Abstract
Recent developments in magnetic resonance (MR) functional quantitative imaging have made it a potentially powerful tool to assess treatment response in radiation therapy. With its abilities to capture functional information on underlying tissue characteristics, MR functional quantitative imaging can be valuable in assessing treatment response and as such to optimize therapeutic outcome. Various MR quantitative imaging techniques, including diffusion weighted imaging, diffusion tensor imaging, MR spectroscopy and dynamic contrast enhanced imaging, have been investigated and found useful for assessment of radiotherapy. However, various aspects including data reproducibility, interpretation of biomarkers, image quality and data analysis impose challenges on applications of MR functional quantitative imaging in radiotherapy assessment. All of these challenging issues shall be addressed to help us understand whether MR functional quantitative imaging is truly beneficial and contributes to future development of radiotherapy. It is evident that individualized therapy is the future direction of patient care. MR functional quantitative imaging might serves as an indispensable tool towards this promising direction.
Keywords: MR functional quantitative imaging, Radiation therapy, Treatment assessment
Core tip: Treatment assessment using magnetic resonance (MR) functional quantitative imaging is the process of using such technique before and/or during and/or after the treatment course to evaluate the changes of functional information. In the area of radiation oncology, MR functional quantitative imaging can be used to quantify radiation-induced functional changes of both radiotherapy targets and critical organs. This article briefly reviews and discusses the basic principles of MR functional quantitative imaging, recent status, critical challenges and future perspectives on radiotherapy assessment. Future clinical trials and research works are needed to further develop MR functional quantitative imaging, towards the goal of individualized radiation therapy.
INTRODUCTION
Recent developments in magnetic resonance imaging (MRI) have substantially improved its performance, making it a potentially powerful tool for not only diagnosis but also treatment planning and assessment. Being an advanced MRI technique, MR functional quantitative imaging offers an approach to extract functional information from MR images. Compared with other functional imaging methods including positron emission tomography (PET) and single photon emission computed tomography on the nuclear medicine basis, MR functional quantitative imaging has a distinguished feature of estimating anatomical and functional information jointly in a single imaging session with potentially improved spatial resolution[1]. In addition, the zero ionizing radiation risk enables MR functional quantitative imaging a good candidate for longitudinal in vivo studies, which require repeated acquisitions within a short period of time. In the past few years, MR functional quantitative imaging has been found valuable in treatment assessment.
Treatment assessment using MR functional quantitative imaging is the process of using such technique before, during and after the treatment course to evaluate the changes of functional information. In the area of radiation oncology, MR functional quantitative imaging can be used to quantify the radiation-induced functional changes of both radiotherapy targets and critical organs. For the optimal therapeutic outcome, the captured early functional change can be utilized to optimize the radiotherapy plan along the treatment course in aspect of fractionation altering, treatment target refinement and dose escalation[2]. Thus, as an key component in the generalized concept of MR image-guided radiotherapy[3,4], MR functional quantitative imaging might serve as an indispensable tool towards individualized radiotherapy[5].
