Abstract
Background:
The relation between elevated blood lactate level and mortality and morbidity rates after coronary bypass surgery is a proven subject. One of the factors that seems to affect directly the blood lactate level is the storage duration of packed red blood cells.
Objectives:
This study aimed to evaluate the effect of storage duration of transfused blood on serum lactate during cardiac surgery and up to 24 hours after that in the ICU.
Patients and Methods:
In a cross-sectional study, 228 patients referred to three hospitals of Mashhad University of Medical Sciences for open cardiac surgery, was enrolled using systematic random sampling method. Immediately after accessing arterial line, the first sample of arterial blood gas (ABG) was obtained. For evaluation of lactate levels, the next samples were obtained at the end of surgery and after 24 hours of staying ICU.
Results:
Among 5 factors which affected lactate level during surgery, diabetes and higher ejection fraction (EF) reduced changes of the lactate level. On the other hand, the number of infused blood units, duration of on-pump time, and the mean storage duration of blood units were associated with elevated serum lactate during surgery. A significant relationship was found between blood storage duration and serum lactate levels 24 hours after surgery.
Conclusions:
Comparing the serum lactate level before operation and 24 hours after the operation showed that the number of received blood units had a significant effect on serum lactate. We found no significant effect for blood storage duration; however, the number of given blood units was more significant.
Keywords: Lactates; Blood, Cardiac Surgical Procedures
1. Background
Today’s advances in technology have contributed to the growing number of cardiac coronary surgery. Determining predictive factors for mortality and morbidity is very important in the management of patients with cardiac surgery. Hyperlactatemia accompanied with metabolic acidosis in patients with systemic hypoperfusion and tissue hypoxia is a common event (1). Hyperlactatemia is a well-recognized marker of circulatory failure and significantly associated with mortality.
In cardiac surgery, increased serum lactate levels both during operation and after transferring the patient to the ICU is associated with poor prognosis (2-4). In children with congenital heart diseases underwent cardiac surgery, it has been demonstrated that providing proper oxygenation during cardiopulmonary bypass can reduce the incidence of hyperlactatemia (3).
Lactic acidosis following cardiopulmonary bypass surgery and tachycardia are indicative of low cardiac output syndrome, and hypoxia is usually associated with clinical evidence of insufficient oxygen delivery, which is associated with poor prognosis. Insufficient revascularization in coronary bypass, insufficient myocardial protection, and coagulation disorders are factors that affect hyperlactatemia. A low cardiac output before surgery has been introduced as the most important cause of insufficient oxygenation, and thus increases the serum lactate level (5). Hyperlactatemia is frequently occurred after cardiac surgery. Serum lactate level more than 3 mmol/L is suggested as an indicator of increased mortality risk (6).
To preserve the hematocrit level and proper oxygenation during cardiac surgeries in adults and especially in children, using packed red blood cells (PRBC) is usually considered essential by anesthesiologists and cardiac surgeons. Yet, blood transfusion may negatively affect the outcome of surgery, which was confirmed by Koch et al. study as the sole definitive and reliable factor in increasing morbidity after surgery. It is supposed that each unit of transfused blood greatly increases the risk of postoperative adverse outcome. Blood storage can lead to many alterations in its elements, in particular, an increase in potassium and lactate levels and a decrease in pH (7). Since oxygen is not available in PRBCs and the energy of blood cells is supplied through anaerobic glycolysis, lactate levels increase and glucose levels decrease, which eventually lead to acidosis.
Using fresh stored blood during cardiac surgery can reduce mortality and morbidity. The blood units stored for more than two weeks may considerably increase the postoperative adverse outcomes and decrease short-term and long-term survival (8). Engoren et al. studied effects of transfusion on the mortality rate after cardiac surgery and concluded that transfusion does not affect mortality after isolated cardiac valve surgery but when it is accompanied by coronary bypass surgery, would most probably increase the mortality. Finally, they suggested that blood transfusion effect depends on the disease (9).
2. Objectives
This study aimed to evaluate the effect of storage duration of transfused blood on serum lactate levels during cardiac surgery and up to 24 hours after that in the ICU.
