Abstract
The geographic interface between the need for and the supply of pediatric hospice may be critical in whether children with cancer access care. This study sought to describe the geographic distribution of pediatric hospice need and supply and identify areas lacking pediatric hospice care in Tennessee over a 3 year time period. Using ArcGIS, a series of maps were created. There was a consistent need for care among children with cancer across the state. Most urban areas were supplied by pediatric hospices, except the Knoxville area. Areas within the state were identified where the supply of pediatric hospice care declined, while the need for hospice care was unchanging. This study has important regulatory implications for clinicians practicing in Certificate of Need states such as Tennessee.
Keywords: pediatric, cancer, hospice care, certificate of need, geographic access
Cancer is one of the leading causes of death for children in the United States. In particular, malignant neoplasms are the fourth highest cause of pediatric mortality and represent 8.8% of pediatric deaths.1 Indeed, in many states, such as Tennessee, cancer is actually the leading health-related cause of death among children, with leukemia, central nervous system cancers, and lymphomas the three most commonly diagnosed childhood cancers.2 For many children with cancer, effective disease-targeted interventions exist, but for those who die from cancer-related causes each year hospice may be an important care option.3 Hospice care has been shown to improve symptom management and quality of end-of-life care for children;4–6 and yet, most children with cancer who might benefit from hospice care do not receive these services. It is estimated that as few as 10% of terminally ill children utilize hospice care.7 Although family and clinicians play an important role in children accessing hospice care,8.9 the interface between the children’s need for hospice care and the supply of pediatric hospice care may be critical in determining whether or not children with terminal cancer are able to access hospice services.
Geographic access to pediatric hospice care for children with cancer, however, is not well understood. Only a handful of studies have explored geographic access to adult hospice care, and the findings have not been consistent. In an early study, based on Medicare data from 2000 to 2002, Virnig and colleagues found that 100% of persons in urban areas were served by hospices.10 However, in rural areas adjacent to urban areas, over 9% of persons were unserved, and in rural areas not adjacent to urban areas, almost 24% of persons were not served by hospices. Using 2005 to 2006 Medicare data, Madigan and colleagues reported that 62% to 92% of rural counties did not have hospice providers.11 In contrast, Jenkins and colleagues using data from 2002 to 2005 Alabama cancer decedents found that approximately 66% of Alabama counties contain at least one hospice.12 The median distance between decedent's residence and the hospice providing care was 9.8 miles. The authors concluded that hospice care was generally available for cancer decedents in Alabama. More recently, Carlson and colleagues used 2008 Medicare data to estimate the proportion of the U.S. population living within 30 and 60 minutes driving time of a hospice.13 The researchers showed that 88% of the population lived in a community within 30 minutes and 98% lived in a community within 60 minutes of a hospice. The literature suggests that the recent growth in the hospice industry may have resulted in widespread geographic access to hospice care in the United States.
Although this research suggests that variation in geographic access to hospice care has occured over time, it has not examined the geographic need for hospice services among pediatric decedents, especially those with cancer. Nor has it identified the geographic distribution or supply of pediatric hospice providers. As a result, there is a critical gap in our understanding of whether the need for pediatric hospice care among children with cancer matches the supply of pediatric hospice care. This study sought to fill this gap by using geo-mapping techniques with a unique dataset of hospices and pediatric cancer decedents to visualize the need and supply of pediatric hospice care.
Investigating geographic access to pediatric hospice care represents an alternative approach to understanding under-utilization of hospice care among children. By exploring the geographic distribution of need and supply, this study may stimulate discussion among policy makers about where efforts and resources should be directed to meet the need for pediatric hospice care. The findings of this study or others examining geographic access to pediatric hospice care for children with cancer may inform the development of state- and federal-level policies aimed at ensuring access and delivery of hospice care for children, especially in certificate of need (CON) states were the supply of hospice providers is regulated. Therefore, the purpose of this study was to describe the geographic distribution of pediatric hospice care need and supply and to identify areas lacking pediatric hospice care in Tennessee over a 3-year time period (2009–2011).