MR FUNCTIONAL QUANTITATIVE IMAGING
Conventional MRI techniques generally provide morphological information of tissue structure, with the superior soft tissue contrast in the anatomical scale. These techniques have demonstrated their effectiveness in the context of oncologic diagnosis and staging. Despite their popularity, the lack of quantitative approach limits conventional MR techniques’ capacity in the derivation of biological processes that occur in the sub-anatomical scale. From radiotherapy perspective in oncologic treatment, it is important to recognize that functional properties, such as tumor cells density, tissue oxygenation, acidosis and microvessel activities, are important factors that influence the radiotherapy outcome via changing cell radiosensitivity[6]. Thus, reliable functional information is in demand to ensure the quality of radiotherapy. Over the past few decades, various MR quantitative methodologies have been developed for functional information assessment: Diffusion weighted imaging (DWI) reflects the cellular density via imaging the random motion of water molecules in the microscopic cellular environment. Under the same concept of capturing water mobility, diffusion tensor imaging (DTI) measures the anisotropic water diffusion process to characterize the tissue’s microstructural organization. MR spectroscopy utilizes its sensitivity to chemical shift and measures the concentration of metabolites of interest. Functional MRI uses blood-oxygen-level-dependent signal variation to quantify local neuronal activity changes. Dynamic contrast-enhanced (DCE) and dynamic susceptibility contrast (DSC) imaging acquires the rapid dynamics of the intravenously administered low molecular-weight contrast agents to depict the process of microvessel kinetics. For easy appreciation, Figures 1-3 show the examples of brain DWI, DTI and DCE data before and after radiotherapy. Previous works have proved MR functional quantitative imaging as a valuable tool to assess radiotherapy response[7-12]. However, various aspects including data reproducibility, interpretation of biomarkers, image quality and novel image analysis methodology all impose challenges on applications of MR functional quantitative imaging in radiotherapy assessment.
Figure 1.
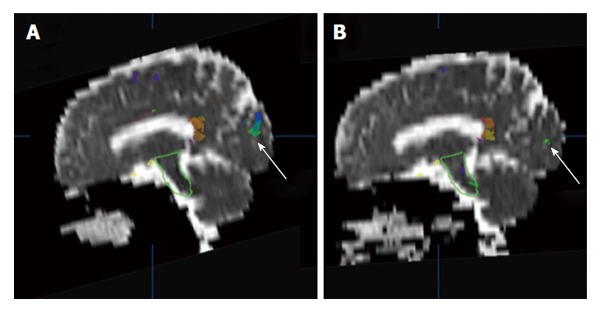
An example of brain apparent diffusion coefficient maps calculated from diffusion weighted images (b = 500 mm2/s) in a sagittal plane before (A) and after (B) radiotherapy. The white arrows indicate a comparison of superimposed colored maps of neural fiber bundles derived from diffusion tensor imaging data (b = 500 mm2/s).
Figure 3.
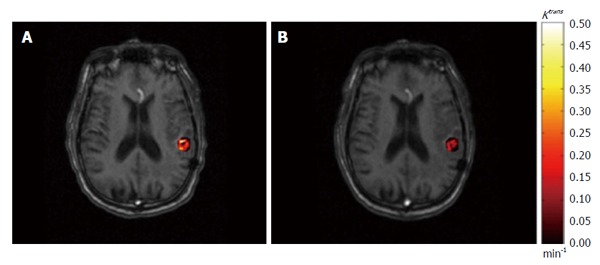
An example of permeability rate constant Ktrans map derived from dynamic contrast-enhanced imaging. The pre-treatment (A) and post-treatment (B) Ktrans results within gross tumor volume are superimposed on axial T1-weighted magnetic resonance images.
Figure 2.
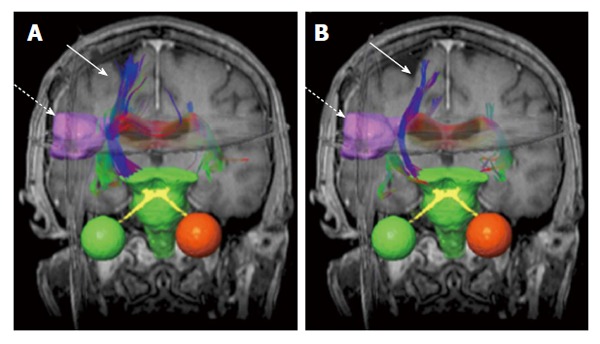
An example of brain neural fiber bundles (solid arrows) derived from diffusion tensor imaging data (b = 500 mm2/s). The pre-treatment (A) and post-treatment (B) results are superimposed on coronal T1-weighted magnetic resonance images. The dashed arrows indicate gross tumor volume (pink boundary).
