Abstract
Background
Although the introduction of ultraporous metals in the forms of acetabular components and augments has increased the orthopaedic surgeon’s ability to reconstruct severely compromised acetabuli, there remain some that cannot be managed readily using cups, augments, or cages. In such situations, allograft-prosthetic composites or custom acetabular components may be called for. However, few studies have reported on the results of these components.
Questions/purposes
The purposes of this study were to determine the (1) frequency of repeat revision, (2) complications and radiographic findings, and (3) Harris hip scores in patients who underwent complex acetabular revision surgery with custom acetabular components.
Methods
Between August 2003 and February 2012, 26 patients (28 hips) have undergone acetabular reconstruction with custom triflange components. During this time, the general indications for using these implants included (1) failed prior salvage reconstruction with cage or porous metal construct augments, (2) large contained defects with possible discontinuity, (3) known pelvic discontinuity, and (4) complex multiply surgically treated hips with insufficient bone stock to reconstruct using other means. This approach was used in a cohort of patients with Paprosky Type 3B acetabular defects, which represented 3% (30 of 955) of the acetabular revisions we performed during the study period. Minimum followup was 2 years (mean, 57 months; range, 28–108 months). Seven patients (eight hips) died during the study period, and three (11%) of these patients (four hips; 14%) were lost to followup before 2 years, leaving 23 patients (24 hips) with minimum 2-year followup. Sixteen patients were women. The mean age of the patients was 67 years (range, 47–85 years) and mean BMI was 28 kg/m2 (range, 23–39 kg/m2). Revisions and complications were identified by chart review; hip scores were registered in our institution’s longitudinal database. Pre- and postoperative radiographs were analyzed by the patient’s surgeon to determine whether migration, fracture of fixation screws, or continued bone loss had occurred.
Results
There have been four subsequent surgical interventions: two failures secondary to sepsis, and one stem revision and one open reduction internal fixation for periprosthetic femoral fracture. There were two minor complications managed nonoperatively, but all of the components were noted to be well-fixed with no obvious migration or loosening observed on the most recent radiographs. Harris hip scores improved from a mean of 42 (SD, ± 16) before surgery to 65 (SD, ± 18) at latest followup (p < 0.001).
Conclusions
Custom acetabular triflange components represent yet another tool in the reconstructive surgeon’s armamentarium. These devices can be helpful in situations of catastrophic bone loss.
Level of Evidence
Level IV, therapeutic study.
Introduction
Revision THA resulting from massive acetabular defects remains a major challenge in joint arthroplasty. Numerous treatment options have been described for massive acetabular defects with variable results. Other methods for the treatment of such defects include bulk structural allograft with or without plating [11, 17, 20, 21, 23], standard acetabular components relocalized to a high hip center [9], oblong acetabular components [4, 5, 24], noncustom cup-cage constructs [1–3, 11, 14, 17, 19], and porous-coated or ultraporous metal jumbo acetabular components with or without porous metal augments [1, 8, 15, 17, 22, 26]. Porous metal components and augments have greatly expanded the reconstructive surgeon’s armamentarium when confronting severe bone loss, allowing for excellent initial fixation and the potential for biologic ingrowth.
Although the introduction of ultraporous metals in the forms of acetabular components and augments has substantially improved the orthopaedic surgeon’s ability to reconstruct severely compromised acetabuli, there remain some revision THAs that are beyond the scope of cups, augments, and cages. In situations involving catastrophic bone loss, allograft-prosthetic composites or custom acetabular components may be considered. Custom components offer the potential advantages of immediate, rigid fixation with a superior fit individualized to each patient. These custom triflange components require a preoperative CT scan with three-dimensional (3-D) reconstruction using rapid prototyping technology, which has evolved substantially during the past decade. The surgeon can fine-tune exact component positioning, determine location and length of screws, modify the fixation surface with, for example, the addition of hydroxyapatite, and dictate which screws will be locked to enhance fixation. Prior studies looking at custom triflange components for use in patients with major acetabular defects have reported results comparable to other methods used to treat major acetabular deficiencies [6, 7, 12, 13, 27] and pelvic discontinuity [6, 7, 10, 25]. However, numerous articles regarding custom triflange components have reported procedures performed before advances in the rapid prototyping technology used to create the custom implants [6, 10, 12, 13, 25, 27].
