Abstract
IL17-dependent autoimmunity to Collagen type V (Col V) has been associated with lung transplant obliterative bronchiolitis. Unlike the Th-1-dependent immune responses to tetanus toxoid (TT), the Th17 response to Col V in lung transplant patients and its Th1/17 variant observed in coronary artery disease patients requires IL-1β, TNFα and CD14+ cells. Given the involvement of the P2X7R in monocyte IL-1β responses, we investigated its role in Th17, Th1/17, and Th1- mediated pro-inflammatory responses. Transfer of antigen-pulsed PBMC from Col V -reactive patients into SCID mouse footpads along with P2X7R antagonists revealed a selective inhibition of Col V-, but not TT -specific swelling responses. P2X7R inhibitors blocked IL-1β induction from monocytes, including both Col V-α1 peptide-induced (T-dependent), as well as native Col V induced (T-independent) responses. Significantly higher P2X7R expression was found on CXCR3negCCR4+/6+ CD4+ [Th17] vs. CXCR3+CCR4/6neg CD4+ [Th1] subsets in PBMC, suggesting that the paradigm of selective dependence on P2X7R might extend beyond Col V autoimmunity. Indeed, P2X7R inhibitors suppressed not only anti-Col V, but also Th1/17–mediated allo-immunity, in a heart transplant patient without affecting anti-viral EBV responses. These results suggest that agents targeting the P2X7R might effectively treat Th17-related transplant pathologies, while maintaining Th1-immunity to infection.
Keywords: P2X7R, Th17, chronic rejection, Col V, IL-1β
INTRODUCTION
The P2X7R has emerged as a potential site of regulation in a number of inflammatory states, including graft versus host disease (1), islet allograft rejection (2), chronic heart rejection (3), rheumatoid arthritis (4, 5) and psoriasis (6). Functioning as an ATP gated ion channel (7, 8), the P2X7R allows cation passage through the cell, leading to downstream activation of inflammasomes and production of IL-1β which is obligatory for Th17 development (9, 10). The loss of tolerance to the minor fibrillar collagen Col V, a sequestered self antigen (11), was a reported common characteristic of patients listed for lung or heart transplantation, such as patients suffering from idiopathic pulmonary fibrosis (12), late stage coronary artery disease (CAD) (13, 14) and patients developing Bronchiolitis Obliterans Syndrome (BOS) after lung transplantation (13, 15). Investigation into the loss of tolerance to Col V in these patient groups has revealed that the cellular immune response to Col V is Th17 mediated, as it was dependent on IL-17 and CD4 T cells, but also required IL-1β, TNFα, and monocytes (14). Similar to the reported IL-17 mediated response to soluble donor antigen (allo) in kidney transplant patients (16), the IL-17 requirement was also associated with IL1β-dependence (14). Unlike Col V, the cellular immune response to Tetanus Toxoid (TT) or Epstein Barr Virus (EBV), is Th1 mediated, as it depends on IFNγ and not IL-17 (14, 16). Knowing that the Th17-mediated Col V response in lung transplant patients differs from the cellular immune response to TT in the requirements for IL1β and monocytes, we tested the hypothesis that P2X7R function (required for inflammasome activation and IL1β production in certain innate immune contexts) was required for the Th17 cellular immune response to Col V. To test this hypothesis, we used pharmacological inhibitors of the P2X7R (Suramin, AZD9056 and periodate-oxidized ATP (oATP)) to evaluate P2X7R involvement in Col V specific cellular immune responses.
METHODS
Human Subjects
Immunologic monitoring was performed on cryo-preserved blood samples from Col V- reactive patients with end stage CAD (n=3), lung pathology due to primary ciliary dyskinesia (n=1), lung transplant (n=1) or heart transplant (n=1). Both transplant recipients were sampled 7–8 years post-transplantation, the lung patient at a time of normal graft function, the heart patient during an episode of acute rejection combined with cardiac allograft vasculopathy (CAV). Subject consent was obtained using human subjects committee-approved, written, informed consent procedures at the University of Wisconsin Hospital and Clinics. Blood was collected and PBMCs were processed as described previously (17). Where applicable, human PBMCs were incubated with CD14 (Miltenyi, 120-001-146) or pan T-cell (Miltenyi, 120-008-788) microbeads and separated using an autoMACS (Miltenyi) as per the manufacturer’s protocol.
YOPRO Uptake Assay
The YOPRO dye uptake assay and the generation of transfected HEK293 cells expressing a human P2X7R with normal (P2X7-wt) or loss of function (P2X7-496) activity was described previously (18, 19). Briefly, 5×104 transfected HEK cells were stimulated for 20 minutes with various concentrations of AZD9056 and Suramin in the presence of 100uM 2′-3′-O-(4-benzoylbenzoyl) adenosine 5′triphosphate (BzATP, Sigma) with 10uM YO-PRO-1 (Invitrogen, Carlsbad, CA).