FUTURE PERSPECTIVES
Reproducibility of quantitative data
As defined by the Toward Quantitative Imaging task force of the Radiological Society of North America: Quantitative imaging is the extraction of quantitative information from clinical images, which can be used to assess change or status of an acute or chronic disease condition relative to normal[13]. In reality, various imaging protocols, scanners and data analysis methods may compromise the reproducibility of data, especially when it comes to multiple center clinical trials. To achieve this goal, standardized acquisition protocols, data analysis and assessment shall be promoted for MR quantitative imaging. As part of these initiatives, the Quantitative Imaging Biomarkers Alliance was established in 2007. The mission of this initiative was to promote and achieve useful and cost-effective standardization across the community on a large scale[13]. All of these efforts are to ensure that quantitative anatomical and physiological information can be accurately and precisely obtained from clinical images and as such can be applied to research and patient care.
Interpretation of biomarker
Though functional biomarkers serve as metrics for functional information evaluation, the physiologic meanings of the selected imaging biomarkers need to be fully examined towards the future clinical application. The interpretation of functional biomarkers quantitative results may depend on the image technical parameters, imaging site, physiologic model selection, and patient’s physiologic variability. For example, as the reported imaging biomarker in DWI, apparent diffusion coefficient (ADC) calculation is affected by the amplitude, duration and spacing of diffusion weighted gradient (jointly expressed as b value) in the pulse sequence. Studies have revealed that different selection of b value had influence on white matter ADC value in brain analysis, and the variation of ADC value showed the potential effect in long-term assessment results[14,15]. In addition, the varying size and location of tumor in different patients with rectal cancer have been shown to have a considerable effect on tumor ADC values[16]. In DCE imaging, the nomenclature of tracer kinetics has been standardized. Nevertheless, when different pharmacokinetics (PK) model are adopted for analysis, the parameters’ may needs to be understood in different ways. Even when same PK model was used, large differences have been reported in the value of contrast agent transfer constant Ktrans in tissue[17,18]. Thus, for the accurate interpretation of functional biomarkers, the correlation of these biomarkers with histological markers shall be validated through rigorous and comprehensive studies. It is crucial to understand how and why these biomarkers can be correlated with clinical outcome.
It is also important to point out that the data consistency between results from MR functional quantitative imaging and those from other imaging modalities may also affect the validity of MR biomarkers’ interpretation. For example, DSC imaging was developed for perfusion study and has been identified by the American Heart Association as a priority for acute stroke treatment[19]. In the brain perfusion quantification, noticeable discrepancies of cerebral blood flow and cerebral blood volume were reported between DSC and gold standard PET measurements[20,21]. Such discrepancies render the quantitative DSC study challenging and elusive. While some studies investigated methods correcting the data discrepancy in DSC studies[22], the issue is not yet completed resolved. The recently emerging PET/MRI modality provides simultaneous MR and PET measurements and might be a valuable tool to help resolve the long standing issue[23]. Future works on PET/MR perfusion research are needed to improve interpretation and quantification of MR perfusion biomarkers.
Image quality improvement
For the radiotherapy assessment purpose, it is important to recognize that image quality of MR functional quantitative imaging may potentially affect the quantitative assessment outcome. Of the factors that contribute to the image quality, spatial resolution is crucial for the precise delineation of target volume. In current state-of-art advanced radiation treatments such as stereotactic radiosurgery and stereotactic body radiotherapy, the target volume is often small while high radiation dose is delivered in a limited number of fractions. Therefore, the target volume needs to be accurately delineated with high spatial resolution to ensure the highly conformal dose distribution. Therefore, clinical needs demand high spatial resolution MR functional quantitative imaging, which has not yet been well developed. Geometrical accuracy is another matter of concern for radiotherapy. As a commonly used imaging technique for clinical investigations, DWI suffers from geometrical deformations that are generally associated with the field inhomogeneity problem using echo-planar imaging sequence[24] (Figure 4). In Brachytherapy, this deformation may have a prominent effect on treatment assessment, where the dose from radiation sources falls quadratically with the distance.
