Summary
Endovascular treatment of wide-neck bifurcation aneurysms is challenging and often requires adjunctive techniques and devices. We report our experience with the hybrid Y stenting with the waffle-cone technique, combining Y stent-assisted coiling and waffle-cone stenting techniques. This approach has been described only in a single case report using a combination of open and closed cell stents. We describe four cases treated by hybrid Y stenting with the waffle-cone procedure with a variation from the originally reported technique, consisting in deploying two closed cell stents. All patients were successfully treated without complications. We propose hybrid Y stenting with the waffle-cone for the treatment of wide-neck bifurcation aneurysms as a bailout technique after failure of Y stent-assisted coiling.
Keywords: intracranial aneurysm, stent, embolization
Introduction
The endovascular treatment of wide-neck bifurcation aneurysms has improved with new techniques and devices. However, it remains challenging in some cases, even if standard adjunctive techniques, such as balloon remodelling 1 or stent-assisted coiling 2 are used. Therefore, some advanced stenting techniques have been developed, such as Y stent-assisted coiling, consisting in deployment of two overlapping stents in both bifurcation branches to reconstruct the neck and to assist coiling of the aneurysm 3-8. Another technique is waffle-cone assisted coiling, in which the terminal aspect of a single stent is placed inside the aneurysm to protect the base from coil protrusion during coiling 9-15. Both techniques have some drawbacks. We describe the use of a hybrid technique, consisting in coiling after the placement of a stent in one bifurcation branch, and then a second stent inside the aneurysm in a waffle-cone fashion. To our knowledge, this technique has been reported only once for the treatment of a basilar tip aneurysm. However that report slightly differed from our cases as both a closed and an open cell devices were used, whereas we only used closed cell stents 16. We propose hybrid Y stenting combined with the waffle-cone as a bailout procedure after failure of conventional Y stent-assisted coiling.
Materials and Methods
We selected from our database all aneurysms treated by hybrid Y stenting combined with the waffle-cone technique. Four patients, all females, were selected (mean age 64.2). In three elective cases, the intention-to-treat was conventional Y stent-assisted coiling but the approach was switched during the procedure; in one ruptured aneurysm, hybrid Y stenting combined with the waffle-cone was planned before the procedure.
Technique
We describe our standard technique, which was similar in all cases. All elective patients were given ticlopidine 250 mg b.i.d. and aspirin 300 mg q.d., starting ten days before the procedure and to be continued for six months; antiplatelet agents resistance was assayed before surgery. In ruptured aneurysms, a single dose of 500 mg i.v. aspirin was given after groin puncture and 600 mg clopidogrel loading dose was given before stenting via a nasogastric tube. All interventions were performed under full anticoagulation (ACT value 250-300). From the femoral access, a 6F 90 cm long Arrow introducer sheath (Arrow International, Reading, PA, USA) was advanced into the internal or common carotid artery, and a 6F 100 cm long Envoy guide catheter (Cordis, Miami, FL, USA) was advanced coaxially in the internal carotid artery. One of the bifurcation branches was catheterized with a Prowler select plus microcatheter (Codman Neurovascular, Miami, FL, USA) over a hydrophilic 0.016” wire (GT wire, Terumo, Tokyo, Japan), then a 4.5×28 Enterprise stent (Codman Neurovascular, Miami, FL, USA) was deployed across the neck of the aneurysm. After failure of catheterization of the other bifurcation branch, necessary for the initially planned Y stenting, the aneurysm was accessed with another Prowler select plus microcatheter, crossing the interstices of the stent. In a single case, the aneurysm was accessed with the Prowler select plus before deployment of the first stent. Then, a second closed cell stent was deployed inside the aneurysm in a waffle-cone configuration (Solitaire AB; eV3/Covidien, Irvine, California, USA or Enterprise stent). Finally, the aneurysm was catheterized again crossing through the stents with an Echelon 10 microcatheter (eV3/Covidien, Irvine, California, USA) and embolized with Galaxy coils (Codman Neurovascular, Miami, FL, USA). Feasibility of the treatment, complication rates, morbidity and mortality, immediate and follow-up angiographic outcome (using the Raymond-Roy scale) were evaluated.
Results
In all cases the procedure was completed. Immediate complete occlusion was obtained in two cases (RR1) and small aneurysm remnants in two cases (RR3).
No complications occurred. At six-month clinical follow-up all patients were asymptomatic (mRS). Angiographic follow-up between six and 36 months (mean 15 months) after treatment was available. All aneurysms remained unchanged without any regrowth (Table 1).