Transvivo Delayed-Type Hypersensitivity Assay
The Trans-vivo delayed type hypersensitivity (TV-DTH) assay was performed as described previously (14, 20). Inactivated Tetanus Toxoid was purchased from Sanofi-Aventis Pasteur. Human Col V was obtained from D. Brand (University of Tennessee, Memphis), and was prepared from placenta as described elsewhere (11). Human Col I was purchased from BD Pharmingen. The Col V-HLA-DR15 restricted α1 peptides, p1049 and p1439 were identified and synthesized as previously described (21). AZD9056 was obtained from Astrazeneca Pharmaceuticals (Wilmington, DE). Suramin and oATP were both purchased from Sigma Chemical (Saint Louis, MO). Neutralizing antibodies to IL-17 (eBioscience, 16-7178-85), IL-1β (eBioscience, 16-7018-85) or IFNγ (eBioscience, 16-7318-85) were used along with normal rabbit IgG (R&D Systems, AB-105-C) where applicable.
Immunohistochemistry
Footpads from SCID mice were harvested and submitted for routine histology and immunohistochemical (IHC) staining as described previously (22).
Intracellular Cytokine Staining (ICCS)
ICCS experiments for IL-1β and TNFα were carried out as described previously (21). All samples were acquired on a FACScaliber flow cytometer and populations of IL-1β and/or TNFα positive cells amongst CD3−/CD14+ subsets were determined with FlowJo analysis software (Treestar).
P2X7R Flow Cytometry Staining
1×106 PBMCs from patients were stained for surface markers CD3 (Biolegend, 344814), CD14 (Biolegend, 325614), CXCR3 (BD Bioscience, 550967), CCR4 (BD Bioscience, 561034) and CCR6 (BD Bioscience, 551773). Following surface staining, cells were fixed, permeabilized (Becton Dickinson, Lyse/Fix Buffer) and subsequently incubated with 1ug of P2X7R antibody (Aviva BioSystems, OASA05733) for 45 minutes on ice, followed by incubation with secondary antibody conjugated to Alexa488 (Invitrogen, A11006) for 30 minutes. Cells were washed three times and fixed in 2%PFA. All samples were acquired on an LSR-II flow cytometer and frequencies of T cell or monocyte populations positive for P2X7R, or corrected median flouresence intensity (MFI)[MFI of sample signal – MFI of isotype control] of P2X7R signal were determined with FlowJo analysis software (Treestar).
Statistical Analysis
Multiple replicates of each sample within sample groups were averaged across each assay and data was combined and analyzed by Mann-Whitney U and ANOVA or paired T test performed with Prism 5.0 (GraphPad Prism software, La Jolla, CA).
RESULTS
The cellular immune response to Col V, but not TT, in Col V reactive patients requires activation of the P2X7R
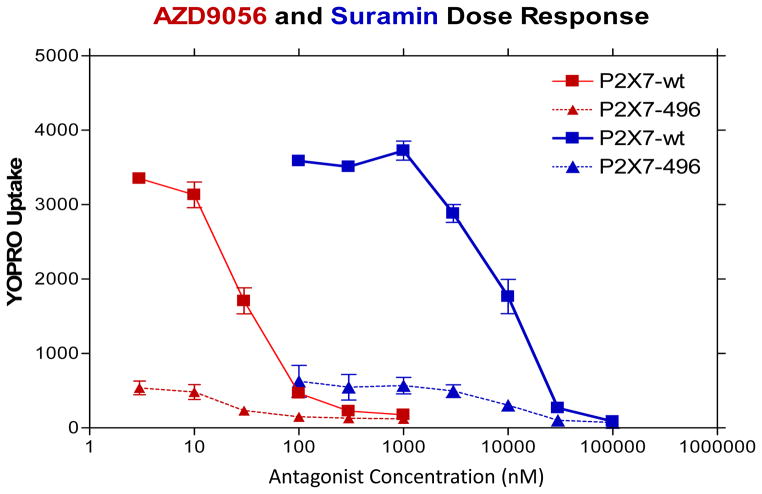
To examine the role of P2X7R in the cellular immune response to Col V and TT, we tested two pharmacological antagonists of P2X7R function, Suramin and AZD9056. We first found the maximum effective concentration of both P2X7R antagonists (Suramin [30uM], and AZD9056 [300nM]) at inhibiting P2X7R pore function (Figure 1). Next we analyzed TV-DTH responses to Col I, Col V and TT by PBMCs of six Col V-reactive patients in the presence or absence of Suramin or AZD9056 (Figure 2A). Col V elicited a significant increase in footpad swelling over PBS and Col I controls, consistent with previous reports (13, 14). Both Suramin and AZD9056 treatment of PBMCs significantly inhibited Col V mediated TV-DTH responses. This effect was not due to toxicity, as Suramin and AZD9056 failed to inhibit the response to TT. Of note, similar levels of P2X7R inhibition of Col V responses were observed in all three groups of Col V reactive patients examined (CAD, lung pathology, heart transplant) (supplemental figure 1). Figure 2B illustrates the alteration in footpad histology of Col V versus TT stimulated PBMCs in the presence of a P2X7R antagonist, Suramin. H&E staining of Col V or TT stimulated, PBMC-injected, mouse footpads revealed a robust infiltration by mononuclear and polymorphonuclear cells extending into the skin and skeletal muscle. The Col V-stimulated pro-inflammatory response was dramatically decreased in the presence of both Suramin (Figure 2B) and AZD9056 (data not shown). Human cells were limited to a highly focused area in the sub-dermal fatty tissue, with few Ly6G+ mouse neutrophils present. In contrast, the TT response exhibited a diffuse infiltration pattern of CD45+ hematopoietic cells, human CD68+ macrophages and Ly6G+ mouse neutrophils both in the presence and absence of P2X7R inhibitors, This histological observation was consistent with the TV-DTH response we observed for each sample.