Figure 4.
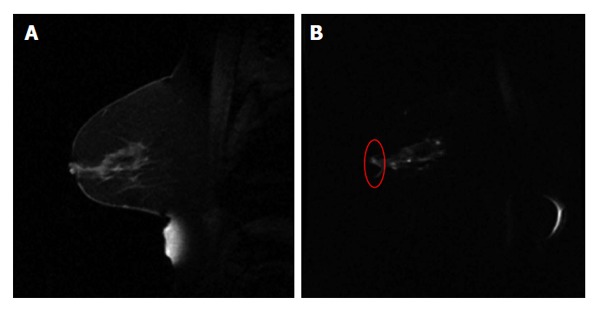
An example of sagittal breast T1w image (A) and the diffusion weighted image (b = 500 mm2/s) using echo planar imaging sequence (B). The red circle in (B) highlights the distorted breast boundary.
As another key factor of MR functional quantitative imaging quality, temporal resolution may affect the accuracy of the dynamics analysis. To assess the permeability and perfusion information using DCE imaging, the arterial input function (AIF) depicting the dynamics of tracers in arterial blood needs to be determined via imaging a major arterial structure in the imaged volume, and the fast acquisition of a second per volume is in demand for the reliable capture of rapid wash-in and wash-out features of AIF[25]. However, because the current imaging time for a 3D volume is often not fast enough (to capture AIF information from a qualified arterial structure for such measurement), population-derived mathematical AIF models are widely used for DCE analysis instead. As simple approaches ignoring the individual physiologic features, these AIF models may introduce errors to the functional parameter results[26]. Parallel imaging techniques have been proposed to accelerate the image acquisition, but the tradeoff of signal-to-noise ratio limits the reliability of the derived quantitative results[27]. Recently, iterative MR reconstruction using undersampled image data with newly-developed mathematical concepts has been proposed. Though shown promising, the reproducibility of functional quantitative results needs to be validated with comprehensive studies.
Novel image analysis methodology
In treatment assessment, it is always critical to accurately interpret and analyze the functional data to reveal underlying context of a tumor or a specific critical organ. Currently, metrics including the average/median value of a certain functional parameter within the region-of-interest and the target volume identified by thresholding the parametric map are widely reported in radiotherapies studies. Focusing on the absolute quantity, these approaches may miss the underlying morphological information hidden in the functional images. As an emerging topic in treatment assessment, image texture features have been investigated for their feasibilities of monitoring treatment assessment[28-30]. As some of the texture features, especially the grey-tone spatial-dependence matrix (GTSDM) features, are defined independent of the parameter’s absolute values, these texture features may be preferred in the case when the quantitative parameter values are not fully reliable. Another promising and interesting topic in the field is to use multiparametric functional MR for assessment purpose. With statistical approaches, multiparametric MR including both anatomical and functional images have been studied in tumor localization and staging[31-33]. Since the mechanisms of some of the functional changes in response to radiotherapy have not been fully understood yet, the creditability of multiparametric MR study results in radiotherapy response may be undermined. With an ultimate goal of individualized radiotherapy, the imaging modalities, imaging parameters, statistical packages and other factors in multiparametric functional MR study need to be standardized and optimized to ensure adequate application to radiotherapy assessment.
CONCLUSION
Further development and research is needed to understand and validate whether MR quantitative imaging is truly beneficial to future radiotherapy treatment. Being a promising imaging modality, MRI not only plays a critical role in diagnosis, but also may lead the future directions of radiotherapy.
ACKNOWLEDGMENTS
The authors would like to thank Kevin Kelly in our department for his help with DCE-MRI data acquisition. We would also like to thank Taylor Richards for his comments and language improvements.