Table 1.
Characteristics of aneurysms, technique and results.
| Case |
Sex Age |
R/ UR |
Site |
Sac size (mm) Neck width (mm) |
Arteries from the sac |
First stent |
Second stent |
Clinical outcome** |
Immediate angiographic result*** |
Follow-up angiographic result*** |
| 1 | F, 65 | UR | ACM | 12×8-8 | N | Enterprise 4.5×28 |
Solitaire 4×20 |
mRS0 | RR 3 | RR 3 (3 y) |
| 2 | F, 57 | R* | AComA | 8×5-5 | Y | Enterprise 4.5×28 |
Solitaire 4×20 |
mRS0 | RR 1 | RR 1 (1 y) |
| 3 | F, 83 | R | AComA | 7×7-6 | Y | Enterprise 4.5×28 |
Solitaire 6×20 |
mRS0 | RR 2 | RR 2 (6 m) |
| 4 | F, 52 | UR | Carotid tip |
8×6-4 | N | Enterprise 4.5×28 |
Enterprise 4.5×22 |
mRS0 | RR 2 | RR 2 (6 m) |
|
* Intraprocedural rupture during Y stenting ** Modified Rankin scale (mRS) at 6 months *** Raymond-Roy (RR) grade. | ||||||||||
Case 1
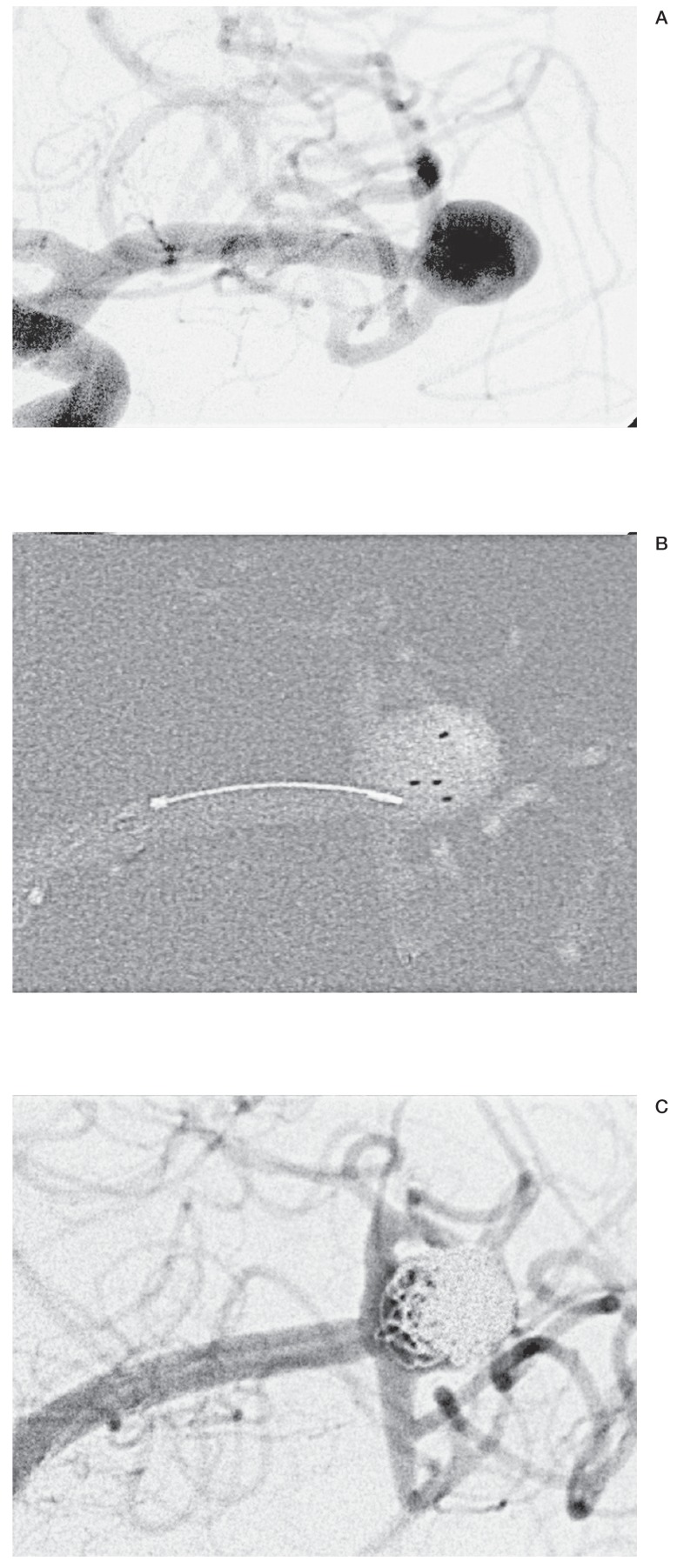
A 65-year-old woman was referred for an incidental middle cerebral artery (MCA) wide-neck bifurcation aneurysm (Figure 1). Both bifurcation branches originated from the neck at an acute angle. Clipping was proposed as a first option but the patient refused, so Y stent-assisted coiling was planned. After deployment of the Enterprise in the inferior branch of the bifurcation, which was the most angulated, catheterization of the superior bifurcation branch through the meshes of the first stent was attempted.
