Abstract
This study evaluated the in vivo potential antihypertensive effect of hydroalcoholic extract of Syzygium cumini leaves (HESC) in normotensive Wistar rats and in spontaneously hypertensive rats (SHR), as well as its in vitro effect on the vascular reactivity of resistance arteries. The hypotensive effect caused by intravenous infusion of HESC (0.01–4.0 mg/kg) in anesthetized Wistar rats was dose-dependent and was partially inhibited by pretreatment with atropine sulfate. SHR received HESC (0.5 g/kg/day), orally, for 8 weeks and mean arterial pressure, heart rate, and vascular reactivity were evaluated. Daily oral administration of HESC resulted in a time-dependent blood pressure reduction in SHR, with a maximum reduction of 62%. In the endothelium-deprived superior mesenteric arteries rings the treatment with HESC reduced by 40% the maximum effect (E max) of contraction induced by NE. The contractile response to calcium and NE of endothelium-deprived mesenteric rings isolated from untreated SHR was reduced in a concentration-dependent manner by HESC (0.1, 0.25, and 0.5 mg/mL). This study demonstrated that Syzygium cumini reduces the blood pressure and heart rate of SHR and that this antihypertensive effect is probably due to the inhibition of arterial tone and extracellular calcium influx.
1. Introduction
More than one-fourth of the world's adult population suffers from arterial hypertension [1]. The objective of antihypertensive treatment is to achieve optimal blood pressure levels during therapy in order to reduce hypertension-related complications. Studies have shown that a reduction of 5 mmHg in systolic blood pressure (SBP) is associated with a 7% reduction in cardiovascular mortality [2, 3]. The research literature indicates that complementary and alternative medicine is an important potential field for the treatment of hypertension by contributing in reducing blood pressure levels and minimizing its complications [4].
Syzygium cumini L. Skeels (syn. Eugenia jambolana Lam.) is a tropical tree of the family Myrtaceae, which is popularly known as jambolan. The plant is extensively used for the treatment of different diseases, such as inflammation, constipation, obesity, urinary disorders, diabetes, and hypertension [5–9]. Pharmacological studies have suggested hypoglycemic and antihyperglycemic properties of this medicinal species [10–19]. Other experimental studies using different extracts of the plant suggest that S. cumini possesses antioxidant activity [20], antiatherosclerotic potential [21], and a cardioprotective effect [22–24].
Despite the biological potential of S. cumini as a pharmacological tool, studies validating its use as an antihypertensive agent are rare. In Brazil, it was observed that an aqueous extract of jambolan leaves reduced the blood pressure and presented diuretic effect in anesthetized normotensive rats [25, 26]. In addition, our group demonstrated an antagonistic action of hydroalcoholic S. cumini leaf extract on contractions induced by calcium in in vitro preparations of aorta from normotensive rats [27].
The use of medicinal plants as primary care is a common practice in Brazil. As a consequence, the Brazilian government has developed a program that compiled a list of medicinal plant species. On this list, called the National Register of Plants of Interest to the National Health System (Relação Nacional de Plantas de Interesse do Sistema Único de Saúde, RENISUS), S. cumini occupies the 64th position, but with the reservation that there are no studies or indication of use. In this respect, our research group has been working tirelessly to obtain data on this plant species and preclinical toxicological studies have shown that S. cumini exhibits no chronic toxicity [28], validating its safe use by the population.
The present study evaluated the antihypertensive effect of hydroalcoholic extract of S. cumini leaves in spontaneously hypertensive rats (SHR), as well as its hypotensive mechanism in in vivo and in vitro assays, in order to validate the use of this species as a pharmacological tool in ethnomedicine.
2. Materials and Methods
2.1. Plant
Leaves of S. cumini were collected from the campus of the Federal University of Maranhão (Universidade Federal do Maranhão, UFMA), São Luís, Brazil, in October 2012. A voucher specimen was identified and deposited in the herbarium of the “Professor Dr. Berta Lange de Morretes” Medicinal Plant Garden, UFMA (number 1069).
2.2. Preparation of the Hydroalcoholic Extract of Syzygium cumini
The leaves were dried at room temperature and pulverized. The crude extract was prepared by maceration of the leaf powder in 70% ethanol and concentration in a rotary evaporator under reduced pressure at a temperature below 60°C. The concentrated extract thus obtained was called the hydroalcoholic extract of S. cumini leaves (HESC) with a dry weight of 60 g, yield of 16.3% (Brazil, PI 1101652-3/18 of June, 2013) [29]. Phytochemical screening revealed the presence of hydrolyzable tannins, phenols, flavonoids, steroids, terpenoids, quinones, and saponins.
