Abstract
Background:
Low health literacy is one among many reasons why preventable diseases remain so common and why people often do not adopt healthy practices. It is important to detect patients with inadequate oral health literacy (OHL) and to improve the level of communication between the provider and the patient. This study was aimed to determine the relationship between OHL with selected socio-demographic variables and oral health status among adults in Virajpet, Karnataka, India.
Materials and Methods:
A convenience sample of 187 subjects from the out-patient department of Coorg-Institute of Dental Sciences Hospital administered the Rapid Estimate of Adult Literacy in Dentistry (REALD-30). The demographic variables and the oral health status were recorded for every participant using World Health Organization oral health survey proforma (1997). Data were analyzed using t-tests, analysis of variance, correlations and Kruskal–Wallis test.
Results:
The associations between REALD-30 scores and gender, age, and ethnicity were not statistically significant. Significant associations were found between REALD scores and the following oral-health related variables: Temperomandibular joint problems, prevalence of prosthetic need, CPI (Community Periodontal Index) and loss of attachment scores. REALD-30 scores were negatively correlated with DMFT (Decayed, Missing and Filled Teeth) scores and DAI (Dental Aesthetic Index) scores.
Conclusion:
OHL was not associated with sex, age, or ethnicity in this sample of the Virajpet population. OHL was associated with oral health status. Lower OHL was associated with poorer oral health status. OHL instruments can be considered to be included as screening tools to identifying individuals or groups with poor oral health outcomes.
Keywords: Dental caries, patient-provider communication, rapid estimate of adult literacy in dentistry
Introduction
Health literacy has been recognized as one of the determinants of staying healthy, recovering from illness and enhancing health-related quality-of-life in individuals. Health literacy may improve knowledge and skill of the members of the society that in turn acts an instrument to address health inequalities.
Healthy people 2010 defined health literacy as ‘‘The degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.”
There are many barriers to utilization of health care and to the adoption of healthy oral health practices. These range from financial issues, lack of access to providers and adequate preventive care to a spectrum of biological, behavioral, community and cultural factors. Low health literacy is also one among these factors.1
Although healthcare professionals generally assume that the health explanations and instructions given to patients and families are readily understood, in reality these instructions are frequently misunderstood, sometimes resulting in serious errors.2 A common reason for misunderstanding health instructions may be the patient’s low health literacy skills.
In the oral health context, literacy can be considered as the skills necessary for people to understand the causes of poor oral health, to learn and adopt fundamental aspects of positive oral self-care behaviors, to communicate with oral health care providers, to place their names on dental treatment waiting lists or organize appointments, to find their way to the dental clinic, to fill out the necessary forms and to comply with any required regimes, including follow-up appointments and compliance with prescribed medication.3 Lack of oral health literacy (OHL) can create a significant barrier to prevent oral disease and to promote oral health.
Previous literatures show a low correlation between years of schooling and literacy, with literacy being several grades below the attained educational level. Thus educational attainment, although easy to access, can be a poor proxy for literacy and does not accurately reflect an individual’s ability to understand and use written information.4
Better health literacy develops competencies of the individual to assimilate, comprehend and adapt to healthy practices and reduce risk behaviors. The level of communication between the provider and the patient both in the clinical setting, as well as community level, can be improved by early detection of patients with inadequate OHL. At the community level, it is important in order to appropriately design educational materials and community intervention programs that coincide with the literacy level of the target population.1
Specifically, the objectives were:
To determine the relationship between OHL, as assessed by Rapid Estimate of Adult Literacy in Dentistry (REALD-30), and selected socio-demographic variables that include gender, age, and ethnicity
To determine the association between OHL and oral health status as assessed by the World Health Organization (WHO) Oral Health Assessment Proforma 1997.5
Materials and Methods
A cross-sectional study was conducted from March 2011 to August 2011. The sample size was estimated based on the prevalence of dental caries, one of the response variables. A pilot study conducted on a sample of 50 subjects revealed the prevalence of dental caries as 85.8%. Based on this, the sample size was estimated to be 187 subjects.
A convenience sampling was done wherein the study subjects were recruited from the waiting area of the main reception unit of the Coorg Institute of Dental Sciences, Virajpet. The sample comprised of patients and their bystanders attending the out-patient department of the dental hospital at Coorg Institute of Dental Sciences, Virajpet. The subjects had to be, at least 18 years of age, be able to understand and communicate in English, without cognitive impairment, without vision or hearing problems, without obvious signs of drug or alcohol intoxication.
