Abstract
Background
Reconstruction of large acetabular defects remains a substantial challenge in hip arthroplasty. There remains a paucity of data on the long-term results of acetabular trabecular metal augments.
Questions/purposes
The purpose of this study was to assess the survivorship, clinical outcomes, restoration of center of rotation of the hip, and radiological signs of component fixation of trabecular metal augments in the context of reconstruction of acetabular defects.
Methods
Between 2002 and 2005, we performed 56 revision (n = 53) and primary (n = 3) THAs using trabecular metal augments in combination with a trabecular metal acetabular component. Of the 56 patients, 16 (29%) died during followup. Of the 40 surviving patients, 37 (93%) had complete radiological followup, 23 (58%) had complete outcome questionnaire followup, and 17 (42%) provided partial questionnaire responses in the clinic or over the telephone. Median followup was 110 months (range, 88–128 months). During that period, we used these implants when preoperative templating indicated that an augment would be required to achieve acetabular implant stability with restoration of the hip center of rotation. We also chose during surgery to use an augment when we could not achieve a stable acetabular trial component without one. The combination of trabecular metal augments and trabecular metal shells was used in 18% (53 of 292) of our acetabular revisions during that time. Survivorship, functional outcome (WOMAC and Oxford hip score), health status (SF-12), and osseointegration according to the criteria of Moore and presence of radiolucencies were determined.
Results
Survivorship of the augments at 10 years was 92% (95% confidence interval, 81%–97%). Four patients underwent cup revision, one for infection and three for loosening. The mean WOMAC global score was 79 (SD 17), the mean Oxford hip score 76 (SD 18), the mean physical component SF-12 score was 39 (SD 11), and the mean mental component SF-12 score was 52 (SD 9). The center of rotation was corrected from more than 35 mm above the inter-teardrop line in 48 of 56 patients preoperatively to only five of 46 postoperatively. One patient had radiographic findings suggestive of loosening, but this patient was asymptomatic.
Conclusions
The results of the acetabular trabecular metal augments continue to be encouraging in the medium to long term with low rates of revision or loosening in this complex group of patients. We continue to recommend the use of these augments in the reconstruction of complex acetabular defects.
Level of Evidence
Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
The creation of a stable acetabular construct and the restoration of lost bone stock remain a significant challenge during revision hip arthroplasty [24]. Smaller bony defects can be addressed with porous-coated components [37]. If the defect is uncontained and too large, sufficient contact with host bone will not be achieved with this tactic and therefore sufficient stability to allow bone ingrowth will not be achieved [18]. Alternatives include impaction allografting with cement with containment created by the use of rim meshes [16, 34], the use of bulk allografts [32], bilobed acetabular components [7], jumbo acetabular components [11, 40], high placement of the hip center of rotation [10], or the use of a reconstruction cage [17].
Our unit has previously described the early results of reconstruction of acetabular bone loss with the use of porous trabecular metal augments in conjunction with a trabecular metal shell in revision hip arthroplasty [33]. Here, we provide a longer-term followup of those patients with the addition of a further 19 patients. Porous trabecular metal, composed of tantalum, has theoretical advantages over conventional porous metals such as titanium, including a high coefficient of friction, a modulus of elasticity closer to that of bone, high volume porosity, and highly interconnected pores resembling the structure of trabecular bone [5, 8]. These properties facilitate early implant stability and bone ingrowth combined with predictable and reliable mechanical properties in the long term.
The purpose of this study was to evaluate (1) the survivorship of these reconstructions in the medium to long term; (2) the functional outcome and health status of these patients; (3) the restoration of the center of rotation of the hip at reconstruction; and (4) the osseointegration of the components as assessed on plain radiographs.