2.3. Animals
Male 12-week-old spontaneously hypertensive rats (SHR) and Wistar rats (Rattus norvegicus), weighing 250 to 300 g, obtained from the Animal House of UFMA were used. The animals were housed under controlled conditions of temperature (21 ± 2°C) under a 12 h light-dark cycle, with ration and water available ad libitum. After a period of adaptation, SHR were randomly divided into a control group and a group treated with HESC (0.5 g/kg/day, orally). Wistar rats were used as normotensive controls. The control groups received a similar volume of water (0.1 mL/100 g). The experimental protocols were approved by the Animal Research Ethics Committee of UEMA, Brazil (Protocol 17/2012).
2.4. Effect of HESC on the Blood Pressure of Normotensive Rats
Wistar rats were anesthetized with 20% urethane (0.8 g/kg, i.p.) and 1% pentobarbital sodium (40 mg/kg, i.p.). Next, tracheostomy was created and the right femoral vein was cannulated for administration of the drugs and extract. A bolus injection of heparin (30 IU) was given immediately after the venous access. The left carotid artery was cannulated for mean arterial pressure (MAP) recording. Pressure variations in the carotid artery were recorded with a pressure transducer (Mod F-60, Narco Biosystems, Inc., Houston, Texas, USA) connected to a Narcotrace 40 polygraph (Narco Biosystems, Inc., Texas, USA). After the surgical procedure, the hemodynamic variables were allowed to stabilize for 15 min before injection of the test substances. All drugs and the extract were dissolved in 0.9% NaCl (saline). Acetylcholine (ACh; 1.0 μg/kg/i.v.) was chosen as the drug standard curve of physiological mechanisms.
The intravenous injections of HESC (0.01–4.0 mg/kg/i.v.) and acetylcholine did not exceed 0.1 mL over a period of 5 s and were followed by the application of 0.1 mL saline to wash the cannula. In addition, the participation of the cholinergic system was evaluated by injecting atropine (ATR; 1.0 mg/kg).
2.5. Effect of Prolonged Treatment with HESC on the Blood Pressure and Heart Rate of SHR
The MAP and heart rate of SHR were measured using the indirect tail-cuff plethysmography method [30]. According to this protocol, an appropriately sized occlusion cuff was placed around the tail of the animals and connected to a plethysmograph (LE 5001 Pressure Meter, Panlab, Cornella, Spain). A mean of three measurements was obtained for each animal. For blood pressure measurement, the animals were warmed up to 42°C for 5 min in a confinement cage. The animals were first submitted to a period of adaptation for 15 days before the experiments and only SHR with an SBP > 170 mmHg were selected for this study. The animals received a daily oral administration of water (0.5 mL/100 g) or HESC (0.5 g/kg) for 8 weeks. In addition, the weight of the animal and food intake were determined weekly and treatment of the animals was always preceded by blood pressure measurement.
2.6. Effect of Prolonged Treatment with HESC on Vascular Reactivity in SHR
Preparations of the mesenteric artery were obtained [30–32] and ring segments (3–5 mm) of the superior mesenteric artery were placed between stainless steel wires (50 μm in diameter) and immersed in an organ bath chamber (5 mL) containing Krebs nutritive solution (118 mM NaCl, 5 mM KCl, 1.2 mM MgCl2, 1.2 mM NaH2PO4, 15.5 mM NaHCO3, 2 mM CaCl2, and 11 mM glucose, pH 7.4) at 37°C, equilibrated with 5% CO2/95% O2. The presence of endothelial function was confirmed by the capacity of acetylcholine (10 μM) to induce more than 70% of relaxation of vessels precontracted with norepinephrine (NE, 10 μM).
Changes in the isometric tension of the preparations were measured with an isometric force transducer (PowerLab, ADInstruments Pty. Ltd., Sydney, Australia). The preparations were first equilibrated under a tension of 1.0 g and washed at intervals of 10 min. After 60 min of successive washes, cumulative dose-response curves to NE (10−9 to 10−4 M) were obtained for SHR treated with HESC (0.5 g/kg/day).
2.7. In Vitro Effect of HESC on Contractions Induced by Norepinephrine or CaCl2 in the Mesenteric Artery of SHR
Spontaneously hypertensive rats were euthanized and superior mesenteric arterial rings were obtained [30–32] and rings without endothelium were used for this experiment. Thereafter, cumulative concentration-response curves to NE (10−9 to 10−4 M) were constructed in the absence or presence of HESC (0.1, 0.25, and 0.5 mg/mL).
To evaluate the antagonistic action of HESC against calcium, vascular tissue was stabilized with normal Krebs solution; after 30 min, the fluid of the preparation was replaced with Ca2+-free Krebs solution (60 mM K+, nominally Ca2+-free). After 30 min of successive washes, the basal tone was recovered, which permitted obtaining cumulative concentration-response curves to CaCl2 (10−6 to 10−2 M) in the absence or presence of HESC (0.1, 0.25, and 0.5 mg/mL).