Figure 1. Dose Response of Suramin and AZD9056 inhibition of P2X7R function in stably transfected HEK293 cells.
5×105 HEK cells stably transfected with either WT P2X7R (P2X7-wt) or an inactive P2X7 receptor construct (P2X7-496) were treated with 100uM BzATP and 10uM YOPRO with or without Suramin (0.1–100uM) or AZD9056 (1–1000nM) for 20 min at room temperature as described previously (18). Fluorescent signal was determined by plate reader and quantified data from at least two individual experiments were performed.
Figure 2. The cellular immune response to Col V, but not TT, in Col V reactive patients requires activation of the P2X7R.

(A) The Col V reactive group is comprised of 3 CAD patients, 2 lung pathology patients, and 1 heart transplant patient. Responses to Col V (5ug), and the recall antigen TT (25ug) are shown with and without treatment of the P2X7R antagonists, Suramin (30uM) and AZD9056 (300nM) in PBMCs from all Col V reactive patients. PBMCs treated with Col I (5ug) were also used as a negative control. All treatment values represent the observed TV-DTH response for the respective group minus the PBS control. Data are from 6 individual patients, repeated 2–5 times each. * denotes a statistically significant inhibition of the Col V response (Suramin, p<.008; AZD9056, p<.005). (B) Representative H&E (x20), human CD45 haemotopoetic cell (x20), human CD68 phagocytic vesicle containing cells (x20) and mouse neutrophil Ly6G (x20) stained footpads following Col V, TT and or P2X7R antagonist treatment. Inset numbers represent the TV-DTH response observed from each respective footpad.
HLA-DR restricted Col V peptide epitopes stimulate Col V specific cellular immunity in a P2X7R dependent manner
We recently identified 2 peptides, p1049 and p1439 located within the immunogenic α1(V) chain of the Col V molecule that bind to DR15 and induce a Th17 response in PBMCs of Col V-reactive DR15+ patients, and in a DR15neg recipient of a DR15+ lung transplant (21). We hypothesized that these short peptides, lacking α-helical structure or post-translational modifications of the parent molecule, will stimulate Th17 cells solely as p/MHC complexes on APCs while circumventing any direct activation of the monocyte. To address whether or not P2X7R antagonists could inhibit TV-DTH responses stimulated by Col V DR-specific peptides, we tested PBMCs from 3 DR15+ Col V-reactive patients. Figure 3A shows that TV-DTH responses to Col V peptides p1049 and p1439, recapitulated that of whole Col V. Like the response to Col V, both p1049 and p1439 induced swelling was significantly inhibited by Suramin and AZD9056. In Figure 3B, representative H&E staining of footpads 24 hours after injection of p1439 or p1049 stimulated PBMCs shows both Suramin and AZD9056 cause a dramatic decrease in the DR restricted peptide induced swelling.
Figure 3. Col V DR specific peptides increase Col V specific cellular immunity in a P2X7R dependent manner.
(A) TV-DTH responses from intact Col V (5ug), or α1(V) peptides p1049 (5ug) and p1439 (5ug) were used to stimulate TV-DTH responses by PBMC from 3 DR15+ Col V-reactive patients. Both p1049 and p1439 stimulated a swelling that was significantly inhibited by both Suramin (1049 p<.02, 1439 p<.01) and AZD9056 (1049 p<.007, 1439 p<.009). Data are from 3 DR15+ Col V- reactive patients. Experiments were repeated at least 2 times. * Denotes statistical significance from respective peptide stimulation. (B) Representative H&E staining (20X) from Col V-DR-specific peptide stimulated PBMCs with and without P2X7R inhibition. Inset numbers represent the TV-DTH response observed from each respective footpad.