Patients and Methods
Fifty-six patients had trabecular metal augments in conjunction with a trabecular metal acetabular component implanted in our unit between September 2002 and December 2005. Fifty-three of the procedures were revision arthroplasties and three were primary procedures (idiopathic osteonecrosis in two hips and osteonecrosis after fracture-dislocation of the hip). Six of the revisions were second-stage reimplantations after infection. In three hips there was a pelvic discontinuity, addressed by plating of the posterior column. Of the 56 patients, 16 (29%) died during followup. Of the 40 surviving patients, 37 (93%) had complete radiological followup, 23 (58%) had complete outcome questionnaire followup, and 17 (42%) provided partial questionnaire responses in the clinic or over the telephone. Median followup was 110 months (range, 88–128 months). During that period, we used these implants when preoperative templating indicated that an augment would be required to achieve acetabular implant stability with restoration of the hip center of rotation. We also chose during surgery to use an augment when we could not achieve a stable acetabular trial component without one. We used the combination of trabecular metal augments and trabecular metal shells in 18% (53 of 292) of our acetabular revisions.
The interval between the index surgery and death in the patients who died (n = 16) was a median of 65 months (range, 24–106 months). The mean age at the time of surgery was 67 years (SD 14.8). There were 30 women and 26 men. The mean body mass index was 27 kg/m2 (SD 4.3). Twenty-seven operations were performed on the left and 29 on the right.
Trabecular metal revision shells were used in all patients (TMR; Zimmer, Inc, Warsaw, IN, USA). Polyethylene liners were cemented into the shells using Simplex with tobramycin in 40 patients (Stryker Canada, Ontario, Canada) or Palacos with gentamycin in 16 patients (Zimmer, Inc). The surgical technique used has been described previously [33]. In short, the need for augments was anticipated on the basis of preoperative templating and intraoperative confirmation of poor stability of the trial components without an augment. The acetabulum was initially reamed for the shell to restore the hip center and an augment used if the surgeon felt this was necessary to restore the center of rotation and achieve stability of the acetabular component by providing support. Trials were used to confirm the optimum implant sizes to achieve this aim. Secondary reaming of the defect was performed with a hemispherical reamer matching the planned size of the augment. Where the surgeon felt they were required, additional screw holes were created with a high-speed 4-mm burr into the cup or the augment to enhance screw fixation. Large morsels of allograft were packed into the augment and impaction grafted into any osteolytic defects. Host bone contact was less than 50% in 31 patients. Bone cement was not deliberately inserted between the augment and shell in all cases. The median number of screws placed through an augment into host bone was two (range, zero to five) and the median number of screws placed through the shell was three (range, two to five). The median trabecular metal shell outer diameter was 62 mm (range, 48–72 mm). The most commonly used trabecular metal augments were the conventional hemispherical augments. These come in a range of diameters (50–70 mm) and thicknesses (10–30 mm); the three most common sizes augments used were the 58 × 20 mm (n = 16), 58 × 10 mm (n = 12), and 56 × 20 mm (n = 7).
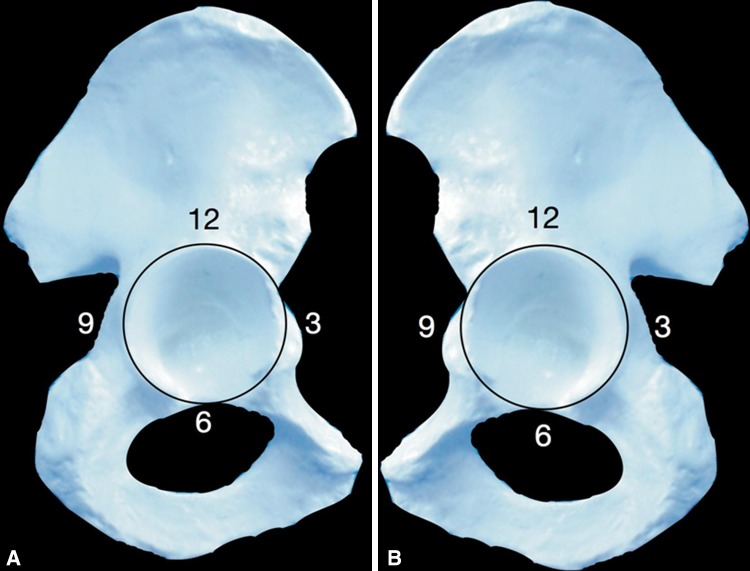
The Paprosky classification [26] was 2A in six patients, 2B in nine patients, 2C in two patients, 3A in 28 patients, and 3B in 11 patients. The classification of the defect was based on the preoperative AP and iliac oblique (Judet) views of the pelvis and confirmed intraoperatively. Further classification of the defect was performed intraoperatively by plotting the location of the defect according to the acetabular clock face where, for example, in a right hip 12 o’clock is superior, 9 o’clock posterior, and 3 o’clock anterior (Fig. 1) [33]. Preoperatively the hip center was located at a mean of 48 mm above the interteardrop line (SD 10.0; range, 29–77 mm). A high hip center was defined as being more than 35 mm above the interteardrop line [2, 28, 33] and this was the case in 48 of the 56 patients preoperatively. Radiographic signs of osseointegration between host bone and the acetabular augment were assessed according to the criteria of Moore et al. [23]. The following signs were noted: (1) absence of radiolucent lines; (2) presence of a superolateral buttress; (3) presence of medial stress shielding; (4) presence of radial trabeculae; and (5) presence of an inferomedial buttress. Moore et al. noted that when three or more signs are present, the positive predictive value for bone ingrowth is 96.9%, the sensitivity is 89.9%, and the specificity 76.9%. The presence or absence of radiolucent lines between the cup/host bone and augment/host bone interfaces was noted.