3. Patients and Method
This is a descriptive study (cross-sectional one), including 228 patients who referred for open cardiac surgery to the teaching hospitals of Mashhad University of Medical Sciences. The patients were recruited systematically and based on their entrance to the operating room. The evaluated factors included anesthesia duration, on-pump duration, length of aortic clamping, the number of received blood units during operation and in the ICU, the mean storage duration of blood units, age, history of diabetes, blood pressure, pulmonary diseases, and ejection fraction before operation. All the patients who were candidates for cardiac surgery (patients were ASA class of at least III and even IV) and survived exclusion criteria were included in the study. Exclusion criteria were as follows:
Having hypotension episodes before operation, including systolic blood pressure (SBP) less than 90 mmHg, or mean arterial pressure (MAP) less than 70 mmHg.
Hypotension episodes as SBP < 90 mmHg or MAP < 70 mmHg during first 24 hours in the ICU for more than 15 minutes.
Need for electrical defibrillation more than 4 times during or after the operation for any reason.
Serum lactate level more than 2 mmol/L in the first ABG obtained from the patient.
Renal failure before surgery.
Use of nephrotoxic drugs before surgery.
Patients who develop drop in arterial oxygen saturation for more than 15 minutes during operation or in the first 24 hours in the ICU.
Emergency or combined surgeries.
Patients’ information, including their demographics, date of storage and identification number of blood unit, number of infused blood units, and measured lactate levels in three samples were collected using a checklist. For each patient, an arterial line was placed in the left or right radial artery under local anesthesia with lidocaine 2%. Then, the first ABG sample was taken while the patient had normal respiration in room air, and the lactate level was documented as the baseline lactate level. The next samples of ABG were obtained at the end of surgery, and after 24 hours in the ICU. The data from noninvasive blood pressure monitoring (NIBP), electrocardiogram, pulse oximetry and urine output were also documented in children after anesthesia.
For adult patients, 1 mg lorazepam was administered in early hours of operation day as a premedication and 10 mg intramuscular morphine was administered 1 hour before the operation. If a patient received aspirin or clopidogrel, and it was not discontinued at least one week before the operation, the intramuscular morphine would not be administered. Premedication was performed in children with administrating 3-5 mL promethazine syrup. All the patients received similar anesthetic procedure while maintaining blood pressure and circulation volume within normal ranges.The anesthetic protocol included propofol 1 mg/kg, sufentanil 50-75 µm, midazolam 0.1 mg/kg, and atracurium 0.5 mg/kg. Anesthesia was maintained by infusing 0.04 mg/kg/min atracurium, 1 µg/kg/min midazolam, and 0.5 µg/min sufentanil. At the end of the surgery and before transferring the patients to the ICU, the second ABG sample was obtained.
In the ICU, routine monitoring was performed for tracking stabilization and after 24 hours, the third ABG sample was obtained. It is noteworthy that during surgery and in the ICU, we attempted to maintain normotensive and normovolemic hemodynamic status. Regarding the statistical analysis, the study variables were analyzed using the SPSS 13 with a stepwise multiple linear regression. And the final model was one of the models contained the most significant predictor variables.
4. Results
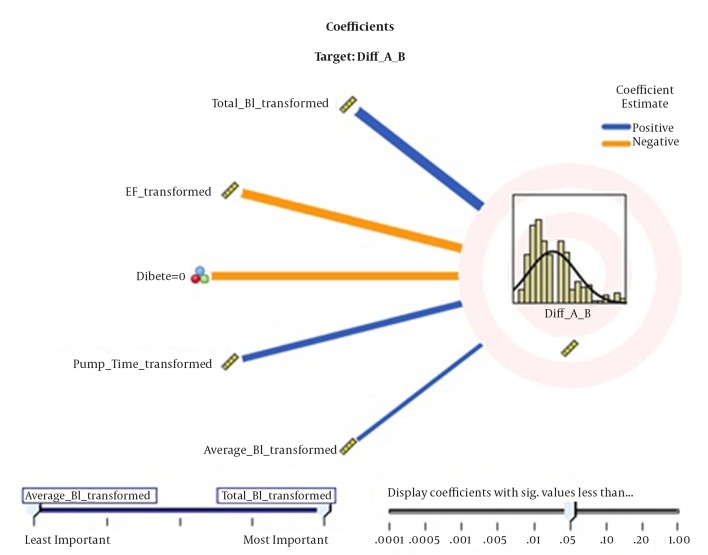
In total, 228 patients (132 [57.89%] male and 96 [42.11%] female) with the mean age of 65.196 ± 11.027 years were included in the study. The results showed that among evaluated variables, the number of transfused blood units, EF before surgery, having diabetes, duration of using pump and storage time of blood respectively, significantly raised postoperative serum lactate compared with pre-operation (Figure 1). The average number of days after blood storage (P = 0.019) and EF value before Surgery (P < 0.001) demonstrated a negative effect on serum lactate, while storage duration of the blood unit (P< 0.001), duration of pump (P< 0.001), and presence of diabetes mellitus (P < 0.001) showed a positive effect on increased serum lactate between pre-operation and post-operative period (Table 1).