T cell dependent and independent production of IL-1β and TNFα by monocytes in response to Col V occurs in a P2X7R sensitive manner
We have previously shown that Col V or Col V-α1 synthetic peptides can stimulate IL-1β production by monocytes cultured overnight in the presence of responder Th17 cells (21). Therefore, we examined whether P2X7R inhibition blocks the production of IL-1β or TNFα from monocytes in Col V and α1-peptide stimulated whole PBMCs, and as a control for possible T-independent effects, in cultures of isolated monocytes. Furthermore, since the Col V molecule, containing numerous post translational modifications (23) could potentially activate the T cell as well as the antigen presenting cell for Col V, the monocyte, through Damage Associated Molecular Patterns (DAMPs) interactions, we investigated whether Col V and DR-restricted peptides could stimulate monocytes directly by separating monocytes from PBMCs and stimulating isolated monocytes. Figure 4A shows representative flow plots of Col V, p1049 and p1439 stimulated PBMCs, in the presence or absence of Suramin or AZD9056. Overnight stimulation of PBMCs with Col V, p1049 or p1439 caused a significant increase in the percentage of IL-1β and TNFα from CD3−/CD14+ populations. Furthermore, the Col V, p1049 and p1439-stimulated production of IL-1β (Figure 4B top) and TNFα (Figure 4B bottom) in PBMC overnight cultures was significantly inhibited by P2X7R antagonism. Unlike the Col V or peptide response, LPS stimulated IL-1β and TNFα production was unaffected by either Suramin or AZD9056 (supplemental figure 2). To investigate whether Col V or DR-restricted peptides could directly stimulate isolated monocytes to produce IL-1β or TNFα, we performed ICCS assays on 2×105 MACS separated monocytes. (Figure 4C) In comparison to monocytes in whole PBMCs exposed to Col V (black bars), in the absence of T cells, Col V stimulated a lower but significant increase in IL-1β and TNFα from isolated monocytes (grey bars, left and right), a response that was sensitive to P2X7R antagonism (supplemental figure 3). Unlike the response of isolated monocytes to whole Col V, both p1049 and p1439 failed to increase IL-1β or TNFα production in isolated monocytes.
Figure 4. T-Dependent and T-Independent Col V and peptide stimulated production of IL-1β and TNFα in Col V reactive patients requires P2X7R activity.
1×106 PBMCs from Col V reactive patients were stimulated overnight with Col V (5ug), p1049 (5ug) or p1439 (5ug) in the presence of Brefeldin A with or without Suramin (30uM) or AZD9056 (300nM). Representative flow plots (A) and quantified flow cytometry data (B) illustrate that Col V (p<.009), p1049 (p<.03) and p1439 (p<.02) stimulate IL-1β and TNFα [Col V (p<.007), p1049 (p<.009), p1439 (p<.009)] production in whole PBMCs from CD3−CD14+ populations. The production of IL-1β and TNFα elicited from Col V, p1049 and p1439 was sensitive to P2X7R antagonists in all cases. [IL-1β: Suramin, p<.02 for all three agonists; AZD9056, p<.02 for all three agonists. TNFα: Suramin, p<.01 for all three agonists; AZD9056, p<.008 for all three agonists]. Inset numbers on flow plots represent the frequency of respective cytokine positive populations in that quadrant. To investigate whether Col V or DR-restricted peptides could directly stimulate isolated monocytes to produce IL-1β or TNFα, 2×105 MACS separated monocytes were stimulated with Col V (5ug), p1049 (5ug) or p1439 (5ug) (Figure 4C). IL-1β and TNFα production from Col V and peptide stimulation in whole PBMCs (black bars) and isolated monocytes (grey bars) is shown. Col V, but not DR-restricted Col V peptides, stimulated a significant increase in IL-1β (p<.04) and TNFα (p<.01) from isolated monoctytes. All Peptide data is from the 3 DR15+ Col V- reactive patients. Experiments were repeated at least twice. *Denotes statistical significance from respective media control. #Denotes statistical significance from respective Col V or peptide stimulation.
Inhibition of P2X7R function on both monocytes and T cells is required to block Th17 cellular immune responses in Col V reactive patients
To examine whether P2X7R function on the monocyte or T cell defines the Col V response in our patient cohort, we used another P2X7R antagonist, oATP. oATP inhibits P2X7R function by covalently binding to the P2X7R (3, 24). This inhibitor, unlike Suramin or AZD9056, irreversibly inhibits P2X7R function on treated cells alleviating concerns regarding potential drug wash off or release. Isolated monocytes and T cells from Col V reactive patients were loaded with oATP. Figure 5 shows that oATP treated whole PBMCs exhibit a significant decrease in Col V stimulated footpad swelling, similar to that observed with Suramin and AZD9056. When isolated monocytes were treated with oATP and added to untreated autologous T cells, there was no significant decrease in the Col V response. Similarly, when oATP treated T cells were added to untreated autologous monocytes, there was no significant reduction in the Col V response. However, when both monocytes and T cells were separately treated with oATP, and added together and stimulated with Col V, there was a significant reduction in the Col V stimulated swelling response. This result indicates that inhibition of P2X7R function on both T cells and monocytes is necessary for inhibiting the pathogenic cellular immune response in Col V-reactive patients.
Figure 5. The P2X7R function on both monocytes and T cells is required for the Col V cellular immune response in Col V reactive patients.