Fig. 1A–B.
An illustration shows the acetabular clock face for the (A) right and (B) left hips.
Health status was assessed with the SF-12 questionnaire [39]. Hip functional outcome was assessed with the Oxford hip score (OHS) [9] and patient functional outcome was assessed using the WOMAC [4].
Statistics
A D’Agostino and Pearson normality test was performed to determine the distribution of data. Where data were normally distributed, central tendency is described with the mean and SDs. The functional outcome scores were normally distributed. Where it was not normally distributed, the median and range were used. Kaplan-Meier survivorship analysis with 95% confidence intervals was performed for the endpoints of revision of the modular tantalum augments or reoperation of any description on the affected hip.
Results
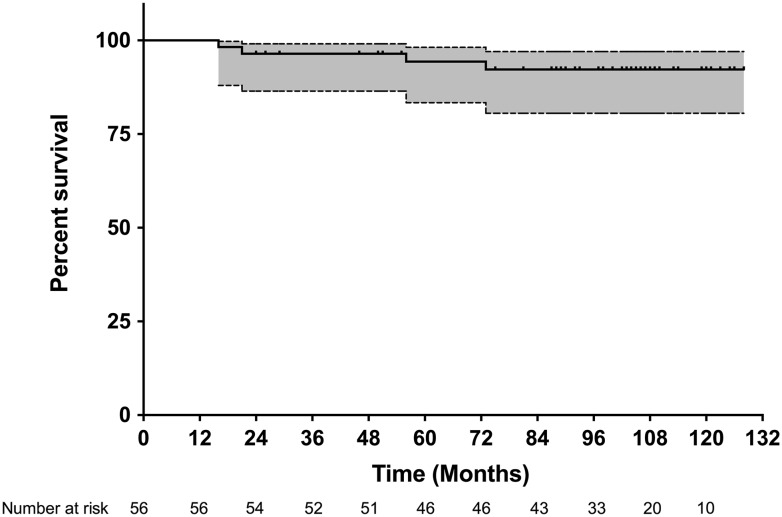
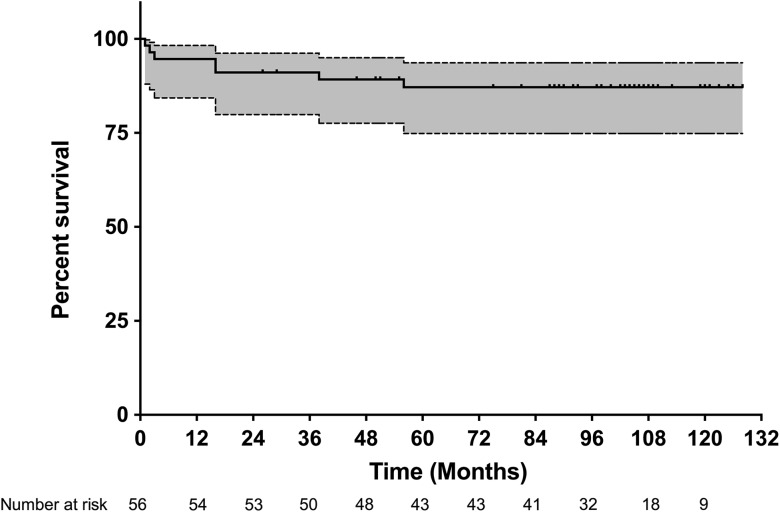
The survivorship of the modular tantalum augments at 10 years, with revision as the end point, was 92% (81%–97%; Fig. 2). The survivorship of the affected hip without reoperation for any reason at 10 years was 87% (75%–94%; Fig. 3). Four revisions of the acetabular augments and associated shells were performed. One was performed for deep infection (initial defect a Paprosky 3A with no discontinuity). The patient was treated with a staged revision, which was complicated by premature loosening and another reoperation for hematoma formation. Three patients underwent revisions for aseptic loosening of the acetabular augment and shell. In addition to the revisions described, three patients underwent a reoperation without revision of the well-fixed augments or shells, including one application of a strut graft to the femur and two procedures for recurrent instability.