Materials and Methods
Data Sources and Sample
This longitudinal descriptive study used multiple data sets. The first data source was the 2009 to 2011 Tennessee Cancer Registry (TCR) from the Tennessee Department of Health. The TCR is a state-wide population cancer surveillance system that collects information on all cancer incidents diagnosed in Tennessee.14 The database includes demographics, diagnostic information, and geocoded addresses. From this data source, we drew a sample of Tennessee children who died with a cancer diagnosis. Children were defined as a person less than18 years of age. Inclusion criteria included patients with a diagnosis of cancer, aged 0–17 years, and who died between January 1, 2009, and December 31, 2011. Children who are residents of another state but died while in Tennessee were excluded, along with duplicate observations. After inclusion and exclusion criteria, the sample of children cancer decedents was 43 in 2009, 35 in 2010, and 41 in 2011.
The second data source was the 2009 to 2011 Joint Annual Report of Hospices (JAR) from the Tennessee Department of Health.15 These files provided administrative, staff, and financial information on hospices, including the counties where care was provided by patient age groups. All hospices in the state were included in the analysis, which included 60 hospices in 2009, 63 hospices in 2010, and 65 hospices in 2011.
The years 2009 to 2011 were used in the study because 2009 was the first year the JAR recorded county-level hospice use by age group (e.g., children 17 and younger) and 2011 was the most current TCR data available. Tennessee was chosen for analysis because cancer is the leading cause of pediatric mortality in Tennessee and because it is a hospice certificate-of-need (CON).2,16 The CON process regulates the number of hospice providers in each county, but not whether care is provided for children. Thus, in Tennessee every county has at least one hospice provider and most counties have multiple hospice providers. However, not all hospices provide care to children.
Measures
Geocoded data was used to create the primary variables of interest: need and supply. The need for pediatric hospice care was operationalized as a geographic coordinate based on the latitude and longitude coordinates of the child's home address. The geocoded addresses of children were used to generate a point location for the children in the county in which they resided. The supply of pediatric hospice care was defined as whether or not a community-based hospice care was provided in a home or facility to children in a given county.
Demographic characteristics of the child were used to describe the children. Age was the age of the child at death. Gender was operationalized as whether the child was male or female. Race/ethnicity was categorized as white, African American, and other (i.e., Asian American, Native American, Hispanic). The cancer type was categorized as central nervous system and brain, bone and soft tissue, leukemia, and other types of cancer (e.g., endocrine, lymphoma, gastro-intestinal, kidney and renal, genital).17 A binary variable was created for whether or not the child had metastasis at diagnosis. The insurance type the child had was defined as no insurance, public insurance, or private insurance.
Characteristics of the hospices were also included. Organization size was categorized as small (<25 patients/day), medium (26–100 patients/day), or large (>100 patients/day). Ownership was operationalized as either for profit or nonprofit/government ownership. Affiliation was defined as freestanding or non-freestanding (i.e., hospital-based, nursing home-based, home health agency-based). Accreditation was defined as whether or not the hospice was accredited by the Joint Commission.
Data Analysis
Univariate statistics were used to describe the children and hospice providers in the study. ArcMap in ArcGIS version10.1 was used to create a series of longitudinal maps showing the spatial relationship between need and supply of pediatric hospice services for each year of the study. Points on the map were used to illustrate the location of the child's residence. In order to maintain the family's anonymity, addresses were coded within a 1-kilometer parameter of the residence. Cloropleth mapping techniques were used to display the counties where pediatric hospice care was supplied. The child's geocoded points were added to the cloropleth maps to identify areas where the need for hospice care matched or did not match the supply of pediatric hospice services. As reference points on the maps, the major metropolitan cities of Tennessee, including Nashville, Memphis, Chattanooga, and Knoxville, were marked. The study was approved by the Institutional Review Board of the University of Tennessee, Knoxville.