Whole PBMCs, MACs separated monocytes, or MACs separated T cells were treated with Suramin (30um), AZD9056 (300nM) or preloaded with oATP (300uM, 3 hour pretreatment) and subsequently stimulated with Col V (5ug). Whereas all three P2X7R antagonists blocked Col V responses in PBMCs or Col V reactive patients, groups of isolated monocytes loaded with oATP added to autologous untreated T cells, or oATP treated T cells added to autologous untreated monocytes, failed to inhibit Col V induced swelling. Only oATP treatment of both monocytes and T cells lead to significant inhibition of Col V responses. Data are from all 6 Col V reactive patients, repeated at least twice.
Chemokine Receptor Defined T cell Subsets Express Different Levels of P2X7R
The use of chemokine receptor expression profiles has proven reliable for identifying subsets of IFNγ or IL-17 producing T cells (25, 26). Most notably, Th1-IFNγ producing T cells can be identified by CXCR3 expression (25, 27, 28), whereas IL-17 producing cells can be identified by the expression of CCR4 and CCR6 (29–32). With a clear effect of P2X7R antagonists on inhibiting cellular immunity to Col V (IL-17 dependent) but not TT (IFNγ dependent) we decided to investigate whether IL-17 producing T cell subsets have higher expression of P2X7R as opposed to their IFNγ producing counterparts. In addition, we also investigated monocyte expression levels of P2X7R. In figure 6A, representative flow plots from a Col V reactive patient show P2X7R expression is highest on monocytes (CD14+/CD3−), followed by CXCR3−/CCR4+/CCR6+ T cells, and finally CXCR3+/CCR4−/CCR6− T cells, as assessed by Median Flourescence Intensity (MFI) of P2X7R staining. This trend of expression was relatively consistent within our patient cohort. Corrected MFI data for each Col V reactive patient was compiled and shows that monocytes have significantly higher expression of P2X7R than CXCR3+/CCR4−/CCR6− T cells and trend toward higher P2X7R expression than CXCR3−/CCR4+/CCR6+ T cells. Furthermore, CXCR3−/CCR4+/CCR6+ T cells have significantly higher expression of P2X7R than CXCR3+/CCR4−/CCR6− T cells (Figure 6B, top). Investigation of the frequency of P2X7R positive cells within monocyte or T cell subset populations illustrates that there are significantly higher frequencies of P2X7R positive cells in monocytes and Th17 populations as compared to Th1 (Figure 6B, bottom).
Figure 6. Chemokine Receptor Expression Defined T cell Subsets Express Different Levels of P2X7R.
1×106 PBMCs were stained with surface markers CD14, CD3, CD4, CXCR3, CCR4 and CCR6. Following surface staining, cells were lysed/fixed and subsequently stained for P2X7R (Aviva Biosystems). Described populations of IFNγ producing (CXCR3+/CCR4−/CCR6−) and IL-17 producing (CXCR3−/CCR4+/CCR6+) T cell subsets, along with monocyte populations (CD3−/CD14+) were then analyzed for relative P2X7R expression. (A) Gating populations and relative P2X7R expression from whole PBMCs for IFNγ and IL-17 producing T cell subsets as well as monocytes. (B) Quantified flow cytometry staining of the corrected Median Flouresence Intensity (MFI of sample signal – MFI of isotype control) (top) and relative frequency of P2X7R expression amongst Th1, Th17 or monocyte populations (bottom). Data is from all 6 Col V reactive patients.
Differential requirement for P2X7R function in viral vs. alloimmune TV-DTH responses in transplant recipients
The finding of differential P2X7R expression on circulating Th1 vs Th17 cells suggested that we broaden the scope of our inquiry into P2X7R dependency of T cell-mediated immunity in transplant patients. To do this, we looked at the P2X7R requirement of TV-DTH responses to allo-antigen and EBV viral proteins, in addition to Col V and TT in a heart transplant patient with mixed chronic and acute rejection, as well as in a well established cohort of chronic kidney rejectors. Figure 7A shows TV-DTH responses to Col V and allo-antigens. A biopsy taken at the time of leukapheresis revealed active acute rejection level 3A and CAV as indicated by luminal occlusion of arterioles (Supplemental Figure 4). Both Col V and allo TV-DTH responses were inhibited by Suramin and AZD9056. In addition, IL-17 and IL-1β neutralization dramatically inhibited TV-DTH responses to both Col V and the allo-indirect pathway. Of note, IFNγ neutralizing antibody also inhibits the cellular immune response to both Col V and the allo-indirect pathway, indicating that this patient exhibits a Th1/17 response in the face of Col V or allo-challenge. Figure 7B shows the P2X7R and cytokine dependency of both TT (open) and EBV (checkered). Both TT and EBV show no decrease in TV-DTH responses in the presence of Suramin and AZD9056. Similarly, IL-17 and IL-1β neutralization do not decrease their cellular immune responses. Only neutralization of IFNγ reduced the response to TT and EBV. To further investigate P2X7R sensitivity of the allo-indirect response versus anti-viral responses to EBV, we used a group of chronic kidney rejectors in the TV-DTH assay in conjunction with P2X7R antagonists and antibody neutralization strategies. Figure 7C shows TV-DTH responses to allo (left) and EBV (right) antigens. AZD9056 and Suramin both significantly inhibit Allo induced swelling, while exhibiting no effect on the EBV response. Furthermore, the allo-indirect response in this chronic kidney rejector group was significantly inhibited by neutralization of IFNγ, IL-17, IL-1β and TNFα (Figure 7D).