Fig. 2.
The survivorship curve shows the Kaplan-Meier analysis with 95% confidence intervals with the need for revision of trabecular metal augment as the endpoint.
Fig. 3.
The survivorship curve shows the Kaplan-Meier analysis with 95% confidence intervals with the need for reoperation for any cause as the endpoint.
The mean WOMAC global score was 79 (SD 17) and the OHS 76 (SD 18). The mean SF-12 score was 39 (SD 10.8) for the physical component and 52 (SD 9.2) for the mental component score. No issues with function or pain were reported by patients (n = 17) followed up in the clinic or over the telephone who did not complete the outcome questionnaire in full.
Postoperatively the mean hip center was 28 mm (SD 6.5; range, 16–48 mm) and five patients had a hip center more than 35 mm above the interteardrop line.
The radiographs of the surviving patients demonstrated five signs of osseointegration in two patients, four signs in 23 patients (Fig. 4), three signs in 11 patients, and two in one patients. In the three patients in whom a radiograph had not been performed within the last 2 years, the latest radiograph available revealed there were four signs of osseointegration in two patients and three signs in one. Radiolucent lines between the acetabular augment and the host bone were not visualized in any of the patients other than those that had been revised for loosening of the augment and acetabular construct; none of these radiolucencies had recurred.
Fig. 4A–C.
The figure shows a typical case with the use of a trabecular metal shell and augment for reconstruction: (A) preoperative AP radiograph; (B) followup AP radiograph at 10 years; (C) followup lateral radiograph at 10 years.
Discussion
The reconstruction of large acetabular defects is a substantial technical challenge. A number of different techniques have been described to facilitate reconstruction. Reconstruction with trabecular metal augments in conjunction with trabecular metal acetabular components is one option that is becoming popular as a result of favorable early results. The longer-term results of the use of this strategy are not known. We therefore sought to evaluate the survivorship, patient-reported outcomes, hip center restoration, and osseointegration of reconstructions using these components in our unit.
Our study is limited by the lack of a comparison group and the small size of the series, as is common in complex revision THA studies. The mean age at followup in the series was 76 years. The SF-12 scores in this series are comparable to population normal values for this age group in large health surveys [38]. This method of reconstruction with the described implants was used as our standard technique during the period of study in which restoration of a migrated center of rotation was desired by the surgeon and adequate stability could not be achieved with a revision shell alone. This represented 18% of our acetabular revisions during this period. The mortality rate in the followup period limits our ability to obtain complete clinical and radiological followup; this is again typical of the population studied. We feel 93% radiological followup (n = 37 of 40) in the surviving patients is good for the population and period of followup. Whereas complete patient-reported outcome questionnaires were only available in 58% of the surviving patients (n = 23 of 40), which is a limitation of the report, clinic or telephone followup was conducted for all surviving patients with none of the patients reporting issues relating to function or pain. The radiographic assessment was performed by an author from the institution, which is a source of potential bias, but the author was not involved in any of the operations.