The purposes of the current study were to determine the (1) frequency of repeat revision, (2) complications and radiographic findings, and (3) Harris hip scores in patients who underwent complex acetabular revision surgery with custom acetabular components.
Patients and Methods
We designed a case series study to investigate the results of a cohort of patients with a Paprosky Type 3B acetabular defect [18] who underwent revision hip arthroplasty at our center. In general, among patients with Paprosky Type 3B defects, the indications for use of custom acetabular components were (1) failed prior salvage reconstruction with cage or porous metal construct augments, (2) large contained defects with possible discontinuity, (3) known discontinuity, and (4) complex multiply surgically treated hips with insufficient bone stock. Other patients with Paprosky Type 3B defects were treated with porous metal cups (plus or minus augmentation) or cage constructs with impaction grafting. Between August 2003 and February 2012, the two senior authors (AVL, KRB) reconstructed 28 hips in 26 patients using a custom triflange acetabular component. Three patients (four hips) were lost to followup before 2 years, leaving 23 patients (24 hips) for analysis. Seven patients were men, 16 were women, and one of the female patients underwent staged bilateral revision hip surgery with custom triflange components and had both hips included in the study. The mean age of the patients at the time of surgery was 67 years (range, 47–85 years) and mean BMI was 28 kg/m2 (range, 23–39 kg/m2) (Table 1). Indications for surgery included component migration (n = 17), osteolysis (n = 3), prior sepsis requiring primary component removal (n = 2), periprosthetic acetabular fracture (n = 1), and dislocation (n = 1). Seven patients (eight hips) died during the study period at a mean of 3 years (range, 1–6 years) postoperatively, all unrelated to the index arthroplasty. Of these, three patients (four hips) were lost to followup before 2 years and therefore were not included for review. The minimum followup for all 23 patients (24 hips) was 2 years (mean, 57 months; range, 28–108 months). Complete data sets including pre- and postoperative radiographs and Harris hip scores were available for all 23 patients (24 hips) with minimum 2-year followup.
Table 1.
Patient demographics and perioperative characteristics
| Variable | All hips |
|---|---|
| Number of hips/patients | 24/23 |
| Sex | |
| Male (%) | 7 (29) |
| Female (%) | 17 (71) |
| Age (years)* | 67 (47–85) |
| Body mass index (kg/m2)* | 28 (23–39) |
| Primary diagnosis | |
| Component migration (%) | 17 (71) |
| Osteolysis (%) | 3 (13) |
| Prior sepsis (%) | 2 (8) |
| Periprosthetic acetabular fracture (%) | 1 (4) |
| Dislocation (%) | 1 (4) |
| Operative side | |
| Right (%) | 14 (58) |
| Left (%) | 10 (42) |
| Constrained liner (%) | 16 (67) |
| Operative time (minutes)* | 178 (98–350) |
| Estimated blood loss (mL)* | 696 (150–1400) |
| Cup diameter (mm)† | 58 (54–66) |
| Head diameter (mm)† | 36 (32–44) |
* Data presented as means with ranges; †data presented as median with ranges.
In the Paprosky Type 3B hips included in this study, bone loss was so severe that alternative modalities were thought to have a high risk of failure because of insufficient bone stock. All acetabular prostheses were RingLoc® Triflange Acetabular Components (Biomet Inc, Warsaw, IN, USA). The triflange acetabular component features a titanium construct with PPS® Porous Plasma Spray-coated bone-implant interface (Biomet Inc) and the option of a hydroxyapatite coating, which was used in all hips. We opted for this coating as an adjunct with the goal that it might enhance fixation. The triflange design allows for intimate contact between the iliac, ischial, and pubic flanges of the prosthesis and the host bone. All devices have been approved by the FDA and were used as labeled.