Figure 1. Factors affect serum Lactate During Surgery.
Table 1. The Relation Between Different Variables With Serum Lactate Model.
| Coefficients | Std. Error | T-Test | P value | 95% Confidence Interval | Importance | ||
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Duration of Pump, min | 0.025 | 0.004 | 6.818 | < 0.001 | 0.018 | 0.032 | 0.604 |
| Storage unit of blood | 0.631 | 0.076 | 8.258 | < 0.001 | 0.480 | 0.782 | 0.538 |
| EF before Surgery | -0.061 | 0.008 | -7.902 | < 0.001 | -0.077 | -0.046 | 0.504 |
| Diabetic = 0 | 1.630 | 0.222 | 7.339 | < 0.001 | 1.192 | 2.068 | 0.458 |
| Average No. of day after blood storage | -0.025 | 0.009 | 2.778 | 0.019 | -0.043 | -0.007 | 0.175 |
5. Discussion
In this study, we evaluated factors, which affect serum lactate level after cardiac surgery. Our results showed that among 10 evaluated variables, the number of received blood units, EF before operation, having diabetes, pump duration, and average storage time of transfused blood significantly affected postoperative lactate level, respectively.
Toramanet al. study on 776 patients with open cardiac surgery showed that elevated level of serum lactate is associated with poor prognosis.Their results demonstrated that increased aorta cross-clamp duration, duration of cardiopulmonary bypass, and high positive fluid balance at the end of operation are associated with an early rise in postoperative lactate levels. It results in the increase in the need for IABP (intra-aortic balloon pump) support, length of ICU stay, need for red blood cell transfusion, length of hospital stay, and mortality rates (1).
Ranucci et al. study on 500 patients with cardiopulmonary bypass indicated that hyperlactatemia during CPB is mainly due to inadequate oxygen delivery to fulfill the metabolic needs of the patient. The factors like preoperative serum creatinine, active endocarditis, duration of cardiopulmonary bypass, low oxygen delivery during bypass, and high levels of serum glucose were introduced as independent factors inducing hyperlactatemia. They found a direct relation between hyperlactatemia and low oxygen delivery to tissues during surgery which induced low cardiac output syndrome and consequently, increased postoperative morbidity but not mortality (2).
Ranucci performed another study in 2010 on 256 children under 6 years old who underwent open cardiac surgery.All the patients were continuously monitored for serum lactate and central venous oxygen saturation. The results showed that each of these two factors independently increase postoperative morbidity, central venous oxygen saturation less than 86%, and lactate level more than 3 mmol/L with positive predictive value of 89%, which had the highest sensitivity for major morbidity. Ranucci suggested that every factor that improves oxygen delivery to tissues during surgery improves these two factors and therefore, decreases morbidity (3). Our results also showed that decrease in EF and increase in serum lactate are both signs of reduced blood volume and inadequate oxygen delivery to tissues, which are associated with increase in serum lactate, and thus similar to Ranucci studies result (2). He also showed in his study that hyperlactatemia induces postoperative low cardiac output syndrome and therefore, increase morbidity (2). However our results showed that hyperlactatemia could be an outcome of low cardiac output (EF) not its cause. Inoue et al. in his study in Ozaka, Japan evaluated the information of 124 patients with cardiopulmonary bypass. They concluded that pathophysiology of postoperative lactic acidosis is based on inadequate oxygen delivery to the tissues during surgery, also the occurrence of hypotension at the beginning of cardiopulmonary bypass (4), which are similar to our results that showed low EF and increased need to blood transfusion are associated with increase in serum lactate.