Figure 7. Differential requirement for P2X7R function in viral vs. allo-immune TV-DTH responses in heart and kidney transplant patients.
(A) TV-DTH responses to Col V (black) and soluble donor antigen (allo) are shown in the presence or absence of P2X7R antagonists, or neutralizing antibodies to IL-17, IL-1β or IFNγ. The TV-DTH response to self antigen (hashed bar) is also shown for comparison. (B) TV-DTH responses to TT or EBV in the presence of P2X7R antagonists or neutralizing antibodies to IL-17, IL-1β and IFNγ are illustrated. Data in A and B is from 1 heart transplant patient repeated at least twice. (C) TV-DTH responses in chronic kidney rejector patients to Allo or EBV in the presence or absence of P2X7R antagonists. Allo-responses were significantly inhibited by AZD9056 (p<.03) and Suramin (p<.02), while EBV responses showed no significant inhibition. (D) TV-DTH responses in chronic kidney rejector patients to Allo in the presence or absence of neutralizing antibodies (10ug) to IL-17, IL-1β, TNFα and IFNγ were significantly inhibited at a level of p<.02. Data in C and D are from 5 chronic kidney rejector patients.
DISCUSSION
We have previously shown that IL-1β and TNFα are required for the IL-17 mediated cellular immune response to Col V (13, 14). More recent reports have shown that innate derived signals, including IL-1β, can release IL-17 producing T cells from quiescence and into active IL-17 producing cells (33). While P2X7R inhibition on monocytes can be associated with the loss of IL-1β production (34), the effect of P2X7R inhibition on T cells is not so clear. What is clear from our study (Figure 6) is that both monocytes and CXCR3−/CCR4+/CCR6+ T cells, a subset of T cells associated with IL-17 production, have higher P2X7R expression than the IFNγ associated T cell subset, CXCR3+/CCR4−/CCR6−. Furthermore, monocytes, consistent with the work of Gu et al. (35), have the highest expression of P2X7R amongst blood mononuclear cells. While the function of the T cell P2X7R was not directly investigated, there is clearly a non-redundant role for this as only when both the monocyte and T cell P2X7R (Figure 5) were blocked by oATP, is the cellular immune response to Col V lost. One way in which the function of P2X7Rs on T cells can be explained in the context of the Th17 mediated Col V response is through an observation made by Schenk et al (36). In this report, ATP signaling through T cell P2X7Rs led to sustained activation of ERK 1/2, causing altered phosphorylation of a family of T cell related transcription factors, the Nuclear Factor of Activated T cell (NFAT). In this study, inhibition of T cell P2X7Rs with oATP blocked ERK 1/2 activation, leading to T cell anergy (36). Interestingly, we found that an ERK 1/2 inhibitor (U0126) blocked the Col V-TV-DTH response to similar levels observed with P2X7R antagonists (supplemental Figure 5). Consistent with Th17 but not Th1 sensitivity to P2X7R inhibition, U0126 did not inhibit the TT response. It’s possible that the role of P2X7Rs on T cells involves releasing Th17 cells from the constraint of intrinsic regulation of TCR signaling. It has been suggested that CD161+ T cells, which comprise the bulk of CD4 and CD8 IL-17 producing T cells, have an intrinsic regulation of TCR signal upon contact with APCs (33). The P2X7R-ERK cascade may unlock the intrinsic regulation of the TCR signal, allowing rapid secretion of IL-17. This cascade may function independently of the IL-1 receptor signaling pathway through which monocyte derived IL-1β promotes IL-17 release (33).
It is now clear that the Col V- α1-derived 15mer peptides are sufficient to elicit a response in the TV-DTH assay equivalent to that of the whole protein (21). The response to peptides of the α1(V) chain, which represents the immunogenic portion of the Col V [α1α2] hetero-trimer (14), was also exquisitely sensitive to P2X7R inhibition, both in vivo (Figure 3) and in vitro (Figure 4). Since the peptides can only induce cellular immune responses via the TCR interaction with pMHC-II complexes on the monocytes, this finding was consistent with the critical importance of innate immune signaling for optimal TCR function in Th17 cells.