Survivorship in the presented cohort was 92% at 10 years when septic and aseptic loosening of the acetabular construct was considered as the endpoint. This experience compares favorably with the report of Abolghasemian et al. [1] in which the survivorship of trabecular metal shells in combination with augments was noted to be 91.1% at 5 years in a series of 34 patients. Although a different classification scheme was used here [29], all three failures resulting from aseptic loosening in their series were in defects equivalent to 3B in the Paprosky classification. Sporer and Paprosky reported no failures resulting from aseptic loosening in a series of 3A defects treated with trabecular metal shells and augments at a mean followup of 3.1 years (28 patients) [35]. In a series of 13 patients with 3B defects, one failure resulting from aseptic loosening at a mean followup of 2.6 years was reported [36]. Structural acetabular allografts are associated with higher complication rates where the allograft supports more than 50% of the implanted components [25]. The results of minor column defects (< 50% of implanted component supported by graft) indicate that survivorship of 80% at a mean followup of 10 years with aseptic loosening as the endpoint may be achieved [42], falling to 55% at 20 years [22]. When a major column graft is used (typically when > 50% of the implanted component is supported by graft), survivorship of 55% at a mean followup of 7 years has been shown [14]. The use of bilobed acetabular components has been associated with failure rates of 24% at a mean followup of less than 4 years [7]. Jumbo cups have been associated with favorable survivorship of 92% to 96% at 14 to 16 years [19, 27] where adequate support can be obtained. Acetabular impaction grafting has shown promising results with 87% survivorship for aseptic loosening at 20 years and 75% for any cause of failure [30]; however, it is technically demanding, time-consuming, and may be associated with higher failure rates in massive bone loss [6]. Combining the technique with trabecular metal augments to support large areas of graft offers promising early results [15].
When compared with our earlier report of patients undergoing this procedure [33], there has been a trend toward a decline in the recorded OHS, which is typical of aging in this population [13, 20]. The WOMAC score did not show any signs of deterioration in comparison with our earlier series, in contrast to the OHS. As is the case with functional outcome scores such as the OHS [13], the activity levels of patients after revision are best predicted by preoperative activity levels [41]. Direct comparison with the functional outcomes of other methods of reconstruction in this population is hampered by the variety of outcome measures used and different methods of reporting. Abolghasemian et al. [1] reported a mean OHS of 38 (on a 0–48 scale) after reconstruction of patients with substantial acetabular bone loss using the same implants as reported here. Sporer and Paprosky [35, 36] reported average modified Postel-Merle d’Aubigne scores of 10.3 and 10.6, respectively, in patients undergoing reconstruction for Paprosky 3B defects with discontinuity and patients with a 3A defect reconstructed with a trabecular metal acetabular component with or without an augment. Gustke et al. [19] and Patel et al. [27] reported average Harris hip scores (HHSs) of 72 and 81, respectively, after reconstruction with jumbo cups. Schreurs et al. [31] reported an average HHS of 79 after reconstruction with impaction grafting and Gehrke et al. [15] an average HHS of 82 when combining impaction grafting with a trabecular metal augment.
The use of the combination of trabecular metal augments and shells allowed us to restore the center of rotation and therefore biomechanics of the hips in the majority of the patients in our series. A high center of rotation of the hip is defined as more than 35 mm above the interteardrop line [2, 28] with a systematic review of the use of highly porous metals in acetabular revisions demonstrating correction from a mean of 39 mm to 24 mm [3]. Successful restoration of the hip center was achieved in all but five of the patients in the series. None of the patients with a hip center above 35 mm failed, the grade of osseointegration was 5 in one patient, 4 in two patients, and 3 in two patients. Although a purely elevated hip center of rotation may not necessarily lead to poor hip abductor function if an increased neck length is used [12], the increased lever arm acting on the head/neck taper in this situation is a potential cause for concern. Elevation of the hip center may also require trochanteric advancement and pelvic osteoplasty to restore the abductor function and prevent impingement and instability [11]. The results in our study are favorable in comparison to other series using similar [1] and alternative techniques [21].
Moore et al.’s criteria for the assessment of osseointegration indicate that if three or more signs of osseointegration between porous components and host bone are present, there is a 97% chance of bone ingrowth into that component [23]. Only one case in this series had a grade of less than 3 according to these criteria. The successful osseointegration of the augments, maintained in the medium to long term in this complex group of patients, is encouraging and similar to the findings of Abolghasemian et al. [1]. The only case in our series with a score of less than 3 was asymptomatic and the Moore grading was stable over time. These results were obtained despite the fact that 31 of the patients in this series had less than 50% contact between host bone and the trabecular metal shell or augment.