Footnotes
P- Reviewer: Azevedo CF, Latsios G, Storto G, Wan YL S- Editor: Song XX L- Editor: A E- Editor: Liu SQ
Conflict-of-interest: The authors have no conflict of interest related to the manuscript.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: October 31, 2014
First decision: November 14, 2014
Article in press: December 31, 2014
References
- 1.Choyke PL, Dwyer AJ, Knopp MV. Functional tumor imaging with dynamic contrast-enhanced magnetic resonance imaging. J Magn Reson Imaging. 2003;17:509–520. doi: 10.1002/jmri.10304. [DOI] [PubMed] [Google Scholar]
- 2.van der Heide UA, Houweling AC, Groenendaal G, Beets-Tan RG, Lambin P. Functional MRI for radiotherapy dose painting. Magn Reson Imaging. 2012;30:1216–1223. doi: 10.1016/j.mri.2012.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Crijns SP, Bakker CJ, Seevinck PR, de Leeuw H, Lagendijk JJ, Raaymakers BW. Towards inherently distortion-free MR images for image-guided radiotherapy on an MRI accelerator. Phys Med Biol. 2012;57:1349–1358. doi: 10.1088/0031-9155/57/5/1349. [DOI] [PubMed] [Google Scholar]
- 4.Verellen D, De Ridder M, Linthout N, Tournel K, Soete G, Storme G. Innovations in image-guided radiotherapy. Nat Rev Cancer. 2007;7:949–960. doi: 10.1038/nrc2288. [DOI] [PubMed] [Google Scholar]
- 5.Yaromina A, Krause M, Baumann M. Individualization of cancer treatment from radiotherapy perspective. Mol Oncol. 2012;6:211–221. doi: 10.1016/j.molonc.2012.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hall EJ, Giaccia AJ. Radiobiology for the Radiologist. Wolters Kluwer Health: 2006. [Google Scholar]
- 7.Yankeelov TE, Lepage M, Chakravarthy A, Broome EE, Niermann KJ, Kelley MC, Meszoely I, Mayer IA, Herman CR, McManus K, et al. Integration of quantitative DCE-MRI and ADC mapping to monitor treatment response in human breast cancer: initial results. Magn Reson Imaging. 2007;25:1–13. doi: 10.1016/j.mri.2006.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haider MA, Chung P, Sweet J, Toi A, Jhaveri K, Ménard C, Warde P, Trachtenberg J, Lockwood G, Milosevic M. Dynamic contrast-enhanced magnetic resonance imaging for localization of recurrent prostate cancer after external beam radiotherapy. Int J Radiat Oncol Biol Phys. 2008;70:425–430. doi: 10.1016/j.ijrobp.2007.06.029. [DOI] [PubMed] [Google Scholar]
- 9.Kim S, Loevner L, Quon H, Sherman E, Weinstein G, Kilger A, Poptani H. Diffusion-weighted magnetic resonance imaging for predicting and detecting early response to chemoradiation therapy of squamous cell carcinomas of the head and neck. Clin Cancer Res. 2009;15:986–994. doi: 10.1158/1078-0432.CCR-08-1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee SC, Poptani H, Pickup S, Jenkins WT, Kim S, Koch CJ, Delikatny EJ, Glickson JD. Early detection of radiation therapy response in non-Hodgkin’s lymphoma xenografts by in vivo 1H magnetic resonance spectroscopy and imaging. NMR Biomed. 2010;23:624–632. doi: 10.1002/nbm.1505. [DOI] [PubMed] [Google Scholar]
- 11.Chang Z, Kirkpatrick JP, Wang Z, Cai J, Adamson J, Yin FF. Evaluating radiation-induced white matter changes in patients treated with stereotactic radiosurgery using diffusion tensor imaging: a pilot study. Technol Cancer Res Treat. 2014;13:21–28. doi: 10.7785/tcrt.2012.500358. [DOI] [PubMed] [Google Scholar]
