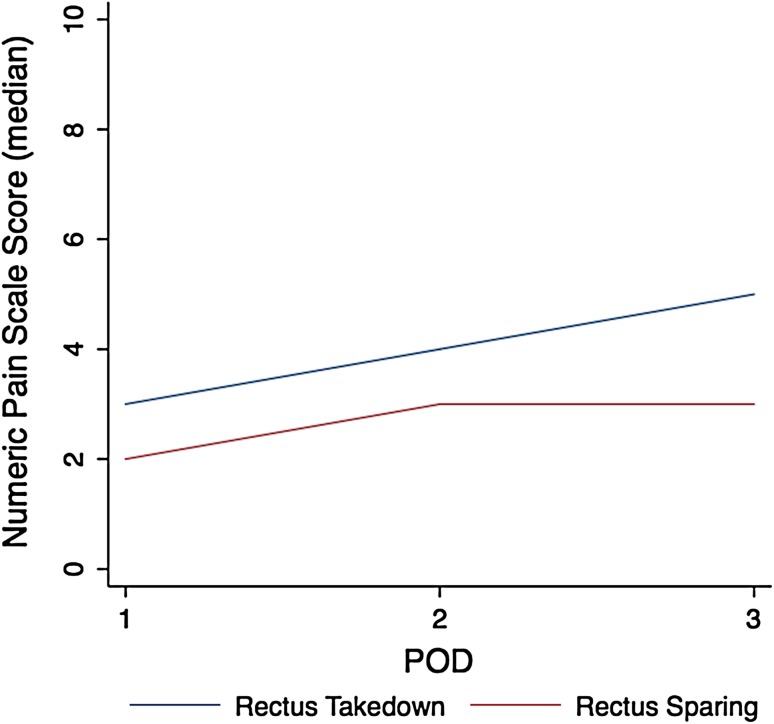
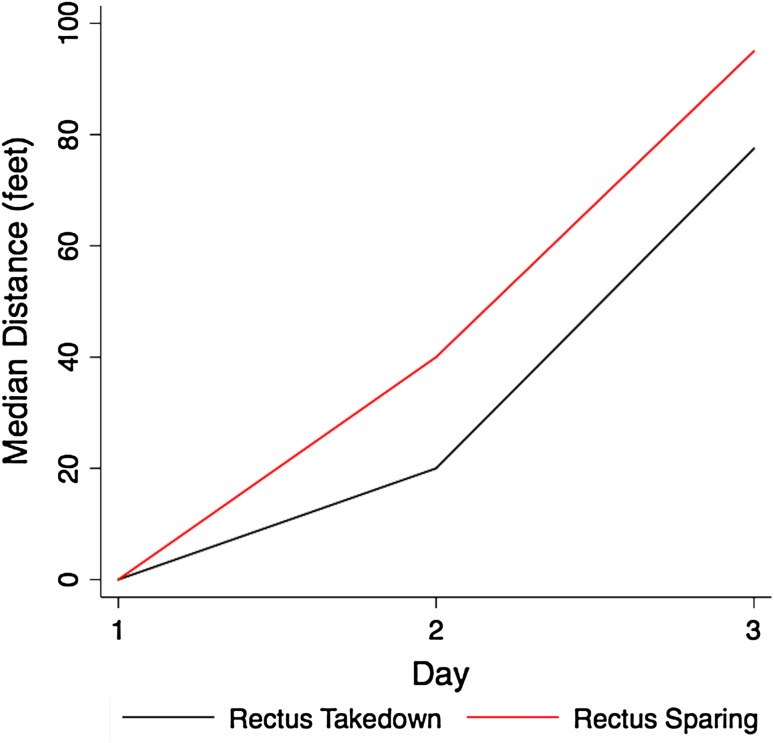
Patients who underwent PAO with a RS approach had less overall inpatient pain (RT median 4, IQR 2–5 versus RS median 2, IQR 1–4, p = 0.001, f2 = 0.059); however, this difference was probably not perceptible to the patients (Fig. 3). With the numbers available, patients treated with the RS approach had similar distances in ambulation (POD 1–3) during the hospital stay with a median ambulation of 11 feet (IQR, 0–72.5) for the RT group and a median of 30 feet (IQR, 0–100) for the RS group (p = 0.215, f2 = 0.095; Table 2; Fig. 4).
Fig. 3.
Line graph demonstrates the difference in pain scores between the groups.
Table 2.
Median (IQR) of the distance ambulated on POD 1–3 between the groups
| Periacetabular osteotomy modification | POD 1 | POD 2 | POD 3 | Overall | p value |
|---|---|---|---|---|---|
| Rectus takedown | 0 (0–3.5) | 20 (0–45) | 77.5 (25–122.5) | 11 (0–72.5) | 0.215 |
| Rectus sparing | 0 (0–15) | 40 (8–75) | 95 (45–150) | 30 (0–100) |
IQR = interquartile range; POD = postoperative day.