In summary, the promising results of our earlier experience [33] have been maintained in the medium to long term. Good survivorship, patient-reported outcome measures, restoration of center of rotation of the hip, and osseointegration of the implants have been demonstrated at 7 to 11 years followup. This surgical technique continues to be our default method where the surgeon wishes to correct the center of rotation of the hip and this cannot be achieved with standard revision components but adequate stability can be achieved without the need for the use of a trabecular metal cup/cage construct.
Acknowledgments
We thank Nelson V. Greidanus MD, MPH, for contributing patients to the study and Daphné Savoy BA, for her assistance in the preparation of the manuscript.
Footnotes
One or more of the authors (BAM, CPD, DSG) certify that they have or may receive payments or benefits (eg, serve as a consultant) from a commercial entity (Zimmer, Inc, Warsaw, IN, USA) related to this work. The institution of the authors has received funding from Zimmer, Inc.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Abolghasemian M, Tangsataporn S, Sternheim A, Backstein D, Safir O, Gross AE. Combined trabecular metal acetabular shell and augment for acetabular revision with substantial bone loss: a mid-term review. J Bone Joint Surg Br. 2013;95:166–172. doi: 10.1302/0301-620X.95B2.30608. [DOI] [PubMed] [Google Scholar]
- 2.Antoniades J, Pellegrini VD. Cross-sectional anatomy of the ilium: implications for acetabular component placement in total hip arthroplasty. Clin Orthop Relat Res. 2012;470:3537–3541. doi: 10.1007/s11999-012-2574-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Banerjee S, Issa K, Kapadia BH, Pivec R, Khanuja HS, Mont MA. Systematic review on outcomes of acetabular revisions with highly-porous metals. Int Orthop. 2014;38:689–702. doi: 10.1007/s00264-013-2145-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 5.Bobyn JD, Poggie RA, Krygier JJ, Lewallen DG, Hanssen AD, Lewis RJ, Unger AS, O’Keefe TJ, Christie MJ, Nasser S, Wood JE, Stulberg SD, Tanzer M. Clinical validation of a structural porous tantalum biomaterial for adult reconstruction. J Bone Joint Surg Am. 2004;86(Suppl 2):123–129. doi: 10.2106/00004623-200412002-00017. [DOI] [PubMed] [Google Scholar]
- 6.Buttaro MA, Comba F, Pusso R, Piccaluga F. Acetabular revision with metal mesh, impaction bone grafting, and a cemented cup. Clin Orthop Relat Res. 2008;466:2482–2490. doi: 10.1007/s11999-008-0442-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen WM, Engh CA, Hopper RH, McAuley JP. Acetabular revision with use of a bilobed component inserted without cement in patients who have acetabular bone-stock deficiency. J Bone Joint Surg Am. 2000;82:197–206. doi: 10.2106/00004623-200002000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Christie MJ. Clinical applications of trabecular metal. Am J Orthop. 2002;31:219–220. [PubMed] [Google Scholar]
- 9.Dawson J, Fitzpatrick R, Carr A, Murray DW. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br. 1996;78:185–190. [PubMed] [Google Scholar]
- 10.Dearborn JT, Harris WH. High placement of an acetabular component inserted without cement in a revision total hip arthroplasty. Results after a mean of ten years. J Bone Joint Surg Am. 1999;81:469–480. doi: 10.2106/00004623-199904000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Dearborn JT, Harris WH. Acetabular revision arthroplasty using so-called jumbo cementless components: an average 7-year follow-up study. J Arthroplasty. 2000;15:8–15. doi: 10.1016/S0883-5403(00)90999-9. [DOI] [PubMed] [Google Scholar]