Results
Description of Sample
Table 1 summarizes the children with cancer who died in Tennessee from 2009 to 2011. Between 2009 and 2011, there were 119 pediatric cancer deaths recorded in Tennessee. The average age of children who died with a cancer diagnosis was 8 years in 2009, 9 years in 2010, and 8 years in 2011. For all three years, boys (51%, 56%, and 55%, respectively) and Caucasians (58%, 82%, and 67%, respectively) were the most common decedents. Children most frequently had CNS and brain cancer in most years of the study (33%, 26%, and 31%, respectively), without metastasis at diagnosis (72%, 68%, and 79%, respectively). In 2009, more than half (53%) of children had private insurance, while less than half (42%) received insurance through public assistance in 2009, with 5% of children having no insurance at all in that same year. In 2010, the number of children who had private insurance increased slightly to 55%, while those who had insurance by way of public assistance declined to 29%, and those without insurance at all rose dramatically to 15%. By 2011, more than half (52%) still had private insurance, while those with public insurance rose to 43%, and those without insurance decreased to 5%.
Table 1.
Characteristics of Pediatric Cancer Decedents by Year, 2009–2011 (N=119)
| Year (n) | |||
|---|---|---|---|
| 2009 (43) |
2010 (34) |
2011 (42) |
|
| Age | |||
| Continuous 0–17 (mean) | 8.00 | 9.00 | 8.00 |
| Gender | |||
| Female (%) | 48.90 | 44.20 | 45.30 |
| Male (%) | 51.10 | 55.80 | 54.70 |
| Race/Ethnicity | |||
| White (%) | 58.10 | 82.36 | 66.60 |
| African American (%) | 32.60 | 8.82 | 33.40 |
| Other Races/Ethnicity (%) | 9.30 | 8.82 | 0.00 |
| Cancer Type | |||
| CNS/Brain Tumor (%) | 32.55 | 26.40 | 30.90 |
| Bone/Soft Tissue (%) | 20.93 | 20.59 | 16.67 |
| Leukemia (%) | 18.60 | 17.65 | 28.57 |
| Other Cancer Types (%) | 27.92 | 35.36 | 23.86 |
| Metastasis | |||
| No (%) | 72.09 | 67.60 | 78.50 |
| Yes (%) | 27.91 | 32.40 | 21.50 |
| Insurance Type | |||
| No insurance (%) | 4.65 | 15.10 | 4.77 |
| Public insurance (%) | 41.90 | 29.10 | 42.85 |
| Private insurance (%) | 53.45 | 55.80 | 52.38 |