Preoperatively, design of the custom prosthesis began with a thin-cut CT scan of the patient’s pelvis. The raw data generated from the CT scan then was sent to the implant manufacturer, where a 3-D reconstruction of the CT image was created (Fig. 1). Computer-aided design was used to create a digital implant proposal based on the 3-D reconstruction of the patient’s hemipelvis, and a physical one-to-one replication of the involved hemipelvis was created using rapid prototyping technology (Fig. 2A). From the CT reconstruction of the hemipelvis, a design was fabricated on the computer and forwarded to the rapid prototyping machine for production of the model custom acetabular component (Fig. 2B). Component flanges were designed with optimal geometry and orientation to provide an intimate fit against the host bone and bridge existing bone defects to facilitate initial fixation. The hip center and cup abduction and anteversion angles were determined based on pelvic landmarks and anatomic planes [6]. Many patient-specific considerations were taken into account while designing the prototype, including leg length discrepancy, cup size, and retention of an existing femoral component. The model hemipelvis and prototype implant were sent to the surgeon for review. At that time, the surgeon could make adjustments to component positioning and choose the location, number, length, and locking nature of the screws. Once the implant design had been finalized, the prototype was digitized and input in computer-controlled machining centers, which milled the final implant out of titanium. Porous and hydroxyapatite coatings, if chosen, were applied to the bone-implant interfaces to facilitate osteointegration.
Fig. 1.
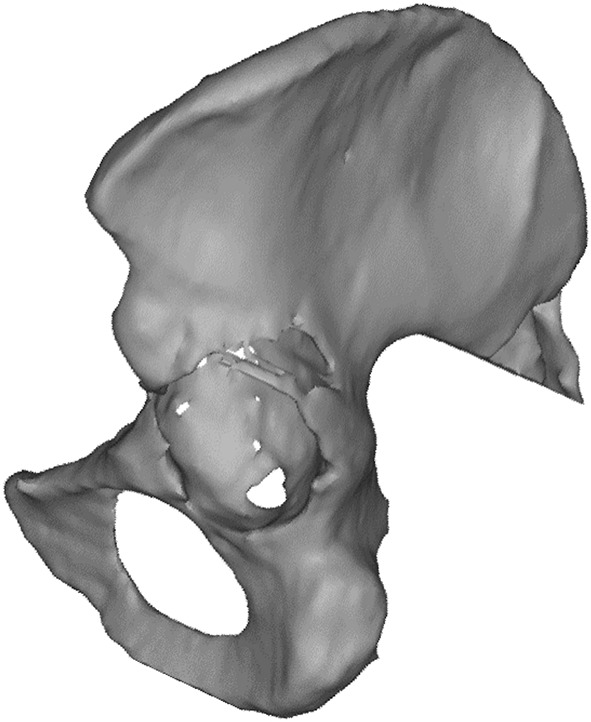
A three-dimensional reconstruction of a hemipelvis created from a raw CT image is shown.
Fig. 2A–B.

(A) A one-to-one replication of the hemipelvis was created using rapid prototyping technology. (B) The custom acetabular component developed using the model hemipelvis is shown. This component is shown postoperatively in Fig. 3.
Perioperatively, patients were placed in a lateral decubitus position and an extended direct lateral approach was used in all hips. The acetabulum was exposed under direct observation and dissection began along the ilium, exposing the wing of the ilium. The dissection was carried along anteriorly, exposing the anterior acetabular bone, pubis, then ultimately the ischium and some of the posterior wall, which allowed for identification of landmarks. After removal of failed components, the trial triflange component was used and bone surfaces were prepared for final placement. The final triflange component then was inserted and seated with proper fixation and positioning. Screws were placed in the ilium, pubis, and ischium and locking screws in the dome (Fig. 3). In some hips, allograft was used to supplement massive acetabular defects. In one case, the custom implant was unable to be inserted because of a deformity not present on the initial CT scan and a cage construct was used with bulk allograft (which later failed).
Fig. 3.