- 12.Delp SL, Wixson RL, Komattu AV, Kocmond JH. How superior placement of the joint center in hip arthroplasty affects the abductor muscles. Clin Orthop Relat Res. 1996;328:137–146. doi: 10.1097/00003086-199607000-00022. [DOI] [PubMed] [Google Scholar]
- 13.Field RE, Cronin MD, Singh PJ. The Oxford hip scores for primary and revision hip replacement. J Bone Joint Surg Br. 2005;87:618–622. doi: 10.1302/0301-620X.87B5.15390. [DOI] [PubMed] [Google Scholar]
- 14.Garbuz D, Morsi E, Gross AE. Revision of the acetabular component of a total hip arthroplasty with a massive structural allograft. Study with a minimum five-year follow-up. J Bone Joint Surg Am. 1996;78:693–697. doi: 10.2106/00004623-199605000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Gehrke T, Bangert Y, Schwantes B, Gebauer M, Kendoff D. Acetabular revision in THA using tantalum augments combined with impaction bone grafting. Hip Int. 2013;23:359–365. doi: 10.5301/hipint.5000044. [DOI] [PubMed] [Google Scholar]
- 16.Gie GA, Linder L, Ling RS, Simon JP, Slooff TJ, Timperley AJ. Impacted cancellous allografts and cement for revision total hip arthroplasty. J Bone Joint Surg Br. 1993;75:14–21. doi: 10.1302/0301-620X.75B1.8421012. [DOI] [PubMed] [Google Scholar]
- 17.Gross AE. Revision arthroplasty of the acetabulum with restoration of bone stock. Clin Orthop Relat Res. 1999;369:198–207. doi: 10.1097/00003086-199912000-00021. [DOI] [PubMed] [Google Scholar]
- 18.Gross AE, Goodman S. The current role of structural grafts and cages in revision arthroplasty of the hip. Clin Orthop Relat Res. 2004;429:193–200. doi: 10.1097/01.blo.0000149822.49890.5e. [DOI] [PubMed] [Google Scholar]
- 19.Gustke KA, Levering MF, Miranda MA. Use of jumbo cups for revision of acetabulae with large bony defects. J Arthroplasty. 2013;29:199–203. doi: 10.1016/j.arth.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 20.Judge A, Arden NK, Batra RN, Thomas G, Beard D, Javaid MK, Cooper C, Murray DW, Exeter Primary Outcomes Study (EPOS) group. The association of patient characteristics and surgical variables on symptoms of pain and function over 5 years following primary hip-replacement surgery: a prospective cohort study. BMJ Open. 2013;3:e002453. [DOI] [PMC free article] [PubMed]
- 21.Kim D-H, Cho S-H, Jeong S-T, Park H-B, Hwang S-C, Park J-S. Restoration of the center of rotation in revision total hip arthroplasty. J Arthroplasty. 2010;25:1041–1046. doi: 10.1016/j.arth.2009.07.023. [DOI] [PubMed] [Google Scholar]
- 22.Lee PTH, Raz G, Safir OA, Backstein DJ, Gross AE. Long-term results for minor column allografts in revision hip arthroplasty. Clin Orthop Relat Res. 2010;468:3295–3303. doi: 10.1007/s11999-010-1591-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moore MS, McAuley JP, Young AM, Engh CA., Sr Radiographic signs of osseointegration in porous-coated acetabular components. Clin Orthop Relat Res. 2006;444:176–183. doi: 10.1097/01.blo.0000201149.14078.50. [DOI] [PubMed] [Google Scholar]
- 24.Paprosky WG, Magnus RE. Principles of bone grafting in revision total hip arthroplasty. Acetabular technique. Clin Orthop Relat Res. 1994;298:147–155. [PubMed] [Google Scholar]
- 25.Paprosky WG, Martin EL. Structural acetabular allograft in revision total hip arthroplasty. Am J Orthop. 2002;31:481–484. [PubMed] [Google Scholar]
- 26.Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty. 1994;9:33–44. doi: 10.1016/0883-5403(94)90135-X. [DOI] [PubMed] [Google Scholar]
- 27.Patel JV, Masonis JL, Bourne RB, Rorabeck CH. The fate of cementless jumbo cups in revision hip arthroplasty. J Arthroplasty. 2003;18:129–133. doi: 10.1054/arth.2003.50038. [DOI] [PubMed] [Google Scholar]