The characteristics of Tennessee hospices from 2009 to 2011 are summarized in Table 2. For all 3 years, all hospice care providers were considered small, i.e. managing 25 or fewer total patients daily. In 2009, 63% of hospice providers were for-profit agencies, although this figure fell slightly in 2010 and 2011 to 60%, with the remaining providers as non-profit or government agencies. Consistently, 68% of the hospices were free standing, and they were generally not accredited by the Joint Commission (70%, 71%, and 66%, respectively).
Table 2.
Characteristics of Hospices by Year, 2009–2011 (N=188)
| Year (n) | |||
|---|---|---|---|
| 2009 (60) |
2010 (63) |
2011 (65) |
|
| Organization Size | |||
| Small <25pt/day (%) | 100.0 | 100.0 | 100.0 |
| Medium 26–100/day (%) | 0.00 | 0.00 | 0.00 |
| Large 101+ (%) | 0.00 | 0.00 | 0.00 |
| Ownership | |||
| For profit (%) | 63.40 | 60.30 | 60.00 |
| Nonprofit/government (%) | 36.60 | 39.60 | 40.00 |
| Affiliation | |||
| Freestanding (%) | 68.40 | 68.30 | 67.70 |
| Non-Freestanding (%) | 31.60 | 31.70 | 32.30 |
| Accreditation: Joint Commission | |||
| No (%) | 70.00 | 71.43 | 66.20 |
| Yes (%) | 30.00 | 28.57 | 33.80 |
Mapping Analysis
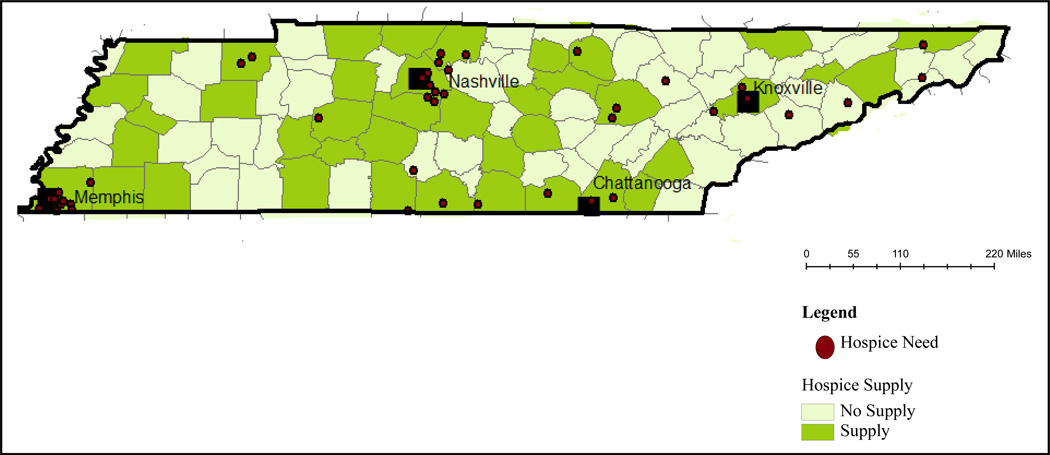
Figure 1 illustrates the geographic need and supply of pediatric hospice care in 2009. The 43 cancer decedents had a need for pediatric hospice care in 21 out of the 95 Tennessee counties. This map suggests that there was geographic variation in need across the state. Areas with the densest concentration of need were found in the counties in and around Memphis, Nashville, Chattanooga, and Knoxville. Pediatric hospice care was supplied in 42% of the counties. It was supplied predominately in the urban areas, with areas east of Memphis and surrounding Knoxville lacking providers. There were five counties where hospice care was needed but not supplied.
Figure 1.
Pediatric Hospice Need and Supply 2009
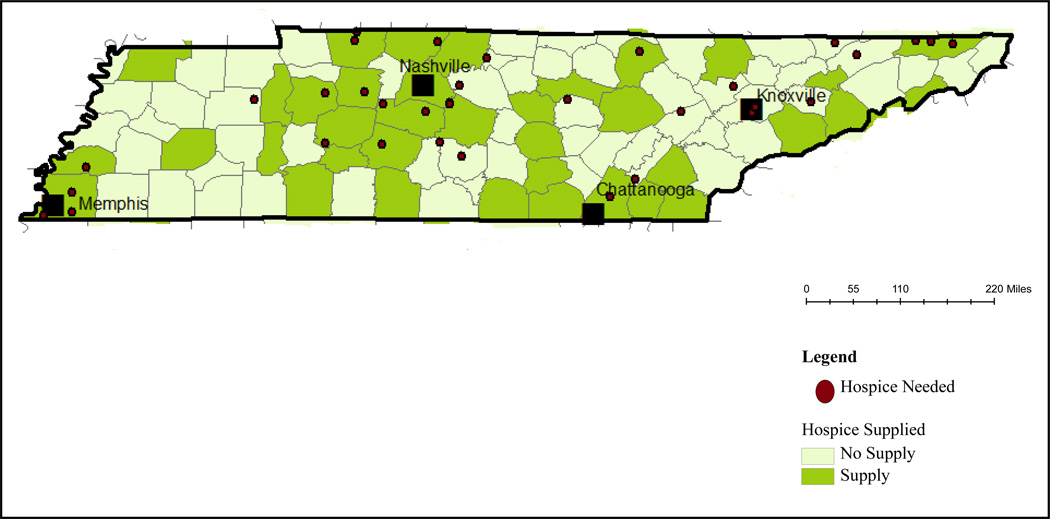
The 2010 need and supply of pediatric hospice care are depicted in Figure 2. The need for hospice care increased to 27 counties that were geographically dispersed in the state. The highest concentration of need was in the Memphis and Knoxville areas. The supply of pediatric hospice care was concentrated in Memphis, Nashville, and Chattanooga and counties in the middle of the state. Hospice care was supplied in 39% of the counties. Knox county (where Knoxville is located) and its surrounding counties were especially void of pediatric hospice providers. By 2010, there were 12 counties where the pediatric hospice need was not met with supply.