Fig. 4.
Line graph demonstrates distance ambulated between the groups.
Patients in the RT group had a median LOS of 4 days (IQR, 4–5) compared with a median of 3 days (IQR, 3–4) in the RS group (p < 0.001, r = 0.45). The median EBL was greater (p = 0.010, r = 0.30) in the RT group (median, 500 mL; IQR, 350–700) versus the RS group (median, 300 mL; IQR, 250–500). The median surgical time was longer (p < 0.001, r = 0.48) in patients undergoing PAO with the RT approach (median, 159.5 minutes; IQR, 145.5–177) compared with the RS approach (median, 103 minutes; IQR, 75–114).
Postoperative radiographic measurements confirmed that there was no compromise with the RS technique in obtaining satisfactory acetabular fragment correction; the “goal” coverage was noted in the same or more patients using the modified RS technique (Table 3).
Table 3.
Radiographic comparison (percent within goal)
| Postoperative measures | Goal | Rectus takedown | Rectus sparing | Odds ratio | 95% confidence interval | p value |
|---|---|---|---|---|---|---|
| Acetabular index | 0°–10° | 70% | 81% | 1.75 | 0.58–5.25 | 0.321 |
| Lateral center-edge angle | 20°–35° | 82% | 74% | 0.64 | 0.21–1.94 | 0.429 |
| Anterior center-edge angle | 20°–35° | 55% | 77% | 2.86 | 1.02–8.0 | 0.046 |
The acetabular index was in goal for 70% of the patients in the RT group and 81% of the patients in the RS group (p = 0.321). The amount of change in the acetabular index was similar (p = 0.377) between the groups with a median 11° (IQR, 7°–14°) change in the RT group and a median 12° (IQR, 9°–16°) in the RS group. The amount of undercorrection in the acetabular index was similar between the approaches (RT 16% versus RS 16%; odds ratio [OR], 1.01; 95% confidence interval [CI], 0.24–4.12; p = 0.980) as was the amount of overcorrection (RT 14% versus RS 3%; OR, 0.21; 95% CI, 0–1.96; p = 0.127).
Eighty-two percent of patients in the RT group were in goal for the LCEA and 74% achieved the goal range in the RS group (p = 0.429; Table 3). The correction evident on the LCEA was also similar between the groups (p = 0.923) with a median change in LCEA of 14° (IQR, 9.5°–18.5°) in the RT group and a median change of 13° (11°–20°) in the RS group. The RT group had fewer patients undercovered compared with the RS group (RT 2.3%, n = 1 versus RS 22.6%, n = 7; OR, 12.54; 95% CI, 1.46–108.1; p = 0.021). The median postoperative LCEA in the undercovered RS patients was 17° (IQR, 14°–19°); the median preoperative LCEA in these same patients was 2° (IQR, −8° to 8°). One patient in the RT group was undercovered with a postoperative LCEA of 0°; however, the preoperative LCEA in this patient was −18°. The amount of overcorrection between the RT group (n = 7 [16%]) and the RS group (n = 1 [3%]) was similar (OR, 0.18; 95% CI, 0.02–1.51; p = 0.113).
Fewer patients were within goal in the RT group (55%) compared with the RS group (77%) when comparing the postoperative ACEA (p = 0.046; Table 3). However, the amount of correction was similar between the groups with a median change of 14° (IQR, 6°–24°) for the RT group and 13° (IQR, 11°–18°) for the RS group (p = 0.908). Five percent (n = 2) of patients in the RT group were undercovered and 19% (n = 6) of patients in the RS group were undercovered (OR, 5.04; 95% CI, 0.94–26.9; p = 0.058). The majority of patients out of goal in the RT group were overcovered (n = 18 [41%]) compared with only 3% (n = 1) in the RS group (OR, 0.05; 95% CI, 0.006–0.39; p = 0.004). The median postoperative ACEA was 41° (IQR, 40°–42°) in the overcovered RT patients.
Discussion
Background and Rationale
Early recovery from the standard Bernese PAO is often limited by pain and symptom-based activity modulation as well as surgeon-based restrictions. Alternative approaches have been developed with the goal of being less invasive while maintaining the ability to reorient the acetabulum and preserve hip flexion strength [2, 14, 19, 20, 23]. We sought to determine whether a modified RS approach would lead to comparable inpatient pain control and ambulation with shorter LOS, less EBL, shorter surgical times, and equivalent success of acetabular reorientation.