An immediate postoperative AP radiograph shows satisfactory position and alignment of the components.
Harris hip scores were prospectively collected at the preoperative visit and at the most recent followup and were available for all 23 patients. Postoperatively, patients followed the standard of care protocol for patients undergoing hip arthroplasty at our institution. Postoperative Harris hip scores collected at routine clinical followups were obtained between March 2006 and June 2014. Additionally, patients were contacted by telephone to determine whether there were any revisions or complications since the last followup. Radiographs were available for all patients, and they were analyzed by the patient’s surgeon (AVL, KRB) to determine whether migration, fracture of fixation screws, or continued bone loss had occurred. The hallmark of failure of ingrowth was obvious migration of the component on serial radiographs.
Descriptive statistics were used to present frequency and percentage for categorical data and means and ranges for continuous data.
Results
Of the 24 hips in this study, there have been four subsequent surgical interventions (Table 2). One patient had a deep infection develop resulting in removal of the triflange component at 22 months postoperatively. This patient underwent reimplantation of a second custom triflange component 28 months postoperatively, sustained a periprosthetic pelvic fracture resulting in a cup revision 2 years after reimplantation, and subsequently underwent a Girdlestone pseudarthrosis 5 years after the initial triflange component was implanted. A second patient had an infection develop and underwent removal of the triflange component 14 months after surgery. This patient had a second triflange component reimplanted 19 months postoperatively, underwent two liner and stem revisions for dislocation 1 and 2 years after reimplantation, and had a disarticulation performed at an outside facility approximately 7 years after the initial triflange component was implanted. Additionally, two periprosthetic femoral fractures resulted in revision and in both hips, the custom triflange acetabular component was retained.
Table 2.
Custom triflange component outcomes
| Variable | All hips (n = 24) |
|---|---|
| Preoperative Harris hip score* | 42 (21–78) |
| Postoperative Harris hip score* | 65 (31–93) |
| Length of followup (months)* | 57 (28–108) |
| Revisions (%) | 4 (17) |
| Infection (%) | 2 (8) |
| Periprosthetic fracture (%) | 2 (8) |
| Time to revision (months)* | 24 (14–31) |
* Data presented as means with ranges.
Additionally, there were two minor complications. One patient had pain related to sciatica 8 years after surgery. Another patient had trochanteric bursitis 9 years after revision surgery with implantation of a custom triflange component. None of the patients exhibited migration or loosening of the components, as per radiographic review of serial postoperative radiographs for component migration. Of the seven patients (eight hips) who died during the study period, five patients (six hips) had no revisions or complications at last followup. There were no dislocations in our series of patients. Of the 20 study hips that were not revised, all 20 had well-fixed components on the most recent radiographic review and 18 had no complications at last followup.
Mean Harris hip scores for the 23 patients (24 hips) in this study improved from 42 preoperatively to 65 (p < 0.001) with a mean pain component score of 36 postoperatively (range, 10–44, with 44 representing no pain) at most recent followup.
Discussion
The introduction of ultraporous metals in acetabular components and augments has substantially improved the ability to reconstruct severely compromised acetabuli. However, there are some complex revisions that include massive acetabular defects that are not readily treated using cups, augments, and cages. In such catastrophic situations, allograft-prosthetic composites or custom acetabular components may be considered. Custom components are created based on preoperative CT scans with 3-D reconstruction using rapid prototyping technology, which has evolved substantially during the past decade. Potential advantages of these components include the ability to fine-tune exact component positioning and fixation and provide an individualized fit to each patient. However, prior studies of custom triflange components have reported on revisions performed more than a decade ago [6, 10, 12, 13, 25, 27]. Because of improvements in the 3-D reconstruction technology, we wanted to determine the (1) frequency of repeat revision, (2) complications and radiographic findings, and (3) Harris hip scores in patients who underwent complex acetabular revision surgery with custom acetabular components.