Figure 1.
A) Left MCA wide-necked aneurysm with a sharp angle between the proximal vessel and the diverging branches. B) After placement of the first stent in lower branch, the second one is deployed inside the aneurysm in a combined Y and waffle-cone fashion, achieving good protection of the MCA branches. C) Final result with evidence of a basal remnant and patency of both branches.
All catheterizations attempt failed, including the exchange manoeuvre after passing the stent with an Echelon 10. At the time of intervention small profile stents that could be delivered by a 10 catheter were still not available. Therefore, a Solitaire stent was deployed with its distal tip inside the aneurysm in a waffle-cone fashion. Finally, the aneurysm was catheterized through the stents and coiled: the presence of the stents allowed coiling with protection of bifurcation branches. The aneurysm was occluded with a small loosely coiled basal remnant, which was stable at three-year follow-up.
Case 2
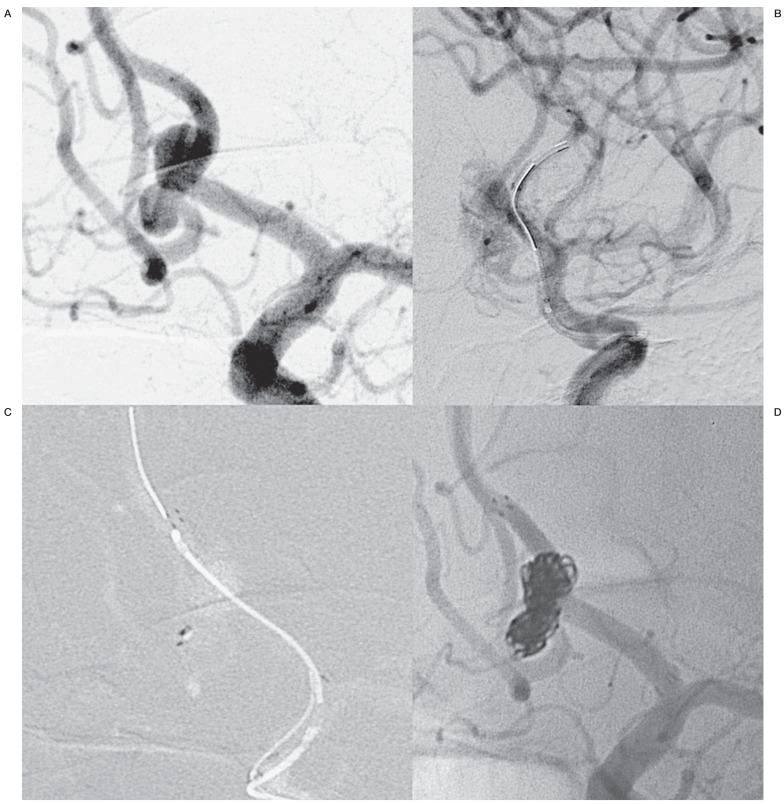
A 57-year-old woman was referred for an unruptured aneurysm of the anterior communicating artery (AComA), with shape and size modifications during MRI follow-up. The sac was bilobated, the largest diameter was 8 mm, the right A2 tract originated from the sac and the right A1 was hypoplastic (Figure 2). Coiling with Y stent-assisted coiling as intention-to-treat was planned. During catheterization attempt of the right A2 tract, the right lobe of the aneurysm was perforated and catheterization failed. Heparin was reversed with protamine sulphate. Sudden catheterization of the left A2 tract was performed and the Enterprise stent was deployed; then, the right lobe of the aneurysm was catheterized through the meshes of the first stent and a 4×20 Solitaire AB stent was deployed inside the aneurysm in a waffle-cone fashion. Finally the aneurysm was coiled with complete occlusion. The patient had good clinical recovery with no neurological deficits. One-year angiographic follow-up confirmed aneurysm occlusion.