- 28.Russotti GM, Harris WH. Proximal placement of the acetabular component in total hip-arthroplasty—a long-term follow-up-study. J Bone Joint Surg Am. 1991;73:587–592. [PubMed] [Google Scholar]
- 29.Saleh KJ, Holtzman J, Gafni ASaleh L, Jaroszynski G, Wong P, Woodgate I, Davis A, Gross AE. Development, test reliability and validation of a classification for revision hip arthroplasty. J Orthop Res. 2001;19:50–56. [DOI] [PubMed]
- 30.Schreurs BW, Keurentjes JC, Gardeniers JWM, Verdonschot N, Slooff TJ, Veth RPH. Acetabular revision with impacted morsellised cancellous bone grafting and a cemented acetabular component: a 20- to 25-year follow-up. J Bone Joint Surg Br. 2009;91:1148–1153. doi: 10.1302/0301-620X.91B9.21750. [DOI] [PubMed] [Google Scholar]
- 31.Schreurs BW, Luttjeboer J, Thien TM, de Waal Malefijt MC, Buma P, Veth RPH, Slooff TJ. Acetabular revision with impacted morsellized cancellous bone graft and a cemented cup in patients with rheumatoid arthritis. A concise follow-up, at eight to nineteen years, of a previous report. J Bone Joint Surg Am. 2009;91:646–651. [DOI] [PubMed]
- 32.Shinar AA, Harris WH. Bulk structural autogenous grafts and allografts for reconstruction of the acetabulum in total hip arthroplasty. Sixteen-year-average follow-up. J Bone Joint Surg Am. 1997;79:159–168. doi: 10.2106/00004623-199702000-00001. [DOI] [PubMed] [Google Scholar]
- 33.Siegmeth A, Duncan CP, Masri BA, Kim WY, Garbuz DS. Modular tantalum augments for acetabular defects in revision hip arthroplasty. Clin Orthop Relat Res. 2009;467:199–205. doi: 10.1007/s11999-008-0549-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Slooff TJ, Buma P, Schreurs BW, Schimmel JW, Huiskes R, Gardeniers J. Acetabular and femoral reconstruction with impacted graft and cement. Clin Orthop Relat Res. 1996;324:108–115. doi: 10.1097/00003086-199603000-00013. [DOI] [PubMed] [Google Scholar]
- 35.Sporer SM, Paprosky WG. The use of a trabecular metal acetabular component and trabecular metal augment for severe acetabular defects. J Arthroplasty. 2006;21:83–86. doi: 10.1016/j.arth.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 36.Sporer SM, Paprosky WG. Acetabular revision using a trabecular metal acetabular component for severe acetabular bone loss associated with a pelvic discontinuity. J Arthroplasty. 2006;21:87–90. doi: 10.1016/j.arth.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 37.Templeton JE, Callaghan J, Goetz D, Sullivan PM, Johnston R. Revision of a cemented acetabular component to a cementless acetabular component. A ten to fourteen-year follow-up study. J Bone Joint Surg Am. 2001;83:1706–1711. doi: 10.2106/00004623-200111000-00014. [DOI] [PubMed] [Google Scholar]
- 38.Utah Department of Health. Interpreting the SF-12. Salt Lake City, UT, USA: Utah Department of Health; 2004:1–17. Available at: http://www.health.utah.gov/opha/publications/2001hss/sf12/SF12_Interpreting.pdf. Accessed September 16, 2013.
- 39.Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 40.Whaley AL, Berry DJ, Harmsen WS. Extra-large uncemented hemispherical acetabular components for revision total hip arthroplasty. J Bone Joint Surg Am. 2001;83:1352–1357. doi: 10.2106/00004623-200109000-00010. [DOI] [PubMed] [Google Scholar]
- 41.Williams DH, Greidanus NV, Masri BA, Duncan CP, Garbuz DS. Predictors of participation in sports after hip and knee arthroplasty. Clin Orthop Relat Res. 2011;470:555–561. doi: 10.1007/s11999-011-2198-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Woodgate IG, Saleh KJ, Jaroszynski G, Agnidis Z, Woodgate MM, Gross AE. Minor column structural acetabular allografts in revision hip arthroplasty. Clin Orthop Relat Res. 2000;371:75–85. doi: 10.1097/00003086-200002000-00009. [DOI] [PubMed] [Google Scholar]