Sikora et al. studied the effects of storage duration of infused blood units during cardiac surgery in children and found a linear relation between increasing storage period and increase in serum lactate and K+, they concluded that it is necessary to use recent stored bloods in open cardiac surgery to prevent side effects like hyperkalemia and consequences of hyperlactatemia and low blood pressure (10). Our results regarding direct relation between infused blood storage duration and increase in serum lactate level during surgery are similar to Sikora's results. However, it is different because we found that the only factor with significant effect onserum lactate after 24 hours of surgery is the number of received blood units.
Hyperlactatemia after cardiac surgery is common and a sign of poor prognosis (6). Blood transfusion during operation is accompanied with postoperative adverse outcome (1). However, Engoren showed that transfusion after isolated valvular surgery did not raise serum lactate unless accompanied with coronary bypass, so he considered the transfusion effects on the operation outcome as disease dependent (9). In this study, combined surgeries were not evaluated. Hyperlactatemia during combined surgeries could be related to the longer operation period compared with isolated surgeries. One study reported that infusing blood with storage period longer than 14 days is associated with adverse outcome, including reducing survival in short-term and long-term period (8). Transfusing blood with storage period longer than 7 days is associated with postoperative bleeding risk in critical patients (11).
Storing blood decreases the blood capacity in transferring oxygen to tissues, which is accompanied with an increase in lactate level (12), while blood units with less than three days storage time has proper oxygen delivery. Ranucciet al. showed that storage period of blood which is used in children prime cardiac surgery is an independent risk factor for morbidity after surgery and hyperlactatemia. They recommended use of fresh blood for cardiopulmonary prime pump (3). On the other hand, freshness of transfused blood reduces side effects in patients (13). In Koch et al. study, storage duration of blood was reported as an independent risk factor for increasing morbidity (7). However in another study, such a relation was not observed and attention was paid to long period of cardiopulmonary bypass, and postoperative hyperlactatemia (14). But in Suzette study, post-operative lactate level had correlation with duration of surgery, which is associated with mortality (15).
Our study results showed that the number of received blood units during operation, and storage duration of blood, increase serum lactate after surgery. Regarding lactate changes during first 24 hours after surgery the only factor that had significant relation was the number of received blood units and storage time was not a significant factor.
Regarding the limitations of the study, we did not separate our patients based on the surgery type, which could influence our results, because more complex surgeries may affect the outcome. We also did not evaluate the venues oxygen saturation level, which could be a good index for determining the amount of proper pump flow (which prevents lactate raise).
Comparing the serum lactate level before operation and 24 hours after the operation showed that the only significant factor on serum lactate is the number of received blood units. We found no significant effect for blood storage duration, whereas the number of blood units was influential.
Acknowledgments
We would like to thank the Anesthesia Department of teaching hospitals of Mashhad University of Medical Sciences.
Footnotes
Authors’ Contributions:Mehdi Fathi and Ghasem Soltani: Design of the project and performing the study; Mehdi Fathi and Azra Izanloo: Analysis and interpretation of data as well as writing the manuscript; and Marjan Joud: Acquisition of data and supervision of the study.
