Abstract
Background:
Oral and maxillofacial surgeons are concern about the intraoperative bleeding because blood supply to face is very generous. Increased blood loss may lead to the need for transfusion of blood and blood products and hence patients are exposed to the risks associated with it. Hence, this study was undertaken to compare whether there is any significant difference in blood loss, surgical field and duration of surgery in patients undergoing maxillofacial surgeries with and without hypotensive anesthesia.
Materials and Methods:
The study was conducted on patients undergoing various maxillofacial surgeries. The patients were randomly divided into two groups, the study group and the control group. In the study group patients, induced hypotension was used in order to maintain systolic pressure of 80-90 mm Hg. In the control group patients, normotensive anesthesia was used. Estimation of blood loss (EBS), quality of the surgical field and duration of surgery was calculated for both groups in three types of surgical procedures. Statistical analysis was performed by using two-tailed Pearson correlation test.
Results:
EBS was found to be significantly less in all the surgical procedures carried out under hypotensive anesthesia (P < 0.05). The quality of the surgical field was better in cases with induced hypotension, but there was no significant difference in duration of the procedures with and without induced hypotension.
Conclusion:
Our study shows that hypotensive anesthesia can be safely used in almost all maxillofacial surgical procedures with reduced blood loss and improved surgical field.
Keywords: Blood loss, hypotensive anesthesia, maxillofacial surgery
Introduction
Blood supply to the face is very generous. An oral and maxillofacial surgeon must be concerned about the intraoperative bleeding. Many of the maxillofacial cases are technically demanding, and visibility may be limited due to excessive bleeding. Increased blood loss may lead to the need for transfusion of blood and blood products and hence patients are exposed to the risks associated with it.
Intraoperative bleeding may be reduced most effectively by induced systemic hypotension. Controlled hypotension is defined as a reduction of the systolic blood pressure to 80-90 mm Hg, a reduction of mean arterial pressure (MAP) to 50-65 mm Hg or a 30% reduction of baseline MAP (diastolic pressure +1/3 pulse pressure).1
There are several important advantages of using intentional hypotensive anesthetic technique during the maxillofacial surgeries like reduction in blood loss hence reduction in blood transfusion rate, improvement in the surgical field and reduction of the duration of surgery. Schaberg et al.2 and Chan et al.3 noted 40% and 41% reduction in red cell loss respectively during hypotensive anesthesia technique. There was also pronounced improvement in the quality of surgical fields in their cases.
Along with the benefits, hypotensive anesthesia is also associated with risks like hypoperfusion of vital organs like the central nervous system, heart, liver and kidney. But the margin of safety is greater during well-managed controlled hypotension because blood flow is preserved due to compensatory mechanisms.4 Safety is also dependent on the way in which hypotensive agents are used. Systemic vasodilators, ganglionic blocking agents and the position of the patient are used to alter tissue perfusion.
Selection of patients, close anesthetic monitoring during surgery and good communication between the surgeon and anesthesiologist are important to bring about the benefits of hypotensive anesthesia in maxillofacial cases.
The purpose of this study was to assess the percentage change in reduction of blood loss, quality of the surgical field and duration of surgery when maxillofacial cases are done with and without hypotensive anesthesia.
Aims and objectives
The aims and objectives of the study are to compare the two anesthetic techniques (hypotensive and normotensive) for estimation of blood loss (EBL), quality of the surgical field and duration of surgery in maxillofacial procedures.
Materials and Methods
The study has been carried out under the Department of Oral and Maxillofacial Surgery after taking the approval from the institutional ethics committee. The study was conducted on 14 patients of unilateral cleft lip repair, 10 patients undergoing secondary alveolar bone grafting (SABG) and 6 patients undergoing Lefort I osteotomy.
The following criteria for inclusion in the study were considered, and all patients were class I ASA.
Procedure
Patient and parental consent to participate in the study was taken. Preoperative investigations done were electrocardiogram (ECG), complete blood count, blood group analyses, hematocrit, serum urea, serum creatinine, alkaline phosphatase and bilirubin. The patients were stratified and blocked according to their proposed surgery and then randomly assigned to either control or study group. The patients baseline blood pressure was determined in the ward by average of three separate preoperative blood pressure measurements determined by the auscultation of Korotkoff sounds. Premedication with injection pethidine 1 mg/kg body weight i.v. was given. All patients were given standardized anesthetic technique consisting of 3.5-5 mg/kg sodium thiopentone, 1.5 mg/kg of succinylchloine after intubation of the patient. General anesthesia maintained by 66% nitrous oxide in 33% oxygen and injection pancuronium 0.1 mg/kg which is repeated as per need. Surgery was performed using the same anesthesia and surgical protocols, and all operations were performed by the same surgical team; hence, differences in results due to variations in surgical technique were believed to be minimal. Intraoperative monitoring consists of ECG and blood pressure was measured with non-invasive blood pressure monitor. To induce hypotension 0.5-2% halothane nitroglycerin 25 mg (in 1 ampule) diluted with 500 ml of 5% dextrose delivered using a syringe pump with a titrated dosage of 0.5-5.4 mg/kg/min in order to maintain systolic pressure of 80-90 mm Hg.