The observation that Col V also stimulated IL-1β and TNFα in isolated monocytes in a P2X7R dependent manner, is consistent with the idea that Col V, a heavily post transcriptionally modified protein (23), can activate leukocytes directly as previously reported for lung epithelial cells in culture (37). How this occurs, and whether Pattern Recognition Receptors (PRRs) are involved is unclear. The downstream signaling from activated P2X7Rs can lead to inflammasome activation (38, 39). This activated complex of proteins is responsible for the processing of pro IL-1β/IL-18 into the mature IL-1β and IL-18 proteins (18, 40, 41). While multiple mechanisms for the secretion of IL-1β in response to LPS exist (42), Col V activation of monocyte IL-1β would appear to utilize a prototypical P2X7R-dependent Nlrp3 inflammasome pathway, consistent with that reported by Jankovic et al as a potential regulator of acute graft-versus-host disease (43). In this study, the authors found that removal or deletion of IL-1β or Nlrp3 inflammasome components increased allo-reactive T cells and decreased IL-17 producing T cells. Furthermore, a recent report from Lasiglie et al (34) underscored the importance of IL-1β/inflammasome functioning in the regulation of Th17 responses in patients with cryopyrin-associated periodic syndrome (CAPS). They reported a naturally occurring mutation in NLRP3, an important member of the inflammasome complex, within the CAPS patient population, caused enhanced IL-1β production from monocytes, and subsequent increased IL-17 serum levels and production in vitro (34). While this report deals with mutations in the inflammasome pathway, the evidence strongly supports a role for IL-1β driving Th17 effector functions, similar to what we observe in our Col V reactive patients.
Our data suggest that there are multiple ways that monocytes can be activated during immune responses to Col V, including: 1) through direct interaction with intact Col V protein, a component of “pro-inflammatory matrix” (44, 45), 2) as a result of TCR interaction with DR-bound α1(V) peptide on the monocyte APC and 3) by interaction with IL-17 [its receptor being abundantly expressed by monocytes (46)]. Consistent with the TV-DTH results, we also observed that the Col V-specific peptides increased IL-1β production in whole PBMCs, albeit at a lower level than observed with whole Col V, and in a P2X7R dependent fashion. Since the peptides are only working through TCR-MHC interactions (Figure 4: i.e. peptides failed to activate monocytes directly), the monocyte would not receive the same amount of stimulation with Col V-peptides as it would with the whole Col V molecule. The coordinated signaling through P2X7Rs on both the monocyte and T cell may release Th17 effector function previously held in check.
We have previously shown that kidney graft chronic rejectors made anti donor antigen responses in the TV-DTH assay that were inhibited by neutralizing both IFNγ and IL-17 (16). Herein, we report that allo-indirect responses of chronic kidney rejectors are also sensitive to IL-1β and TNFα neutralization as well as P2X7R inhibitors. One important conclusion from this study is that P2X7R inhibition in a heart transplant patient or a group of chronic kidney rejectors does not just selectively block the cellular immune response to sequestered self antigens like Col V, but also inhibits the allo-response to donor antigen, while not affecting the viral (EBV) or bacterial (TT) response (Figure 7). In both groups of chronic rejectors, both the Col V and indirect allo-response were dependent on both IL-17 and IFNγ, indicating a Th1/Th17 response, whereas the EBV and TT responses were purely IFNγ dependent. Since P2X7R inhibitors appear to selectively inhibit the self-and allo-responses while maintaining viral and bacterial immune responses, the use of specific inhibitors to P2X7R may be ideal for anti-rejection drugs as viral and bacterial immunity would be unaffected while immune responses to allo- and self would be attenuated.
Supplementary Material
Acknowledgments
The authors wish to thank Matt Pestrak for aiding in the completion of the experiments, Dr. Jose Torrealba for reviewing the histology data and the laboratory of Sam Gellman for the production of Col V (α1) peptides. The authors would like to further thank Dr. Richard Derks, and Dr. Jenny Gumperz for their expert consultation and guidance throughout this project. This work was supported by NIH grant #PO1AI084853 (JAS, EJG, DSW, WJB), by the EU-sponsored One Study (WJB), and by R01# HL115118 (LCD and LS).
Abbreviations
- P2X7R
P2X7 receptor
- Col V
Collagen type V
- TT
Tetanus Toxoid
- EBV
Epstein Barr Virus
- BOS
Bronchiolitis Obliterans Syndrome
- CAV
Cardiac Allograft Vasculopathy
- CAD
Coronary Artery Disease
- oATP
periodate oxidized ATP
- TV-DTH
Trans-vivo delayed type hypersensitivity
Footnotes
AUTHORSHIP CONTRIBUTIONS AND CONFLICTS
J.A. Sullivan designed the research, performed the experiments, analyzed the data and wrote the paper. E. Jankowska-Gan performed experiments, analyzed data and helped write the paper. L. Shi performed experiments and analzyed data. S. Hegde helped design experiments. D. Greenspan provided access to cells from CAD patients enrolled in his atherosclerosis study, and helped design experiments. D.S. Wilkes helped design experiments and provided helpful comments on the manuscript. L.C. Denlinger helped design experiments, provided vital reagents and analyzed data. W.J. Burlingham designed experiments, analyzed data, and helped write the manuscript. David S. Wilkes is a co-founder of ImmuneWorks, Inc., a biotechnology company involved in designing therapeutics for various forms of lung diseases. All other authors have no conflicting interests.