References
- 1.Toraman F, Evrenkaya S, Yuce M, Aksoy N, Karabulut H, Bozkulak Y, et al. Lactic acidosis after cardiac surgery is associated with adverse outcome. Heart Surg Forum. 2004;7(2):E155–9. doi: 10.1532/HSF98.20041002. [DOI] [PubMed] [Google Scholar]
- 2.Ranucci M, De Toffol B, Isgro G, Romitti F, Conti D, Vicentini M. Hyperlactatemia during cardiopulmonary bypass: determinants and impact on postoperative outcome. Crit Care. 2006;10(6):R167. doi: 10.1186/cc5113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ranucci M, Isgro G, Carlucci C, De La Torre T, Enginoli S, Frigiola A, et al. Central venous oxygen saturation and blood lactate levels during cardiopulmonary bypass are associated with outcome after pediatric cardiac surgery. Crit Care. 2010;14(4):R149. doi: 10.1186/cc9217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Inoue S, Kuro M, Furuya H. What factors are associated with hyperlactatemia after cardiac surgery characterized by well-maintained oxygen delivery and a normal postoperative course? A retrospective study. Eur J Anaesthesiol. 2001;18(9):576–84. doi: 10.1046/j.1365-2346.2001.00893.x. [DOI] [PubMed] [Google Scholar]
- 5.Ranucci M, Ballotta A, Castelvecchio S, Baryshnikova E, Brozzi S, Boncilli A, et al. Intensive care unit admission parameters improve the accuracy of operative mortality predictive models in cardiac surgery. PLoS One. 2010;5(10) doi: 10.1371/journal.pone.0013551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maillet JM, Le Besnerais P, Cantoni M, Nataf P, Ruffenach A, Lessana A, et al. Frequency, risk factors, and outcome of hyperlactatemia after cardiac surgery. Chest. 2003;123(5):1361–6. doi: 10.1378/chest.123.5.1361. [DOI] [PubMed] [Google Scholar]
- 7.Koch CG, Li L, Duncan AI, Mihaljevic T, Cosgrove DM, Loop FD, et al. Morbidity and mortality risk associated with red blood cell and blood-component transfusion in isolated coronary artery bypass grafting. Crit Care Med. 2006;34(6):1608–16. doi: 10.1097/01.CCM.0000217920.48559.D8. [DOI] [PubMed] [Google Scholar]
- 8.Koch CG, Li L, Sessler DI, Figueroa P, Hoeltge GA, Mihaljevic T, et al. Duration of red-cell storage and complications after cardiac surgery. N Engl J Med. 2008;358(12):1229–39. doi: 10.1056/NEJMoa070403. [DOI] [PubMed] [Google Scholar]
- 9.Engoren MC, Habib RH, Zacharias A, Schwann TA, Riordan CJ, Durham SJ. Effect of blood transfusion on long-term survival after cardiac operation. Ann Thorac Surg. 2002;74(4):1180–6. doi: 10.1016/s0003-4975(02)03766-9. [DOI] [PubMed] [Google Scholar]
- 10.Sikora N, Ozolins V, Smits L, Teivane E, Bergmane I, Lacis A. The metabolic changes in fresh versus old stored blood used in priming of extracorporeal circuit in cardiopulmonary bypass for pediatric patients. Acta Chirurgica Latviensis. 2009;9(1):24–7. [Google Scholar]
- 11.Berezina TL, Zaets SB, Morgan C, Spillert CR, Kamiyama M, Spolarics Z, et al. Influence of storage on red blood cell rheological properties. J Surg Res. 2002;102(1):6–12. doi: 10.1006/jsre.2001.6306. [DOI] [PubMed] [Google Scholar]
- 12.Ayhan B, Yuruk K, Koene S, Sahin A, Ince C, Aypar U. The effects of non-leukoreduced red blood cell transfusions on microcirculation in mixed surgical patients. Transfus Apher Sci. 2013;49(2):212–22. doi: 10.1016/j.transci.2013.01.016. [DOI] [PubMed] [Google Scholar]
- 13.Biffl WL, Moore EE, Offner PJ, Ciesla DJ, Gonzalez RJ, Silliman CC. Plasma from aged stored red blood cells delays neutrophil apoptosis and primes for cytotoxicity: abrogation by poststorage washing but not prestorage leukoreduction. J Trauma. 2001;50(3):426–31. doi: 10.1097/00005373-200103000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Duke T, Butt W, South M, Karl TR. Early markers of major adverse events in children after cardiac operations. J Thorac Cardiovasc Surg. 1997;114(6):1042–52. doi: 10.1016/S0022-5223(97)70018-7. [DOI] [PubMed] [Google Scholar]
- 15.Suzette M, Lourdes SR, Juliet J. Lactate level as an early prognostic marker of major adverse events in pediatric open heart surgery. Phil Heart Center J . 2012;16(2):27–34. [Google Scholar]