Rating of the surgical field was done every 15 min using Fromme ordinal scale for assessment of the surgical field.5 The numerical values were then averaged. The duration of the procedure was calculated from the time, when local anesthetic solution was injected, to the time, when the oral mucosal wound was closed. The intra-operative EBL for each procedure was calculated by weighing the surgical gauze swabs and measuring the contents of the suction bottle (with adjustment made for the amount of saline irrigation used).6 The hemoglobin level and hematocrit value (packed-cell volume) were obtained on the pre-operative day and first post-operative day.
Results
The total number of patients included in the study was 30. Of them 14 patients were in unilateral cleft lip (7 in study and 7 in control), 10 were in SABG (5 in study and 5 in control) and 6 patients were in Lefort I osteotomy (3 in study and 3 in control). No patient was excluded because of any contraindication to hypotensive anesthesia.
All data were analyzed using the Statistical Package for Social Science (Windows version 17.0; SPSS Inc., Chicago, United States). The two-tailed Pearson correlation test was used to assess the bivariate correlation between EBL, surgical field and the duration of surgery. A probability level of P < 0.05 was accepted as being significant.
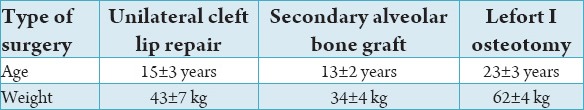
The mean and standard deviation of EBL for all the three surgical procedures in both hypotensive and normotensive groups are given in Table 1. EBL was found to be significantly less in cleft lip repair, SABG and Lefort I surgical procedures that were carried out under hypotensive anesthesia. Paired t-test was done between the groups. P value was significant in all the groups.
Table 1.
EBL in normotensive and hypotensive anesthesia. In cleft lip, Lefort I and SABG patients.
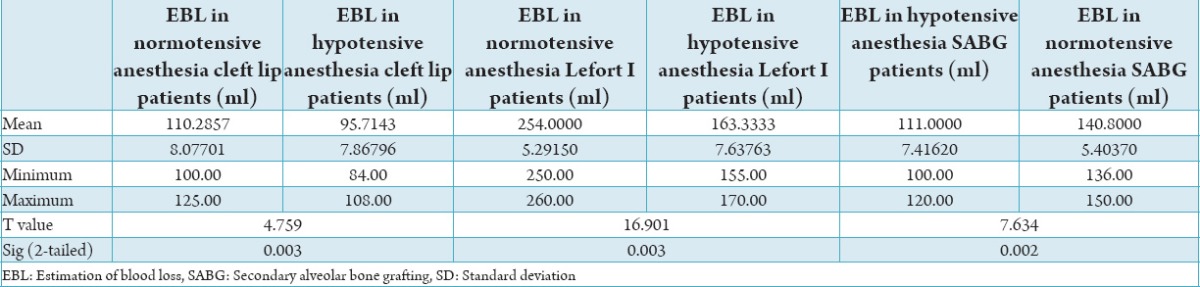
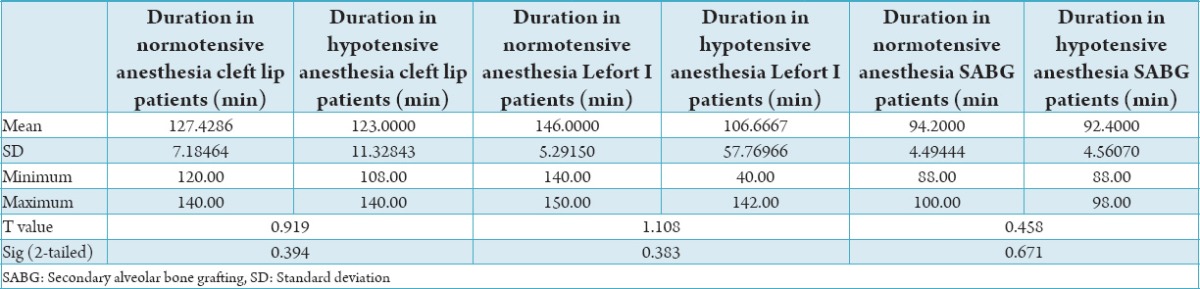
The mean and standard deviation of the surgical field and duration of surgery for all the three surgical procedures in both hypotensive and normotensive groups are given in Tables 2 and 3, respectively. The quality of surgical field was also better in all the procedures carried out under induced hypotension (P < 0.05), but there was no significant difference in duration of the procedures with and without induced hypotension (P > 0.05).