Figure 2.
A) AComA bilobated aneurysm with origin of right A2 tract from the sac. B) After aneurysm rupture, during a right A2 catheterization attempt, a microcatheter is placed in the left A2 and the first stent is deployed. C) Another stent is deployed inside the right aneurysmal lobe, in a hybrid Y stenting technique combined with waffle-cone configuration. D) The aneurysm is coiled with complete occlusion.
Case 3
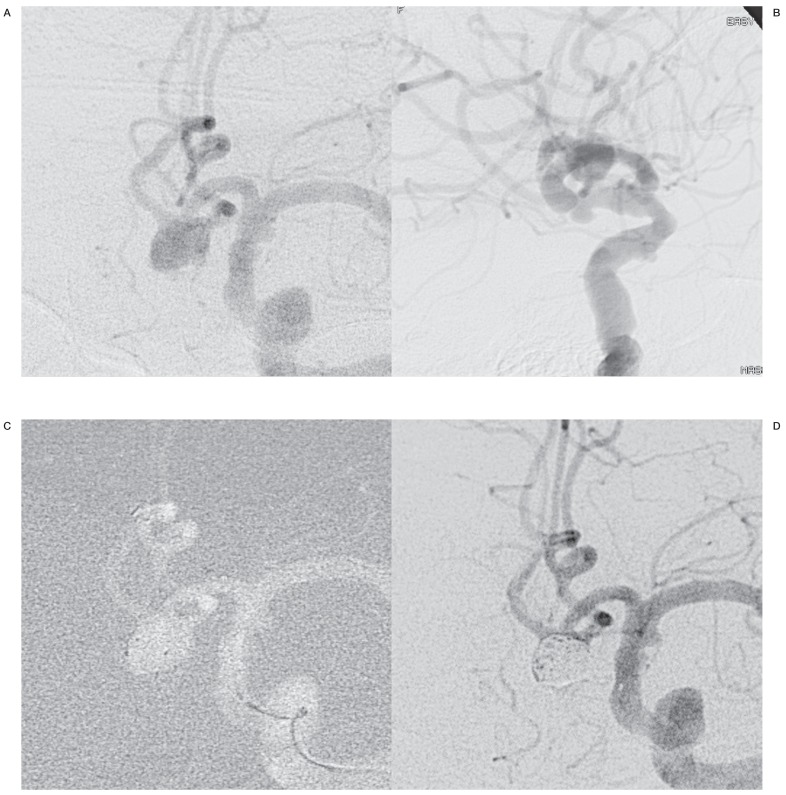
An 83-year-old woman was referred for acute subarachnoid haemorrhage (Fisher 3, H&H 2). She was already known to have a wide-neck AComA aneurysm, which had not been previously treated because of patient's age. Angiography confirmed a wide-necked 7 mm AComA aneurysm, with left A2 segment originating from the basal aspect of the sac at an acute angle; the right A1 segment was hypoplastic (Figure 3). Diffuse atherosclerotic changes to the left carotid siphon were also present. Since the patient's clinical status was good and no significant comorbidities were reported, we decided to treat the aneurysm. In consideration of aneurysm shape and vascular conditions, clipping would have been the most suitable option. However, patient age was considered a very limiting factor for clipping, so endovascular coiling was decided. The intention-to-treat of the endovascular intervention was hybrid Y stenting with the waffle-cone, since we felt that neither balloon-assisted coiling nor conventional stent-assisted coiling could achieve protection of the parent vessel and bifurcation branches. Double balloon remodelling was not contemplated because we estimated that left A2 catheterization was too dangerous and that this technique would not have guaranteed artery protection. Y stent-assisted coiling was not contemplated because catheterization of the left A1 was considered too difficult and dangerous. The first stent was deployed from the left A1 tract to right A2 tract, then a 6×20 Solitaire AB was deployed inside the aneurysm. Subsequent catheterization of the aneurysm navigating the two telescopic stents was challenging. Afterwards the aneurysm was coiled achieving compact packaging of the body and dome of the sac, with a loosely coiled basal remnant. At six-month angiographic follow-up the aneurysm remnant is stable and the patient has no neurological deficits.
Figure 3.
Ruptured wide-necked AComA aneurysm in working frontal (A) and lateral (B) projections. C) An Enterprise is placed in the right A2 tract and a Solitaire is deployed inside the aneurysm. D) After coiling the aneurysm is occluded with a loosely coiled remnant and the bifurcation branches are patent.