- 12.White D, Mason RP. Non-invasive pre-clinical MR imaging of prostate tumor hypoxia for radiation therapy prognosis. Int J Cancer Ther Oncol. 2014;2:020243. [Google Scholar]
- 13.Buckler AJ, Bresolin L, Dunnick NR, Sullivan DC. A collaborative enterprise for multi-stakeholder participation in the advancement of quantitative imaging. Radiology. 2011;258:906–914. doi: 10.1148/radiol.10100799. [DOI] [PubMed] [Google Scholar]
- 14.Ben Bashat D, Ben Sira L, Graif M, Pianka P, Hendler T, Cohen Y, Assaf Y. Normal white matter development from infancy to adulthood: comparing diffusion tensor and high b value diffusion weighted MR images. J Magn Reson Imaging. 2005;21:503–511. doi: 10.1002/jmri.20281. [DOI] [PubMed] [Google Scholar]
- 15.Zhou XJ, Gao Q, Abdullah O, Magin RL. Studies of anomalous diffusion in the human brain using fractional order calculus. Magn Reson Med. 2010;63:562–569. doi: 10.1002/mrm.22285. [DOI] [PubMed] [Google Scholar]
- 16.Lambregts DM, Beets GL, Maas M, Curvo-Semedo L, Kessels AG, Thywissen T, Beets-Tan RG. Tumour ADC measurements in rectal cancer: effect of ROI methods on ADC values and interobserver variability. Eur Radiol. 2011;21:2567–2574. doi: 10.1007/s00330-011-2220-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kozlowski P, Chang SD, Meng R, Mädler B, Bell R, Jones EC, Goldenberg SL. Combined prostate diffusion tensor imaging and dynamic contrast enhanced MRI at 3T--quantitative correlation with biopsy. Magn Reson Imaging. 2010;28:621–628. doi: 10.1016/j.mri.2010.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Langer DL, van der Kwast TH, Evans AJ, Plotkin A, Trachtenberg J, Wilson BC, Haider MA. Prostate tissue composition and MR measurements: investigating the relationships between ADC, T2, K(trans), v(e), and corresponding histologic features. Radiology. 2010;255:485–494. doi: 10.1148/radiol.10091343. [DOI] [PubMed] [Google Scholar]
- 19.Latchaw RE, Yonas H, Hunter GJ, Yuh WT, Ueda T, Sorensen AG, Sunshine JL, Biller J, Wechsler L, Higashida R, et al. Guidelines and recommendations for perfusion imaging in cerebral ischemia: A scientific statement for healthcare professionals by the writing group on perfusion imaging, from the Council on Cardiovascular Radiology of the American Heart Association. Stroke. 2003;34:1084–1104. doi: 10.1161/01.STR.0000064840.99271.9E. [DOI] [PubMed] [Google Scholar]
- 20.Calamante F. Bolus dispersion issues related to the quantification of perfusion MRI data. J Magn Reson Imaging. 2005;22:718–722. doi: 10.1002/jmri.20454. [DOI] [PubMed] [Google Scholar]
- 21.Xu G, Rowley HA, Wu G, Alsop DC, Shankaranarayanan A, Dowling M, Christian BT, Oakes TR, Johnson SC. Reliability and precision of pseudo-continuous arterial spin labeling perfusion MRI on 3.0 T and comparison with 15O-water PET in elderly subjects at risk for Alzheimer’s disease. NMR Biomed. 2010;23:286–293. doi: 10.1002/nbm.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shin W, Horowitz S, Ragin A, Chen Y, Walker M, Carroll TJ. Quantitative cerebral perfusion using dynamic susceptibility contrast MRI: evaluation of reproducibility and age- and gender-dependence with fully automatic image postprocessing algorithm. Magn Reson Med. 2007;58:1232–1241. doi: 10.1002/mrm.21420. [DOI] [PubMed] [Google Scholar]