Table 2.
SF in normotensive and hypotensive anesthesia in cleft lip, Lefort I and SABG patients.

Table 3.
Duration of surgery in normotensive and hypotensive anesthesia in cleft lip, Lefort I and SABG patients.
Discussion
Deliberate or controlled or induced hypotensive anesthesia is widely used in neuro, plastic, head and neck, orthopedic and oncological surgeries. Thus, leading to more accurate surgery and decreased operative time. Though widely recommended, due to lack of trained anesthetists and invasive monitoring equipment it is not universally practiced.3 Face is highly vascular, but many maxillofacial surgeries have been done under normotension in most dental colleges and hospitals. We undertook this study to compare the relative advantages of this measure.
Our study is a controlled trial that randomized patients into different surgical groups to test the effect of induced hypotensive general anesthesia on blood loss, quality of surgical field and operating time. The results of our study are comparable to some international studies. The MAP in our hypotensive group was 58 mm Hg which produced good operating condition for the surgeons. Schindler et al.7 induced moderate hypotension when they performed maxillofacial surgery and found that, with the exception of the first 30 min of the operation, an average systolic arterial pressure of 89 mm Hg and a MAP of 65 mm Hg produced satisfactory operating conditions.
One might question the use and accuracy of noninvasive blood pressure monitor for the study of this nature. Certainly, the “gold standard” of blood pressure measurement is an invasive intra-arterial catheter transducer system. They are, however not without risk, albeit small. If are more volatile hypotensive agents such as sodium nitroprusside are used, invasive monitoring becomes mandatory, as accuracy is synonymous with safety. Induced hypotension can be achieved by different pharmacologic agents either primarily or in combination with other anesthetic agents. Deliberate hypotension can be well-tolerated by most patients to levels of MAP as low as 35-40 mm Hg. However, some patients may experience significant end-organ hypoperfusion at a MAP in the range of 50-55 mm Hg.
Hypotensive anesthesia has been shown to be relatively safe technique. MAP of 50-60 mm Hg have been shown to be safe even in a group of the elderly patient (mean age 57) by study conducted by Chan et al.3 in 1980. Contraindication to the use of induced hypotension anesthesia is often related to pre-existing poor organ perfusion and oxygen delivery, because of lack of controlled study as to what constitutes an absolute contraindication to deliberate hypotension. Under most circumstances the following be regarded as contraindication to deliberate reduction of blood pressure: Fixed cardiac output (e.g. Aortic stenosis, obstructive and restrictive cardiomyopathy, left ventricular failure), hypertension that is inadequately treated or associated with left ventricular hypertrophy, angina; myocardial infarction within previous 6 months, carotid artery stenosis; previous cerebro vascular accident, hypovolemia and pregnancy.8 Improved and meticulous monitoring have reduced the relative risks of systematically reducing MAP. But in our study there were no major complications. Only one patient each in SABG and Lefort I surgery of normotensive group received blood transfusion.
The reduction of blood loss in all the three surgical groups of hypotensive anesthesia was statistically significant. The mean EBL in cleft lip surgery was 110.2857, 95.7143 (control) (study). The mean of EBL in secondary alveolar bone graft surgery was 111.00 ml, 140.80 ml (control) (study). The mean EBL in Lefort I surgery was 254.00 ml, 163.33 ml (control) (study). The mean blood loss in the study conducted by Samman et al.9 was 600 ml. Hypotensive general anesthesia brought about a 40% reduction in the volume of whole blood lost and a 44% reduction in the volume of red blood cells lost, compared with when normotensive general anesthesia was used in studies of Schaberg et al.2 and Chan et al.3
The quality of the surgical field was assessed by the operating surgeons every 15 min using Fromme ordinal scale for assessment of the surgical field. The numerical values were then averaged. Formme’s ordinal scale as a tool of surgical field assessment is a reasonable attempt to objectively standardize this difficulty to assess subjective parameter. One can foresee some potential bias, dependent on the difficulty of the surgery, despite the effort to block and stratify surgical cases. In our study though there was a decrease in the duration of surgery in hypotensive group, but it was not statistically significant. The same observation was seen in the study conducted by Praveen et al.10
Many studies, including our study, however, have confirmed the positive role of hypotensive general anesthesia in providing a clear operative field, decreasing operating time, and hence obviating the need for blood transfusion.11-14 Although Enlund et al.15 found that induced hypotension may decrease the bleeding rate in orthognathic surgery, they concluded that it is not a crucial factor.