Limitations
This study is limited by the inherent nature of retrospective reviews and by adjustments to surgical corrections by the senior surgeon (CLP) during the same period. This is likely the reason, rather than any influence of the RS approach, for the variance in obtaining the radiographic goals with more patients within goal for ACEAs in the RS group. This may reflect the senior author’s desire to precisely position the acetabular fragment and avoid anterior overcorrection to prevent future femoroacetabular impingement (FAI), because untreated FAI has been associated with inferior long-term survivorship after PAO. Although the study and control groups differed in some respects (sex, slight but probably not clinically significant differences in the magnitude of radiographic dysplasia), we attempted to minimize selection bias by performing the different surgical approaches in consecutive series of patients. The “learning curve” for adopting the RS approach was quite low and the modification of the original approach was easily incorporated into the surgical workflow and required no modification of the classic osteotomies for a standard PAO [16]. The fact that preservation of the rectus tendon origin was intuitive and did not complicate osteotomy, mobilization or reorientation of the acetabular fragment made it relatively easy to perform on a consecutive series of patients without the need for selection of “simpler” cases. Lastly, although there was no change in preoperative indications for surgery, the groups differed radiographically. The RS group demonstrated less overall dysplasia, more osteoarthritis (Tönnis grade), and fewer cases of acetabular retroversion.
Our data demonstrated that patients undergoing PAO with a RS approach experienced less overall inpatient pain with a median difference of two on a 0 to 10 numeric pain scale. Although this difference may not have been perceptible to the patients, it still may have contributed to improved ability to perform inpatient physical therapy as noted by our physical therapists. Nevertheless, because PAO involves substantial subperiosteal dissection and multiple pelvic osteotomies regardless of approach, it is possible that soft tissue management may be only a minor contributor to overall pain levels as an inpatient.
With the numbers available, patients undergoing PAO with the modified technique ambulated similar distances while an inpatient. Similarly, this may again be reflective of the soft tissue component of the operation being a minor factor in ambulation potential. Undoubtedly more sensitive measurements such as gait studies or muscle function studies would provide greater insight into this question.
We also found improved perioperative variables including a shorter hospital LOS, less EBL, and decreased surgical times with the RS technique. Previous literature reports similar improvements in the perioperative variables. Troelsen et al. [23] compared an ilioinguinal approach versus a minimally invasive (both RS) and demonstrated decreased LOS, blood loss, and surgical times for the minimally invasive (so-called transsartorius approach) group.
The ability to meet postoperative acetabular coverage goals was not compromised by the less invasive approach. This was similar the finding of Bernstein et al. [2] and Troelsen et al. [23] who both reported similar acetabular correction normalization between groups with standard versus minimally invasive approaches.
A modification of the Bernese PAO with preservation of the rectus femoris origin demonstrated equivalent or improved inpatient pain and ambulation, marginally shorter LOS, less EBL, and shorter surgical times. Perhaps most importantly, the ability to meet postoperative acetabular coverage goals was not compromised by the modified approach. The approach modification was straightforward to implement (did not require stringent patient selection criteria) and did not compromise acetabular fragment mobilization or final positioning. More definitive evidence for clinical superiority in terms of pain, ambulation, and return of muscle function will likely require more sophisticated instruments such as gait analysis, muscle strength testing, and longer-term outcome studies with sensitive instruments.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Anderson LA, Gililland J, Pelt C, Linford S, Stoddard GJ, Peters CL. Center edge angle measurement for hip preservation surgery: technique and caveats. Orthopedics. 2011;34:86. doi: 10.3928/01477447-20101221-17. [DOI] [PubMed] [Google Scholar]