Case 4
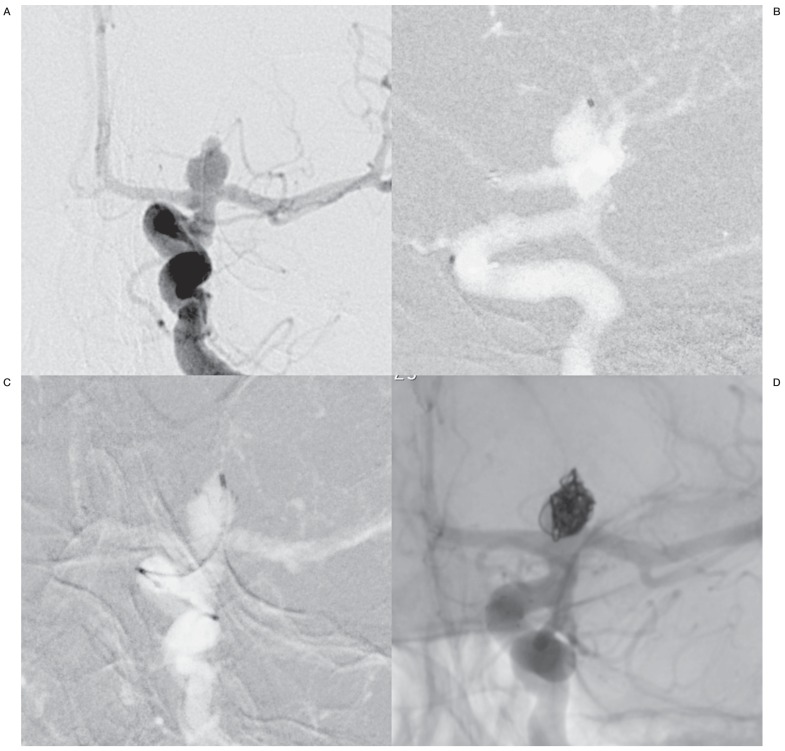
A 52-year-old woman was referred for an 8 mm, wide-necked unruptured left carotid tip aneurysm (Figure 4). Y stent-assisted coiling was planned. After placement of the first stent in the A1 tract, catheterization of the middle cerebral artery failed, even though the stent could be crossed with the guidewire.
Figure 4.
A) Left carotid tip aneurysm in working projection. B) A stent is deployed in the anterior cerebral artery and a microcatheter is then placed inside the aneurysm. C) After deployment of the waffle-cone stent, another catheter is placed inside the aneurysm for coiling. D) Final unsubtracted view after coiling.
Therefore, the aneurysm was catheterized through the stent and a second Enterprise was placed in a waffle-cone configuration. Finally, the aneurysm was coiled achieving complete occlusion.
No complications occurred. At six-month angiographic follow-up the aneurysm is occluded and the patient has no neurological deficits.
Discussion
Endovascular treatment of wide-neck bifurcation aneurysms is still challenging. Since simple coiling is often not possible, some adjunctive techniques have been developed, such as the balloon remodelling technique 1 and stent-assisted coiling 2, which allow treatment of most aneurysms. Nevertheless, complex morphological conditions such as very wide-neck, arteries incorporated with the aneurysm or impossible distal catheterization due to an acute bifurcation angle can prevent the treatment even with standard adjunctive techniques 17.
One technique used for complex aneurysms not amenable to conventional endovascular techniques is Y stent-assisted coiling, consisting in placement of two crossing stents in a Y configuration to protect the bifurcation branches during coiling 3-8. A variation of this technique consists in deploying two parallel stents 18. Y stent-assisted coiling leads to a very high occlusion rate but it has some drawbacks: the procedure is challenging with possible aneurysm perforation, moreover the presence of two crossing stents in the parent vessel could lead to an increased risk of acute thrombosis or late stenosis. If the catheterization of both bifurcation vessels cannot be accomplished because of vessel angulations or difficulty in crossing the interstices of the first stent, Y stenting cannot be achieved. In addition, flow diverter stents have been used for bifurcation aneurysm treatment, but although they allow a high occlusion rate, the patency of the unstented branch is a major concern 19. Recently, flow disruption with intra-aneurysmal devices has been proposed and appears an interesting approach for bifurcation aneurysms 20, however few data are available on the safety and efficacy of these devices.