The concentration necessary to elicit 50% of the maximum response (EC50) was determined using nonlinear regression analysis. The negative logarithms of the EC50 values (pD2) were used for statistical analysis. In the experiments involving high extracellular K+, Krebs solution containing 60 mM KCl was prepared by replacing an equimolar concentration of NaCl with KCl.
2.8. Statistical Analysis
The results were expressed as the mean ± standard error of the mean (SEM). One-way analysis of variance (ANOVA) followed by the Newman-Keuls posttest was used for multiple comparisons and Student's t-test for comparison of unpaired data. A P value < 0.05 was considered significant. Statistical analysis was performed using the GraphPad Prism 5.0 program.
3. Results
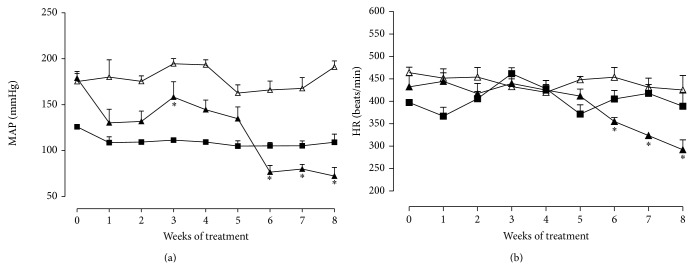
The administration of HESC to anesthetized normotensive rats (baseline MAP: 98.6 ± 0.05 mmHg) caused a dose-dependent reduction in MAP of 11.2 to 58.3 mmHg. The hypotension produced was reversed rapidly, returning to baseline values within 1 to 10 min depending on the dose administered. The administration of isotonic solution (0.9% NaCl, 1 mL/kg) did not cause significant blood pressure changes (Figure 1(a)). The hypotensive effect of the average HESC dose (0.5 mg/kg) on the MAP of anesthetized rats was modified in part by pretreatment with atropine sulfate (1 mg/kg), a dose sufficient to promote total blockade of acetylcholine (1 μg/kg) (Figure 1(b)).
Figure 1.
Effect of intravenous injections of the hydroalcoholic extract of Syzygium cumini leaves (HESC; 0.01 to 4.0 mg/kg) on the blood pressure of Wistar anesthetized rats. (a) Dose-dependent hypotensive effect of HESC. (b) Partial inhibition of the hypotension induced by HESC (0.5 mg/kg) by atropine (ATR). Acetylcholine (ACh, 1.0 μg/kg) was used as an agonist in the production of the hypotensive effect. The columns and vertical bars indicate the mean ± SEM, respectively (n = 5) P < 0.05 ∗ versus isotonic solution; ∗∗ versus ACh 1.0 µg/kg and ∗∗∗ versus HESC 0.5 mg/kg (ANOVA, Newman-Keuls test). MAP: mean arterial pressure.
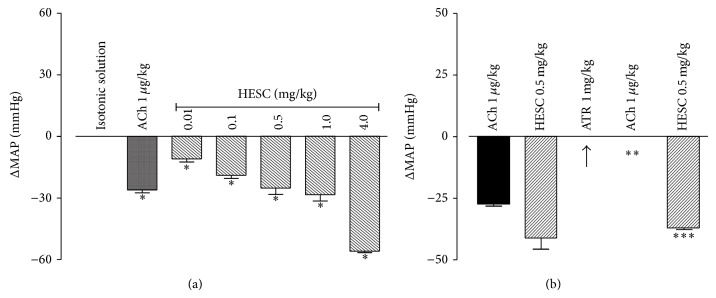
Figure 2 shows the effects of repeated oral administration of HESC (0.5 mg/kg/day) for 8 consecutive weeks on the MAP and heart rate of SHR. Baseline MAP and heart rate were, respectively, 126 ± 2.1 mmHg and 397.5 ± 6.4 bpm in Wistar rats (n = 7) and 175 ± 8.6 mmHg and 473.5 ± 8.4 bpm in SHR (n = 5–7). Oral HESC (0.5 mg/kg) significantly reduced the MAP and heart rate of SHR when compared to the group receiving only vehicle. This finding indicates a time-dependent antihypertensive effect, with this reduction ranging from 25% to 62% between weeks 4 and 8 of treatment (Figure 2(a)). In addition, a reduction in heart rate of 21% to 32% was observed between weeks 6 and 8 of treatment (Figure 2(b)).
Figure 2.
Effect of oral administration of the hydroalcoholic extract of Syzygium cumini leaves (HESC) for 8 weeks on the mean arterial pressure (MAP, a) and heart rate (HR, b) of spontaneously hypertensive rats. SHR control (Δ), SHR-HESC 0.5 g/kg (▲), and Wistar rats (■). Values are the mean ± SEM (n = 6-7). * P < 0.05 versus SHR control.
On the other hand, HESC altered the vascular reactivity of isolated mesenteric arteries from SHR treated for 8 weeks. The maximum effect (E max) of the cumulative NE concentration-response curves was reduced by 40% (Figure 3) compared to the SHR control group, without the observation of changes in EC50 values (1.6 × 10−7 ± 3.0).