Figure 2.
Pediatric Hospice Need and Supply, 2010
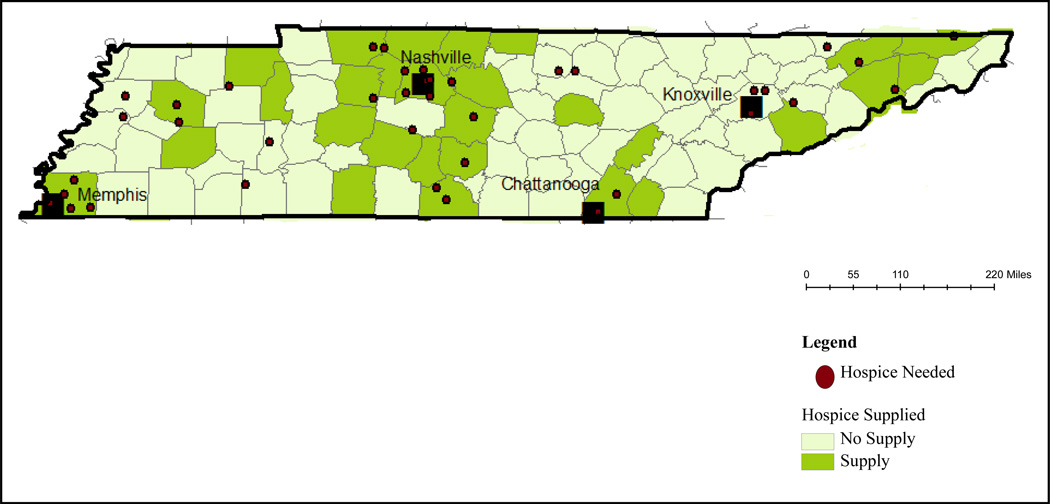
Figure 3 presents the pediatric hospice care need and supply for 2011. Children who died with cancer had a need for hospice care in 25 counties, a slight decline from 2010. The geographic distribution of need was relatively widespread across the state with the density of need in the Memphis, Nashville, and Knoxville areas. By 2011, the number of hospice providers that supplied pediatric care dwindled to 32% of Tennessee counties, with 10 counties showing a need for pediatric hospice care that was not supplied. The supply of pediatric hospice care was predominately in the mid-section of the state around Nashville, whereas the counties surrounding Knoxville generally lacked providers.
Figure 3.
Pediatric Hospice Need and Supply, 2011
Discussion
As one of the first studies to examine the geographic distribution of need and supply of pediatric hospice care over time, this study sought to map and describe geographic variation in the need for hospice care by a group of pediatric cancer decedents, relative to the supply of pediatric hospice care by a set of hospice providers in Tennessee over a 3-year period of time. A measure of need for pediatric hospice care based on cancer mortality was used, along with a measure of supply of pediatric hospice care based on whether hospice care was provided to children in each county. Although the sample of children and hospice providers was relatively homogenous, the study identified critical areas within the state where the supply of pediatric hospice care consistently did not match the need, or where supply declined, while the need for hospice care was unchanging.
The findings demonstrated that there is a consistent need for hospice care for children with a terminal cancer diagnosis that was geographically dispersed across the state of Tennessee. Jenkins and colleagues found similar results in their hospice study of cancer decedents of all ages in Alabama.12 Conversely, we found that the supply of pediatric hospice care declined in the three-year period. In 2009 pediatric hospice care was supplied in 40 counties, which dropped to 30 counties by 2011. This finding, while counterintuitive in an era of explosive hospice industry growth,18 is consistent pediatric hospice research, which found that the percentage of pediatric hospice providers declined over a 7-year period in California.19 The change in geographic supply may be attributable to the small size of hospices in Tennessee. In certain geographic markets, hospices may lack resources to care for children. Studies have shown that small and medium sized hospices often do not have the financial resources and physical assets to provide pediatric care.19 Thus, future research might examine the influence of organization size on geographic supply of pediatric hospice care, or it might identify practical means by which clinicians may address these resource gaps to better serve pediatric patients.