An alternative technique is waffle-cone assisted coiling: the distal component of the stent is deployed inside the aneurysms where it is allowed to fan out, supporting the subsequent coiling 9-15. In early reports, this technique was performed with open cell devices 9, but more recently a waffle-cone technique using a closed cell stent has been described 10-15,18. A good coverage of the neck is not always possible and placement of the stent into the aneurysm entails the potential risk of perforation.
We describe a combined approach, which could help in difficult cases. With this technique, since one of the bifurcation branches is protected by the first stent, the waffle-cone stent is adequate to support coiling by creating scaffolding for coils thus preventing their prolapse towards the parent vessel or the bifurcation branches.
To our knowledge, a single case report of hybrid Y stenting with the waffle-cone has been reported in the literature by Cho et al. 16. Moreover, Hauck et al. described the case of a giant ophthalmic aneurysm growing after waffle-cone-assisted coiling and retreated deploying a stent through the initially placed stent to recreate the aneurysm neck and assist coiling. However, this case should be regarded as a failure of the waffle-cone technique as the intention-to-treat was not the hybrid waffle-cone technique 21.
In the report by Cho et al., a ruptured broad base basilar tip aneurysm was treated with this technique after failure of conventional Y stent-assisted coiling. The authors first placed a closed cell stent (Enterprise) in one posterior cerebral artery, then they deployed an open cell stent into the aneurysm through the interstices of the first one, stating that the closed strut system of the first stent holds the open cell stent at the point of penetration making a waffle-cone shape with a narrower base 16. We agree that the first stent should be a closed cell one, since it can be navigated and deployed more easily than an open cell stent. However, we believe that the second stent should be a closed cell device too, because of many advantages. An open cell stent can be repositioned without displacing the first stent; moreover a tapered stent with a flared end and without platinum wire reduces the risk of perforation, making the procedure safer. In our experience, the second stent was a Solitaire in three out of four cases, because it can be deployed very easily, can be fully recovered before detachment, it has no distal platinum wire purchase and its largest available diameter is 6mm. We believe that the second stent should be larger than the parent vessel, in order to freely expand inside the aneurysm assuming a waffle-cone shape, but not larger than the aneurysm diameter to avoid perforations.
It may be argued that these aneurysms could have been treated with a single stent placed in a waffle-cone configuration. However, given the broad base of these aneurysms, it is unlikely that the waffle-cone stent would have fully covered the base of the aneurysm (especially for cases 1, 2 and 3). Moreover, in three out of four cases a stent had already been deployed in one bifurcation branch since the intention to treat was Y stenting. In the other patient (case 3), hybrid Y stenting with the waffle-cone was the first choice because we estimated that a single waffle-cone stent was not adequate to protect the bifurcation vessels since the neck was very large.
Compared with the conventional waffle-cone technique, we believe that hybrid Y stenting with the waffle-cone allows safer protection of the neck and the bifurcation branches because of greater neck coverage even in case of very complex morphology. Recently, a new device designed for waffle-cone-assisted coiling has been proposed (pCONus, Phenox, Bochum, Germany). There are still few reported data about this device, but it should help obtain a more complete coiling with an easier neck protection than conventional stents placed in a waffle-cone fashion 22. Nevertheless, the feasibility of this technique must still be demonstrated in case of very complex shape aneurysms, when simple scaffolding of the neck may not be enough to protect from coil prolapse. The combination of pCONus with other devices could be an interesting possibility. Recently, placement of two pCONus devices in a Y configuration has been reported 23.
In case of the standard waffle-cone technique, the flow is directed by the stent towards the base of the aneurysm, so potentially increasing the chance of recurrence. One advantage of Y stent-assisted coiling over waffle-cone-assisted embolization is the flow-diverting effect of the crossing stents 24,25, which is expected to limit the chance of recurrences. We have no data on flow modification after hybrid Y stenting with the waffle-cone, but it is likely that the crossing of the stents and the presence of one stent placed in a standard fashion would avoid direct flow towards the base of the aneurysm.
One drawback of this technique is the theoretical risk of acute or late ischaemia due to the incomplete opening of one of the two stents at the crossing point. In our small series we did not observe any ischaemic event, although the number of patients is too small to assess this point. The same risk occurs with Y stent-assisted coiling, but in the largest series of aneurysms treated with this technique the ischaemic complication rate was low 7,8.
An alternative technique for very wide-neck aneurysms is double balloon remodelling. However this technique is challenging and we never use it in elective patients (three out four of our cases). We do not believe that hybrid Y stenting with waffle-cone-assisted coiling should be proposed as a first-line technique for aneurysm treatment. In three out of four cases, we first tried to perform conventional Y stent-assisted coiling but this technique failed because of the angulation of one bifurcation branch and its difficult catheterization. In the other case, the aneurysm had such a complex morphology that would have usually contraindicated an endovascular approach, but we decided to treat it because the advanced age of the patient made clipping more dangerous.