Informed consent was obtained from all the participants. Individuals who refused to give consent were excluded from the study. The research protocol was approved by the Institutional Review Board of Coorg Institute of Dental Sciences.
The subjects who consented consented to participate underwent a clinical oral examination by a calibrated examiner. To record the various components of oral health status, the WHO Oral Health Survey Proforma (1997) was used.
Socio-demographic details as required by the study objectives were recorded. Majority of the patients visiting the hospital of Coorg Institute of Dental Sciences have one of the languages (given below) as their mother tongue. For this reason, the mother tongue of the patient was chosen as the basis for classification of ethnicity. Thus, codes for ethnicity were as follows: Coorgi/Kodava language: 1, Kannada: 2, Malayalam: 3, Urdu: 4, other languages (Tamil/Tibetan/Tulu):
For the clinical examinations, all the components of the WHO Oral Health Survey were recorded for every patient. Patients were examined on dental chairs in the Department of Oral Medicine and Radiology, Coorg Institute of Dental Sciences. Mouth mirrors and community periodontal index (CPI) probes were used for the examination.
The following were computed from the data collected by the proforma:
Decayed, Missing and Filled Teeth (DMFT) index as well as its individual components (decayed teeth [DT], filled teeth [FT], and missing teeth [MT])
Dental Aesthetic Index (DAI) score.
For analytical purpose, certain components of the Oral Health Survey Proforma were dichotomized as absent and present of a particular condition. Scores other than “0” or “9” for any of the boxes in each component meant the condition was present. The oral health-related variables which were dichotomized were:
Temperomandibular joint (TMJ) problems
Oral mucosal lesions/conditions
Enamel opacities
Dental fluorosis
Prosthetic status (presence of any prosthesis), and
Prosthetic need.
An instrument used to measure OHL, REALD-30 required an interview that was performed after the oral health examinations. Each interview with the participant took about 5 min. Participants were instructed not to pronounce those words for which they did not know the correct pronunciation. This was done in order to check the possibility of subjects pronouncing the words correctly by chance.
Statistical analysis
The collected data was subjected to statistical analysis by using Independent samples t-tests, one-way analysis of variance, Karl Pearson’s correlation co-efficient (r) and Kruskal–Wallis test. The SPSS-16 software (SPSS Inc., 2007) was used.
Results
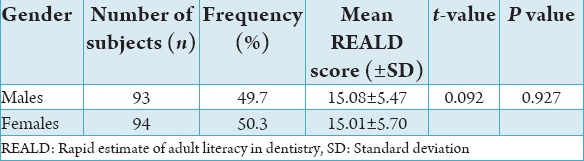
There were no statistically significant differences in the measurements for intra-examiner reliability (P = 0.048, paired t-test). A total of 187 individuals who underwent the oral examination and interview were included in the analyses. Males comprised 49.7% (n = 93) of the sample. The mean age of the participants was 37.4 ± 13.7 years (range: 18-73 years). The mean OHL score REALD was 15.04 ± 5.57. The minimum score obtained was 4 and the maximum was 26 (Table 1).
Table 1.
Distribution of subjects by gender and its association with REALD scores.