Although previous conflicting studies question the efficiency of hypotensive anesthesia in reducing blood loss, decreasing surgical time, improving surgical field, it appears that even in studies that refute the technique, there continuous to be a trend toward reduced blood loss in hypotensive anesthesia.
Summary and Conclusion
Improved surgical field or “bloodless field” is the desired end point for any surgeon. A reduction of blood loss is advantage in terms hemodynamic and metabolic stability, transfusion requirement and infection transmission. Induced hypotension is one of the most effective ways towards achieving the above goals. Our research efforts show that there is a significant reduction in blood loss and improvement to the surgical field, but no significant reduction in duration of surgery. Induced hypotension, continues to be justifiable and useful technique in selected cases.
Footnotes
Source of Support: Nil
Conflict of Interest: None
References
- 1.Degoute CS. Controlled hypotension: Aguide to drug choice. Drugs. 2007;67(7):1053–76.1. doi: 10.2165/00003495-200767070-00007. [DOI] [PubMed] [Google Scholar]
- 2.Schaberg SJ, Kelly JF, Terry BC, Posner MA, Anderson EF. Blood loss and hypotensive anesthesia in oral-facial corrective surgery. JOral Surg. 1976;34(2):147–56. [PubMed] [Google Scholar]
- 3.Chan W, Smith DE, Ware WH. Effects of hypotensive anesthesia in anterior maxillary osteotomy. JOral Surg. 1980;38(7):504–8. [PubMed] [Google Scholar]
- 4.Rollason WN, Hough JM. Are-examination of some electrocardiographic studies during hypotensive anaesthesia. The effect of rate of fall of blood pressure. Br J Anaesth. 1969;41(11):985–6. doi: 10.1093/bja/41.11.985. [DOI] [PubMed] [Google Scholar]
- 5.Choi WS, Samman N. Risks and benefits of deliberate hypotension in anaesthesia: Asystematic review. Int J Oral Maxillofac Surg. 2008;37(8):687–703. doi: 10.1016/j.ijom.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 6.Yu CN, Chow TK, Kwan AS, Wong SL, Fung SC. Intra-operative blood loss and operating time in orthognathic surgery using induced hypotensive general anaesthesia: Prospective study. Hong Kong Med J. 2000;6(3):307–11. [PubMed] [Google Scholar]
- 7.Schindler I, Andel H, Leber J, Kimla T. Moderate induced hypotension provides satisfactory operating conditions in maxillofacial surgery. Acta Anaesthesiol Scand. 1994;38(4):384–7. doi: 10.1111/j.1399-6576.1994.tb03912.x. [DOI] [PubMed] [Google Scholar]
- 8.Rodrigo C. Induced hypotension during anesthesia with special reference to orthognathic surgery. Anesth Prog. 1995;42(2):41–58. [PMC free article] [PubMed] [Google Scholar]
- 9.Samman N, Cheung LK, Tong AC, Tideman H. Blood loss and transfusion requirements in orthognatic surgery. J Oral Maxillofac Surg. 1996;54(1):21–4. doi: 10.1016/s0278-2391(96)90295-5. [DOI] [PubMed] [Google Scholar]
- 10.Praveen K, Narayanan V, Muthusekhar MR, Baig MF. Hypotensive anaesthesia and blood loss in orthognathic surgery: Aclinical study. Br J Oral Maxillofac Surg. 2001;39(2):138–40. doi: 10.1054/bjom.2000.0593. [DOI] [PubMed] [Google Scholar]
- 11.Gallagher DM, Milliken RA. Induced hypotension for orthognathic surgery. JOral Surg. 1979;37(1):47–51. [PubMed] [Google Scholar]
- 12.Tobias JD. Nicardipine for controlled hypotension during orthognathic surgery. Plast Reconstr Surg. 1997;99(6):1539–43. [PubMed] [Google Scholar]
- 13.Rohling RG, Haers PE, Zimmermann AP, Schanz U, Marquetand R, Sailer HF. Multimodal strategy for reduction of homologous transfusions in cranio-maxillofacial surgery. Int J Oral Maxillofac Surg. 1999;28(2):137–42. [PubMed] [Google Scholar]
- 14.Precious DS, Splinter W, Bosco D. Induced hypotensive anesthesia for adolescent orthognathic surgery patients. J Oral Maxillofac Surg. 1996;54(6):680–3. doi: 10.1016/s0278-2391(96)90679-5. [DOI] [PubMed] [Google Scholar]
- 15.Enlund MG, Ahlstedt BL, Andersson LG, Krekmanov LI. Induced hypotension may influence blood loss in orthognathic surgery, but it is not crucial. Scand J Plast Reconstr Surg Hand Surg. 1997;31(4):311–7. doi: 10.3109/02844319709008977. [DOI] [PubMed] [Google Scholar]