The study also identified areas lacking pediatric hospice care in Tennessee. We observed that, while urban areas were relatively well supplied by pediatric hospice providers, the Knoxville area had a poor supply of providers, especially in 2010 and 2011. In addition, the counties where need and supply were mismatched increased from 5 counties in 2009 to a high of 12 counties in 2010, and finally decreased only slightly to 10 counties in 2011. These findings were generally consistent with those of Virnig et al. and Madigan et al., who found that hospice care clustered around urban areas.10,11 It is possible that areas where supply does not meet the need for pediatric hospice care may be the result of small hospice size. With few staff and resources, a small hospice in an area may have difficulty retaining staff (e.g., registered nurses) with knowledge of pediatric hospice care. Hospice staff who were once experienced with providing care for children may have terminated their employment with the hospice agency, thereby creating a pediatric hospice care void in the community. Given recent concerns about hospice nursing turnover,20 further inquiry is warranted.
There are several limitations in the study. First, the study was focused on Tennessee, which limits generalizability to other states. Although as many as 18 states have hospice CON laws, caution should be used in interpreting results beyond Tennessee.21 Second, the descriptive nature of our analysis prevents any causal relationships from being discussed. Finally, the secondary data used in the study omitted key variables. For example, the Tennessee Cancer Registry, although it reported the number of children who died with a cancer diagnosis each year, did not report whether children used hospice services. Future researchers will need to explore ways of combining data sources such as Medicaid claims data to understand the difference between potential need and realized need.22
Despite the limitations, the findings from this study have significant policy implications for clinicians and policy-makers, especially those in Certificate of Need states. In the regulatory environment of a hospice Certificate of Need, the state establishes criteria for hospices to supply a given area of the state. The findings of the study suggest that the Certificate of Need process at the state-level might include regulatory language on pediatric hospice care as a criteria for ensuring geographic access to pediatric hospice care in the state. Certificate of need states such as Tennessee that do not current ask hospice providers whether they provide care to children or that care be supplied specifically for children, may benefit from establishing provider criteria 16 Thus, through regulatory measures, the supply of pediatric hospice care might be maintained for all children in a given geographical region of a state over time.
In summary, the descriptive mapping analysis showed that in a relatively short period of time the supply of pediatric care generally failed to meet need for care across a state. Although some regions of the state regularly supplied pediatric hospice care for children in need, the supply declined in the Knoxville area, where there was consistent need by children with cancer and their families. Given the regulatory nature of hospice care in many states, the Certificate of Need process—if revised with these results in mind—could aide in assuring a continuous supply of hospice care to meet the care needs of children with cancer at end of life.
Acknowledgement
The authors acknowledge Ms. Beth Schewe for her expert assistance in the preparation of this manuscript.
Funding: This publication was made possible by Grant Number K01NR014490 from the National Institute of Nursing Research and an internal grant from the University of Tennessee, Knoxville - Center for Health Policy & Services Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Nursing Research or National Institutes of Health or the University of Tennessee.
Footnotes
Declaration of Conflict of Interest:
The authors declares no conflicts of interest with respect to the authorship and/or publication of this article.
References
- 1.Kochanek KD, Kirmeyer SE, Martin JA, et al. Annual summary of vital statistics: 2009. Pediatr. 2012;129:338–348. doi: 10.1542/peds.2011-3435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.State of Tennessee, Department of Health. [Accessed October 20, 2011];Cancer in Tennessee: 2003–2007. 2010 Available at: http://health.state.tn.us/TCR/PDFs/TCR_Annual_Report_2003_2007_Rev1010.pdf.