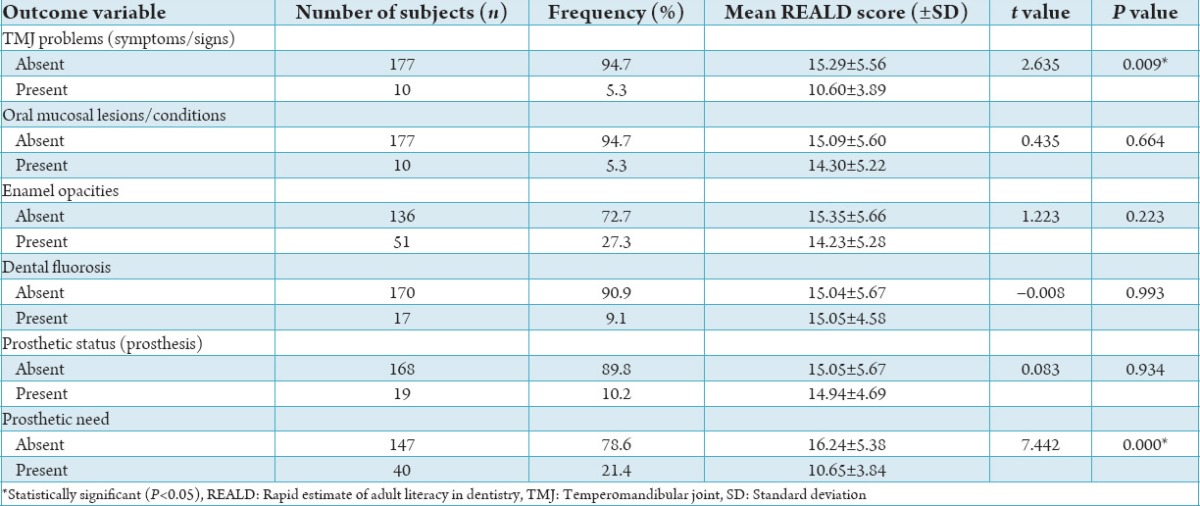
Of the different oral-health related conditions which were assessed by the WHO Oral Health Proforma and subsequently dichotomized for analytical purpose, the prevalence of the following were <10% in the study sample.
Tempero-mandibular joint problems (including symptoms and signs)
Oral mucosal conditions, and
Dental fluorosis.
Other components that were dichotomized and had a prevalence of more than 10% in the present sample were:
Enamel opacities
Presence of a dental prosthesis (in the upper and/or lower arches), and
Prosthetic need (in either the upper or lower arch or both) (Table 2).
Table 2.
Frequency distribution of study subjects based on dichotomized outcome variables and their associations with REALD scores (independent-samples t-test).
Majority (37.4%) of the participants had 2 as their maximum CPI score while 1.6% of them had 4 as their maximum score. A considerable number of subjects (97.3%) had no loss of attachment (LA), i.e., a Score 0.
The mean DMFT index and DAI scores of the sample were 4.40 ± 4.14 and 59.75 ± 17.12. Also shown in table are the means of the individual components of DMFT index namely DT, MT and FT (Table 3).
Table 3.
Mean DMFT, DT, MT, FT scores and DAI scores of the subjects.

Results of independent samples t-test to test differences in REALD scores between males and females revealed that no statistically significant difference (P > 0.05) existed between the genders.
When the subjects were classified based on language (ethnicity), majority of the participants (44.9%) were those who spoke Malayalam as their mother tongue, and then Kodava-speaking (25.7%) and Kannada-speaking (21.9%) subjects. Since it was observed that only a meager number of subjects (7.5%) belonged to other ethnic groups, it was decided to eliminate them from the analysis of the association between ethnicity and OHL and from subsequent analyses if the association between the two were found not to be significant. The association between ethnicity and REALD scores was not statistically significant (P > 0.05).
It was observed that the mean REALD scores were higher in those who did not have TMJ problems, oral mucosal conditions or lesions, enamel opacities, any prosthesis and prosthetic need/needs. However, the mean differences were found to be significant only with respect to those who had TMJ problems (P = 0.009) and those who required prosthesis (P = 0.00). Those who had dental fluorosis obtained a higher mean REALD when compared to those without fluorosis. This difference (0.011) was not, however, statistically significant (P = 0.993) (Table 2).
Correlation coefficients between REALD scores and each of other parametric variables assessed in the study were computed. Age was negatively correlated with REALD score, but the correlation was not significant. DMFT, DT, MT and DAI scores were negatively correlated with REALD and were statistically significant (P < 0.05). FT scores were positively correlated with REALD scores. However, this correlation was not statistically significant (Table 4).
Table 4.
Correlations of REALD scores with age, DMFT, DT, MT, FT, DAI scores.

The mean REALD score was found to be the highest (17.44 ± 5.57) in that group of subjects who had a CPI score of 0 for all the sextants. A steady decrease was observed in the mean REALD scores was observed with an increase in the maximum CPI score of the subjects. The differences in the REALD scores between the subjects with different maximum CPI scores were found to be highly significant (P = 0.00) (Table 5).
Table 5.
Associations between CPI scores, LA scores and REALD scores ANOVA.