The first limitation of our study is that it was designed retrospectively and therefore may be subject to selection bias. However, we used only custom triflange components in patients having an acetabular defect classified as Paprosky Type 3B [18] to minimize preoperative differences. Furthermore, the total number of hips with a Paprosky Type 3B defect treated with an alternative approach during the study period is unknown, as we do not routinely grade and document defect classification preoperatively. Another limitation resulting from the retrospective nature is that seven patients (eight hips) died before data were collected for this study, and three of those patients (four hips) had not been seen for a 2-year clinical followup. Only one of the seven patients died before reaching 2 years postoperatively, and we know that two of the patients had revision surgery before death. The other five patients (six hips) had no known complications or revision surgeries at the time of last followup. Twenty-six patients (28 hips) underwent acetabular reconstruction with custom triflange components during the study period; three patients died and were lost to followup before 2 years. Complete data sets were available for the 23 patients (24 hips) with minimum 2-year followup. Preoperative medical clearance was identical to that of other patients having revision surgery and this high death rate may represent the associated morbidity with these catastrophic failures. The third limitation is that it can be difficult to be sure whether these components are well-fixed, as most of the interface surface is obscured on radiographs. We hoped to minimize this concern through consistency with positioning during surgery by ensuring that the flanges of the custom implant were in intimate contact with the bone, and by reviewing serial postoperative radiographs for obvious migration of the component.
The revision rate of triflange components in the current study (8%) was in line with revision rates reported by Wind et al. [27] (11%) and Holt and Dennis [12] (12%) for patients with Paprosky Type 3B acetabular defects (Table 3). Joshi et al. [13] similarly reported a 7% component revision rate for patients with American Academy of Orthopaedic Surgeons (AAOS) Type III acetabular defects, whereas two other studies reported no failures of triflange components in patients with AAOS Types III/IV defects [6, 7]. In the current study, the overall revision rate for any reason (17%) was lower than in studies by DeBoer et al. [10] (30%) and Taunton et al. [25] (35%), both of which treated patients with pelvic discontinuity. It is possible the shorter followup period of our study (mean, 57 months) may have influenced the lower complication rate in our study, as compared with the studies by DeBoer et al. [10] (mean followup, 123 months) and Taunton et al. [25] (mean followup, 76 months). In the current study and the study by DeBoer et al. [10], there were no failures related to the custom triflange component and implant failure was reported in only 5% of the hips in the study by Taunton et al. [25]. In a study by Nieminen et al. [16], evaluating various treatment methods of complex acetabular defects, custom-made triflange cups were included as a modern option for treatment of acetabular bone defects. However, they reported that complete osseointegration is mandatory for success [16].
Table 3.
Studies of custom triflange components in revision hip arthroplasty
| Study (country) | Number of patients (hips) | Males:females | Mean age of patients (years) | Type of acetabular defect | Observation time | Results |
|---|---|---|---|---|---|---|
| Christie et al. (US) [6] | 76 (78) | 20:56 | 59 | AAOS Types III/IV | Surgeries 1992–1998; mean followup 53 months | 6 reoperations for recurrent dislocation (8%); no removal of triflange components; preoperative HHS: 33; postoperative HHS: 82 |
| Colen et al. (Belgium) [7] | 6 (6) | 3:3 | 69 | AAOS Types III/IV | Surgeries 2007–2011; mean followup 28 months | 0 revisions; postoperative HHS: 61 |
| DeBoer et al. (US) [10] | 18 (20) | 3:15 | 56 | Pelvic discontinuity | Surgeries 1992–1998; mean followup 123 months | 6 revisions (30%); no removal of triflange components; preoperative HHS: 41; postoperative HHS: 80 |
| Holt and Dennis (US) [12] | 26 (26) | 8:18 | 69 | Paprosky Type 3B; AAOS Types III/IV | Mean followup 54 months | 3 failures of triflange components (12%); preoperative HHS: 39; postoperative HHS: 78 |
| Joshi et al. (US) [13] | 27 (27) | 9:18 | 68 | AAOS Type III | Surgeries 1993–1996; mean followup 58 months | 2 revisions with removal of triflange components (7%) |
| Taunton et al. (US) [25] | 57 (57) | 6:51 | 61 | Pelvic discontinuity | Surgeries 1992–2008; mean followup 76 months | 20 revisions for any reason (35%); 3 failures of triflange components (5%); postoperative HHS: 75 |
| Wind et al. (US) [27] | 19 (19) | 7:12 | 58 | Paprosky Types 3A/3B; AAOS Types III/IV | Surgeries 2001–2005; mean followup 31 months | 2 revisions for failure of triflange components (11%); preoperative HHS: 38; postoperative HHS: 63 |
| Current study (US) | 23 (24) | 7:16 | 67 | Paprosky Type 3B | Surgeries 2003–2012; mean followup 57 months | 4 revisions for any reason (17%); 2 failures of triflange components resulting from infection (8%); preoperative HHS: 42; postoperative HHS: 65 |
AAOS = American Academy of Orthopaedic Surgeons; HHS = Harris hip score.