- 23.Wehrl HF, Judenhofer MS, Wiehr S, Pichler BJ. Pre-clinical PET/MR: technological advances and new perspectives in biomedical research. Eur J Nucl Med Mol Imaging. 2009;36 Suppl 1:S56–S68. doi: 10.1007/s00259-009-1078-0. [DOI] [PubMed] [Google Scholar]
- 24.Wu M, Chang LC, Walker L, Lemaitre H, Barnett AS, Marenco S, Pierpaoli C. Comparison of EPI distortion correction methods in diffusion tensor MRI using a novel framework. Med Image Comput Comput Assist Interv. 2008;11:321–329. doi: 10.1007/978-3-540-85990-1_39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Henderson E, Rutt BK, Lee TY. Temporal sampling requirements for the tracer kinetics modeling of breast disease. Magn Reson Imaging. 1998;16:1057–1073. doi: 10.1016/s0730-725x(98)00130-1. [DOI] [PubMed] [Google Scholar]
- 26.Wang CH, Yin FF, Horton J, Chang Z. Review of treatment assessment using DCE-MRI in breast cancer radiation therapy. World J Methodol. 2014;4:46–58. doi: 10.5662/wjm.v4.i2.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Deshmane A, Gulani V, Griswold MA, Seiberlich N. Parallel MR imaging. J Magn Reson Imaging. 2012;36:55–72. doi: 10.1002/jmri.23639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li KL, Wilmes LJ, Henry RG, Pallavicini MG, Park JW, Hu-Lowe DD, McShane TM, Shalinsky DR, Fu YJ, Brasch RC, et al. Heterogeneity in the angiogenic response of a BT474 human breast cancer to a novel vascular endothelial growth factor-receptor tyrosine kinase inhibitor: assessment by voxel analysis of dynamic contrast-enhanced MRI. J Magn Reson Imaging. 2005;22:511–519. doi: 10.1002/jmri.20387. [DOI] [PubMed] [Google Scholar]
- 29.Karahaliou A, Vassiou K, Arikidis NS, Skiadopoulos S, Kanavou T, Costaridou L. Assessing heterogeneity of lesion enhancement kinetics in dynamic contrast-enhanced MRI for breast cancer diagnosis. Br J Radiol. 2010;83:296–309. doi: 10.1259/bjr/50743919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alic L, van Vliet M, van Dijke CF, Eggermont AM, Veenland JF, Niessen WJ. Heterogeneity in DCE-MRI parametric maps: a biomarker for treatment response? Phys Med Biol. 2011;56:1601–1616. doi: 10.1088/0031-9155/56/6/006. [DOI] [PubMed] [Google Scholar]
- 31.Turkbey B, Pinto PA, Mani H, Bernardo M, Pang Y, McKinney YL, Khurana K, Ravizzini GC, Albert PS, Merino MJ, et al. Prostate cancer: value of multiparametric MR imaging at 3 T for detection--histopathologic correlation. Radiology. 2010;255:89–99. doi: 10.1148/radiol.09090475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Franiel T, Stephan C, Erbersdobler A, Dietz E, Maxeiner A, Hell N, Huppertz A, Miller K, Strecker R, Hamm B. Areas suspicious for prostate cancer: MR-guided biopsy in patients with at least one transrectal US-guided biopsy with a negative finding--multiparametric MR imaging for detection and biopsy planning. Radiology. 2011;259:162–172. doi: 10.1148/radiol.10101251. [DOI] [PubMed] [Google Scholar]
- 33.Hoeks CM, Barentsz JO, Hambrock T, Yakar D, Somford DM, Heijmink SW, Scheenen TW, Vos PC, Huisman H, van Oort IM, et al. Prostate cancer: multiparametric MR imaging for detection, localization, and staging. Radiology. 2011;261:46–66. doi: 10.1148/radiol.11091822. [DOI] [PubMed] [Google Scholar]