The association between LA scores and REALD was also statistically significant (P = 0.005). The mean REALD score was higher (15.23 ± 5.48) in those who had no LA (Score 0) when compared to that (8.20 ± 4.91) of those who had (Score 1) (Table 5).
Discussion
The sample was one of convenience, meaning that it cannot be considered to be representative of the population of Virajpet. Also, only patients who could read, speak, and understand English were included in this study. This inclusion criterion was essential as the test for OHL used in our study, REALD-30 has been validated in English only.4 Since English as a language is not generally learnt, used or understood by most of those belonging to the lower socioeconomic strata, this inclusion criterion could have caused a bias with respect to the representation of the sample. Hence, generalizing the findings should be done with caution. Nevertheless, this study is one of the first attempts to measure OHL in a population of this part of the country.
Another limitation would be that the participants were recruited from the clinical environment, a setting that can introduce a selection bias because majority of the sample subjects were those who sought care. Furthermore, those who opted not to participate in the study may have refused to do so as they were aware of their limited literacy skills. Although these factors may have influenced the overall mean OHL scores of the sample subjects, they do not underrate the associations of OHL with other variables assessed in the study namely age, sex, ethnicity and oral health outcome variables.
The shortcomings of REALD-30, particularly in that it measures word recognition only with no test of comprehension or function have been acknowledged. Nevertheless, it has been demonstrated by previous studies that OHL estimates derived from word recognition tests such as REALD-30 correlate well with comprehension and functional health literacy.6
The mean OHL REALD-30 score of this South Indian population was 15.04 ± 5.57. No cut-off points have been established for the REALD-30 to determine what score would indicate inadequate OHL. Comparable mean scores were obtained in previous studies on other populations that have used the same OHL instrument by: (1) on an indigenous Australian community3 and (2) on low-income WIC population in seven counties in North Carolina, USA.4
A study on adult dental patients attending private clinics in North Carolina, USA demonstrated a higher mean REALD score (23.9 ± 1.29) than that obtained in our study. It must be noted that the subjects in this study were recruited from private dental practices while the study setting in the present study was a dental hospital.7
Our study showed that OHL scores were not different between the sexes. This finding was similar to that obtained in the study.7 OHL was not associated with gender in a study on patients attending urban clinic in Los Angeles, California.
In our study, OHL scores showed a negative correlation with age, indicating better literacy skills in the younger age groups. This correlation was not statistically significant. While Jones et al., in their study reported higher REALD scores in ≥40 years age group, the differences between the age groups were not significant.7 A study assessing health literacy in patients found that literacy skills were related to age, with younger patients having better skills. However, it was seen that these differences did not exist when the subjects were stratified by education.8 Hence, this relationship with age would have been more meaningful if they were interpreted along with educational levels, which were not recorded in our study.
With respect to associations between the various components of oral health and OHL scores, much anticipated findings were observed. The prevalence of the following conditions was higher in those with lower mean REALD scores: TMJ problems, oral mucosal lesions or conditions, enamel opacities, presence of the prosthesis, and a prosthetic need. Of these, TMJ problems and the need for prosthesis was significantly associated with REALD scores. The only oral condition where the OHL scores were higher in those who had it than those who did not was dental fluorosis. However, the mean difference between the groups was negligible.
It was observed that higher REALD scores were associated with lower caries experience (DMFT score). When the individual components of DMFT were analyzed, it was found that both (DT score) and (MT score) were negatively correlated with REALD scores. These associations of REALD with DMFT, DT and MT were significant. The FT scores were however positively correlated with REALD scores, though not significantly. These findings thus imply that those who had higher OHL scores were more likely to get their teeth filled.
REALD and DAI scores were negatively correlated, and the association was significant. Thus, the study found that the malocclusion status (as assessed by DAI) was significantly associated with OHL.
Studies have shown that a health-literate individual has the knowledge, skills, and confidence that will enable him to manage health on a daily basis. This includes the ability to know when and how to enter the health care system and how to make the best use of health services.9 This can be extrapolated to the context of OHL and navigation of oral health systems. Better navigation skills will result in appropriate utilization of dental services and therefore will improve oral health outcomes.