In our small series, we did not experience any complication from this technique. However, we believe that hybrid Y stenting with the waffle-cone is technically challenging and the risk of complications must not be underestimated. This technique should not be attempted for aneurysms with short dome heights where a deployment error could result in rupture, or aneurysms with necks less than the size of the distal stent flare, because of the risk of perforation.
Therefore, hybrid Y stenting with the waffle-cone should be regarded as a bailout procedure for complex shape bifurcation aneurysms after failure of conventional Y stent-assisted coiling or other treatment modalities.
References
- 1.Pierot L, Cognard C, Spelle L, et al. Safety and efficacy of balloon remodeling technique during endovascular treatment of intracranial aneurysms: critical review of the literature. Am J Neuroradiol. 2012;33(1):12–15. doi: 10.3174/ajnr.A2403. doi: 10.3174/ajnr.A2403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Geyik S, Yavuz K, Yurttutan N, et al. Stent-assisted coiling in endovascular treatment of 500 consecutive cerebral aneurysms with long-term follow-up. Am J Neuroradiol. 2013;34(11):2157–2162. doi: 10.3174/ajnr.A3574. doi: 10.3174/ajnr.A3574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chow MM, Woo HH, Masaryk TJ, et al. A novel endovascular treatment of a wide-necked basilar apex aneurysm by using a Y-configuration, double-stent technique. Am J Neuroradiol. 2004;25(3):509–512. [PMC free article] [PubMed] [Google Scholar]
- 4.Perez-Arjona E, Fessler RD. Basilar artery to bilateral posterior cerebral artery 'Y stenting' for endovascular reconstruction of wide-necked basilar apex aneurysms: report of three cases. Neurol Res. 2004;26(3):276–281. doi: 10.1179/016164104225013969. doi: 10.1179/016164104225013969. [DOI] [PubMed] [Google Scholar]
- 5.Thorell WE, Chow MM, Woo HH, et al. Y-configured dual intracranial stent-assisted coil embolization for the treatment of wide-necked basilar tip aneurysms. Neurosurgery. 2005;56(5):1035–1040. [PubMed] [Google Scholar]
- 6.Conrad MD, Brasiliense LB, Richie AN, et al. Y stenting assisted coiling using a new low profile visible intraluminal support device for wide necked basilar tip aneurysms: a technical report. J Neurointerv Surg. 2013 doi: 10.1136/neurintsurg-2013-010818. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 7.Yavuz K, Geyik S, Cekirge S, et al. Double stent-assisted coil embolization treatment for bifurcation aneurysms: immediate treatment results and long-term angiographic outcome. Am J Neuroradiol. 2013;34(9):1778–1784. doi: 10.3174/ajnr.A3464. doi: 10.3174/ajnr.A3464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fargen KM, Mocco J, Neal D, et al. A multicenter study of stent-assisted coiling of cerebral aneurysms with a Y configuration. Neurosurgery. 2013;73(3):466–472. doi: 10.1227/NEU.0000000000000015. doi: 10.1227/NEU.0000000000000015. [DOI] [PubMed] [Google Scholar]
- 9.Horowitz M, Levy E, Sauvageau E, et al. Intra/extra-aneurysmal stent placement for management of complex and wide-necked- bifurcation aneurysms: eight cases using the waffle cone technique. Neurosurgery. 2006;58(4) Suppl 2:ONS258–ONS262. doi: 10.1227/01.NEU.0000204713.24945.D2. discussion ONS262. [DOI] [PubMed] [Google Scholar]
- 10.Yang TH, Wong HF, Yang MS, et al. "Waffle cone" technique for intra/extra-aneurysmal stent placement for the treatment of complex and wide-necked bifurcation aneurysm. Interv Neuroradiol. 2008;14(Suppl 2):49–52. doi: 10.1177/15910199080140S210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sychra V, Klisch J, Werner MD, et al. Waffle-cone technique with Solitaire™ AB remodeling device: endovascular treatment of highly selected complex cerebral aneurysms. Neuroradiology. 2011;53:961–972. doi: 10.1007/s00234-010-0766-6. doi: 10.1007/s00234-010-0766-6. [DOI] [PubMed] [Google Scholar]