- 3.Institute of Medicine. When children die: improving palliative and end-of-life care for children and their families. Washington: National Academy Press; 2003. [Google Scholar]
- 4.Davies B, Brenner P, Orloff S, et al. Addressing spirituality in pediatric hospice and palliative care. J Palliat Care. 2002;18:59–67. [PubMed] [Google Scholar]
- 5.Dickens DS. Comparing pediatric deaths with and without hospice support. Pediatric Blood Cancer. 2010;54:746–750. doi: 10.1002/pbc.22413. [DOI] [PubMed] [Google Scholar]
- 6.Hendricks-Ferguson V. Physical symptoms of children receiving pediatric hospice care at home during the last week of life. Oncol Nurs Forum. 2008;35:e108–e115. doi: 10.1188/08.onf.e108-e115. [DOI] [PubMed] [Google Scholar]
- 7.Lindley LC, Lyon ME. A profile of children with complex chronic conditions at end of life among Medicaid-beneficiaries: Implications for healthcare reform. J Palliat Med. 2013;16(11):1388–1393. doi: 10.1089/jpm.2013.0099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dabbs D, Butterworth L, Hall E. Tender mercies: increasing access to hospice services for children with life-threatening conditions. Am J Matern Child Nurs. 2007;32:311–319. doi: 10.1097/01.NMC.0000288003.10500.00. [DOI] [PubMed] [Google Scholar]
- 9.Davies B, Sehring SA, Partridge J, et al. Barriers to palliative care for children: perceptions of pediatric health care providers. Pediatrics. 2008;121:282–288. doi: 10.1542/peds.2006-3153. [DOI] [PubMed] [Google Scholar]
- 10.Virnig B, Ma H, Hartman L, et al. Access to home-based hospice care for rural populations: identification of areas lacking service. J Palliat Med. 2006;9:1292–1299. doi: 10.1089/jpm.2006.9.1292. [DOI] [PubMed] [Google Scholar]
- 11.Madigan EA, Wiencek CA, Vander Schrier AL. Patterns of community-based end-of-life care in rural areas of the United States. Policy, Politics, & Nursing Practice. 2009;10:71–81. doi: 10.1177/1527154409333861. [DOI] [PubMed] [Google Scholar]
- 12.Jenkins T, Chapman K, Harshbarger D, et al. Hospice use among cancer decedents in Alabama, 2002–2005. Preventing Chronic Disease. 2009;6:1–8. [PMC free article] [PubMed] [Google Scholar]
- 13.Carlson M, Bradley E, Du Q, et al. Geographic access to hospice in the United States. Journal of Palliative Medicine. 2010;13:1331–1338. doi: 10.1089/jpm.2010.0209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.State of Tennessee, Department of Health. [Accessed March 17, 2014];State of Tennessee comprehensive cancer control plan, 2009–2012. 2013 Available at: https://health.state.tn.us/CCCP/TCCC_Plan.pdf.
- 15. [Accessed April 1, 2012];State of Tennessee, Department of Health. 2009 to 2011 Joint annual report of hospices. Available at http://health.state.tn.us/statistics/jar.htm.
- 16.State of Tennessee, Department of Health. [Accessed January 12, 2014];State health plan: certificate of need standards and criteria for residential hospices services and hospice services. 2012 Available at: tennessee.gov/.../con_standard.../ Hospice%20Services%20Final%20Draft%20for%20SHP[2].pdf.
- 17.National Cancer Institute. [Accessed February 17, 2014];Site Code ICD-O-3 Definition - SEER Data Reporting. 2003 Available at: http://seer.cancer.gov/siterecode/icdo3_d01272003/.
- 18.Thompson JW, Carlson MD, Bradley EH. US hospice industry experienced considerable turbulence from changes in ownership, growth, and shift to for-profit status. Health Affairs. 2012;31(6):1286–1293. doi: 10.1377/hlthaff.2011.1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lindley LC, Mark BA, Lee S-Y, et al. Factors associated with the provision of hospice care for children. J Pain Symptom Manage. 2013;45(4):701–711. doi: 10.1016/j.jpainsymman.2012.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hospice and Palliative Nurses Association. [Accessed February 3, 2014];HPNA position statement: shortage of registered nurses. 2011 Retrieved from https://www.hpna.org/PicVIew.aspx?ID=28.
- 21.National Conference of State Legislatures. [Accessed March 4, 2014];Certificate of need: state health laws and programs. 2013 Retrieved from http://www.ncsl.org/research/health/con-certificate-of-need-state-laws.aspx.
- 22.Feldstein PJ. Health Care Economics. Clifton, NY: Thomson Delmar Learning; 2011. [Google Scholar]