OHL was significantly associated with periodontal status in this population. This included both CPI and LA index scores. There was a steady decline in the REALD scores with higher scores of CPI as well as LA index. Thus, those with better OHL had better periodontal health. Low levels of health literacy are associated with poorer knowledge particularly about chronic illnesses and its causes and compromised self-care behavior.4
These reasons also explain the higher prevalence of the prosthetic need, higher malocclusion index DAI scores and higher caries incidence in low oral health-literate individuals found in our study.
Patients with low levels of literacy find it difficult to understand instructions or importance of preventive dental procedures. In all its probability, these patients may also be less compliant with recommendations.7
This study confirms the association OHL and oral health status. It demonstrates that it is necessary to consider OHL in addition to the other determinative covariates (such as age, gender, socioeconomic level) in identifying groups or individuals with poorer oral health outcomes. Studies taking into account the educational level of the subjects may throw more light upon the associations between OHL and oral health status found in our study. It is recommended that research in this area be pursued.
Adult basic education programs may provide an important avenue for strengthening OHL skills. It requires intensive collaborative efforts among health providers, researchers, educators, policy-makers, public officials, the commercial sector, and the public to improve OHL.10
Conclusions
The conclusions that can be drawn from the study are:
OHL was not associated with sex, age, or ethnicity in this sample of the Virajpet population
-
OHL is associated with oral health status. The oral-health outcomes which were significantly associated with OHL were
- TMJ problems
- Prosthetic need
- Dental caries experience
- Malocclusion status
- Periodontal disease status.
Lower OHL was associated with poorer oral health status.
OHL instruments can be considered to be included as screening tools to identifying individuals or groups with poor oral health outcomes.
Footnotes
Source of Support: Nil
Conflict of Interest: None
References
- 1.Devi MA, Soni S, Radha G, Kadanakuppe S, Nagashree SR, Pallavi SK. Reliability and validity of a questionnaire to assess oral health literacy among college students in Bangalore city. Int J Contemp Dent. 2011;2(2):43–6. [Google Scholar]
- 2.Cornett S. Assessing and addressing health literacy. [Last accessed on 2010 Jan 02];OJIN Online J Issues Nurs. 2009 14(3) Manuscript 2. [Google Scholar]
- 3.Parker EJ, Jamieson LM. Associations between indigenous Australian oral health literacy and self-reported oral health outcomes. BMC Oral Health. 2010;10:3. doi: 10.1186/1472-6831-10-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee JY, Rozier RG, Lee SY, Bender D, Ruiz RE. Development of a word recognition instrument to test health literacy in dentistry: The REALD-30 –A brief communication. J Public Health Dent. 2007;67(2):94–8. doi: 10.1111/j.1752-7325.2007.00021.x. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Basic Methods. 4th ed. Geneva: World Health Organization; 1997. Oral Health Surveys. [Google Scholar]
- 6.Vann WF, Jr, Lee JY, Baker D, Divaris K. Oral health literacy among female caregivers: Impact on oral health outcomes in early childhood. JDent Res. 2010;89(12):1395–400. doi: 10.1177/0022034510379601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones M, Lee JY, Rozier RG. Oral health literacy among adult patients seeking dental care. JAm Dent Assoc. 2007;138(9):1199–208. doi: 10.14219/jada.archive.2007.0344. [DOI] [PubMed] [Google Scholar]
- 8.Shea JA, Beers BB, McDonald VJ, Quistberg DA, Ravenell KL, Asch DA. Assessing health literacy in African American and Caucasian adults: Disparities in rapid estimate of adult literacy in medicine (REALM) scores. Fam Med. 2004;36(8):575–81. [PubMed] [Google Scholar]
- 9.Kickbusch I. Improving health literacy- A key priority for enabling good health in Europe. European Health Forum Gastein 2004- Special Interest Session [Google Scholar]
- 10.National Institute of Dental and Craniofacial Research, National Institute of Health, U.S. Public Health Service, Department of Health and Human Services. The invisible barrier: Literacy and its relationship with oral health. A report of a workgroup sponsored by the National Institute of Dental and Craniofacial Research, National Institute of Health, U.S. Public Health Service, Department of Health and Human Services. J Public Health Dent. 2005;65(3):174–82. doi: 10.1111/j.1752-7325.2005.tb02808.x. [DOI] [PubMed] [Google Scholar]