Figure 3.
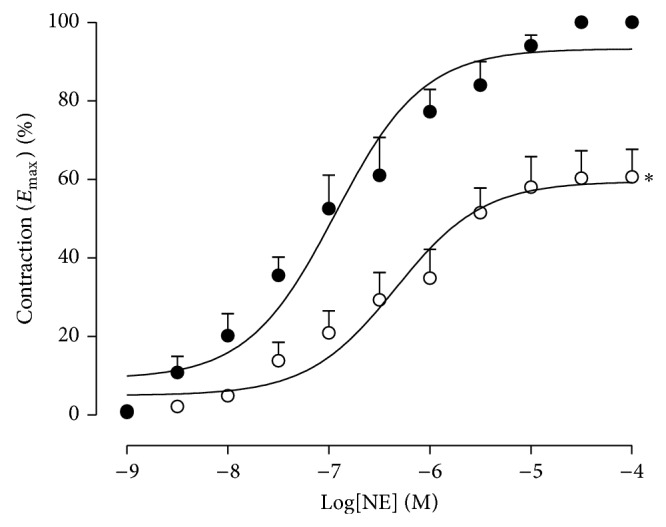
Cumulative dose-response curves to norepinephrine (NE) in isolated mesenteric arterial preparations from spontaneously hypertensive rats treated orally with the hydroalcoholic extract of Syzygium cumini leaves (HESC) (daily for 8 weeks). SHR control (●) and SHR-HESC 0.5 g/kg (о). Values are the mean ± SEM (n = 6-7). * P < 0.05 versus SHR control.
In vitro, HESC at concentrations of 0.1, 0.25, and 0.5 mg/mL reduced the E max value for NE by 14%, 23%, and 78%, respectively. There was a displacement of the NE curves to the right, changing pD2 from 6.5 ± 0.1 to 5.68 ± 0.94, 6.17 ± 3.7, and 6.04 ± 0.2, respectively (Figure 4).
Figure 4.
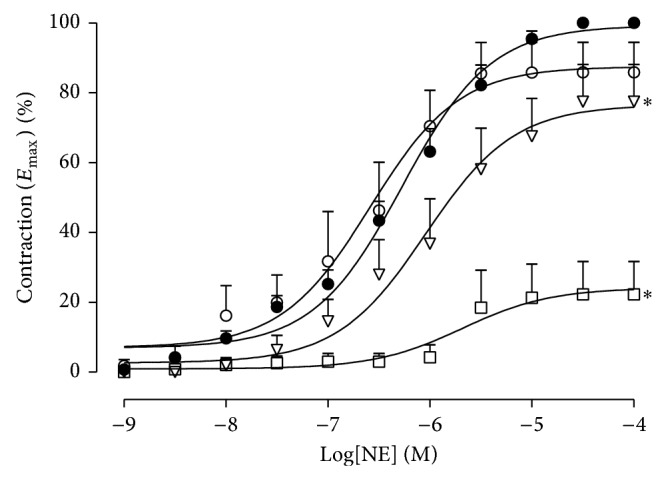
Cumulative dose-response curves to norepinephrine (NE) in isolated endothelium-deprived mesenteric arteries from spontaneously hypertensive rats. Control (●), HESC 0.1 mg/mL (o), HESC 0.25 mg/mL (∇), and HESC 0.5 mg/mL (□). Values are the mean ± SEM (n = 6-7). * P < 0.05 versus control.
In addition, contractions induced by CaCl2 in endothelium-deprived mesenteric arterial rings were reduced in a concentration-dependent manner after incubation with 0.1, 0.25, and 0.5 mg/mL HESC, with a reduction in maximum contraction to 75%, 53%, and 32% (n = 5–7), respectively (Figure 5). These effects were reversed after washing with Krebs solution.
Figure 5.
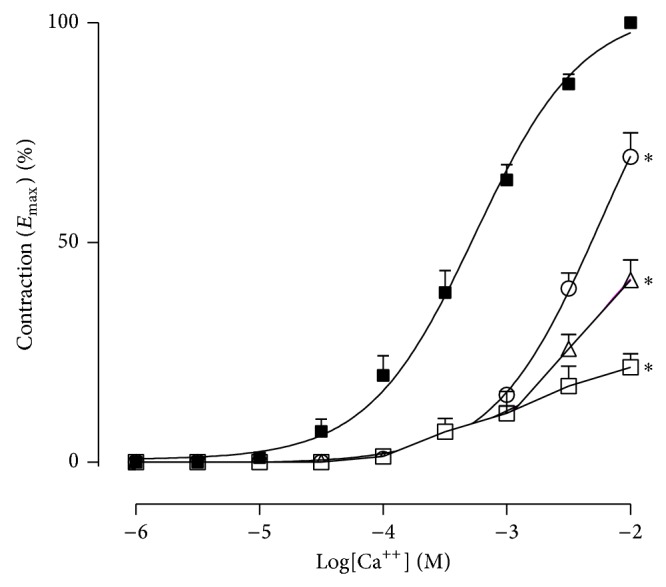
Cumulative dose-response curves to CaCl2 in isolated endothelium-deprived and depolarized mesenteric arteries from spontaneously hypertensive rats. Control (■), HESC 0.1 mg/mL (о), HESC 0.25 mg/mL (Δ), and HESC 0.5 mg/mL (□). Values are the mean ± SEM (n = 6-7). * P < 0.05 versus control.