Dislocation was the most frequent complication not requiring revision reported in comparable studies, with rates ranging from 4% to 30% [6, 10, 12, 13, 25, 27]. Although this did not occur in any of our study hips, one of the hips revised for deep infection was reimplanted with a second triflange component which subsequently underwent two liner and stem revisions to treat prosthetic dislocations. Another complication absent in our study was nerve injury, which was a minor complication commonly reported with rates ranging from 4% to 8% [6, 12, 13, 25, 27]. Several studies we reviewed, like our study, reported no signs of migration on followup radiographs, although a few studies reported migration on 11% to 14% of hips [12, 25, 27]. The increase between mean pre- and postoperative Harris hip scores in our patients was 23 points, which was similar to the mean 25 points reported by Wind et al. [27] but lower than the increases reported by Christie et al. [6], DeBoer et al. [10], and Holt and Dennis [12].
Accurate placement of the custom triflange component requires substantial exposure of the ilium, increasing the risk of nerve and vascular injury [16]. High importance should be placed on patient selection and surgical technique when using the custom triflange component for reconstruction of massive acetabular bone defects. We chose to limit our use of custom triflange components to patients having a Paprosky Type 3B [18] acetabular defect that was unable to be treated using cups, augments, or cages. Previous studies of custom triflange components had results comparable to other methods used to treat massive acetabular deficiencies [6, 7, 10, 12, 25, 27]. Our current study of custom triflange components created using modern rapid prototyping technology showed results similar to those of prior studies of custom triflange components [6, 10, 12, 13, 25, 27]. The cost of the component was comparable to other extensive revision options such as trabecular metal cup-cage constructs, but pricing is based on local discounts and influenced by volume, industry relationships, and other factors. New developments in implants and materials have increased the reconstructive surgeon’s armamentarium when dealing with severely compromised acetabuli. Cups, cages, and acetabular augments have been used in increasingly complex primary and revision arthroplasties. However, despite these advances, certain acetabular defects remain that are beyond the scope of these reconstructive options. Custom triflanged acetabular components may be effective options in such hips.
Footnotes
The institution of one or more of the authors has received funding from Biomet Inc (Warsaw, IN, USA) (KRB, AVL), Kinamed Inc (Camarillo, CA, USA) (AVL), Pacira Pharmaceuticals Inc (Parsippany, NJ, USA) (AVL), and Stryker Orthopaedics (Mahwah, NJ, USA) (KRB, AVL). One of the authors certifies that he (AVL) has or may receive payments or benefits, during the study period, an amount of more than USD 1,000,001 from Biomet Inc, an amount of USD 10,000 to 100,000 from Innomed, Inc (Savannah, GA, USA), and an amount of less than USD 10,000 from Pacira Pharmaceuticals Inc. One of the authors certifies that he (KRB) has or may receive payments or benefits, during the study period, an amount of more than USD 1,000,001 from Biomet Inc.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Joint Implant Surgeons, Inc (New Albany, OH, USA).