- 12.Park HR, Yoon SM, Shim JJ, et al. Waffle-cone technique using solitaire AB stent. J Korean Neurosurg Soc. 2012;51(4):222–226. doi: 10.3340/jkns.2012.51.4.222. doi: 10.3340/jkns.2012.51.4.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xu F, Qin X, Tian Y, et al. Endovascular treatment of complex intracranial aneurysms using intra/extra-aneurysmal stent. Acta Neurochir (Wien) 2011;153(4):923–930. doi: 10.1007/s00701-010-0934-9. doi: 10.1007/s00701-010-0934-9. [DOI] [PubMed] [Google Scholar]
- 14.Liu W, Kung DK, Policeni B, et al. Stent-assisted coil embolization of complex wide-necked bifurcation cerebral aneurysms using the "waffle cone" technique. A review of ten consecutive cases. Interv Neuroradiol. 2012;18(1):20–28. doi: 10.1177/159101991201800103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Padalino DJ, Singla A, Jacobsen W, et al. Enterprise stent for waffle-cone stent-assisted coil embolization of large wide-necked arterial bifurcation aneurysms. Surg Neurol Int. 2013;4:9. doi: 10.4103/2152-7806.106268. doi: 10.4103/2152-7806.106268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cho JS, Kim YJ. Modified 'y-configured stents with waffle cone technique' for broad neck basilar top aneurysm. J Korean Neurosurg Soc. 2011;50(6):517–519. doi: 10.3340/jkns.2011.50.6.517. doi: 10.3340/jkns.2011.50.6.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mangiafico S, Guarnieri G, Consoli A, et al. Endovascular strategy for unruptured cerebral aneurysms. Eur J Radiol. 2013;82(10):1638–1645. doi: 10.1016/j.ejrad.2012.11.005. doi: 10.1016/j.ejrad.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 18.Jankowitz BT, Thomas A, Jovin T, et al. Y stenting using kissing stents for the treatment of bifurcation aneurysms. J Neurointerv Surg. 2012;4(1):16–21. doi: 10.1136/jnis.2010.004275. doi: 10.1136/jnis.2010.004275. [DOI] [PubMed] [Google Scholar]
- 19.Yavuz K, Geyik S, Saatci I, et al. Endovascular treatment of middle cerebral artery aneurysms with flow modification with the use of the pipeline embolization device. Am J Neuroradiol. 2014;35(3):529–535. doi: 10.3174/ajnr.A3692. doi: 10.3174/ajnr.A3692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lubicz B, Klisch J, Gauvrit JY, et al. WEB-DL Endovascular treatment of wide-neck bifurcation aneurysms: short- and midterm results in a european study. Am J Neuroradiol. 2014;35(3):432–438. doi: 10.3174/ajnr.A3869. doi: 10.3174/ajnr.A3869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hauck EF, Natarajan SK, Hopkins LN, et al. Salvage Neuroform stent-assisted coiling for recurrent giant aneurysm after waffle-cone treatment. J Neurointerv Surg. 2011;3(1):27–29. doi: 10.1136/jnis.2010.002931. doi: 10.1136/jnis.2010.002931. [DOI] [PubMed] [Google Scholar]
- 22.Aguilar-Pérez M, Kurre W, Fischer S, et al. Coil occlusion of wide-neck bifurcation aneurysms assisted by a novel intra- to extra-aneurysmatic neck-bridging device (pCONus): initial experience. Am J Neuroradiol. 2013 doi: 10.3174/ajnr.A3807. doi: 10.3174/ajnr.A3807. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mpotsaris A, Henkes H, Weber W. Waffle Y technique: pCONus for tandem bifurcation aneurysms of the middle cerebral artery. J Neurointerv Surg. 2013 doi: 10.1136/neurintsurg-2013-010921.rep. doi: 10.1136/neurintsurg-2013-010921.rep. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 24.Kono K, Terada T. Hemodynamics of 8 different configurations of stenting for bifurcation aneurysms. Am J Neuroradiol. 2013;34(10):1980–1986. doi: 10.3174/ajnr.A3479. doi: 10.3174/ajnr.A3479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gao B, Baharoglu MI, Cohen AD, et al. Y-stent coiling of basilar bifurcation aneurysms induces a dynamic angular vascular remodeling with alteration of the apical wall shear stress pattern. Neurosurgery. 2013;72(4):617–629. doi: 10.1227/NEU.0b013e3182846d9f. discussion 628-629. doi: 10.1227/NEU.0b013e3182846d9f. [DOI] [PubMed] [Google Scholar]