4. Discussion
The present study showed an antihypertensive and bradycardic effect of Syzygium cumini in SHR. The hypotension promoted by HESC was modified by pretreatment with atropine sulfate, as observed in anesthetized rats, suggesting that muscarinic receptors play a role in the hypotensive mechanism of HESC. However, this effect may also be related in part to a reduction in peripheral vascular resistance as a result of the blockade of Ca2+ channels, as demonstrated in this study in vitro.
The finding that atropine sulfate partially modifies the hypotension produced by HESC (Figure 1(b)) indicates the participation of the cholinergic pathway, suggesting that the hypotensive effect of Syzygium cumini may be related to presence of cholinomimetic-muscarinic components [33, 34] (Figures 2(a) and 2(b)).
SHR were used in the present study which are a good experimental model to investigate factors involved in the pathogenesis of arterial hypertension, since these animals exhibit an increase in vascular reactivity accompanied by hyperresponsiveness to vasoconstrictor agonists [35]. The structural and functional vascular alterations that occur during hypertension are important pathological mechanisms that lead to the increase in blood pressure and are the targets of antihypertensive therapy [36, 37].
In this respect, S. cumini may be a potential candidate for antihypertensive therapy since HESC exerted a substantial blood pressure-lowering effect in SHR submitted to prolonged treatment (Figure 2(a)). The blood pressure reduction induced by the extract may be due in part to a decrease in peripheral vascular resistance, as demonstrated by the effect of HESC on NE-induced E max in superior mesenteric arterial rings of treated SHR. The participation of the sympathetic autonomic nervous system in the development and maintenance of different types of hypertension has been well established in the literature [38, 39].
Vasoconstrictor agents act on the regulation of intracellular calcium concentrations. Norepinephrine elicits a contractile response in vascular smooth muscle (VSM) mediated by the activation of G protein-coupled α-adrenergic receptors [40]. This activation, in turn, induces the formation of inositol triphosphate, corroborating the increase in intracellular calcium concentrations [41–44]. Calcium is therefore the primary regulator of tension in VSM [45, 46]. The maintenance of contraction depends on the influx of Ca2+ from the extracellular space through voltage- and/or receptor-operated calcium channels [47, 48]. Contractile agents such as KCl produce a significant increase in intracellular calcium through the activation of voltage-operated calcium channels. Therefore, contractions in VSM induced by depolarizing solutions (high K+ concentration and nominally Ca2+-free) have been frequently used to investigate the role of calcium in mechanisms that reduce vascular tone [49].
The present results showed that the S. cumini extract reduced the vasoconstrictor activity of calcium in a concentration-dependent manner in endothelium-deprived mesenteric arteries exposed to a depolarizing solution (60 mM KCl, nominally Ca2+-free). This finding indicates that HESC contains components that interfere with the responsiveness of VSM, probably acting on the regulation of intracellular calcium levels through voltage-operated calcium channels. Similar results of inhibition of contractile responses to calcium were found in previous studies with the hydroalcoholic extract of S. cumini by our laboratory in preparation of aortic rings isolated from normotensive rats in the presence of endothelium [27].
Many studies have shown that plant extracts containing flavonoids and/or triterpenes exert antihypertensive effects through the combination of the vasodilatory and antioxidant activities of these classes of compounds [37, 50]. The results of phytochemical screening showed that HESC is rich in these compounds, which may be responsible for the antihypertensive property of the plant.
In conclusion, the in vivo and in vitro results of the present study show that Syzygium cumini reduces the blood pressure and heart rate of SHR. This antihypertensive effect is probably due to inhibition of arterial tone by the blockade of extracellular Ca2+ influx. These effects can be attributed to the presence of flavonoids detected by phytochemical screening. The results may partially explain the traditional use of S. cumini for the treatment of disorders such as hypertension. However, further studies are needed to elucidate the possible antihypertensive mechanism of this medicinal plant.
Acknowledgments
The authors thank the Brazilian funding agencies CAPES, CNPq, and FAPEMA for financial support.
Disclosure
The study is part of the thesis presented by Rachel Melo Ribeiro to the Postgraduate Program in Biotechnology (RENORBIO)/Federal University of Maranhão (UFMA).