References
- 1.Ballester Alfaro JJ, Sueiro Fernandez J. Trabecular Metal buttress augment and the Trabecular Metal cup-cage construct in revision hip arthroplasty for severe acetabular bone loss and pelvic discontinuity. Hip Int. 2010;20(suppl 7):S119–S127. doi: 10.5301/HIP.2010.5297. [DOI] [PubMed] [Google Scholar]
- 2.Berry DJ, Lewallen DG, Hanssen AD, Cabanela ME. Pelvic discontinuity in revision total hip arthroplasty. J Bone Joint Surg Am. 1999;81:1692–1702. doi: 10.2106/00004623-199912000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Berry DJ, Muller ME. Revision arthroplasty using an anti-protrusio cage for massive acetabular bone deficiency. J Bone Joint Surg Br. 1992;74:711–715. doi: 10.1302/0301-620X.74B5.1527119. [DOI] [PubMed] [Google Scholar]
- 4.Berry DJ, Sutherland CJ, Trousdale RT, Colwell CW, Jr, Chandler HP, Ayres D, Yashar AA. Bilobed oblong porous coated acetabular components in revision total hip arthroplasty. Clin Orthop Relat Res. 2000;371:154–160. doi: 10.1097/00003086-200002000-00019. [DOI] [PubMed] [Google Scholar]
- 5.Chen WM, Engh CA, Jr, Hopper RH, Jr, McAuley JP, Engh CA. Acetabular revision with use of a bilobed component inserted without cement in patients who have acetabular bone-stock deficiency. J Bone Joint Surg Am. 2000;82:197–206. doi: 10.2106/00004623-200002000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Christie MJ, Barrington SA, Brinson MF, Ruhling ME, DeBoer DK. Bridging massive acetabular defects with the triflange cup: 2- to 9-year results. Clin Orthop Relat Res. 2001;393:216–227. doi: 10.1097/00003086-200112000-00024. [DOI] [PubMed] [Google Scholar]
- 7.Colen S, Harake R, De Haan J, Mulier M. A modified custom-made triflanged acetabular reconstruction ring (MCTARR) for revision hip arthroplasty with severe acetabular defects. Acta Orthop Belg. 2013;79:71–75. [PubMed] [Google Scholar]
- 8.Davies JH, Laflamme GY, Delisle J, Fernandes J. Trabecular metal used for major bone loss in acetabular hip revision. J Arthroplasty. 2011;26:1245–1250. doi: 10.1016/j.arth.2011.02.022. [DOI] [PubMed] [Google Scholar]
- 9.Dearborn JT, Harris WH. High placement of an acetabular component inserted without cement in a revision total hip arthroplasty: results after a mean of ten years. J Bone Joint Surg Am. 1999;81:469–480. doi: 10.2106/00004623-199904000-00004. [DOI] [PubMed] [Google Scholar]
- 10.DeBoer DK, Christie MJ, Brinson MF, Morrison JC. Revision total hip arthroplasty for pelvic discontinuity. J Bone Joint Surg Am. 2007;89:835–840. doi: 10.2106/JBJS.F.00313. [DOI] [PubMed] [Google Scholar]
- 11.Gross AE. Revision arthroplasty of the acetabulum with restoration of bone stock. Clin Orthop Relat Res. 1999;369:198–207. doi: 10.1097/00003086-199912000-00021. [DOI] [PubMed] [Google Scholar]
- 12.Holt GE, Dennis DA. Use of custom triflanged acetabular components in revision total hip arthroplasty. Clin Orthop Relat Res. 2004;429:209–214. doi: 10.1097/01.blo.0000150252.19780.74. [DOI] [PubMed] [Google Scholar]
- 13.Joshi AB, Lee J, Christensen C. Results for a custom acetabular component for acetabular deficiency. J Arthroplasty. 2002;17:643–648. doi: 10.1054/arth.2002.32106. [DOI] [PubMed] [Google Scholar]
- 14.Kosashvili Y, Backstein D, Safir O, Lakstein D, Gross AE. Acetabular revision using an anti-protrusion (ilio-ischial) cage and trabecular metal acetabular component for severe acetabular bone loss associated with pelvic discontinuity. J Bone Joint Surg Br. 2009;91:870–876. doi: 10.1302/0301-620X.91B7.22181. [DOI] [PubMed] [Google Scholar]