- 2.Bernstein P, Thielemann F, Gunther KP. A modification of periacetabular osteotomy using a two-incision approach. Open Orthop J. 2007;1:13–18. doi: 10.2174/1874325000701010013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bouttier R, Morvan J, Mazieres B, Rat AC, Ziegler LE, Fardellone P, Fautrel B, Guillemin F, Pouchot J, Roux C, Coste J, Saraux A. Reproducibility of radiographic hip measurements in adults. Joint Bone Spine. 2013;80:52–56. doi: 10.1016/j.jbspin.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 4.Carlisle JC, Zebala LP, Shia DS, Hunt D, Morgan PM, Prather H, Wright RW, Steger-May K, Clohisy JC. Reliability of various observers in determining common radiographic parameters of adult hip structural anatomy. Iowa Orthop J. 2011;31:52–58. [PMC free article] [PubMed] [Google Scholar]
- 5.Clohisy JC, Barrett SE, Gordon JE, Delgado ED, Schoenecker PL. Periacetabular osteotomy in the treatment of severe acetabular dysplasia. Surgical technique. J Bone Joint Surg Am. 2006;88(Suppl 1):65–83. doi: 10.2106/JBJS.E.00887. [DOI] [PubMed] [Google Scholar]
- 6.Clohisy JC, Carlisle JC, Beaule PE, Kim YJ, Trousdale RT, Sierra RJ, Leunig M, Schoenecker PL, Millis MB. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90(Suppl 4):47–66. doi: 10.2106/JBJS.H.00756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Field A. Discovering Statistics Using SPSS. London, UK: Sage Publications; 2009. [Google Scholar]
- 8.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res. 1988;232:26–36. [PubMed] [Google Scholar]
- 9.Hussell JG, Mast JW, Mayo KA, Howie DW, Ganz R. A comparison of different surgical approaches for the periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:64–72. [PubMed] [Google Scholar]
- 10.Mast NH, Impellizzeri F, Keller S, Leunig M. Reliability and agreement of measures used in radiographic evaluation of the adult hip. Clin Orthop Relat Res. 2011;469:188–199. doi: 10.1007/s11999-010-1447-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matta JM, Stover MD, Siebenrock K. Periacetabular osteotomy through the Smith-Petersen approach. Clin Orthop Relat Res. 1999;363:21–32. [PubMed] [Google Scholar]
- 12.Monazzam S, Bomar JD, Cidambi K, Kruk P, Hosalkar H. Lateral center-edge angle on conventional radiography and computed tomography. Clin Orthop Relat Res. 2013;471:2233–2237. doi: 10.1007/s11999-012-2651-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murphy SB, Millis MB, Hall JE. Surgical correction of acetabular dysplasia in the adult. A Boston experience. Clin Orthop Relat Res. 1999;363:38–44. [PubMed] [Google Scholar]
- 14.Pajarinen J, Hirvensalo E. Two-incision technique for rotational acetabular osteotomy: good outcome in 35 hips. Acta Orthop Scand. 2003;74:133–139. doi: 10.1080/00016470310013842. [DOI] [PubMed] [Google Scholar]
- 15.Pereira F, Giles A, Wood G, Board TN. Recognition of minor adult hip dysplasia: which anatomical indices are important? Hip Int. 2014;24:175–179. doi: 10.5301/hipint.5000119. [DOI] [PubMed] [Google Scholar]
- 16.Peters CL, Erickson JA, Hines JL. Early results of the Bernese periacetabular osteotomy: the learning curve at an academic medical center. J Bone Joint Surg Am. 2006;88:1920–1926. doi: 10.2106/JBJS.E.00515. [DOI] [PubMed] [Google Scholar]
- 17.Selya AS, Rose JS, Dierker LC, Hedeker D, Mermelstein RJ. A practical guide to calculating Cohen’s f(2), a measure of local effect size, from PROC MIXED. Front Psychol. 2012;3:111. doi: 10.3389/fpsyg.2012.00111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85:278–286. doi: 10.2106/00004623-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 19.Soballe K, Troelsen A. Approaches and perioperative management in periacetabular osteotomy surgery: the minimally invasive transsartorial approach. Instr Course Lect. 2013;62:297–303. [PubMed] [Google Scholar]
- 20.Sucato DJ, Tulchin K, Shrader MW, DeLaRocha A, Gist T, Sheu G. Gait, hip strength and functional outcomes after a Ganz periacetabular osteotomy for adolescent hip dysplasia. J Pediatr Orthop. 2010;30:344–350. doi: 10.1097/BPO.0b013e3181d9bfa2. [DOI] [PubMed] [Google Scholar]
- 21.Tan L, Aktas S, Copuroglu C, Ozcan M, Ture M. Reliability of radiological parameters measured on anteroposterior pelvis radiographs of patients with developmental dysplasia of the hip. Acta Orthop Belg. 2001;67:374–379. [PubMed] [Google Scholar]
- 22.Tibor LM, Sink EL. Periacetabular osteotomy for hip preservation. Orthop Clin North Am. 2012;43:343–357. doi: 10.1016/j.ocl.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 23.Troelsen A, Elmengaard B, Soballe K. Comparison of the minimally invasive and ilioinguinal approaches for periacetabular osteotomy: 263 single-surgeon procedures in well-defined study groups. Acta Orthop. 2008;79:777–784. doi: 10.1080/17453670810016849. [DOI] [PubMed] [Google Scholar]
- 24.Troelsen A, Elmengaard B, Soballe K. Medium-term outcome of periacetabular osteotomy and predictors of conversion to total hip replacement. J Bone Joint Surg Am. 2009;91:2169–2179. doi: 10.2106/JBJS.H.00994. [DOI] [PubMed] [Google Scholar]
- 25.Trousdale RT, Cabanela ME. Lessons learned after more than 250 periacetabular osteotomies. Acta Orthop Scand. 2003;74:119–126. doi: 10.1080/00016470310013824. [DOI] [PubMed] [Google Scholar]