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- 1.Go A. S., Mozaffarian D., Roger V. L., et al. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013:127–245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Whelton P. K., He J., Appel L. J., et al. Primary prevention of hypertension: clinical and public health advisory from the National High Blood Pressure Education Program. Journal of the American Medical Association. 2002;288(15):1882–1888. doi: 10.1001/jama.288.15.1882. [DOI] [PubMed] [Google Scholar]
- 3.Chobanian A. V., Bakris G. L., Black H. R., et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42(6):1206–1252. doi: 10.1161/01.hyp.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 4.Nahas R. Complementary and alternative medicine approaches to blood pressure reduction: an evidence-based review. Canadian Family Physician. 2008;54(11):1529–1533. [PMC free article] [PubMed] [Google Scholar]
- 5.Morton J. F. The Jambolan (Syzygium cumini Skeels) its food, medicinal, ornamental and other uses. Proceedings of the Florida State Horticultural Society. 1963;76:328–338. [Google Scholar]
- 6.Pepato M. T., Mori D. M., Baviera A. M., Harami J. B., Vendramini R. C., Brunetti I. L. Fruit of the jambolan tree (Eugenia jambolana Lam.) and experimental diabetes. Journal of Ethnopharmacology. 2005;96(1-2):43–48. doi: 10.1016/j.jep.2004.07.029. [DOI] [PubMed] [Google Scholar]
- 7.Migliato K. F., Baby A. R., Zague V., et al. Pharmacological action of Syxygium cumini (L.) skeels. Acta Farmaceutica Bonaerense. 2006;25(2):310–314. [Google Scholar]
- 8.Dickel M. L., Rates S. M. K., Ritter M. R. Plants popularly used for loosing weight purposes in Porto Alegre, South Brazil. Journal of Ethnopharmacology. 2007;109(1):60–71. doi: 10.1016/j.jep.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 9.Abbas S. Q., Mushtaq S. Addition to mycoflora of Syzygium cumini from Pakistan. Mycopath. 2008;6(1-2):57–61. [Google Scholar]
- 10.Achrekar S., Kaklij G. S., Pote M. S., Kelkar S. M. Hypoglicemic activity of Eugenia jambolana and Ficus benglensis: mechanism of action. In Vivo. 1991;5(2):143–147. [PubMed] [Google Scholar]
- 11.Vikrant V., Grover J. K., Tandon N., Rathi S. S., Gupta N. Treatment with extracts of Momordica charantia and Eugenia jambolana prevents hyperglycemia and hyperinsulinemia in fructose fed rats. Journal of Ethnopharmacology. 2001;76(2):201–206. doi: 10.1016/s0378-8741(01)00218-5. [DOI] [PubMed] [Google Scholar]
- 12.Grover J. K., Yadav S., Vats V. Medicinal plants of India with anti-diabetic potential. Journal of Ethnopharmacology. 2002;81(1):81–100. doi: 10.1016/S0378-8741(02)00059-4. [DOI] [PubMed] [Google Scholar]
- 13.Ravi K., Sivagnanam K., Subramanian S. Anti-diabetic activity of Eugenia jambolana seed kernels on streptozotocin-induced diabetic rats. Journal of Medicinal Food. 2004;7(2):187–191. doi: 10.1089/1096620041224067. [DOI] [PubMed] [Google Scholar]
- 14.Sridhar S. B., Sheetal U. D., Pai M. R. S. M., Shastri M. S. Preclinical evaluation of the antidiabetic effect of Eugenia jambolana seed powder in streptozotocin-diabetic rats. Brazilian Journal of Medical and Biological Research. 2005;38(3):463–468. doi: 10.1590/s0100-879x2005000300018. [DOI] [PubMed] [Google Scholar]
- 15.Villaseñor I. M., Lamadrid M. R. Comparative anti-hyperglycemic potentials of medicinal plants. Journal of Ethnopharmacology. 2006;104(1-2):129–131. doi: 10.1016/j.jep.2005.08.067. [DOI] [PubMed] [Google Scholar]
- 16.Kumar A. R., Ponnusamy S., Ravindran R., Zinjarde S., Bhargava S. Evaluation of traditional Indian antidiabetic medicinal plants for human pancreatic amylase inhibitory effect in vitro . Evidence-based Complementary and Alternative Medicine. 2011;2011:10. doi: 10.1155/2011/515647.515647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Joshi B. N., Bhat M., Zinjarde S. S., Bhargava S. Y., Kumar A. R. Antidiabetic Indian plants: a good source of potent amylase inhibitors. Evidence-Based Complementary and Alternative Medicine. 2011;2011:6. doi: 10.1093/ecam/nen040.810207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sharma B., Tanwar R. S., Nasir A., Prabhu K. M. Antihyperlipidemic effect of active principle isolated from seed of Eugenia jambolana on alloxan-induced diabetic rabbits. Journal of Medicinal Food. 2011;14(4):353–359. doi: 10.1089/jmf.2010.1227. [DOI] [PubMed] [Google Scholar]