- 15.Nehme A, Lewallen DG, Hanssen AD. Modular porous metal augments for treatment of severe acetabular bone loss during revision hip arthroplasty. Clin Orthop Relat Res. 2004;429:201–208. doi: 10.1097/01.blo.0000150133.88271.80. [DOI] [PubMed] [Google Scholar]
- 16.Nieminen J, Pakarinen TK, Laitinen M. Orthopaedic reconstruction of complex pelvic bone defects: evaluation of various treatment methods. Scand J Surg. 2013;102:36–41. doi: 10.1177/145749691310200108. [DOI] [PubMed] [Google Scholar]
- 17.Paprosky WG, O’Rourke M, Sporer SM. The treatment of acetabular bone defects with an associated pelvic discontinuity. Clin Orthop Relat Res. 2005;441:216–220. doi: 10.1097/01.blo.0000194311.20901.f9. [DOI] [PubMed] [Google Scholar]
- 18.Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty: a 6-year follow-up evaluation. J Arthroplasty. 1994;9:33–44. doi: 10.1016/0883-5403(94)90135-X. [DOI] [PubMed] [Google Scholar]
- 19.Regis D, Sandri A, Bonetti I, Bortolami O, Bartolozzi P. A minimum of 10-year follow-up of the Burch-Schneider cage and bulk allografts for the revision of pelvic discontinuity. J Arthroplasty. 2012;27(1057–1063):e1. doi: 10.1016/j.arth.2011.11.019. [DOI] [PubMed] [Google Scholar]
- 20.Saleh KJ, Jaroszynski G, Woodgate I, Saleh L, Gross AE. Revision total hip arthroplasty with the use of structural acetabular allograft and reconstruction ring: a case series with a 10-year average follow-up. J Arthroplasty. 2000;15:951–958. doi: 10.1054/arth.2000.9055. [DOI] [PubMed] [Google Scholar]
- 21.Shinar AA, Harris WH. Bulk structural autogenous grafts and allografts for reconstruction of the acetabulum in total hip arthroplasty: sixteen-year-average follow-up. J Bone Joint Surg Am. 1997;79:159–168. doi: 10.2106/00004623-199702000-00001. [DOI] [PubMed] [Google Scholar]
- 22.Sporer SM, Paprosky WG. Acetabular revision using a trabecular metal acetabular component for severe acetabular bone loss associated with a pelvic discontinuity. J Arthroplasty. 2006;21(6 suppl 2):87–90. doi: 10.1016/j.arth.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 23.Stiehl JB, Saluja R, Diener T. Reconstruction of major column defects and pelvic discontinuity in revision total hip arthroplasty. J Arthroplasty. 2000;15:849–857. doi: 10.1054/arth.2000.9320. [DOI] [PubMed] [Google Scholar]
- 24.Sutherland CJ. Early experience with eccentric acetabular components in revision total hip arthroplasty. Am J Orthop (Belle Mead NJ). 1996;25:284–289. [PubMed] [Google Scholar]
- 25.Taunton MJ, Fehring TK, Edwards P, Bernasek T, Holt GE, Christie MJ. Pelvic discontinuity treated with custom triflange component: a reliable option. Clin Orthop Relat Res. 2012;470:428–434. doi: 10.1007/s11999-011-2126-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weeden SH, Schmidt RH. The use of tantalum porous metal implants for Paprosky 3A and 3B defects. J Arthroplasty. 2007;22(6 suppl 2):151–155. doi: 10.1016/j.arth.2007.04.024. [DOI] [PubMed] [Google Scholar]
- 27.Wind MA, Jr, Swank ML, Sorger JI. Short-term results of a custom triflange acetabular component for massive acetabular bone loss in revision THA. Orthopedics. 2013;36:e260–e265. doi: 10.3928/01477447-20130222-11. [DOI] [PubMed] [Google Scholar]