- 19.Sharma S. B., Rajpoot R., Nasir A., Prabhu K. M., Murthy P. S. Ameliorative effect of active principle isolated from seeds of Eugenia jambolana on carbohydrate metabolism in experimental diabetes. Evidence-Based Complementary and Alternative Medicine. 2011;2011:9. doi: 10.1093/ecam/nep233.789871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhi P. R., Liang L. Z., Yi M. L. Evaluation of the antioxidant activity of Syzygium cumini leaves. Molecules. 2008;13(10):2545–2556. doi: 10.3390/molecules13102545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tanwar R. S., Sharma S. B., Singh U. R., Prabhu K. M. Antiatherosclerotic potential of active principle isolated from Eugenia jambolana in streptozotocin-induced diabetic rats. Evidence-Based Complementary and Alternative Medicine. 2011;2011:9. doi: 10.1155/2011/127641.127641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Atale N., Chakraborty M., Mohanty S., et al. Cardioprotective role of Syzygium cumini against glucose-induced oxidative stress in H9C2 cardiac myocytes. Cardiovascular Toxicology. 2013;13(3):278–289. doi: 10.1007/s12012-013-9207-1. [DOI] [PubMed] [Google Scholar]
- 23.Shukla S. K., Sharma S. B., Singh U. R., et al. Eugenia jambolana pretreatment prevents isoproterenol-induced myocardial damage in rats: evidence from biochemical, molecular, and histopathological studies. Journal of Medicinal Food. 2014;17(2):244–253. doi: 10.1089/jmf.2013.2795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Atale N., Gupta K., Rani V. Protective effect of Syzygium cumini against pesticide-induced cardiotoxicity. Environmental Science and Pollution Research. 2014;21(13):7956–7972. doi: 10.1007/s11356-014-2684-3. [DOI] [PubMed] [Google Scholar]
- 25.Cirqueira R. T., Alves M. J. Q. F. Efeitos hipotensivo e diurético dos extratos aquosos de pitanga (Eugenia uniflora L.) e jambolão (Eugenia jambolana Lam.) em ratos normotensos anestesiados. Revista Brasileira de Plantas Medicinais. 2005;7:86–91. [Google Scholar]
- 26.Silva-Netto C. R., Lopes R. A., Pozetti G. L. Effects of extract of dried leaves of Jambolao (Syzygium Jambolanum) on renal excretion of water, sodium and potassium in rats. Preliminary results. Revista da Faculdade de Odontologia de Ribeirao Preto. 1986;23(2):213–215. [PubMed] [Google Scholar]
- 27.Abreu I. C., Silva S. N., Ribeiro R. M., et al. Efeito dos extratos de Jatropha gossypiifolia L., Passiflora edulis Sims, Syzygium jambolanum D.C. na disponibilidade de íons cálcio. Revista de Ciências da Saúde. 2002;4:41–46. [Google Scholar]
- 28.Silva S. N., Abreu I. C., Silva G. F. C., et al. The toxicity evaluation of Syzygium cumini leaves in rodents. Revista Brasileira de Farmacognosia. 2012;22:102–108. [Google Scholar]
- 29.Ribeiro R. M., Borges A. C. R., Neto V. F. P., et al. Formulação de composição farmacêutica de liofilizado de extrato e/ou fração ativas de partes aéreas de syzygium cumini, e seu uso na redução da pressão arterial. Brazil Patent PI1101652-3A2, 2013.
- 30.Borges A. C. R., Feres T., Vianna L. M., Paiva T. B. Recovery of impaired K+ channels in mesenteric arteries from spontaneously hypertensive rats by prolonged treatment with cholecalciferol. British Journal of Pharmacology. 1999;127(3):772–778. doi: 10.1038/sj.bjp.0702581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Borges A. C. R., Feres T., Vianna L. M., Paiva T. B. Effect of cholecalciferol treatment on the relaxant responses of SHR arteries to acetylcholine. Hypertension. 1999;34(4):897–901. doi: 10.1161/01.hyp.34.4.897. [DOI] [PubMed] [Google Scholar]
- 32.Abreu I. C., Marinho A. S. S., Paes A. M. A., et al. Hypotensive and vasorelaxant effects of ethanolic extract from Jatropha gossypiifolia L. in rats. Fitoterapia. 2003;74(7-8):650–657. doi: 10.1016/j.fitote.2003.07.002. [DOI] [PubMed] [Google Scholar]
- 33.Amaechina F. C., Omogbai E. K. Hypotensive effect of aqueous extract of the leaves of Phyllanthus amarus Schum and Thonn (Euphorbiaceae) Acta Poloniae Pharmaceutica-Drug Research. 2007;64(6):547–552. [PubMed] [Google Scholar]
- 34.Assaidi A., Legssyer A., Berrichi A., et al. Hypotensive property of Chenopodium ambrosioides in anesthetized normotensive rats. Journal of Complementary and Integrative Medicine. 2014;11(1):1–7. doi: 10.1515/jcim-2013-0045. [DOI] [PubMed] [Google Scholar]
- 35.Schlegel P. A., Monney M., Brunner H. R. Isolated perfused mesenteric arteries of hypertensive and normotensive rats, response to noradrenaline, lysine vasopressin and angiotensin II. Clinical and Experimental Hypertension Part A. 1985;7(11):1583–1596. doi: 10.3109/10641968509073611. [DOI] [PubMed] [Google Scholar]
- 36.Oh K.-S., Han W., Wang M.-H., Lee B. H. The effects of chronic treatment with Morus bombycis KOIDZUMI in spontaneously hypertensive rats. Biological and Pharmaceutical Bulletin. 2007;30(7):1278–1283. doi: 10.1248/bpb.30.1278. [DOI] [PubMed] [Google Scholar]
- 37.Oh K. S., Ryu S. Y., Oh B. K., Seo H. W., Kim Y. S., Lee B. H. Antihypertensive, vasorelaxant, and antioxidant effect of root bark of Ulmus macrocarpa. Biological and Pharmaceutical Bulletin. 2008;31(11):2090–2096. doi: 10.1248/bpb.31.2090. [DOI] [PubMed] [Google Scholar]
- 38.Piascik M. T., Soltis E. E., Piascik M. M., Macmillan L. B. α-Adrenoceptors and vascular regulation: molecular, pharmacologic and clinical correlates. Pharmacology and Therapeutics. 1996;72(3):215–241. doi: 10.1016/s0163-7258(96)00117-9. [DOI] [PubMed] [Google Scholar]
- 39.Colombo F. M., Krieger E. M. Sistema nervoso simpático e hipertensão arterial. Revista Brasileira de Hipertensão. 2000;3:86–89. [Google Scholar]
- 40.Perez-Vizcaino F., Cogolludo A. L., Villamor E., Tamargo J. Role of K+ channel opening and stimulation of cyclic GMP in the vasorelaxant effects of nicorandil in isolated piglet pulmonary and mesenteric arteries: relative efficacy and interactions between both pathways. British Journal of Pharmacology. 1998;123(5):781–1022. doi: 10.1038/sj.bjp.0701693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Leijten P. A., Van Breemen C. The effects of caffeine on the noradrenaline-sensitive calcium store in rabbit aorta. Journal of Physiology. 1984;357:327–339. doi: 10.1113/jphysiol.1984.sp015502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Marín J., Encabo A., Briones A., Cohen E.-C. G., Alonso M. J. Mechanisms involved in the cellular calcium homeostasis in vascular smooth muscle: calcium pumps. Life Sciences. 1999;64(5):279–303. doi: 10.1016/s0024-3205(98)00393-2. [DOI] [PubMed] [Google Scholar]
- 43.Zhao G., Neeb Z. P., Dennis Leo M., et al. Type 1 IP3 receptors activate BKCa channels via local molecular coupling in arterial smooth muscle cells. Journal of General Physiology. 2010;136(3):283–291. doi: 10.1085/jgp.201010453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Docherty J. R. Subtypes of functional α 1-adrenoceptor. Cellular and Molecular Life Sciences. 2010;67(3):405–417. doi: 10.1007/s00018-009-0174-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Karaki H., Ozaki H., Hori M., et al. Calcium movements, distribution, and functions in smooth muscle. Pharmacological Reviews. 1997;49(2):157–230. [PubMed] [Google Scholar]
- 46.Gurney A. M. Mechanisms of drug-induced vasodilation. Journal of Pharmacy and Pharmacology. 1994;46(4):242–251. doi: 10.1111/j.2042-7158.1994.tb03789.x. [DOI] [PubMed] [Google Scholar]
- 47.Karaki H., Weiss G. B. Calcium release in smooth muscle. Life Sciences. 1988;42(2):111–122. doi: 10.1016/0024-3205(88)90674-1. [DOI] [PubMed] [Google Scholar]
- 48.Nelson M. T., Patlak J. B., Worley J. F., Standen N. B. Calcium channels, potassium channels, and voltage dependence of arterial smooth muscle tone. The American Journal of Physiology. 1990;259:3–18. doi: 10.1152/ajpcell.1990.259.1.C3. [DOI] [PubMed] [Google Scholar]
- 49.Adaramoye O. A., Anjos R. M., Almeida M. M., et al. Hypotensive and endothelium-independent vasorelaxant effects of methanolic extract from Curcuma longa L. in rats. Journal of Ethnopharmacology. 2009;124(3):457–462. doi: 10.1016/j.jep.2009.05.021. [DOI] [PubMed] [Google Scholar]
- 50.Curin Y., Andriantsitohaina R. Polyphenols as potential therapeutical agents against cardiovascular diseases. Pharmacological Reports. 2005;57:97–107. [PubMed] [Google Scholar]