Literature Cited
- 1.Wilhelm K, Ganesan J, Muller T, Durr C, Grimm M, Beilhack A, Krempl CD, Sorichter S, Gerlach UV, Juttner E, Zerweck A, Gartner F, Pellegatti P, Di Virgilio F, Ferrari D, Kambham N, Fisch P, Finke J, Idzko M, Zeiser R. Graft-versus-host disease is enhanced by extracellular ATP activating P2X7R. Nature medicine. 2010;16:1434–1438. doi: 10.1038/nm.2242. [DOI] [PubMed] [Google Scholar]
- 2.Vergani A, Fotino C, D’Addio F, Tezza S, Podetta M, Gatti F, Chin M, Bassi R, Molano RD, Corradi D, Gatti R, Ferrero ME, Secchi A, Grassi F, Ricordi C, Sayegh MH, Maffi P, Pileggi A, Fiorina P. Effect of the purinergic inhibitor oxidized ATP in a model of islet allograft rejection. Diabetes. 2013;62:1665–1675. doi: 10.2337/db12-0242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vergani A, Tezza S, D’Addio F, Fotino C, Liu K, Niewczas M, Bassi R, Molano RD, Kleffel S, Petrelli A, Soleti A, Ammirati E, Frigerio M, Visner G, Grassi F, Ferrero ME, Corradi D, Abdi R, Ricordi C, Sayegh MH, Pileggi A, Fiorina P. Long-term heart transplant survival by targeting the ionotropic purinergic receptor P2X7. Circulation. 2013;127:463–475. doi: 10.1161/CIRCULATIONAHA.112.123653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zeiser R, Penack O, Holler E, Idzko M. Danger signals activating innate immunity in graft-versus-host disease. J Mol Med (Berl) 2011;89:833–845. doi: 10.1007/s00109-011-0767-x. [DOI] [PubMed] [Google Scholar]
- 5.Al-Shukaili A, Al-Kaabi J, Hassan B, Al-Araimi T, Al-Tobi M, Al-Kindi M, Al-Maniri A, Al-Gheilani A, Al-Ansari A. P2X7 receptor gene polymorphism analysis in rheumatoid arthritis. International journal of immunogenetics. 2011;38:389–396. doi: 10.1111/j.1744-313X.2011.01019.x. [DOI] [PubMed] [Google Scholar]
- 6.Killeen ME, Ferris L, Kupetsky EA, Falo L, Jr, Mathers AR. Signaling through purinergic receptors for ATP induces human cutaneous innate and adaptive Th17 responses: implications in the pathogenesis of psoriasis. J Immunol. 2013;190:4324–4336. doi: 10.4049/jimmunol.1202045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Skaper SD, Debetto P, Giusti P. The P2X7 purinergic receptor: from physiology to neurological disorders. FASEB journal: official publication of the Federation of American Societies for Experimental Biology. 2010;24:337–345. doi: 10.1096/fj.09-138883. [DOI] [PubMed] [Google Scholar]
- 8.Dubyak GR. Go it alone no more--P2X7 joins the society of heteromeric ATP-gated receptor channels. Molecular pharmacology. 2007;72:1402–1405. doi: 10.1124/mol.107.042077. [DOI] [PubMed] [Google Scholar]
- 9.Sallusto F, Zielinski CE, Lanzavecchia A. Human Th17 subsets. European journal of immunology. 2012;42:2215–2220. doi: 10.1002/eji.201242741. [DOI] [PubMed] [Google Scholar]
- 10.Acosta-Rodriguez EV, Napolitani G, Lanzavecchia A, Sallusto F. Interleukins 1beta and 6 but not transforming growth factor-beta are essential for the differentiation of interleukin 17-producing human T helper cells. Nature immunology. 2007;8:942–949. doi: 10.1038/ni1496. [DOI] [PubMed] [Google Scholar]
- 11.Yoshida S, Haque A, Mizobuchi T, Iwata T, Chiyo M, Webb TJ, Baldridge LA, Heidler KM, Cummings OW, Fujisawa T, Blum JS, Brand DD, Wilkes DS. Anti-type V collagen lymphocytes that express IL-17 and IL-23 induce rejection pathology in fresh and well-healed lung transplants. American journal of transplantation: official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2006;6:724–735. doi: 10.1111/j.1600-6143.2006.01236.x. [DOI] [PubMed] [Google Scholar]
- 12.Bobadilla JL, Love RB, Jankowska-Gan E, Xu Q, Haynes LD, Braun RK, Hayney MS, Munoz del Rio A, Meyer K, Greenspan DS, Torrealba J, Heidler KM, Cummings OW, Iwata T, Brand D, Presson R, Burlingham WJ, Wilkes DS. Th-17, monokines, collagen type V, and primary graft dysfunction in lung transplantation. American journal of respiratory and critical care medicine. 2008;177:660–668. doi: 10.1164/rccm.200612-1901OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dart ML, Jankowska-Gan E, Huang G, Roenneburg DA, Keller MR, Torrealba JR, Rhoads A, Kim B, Bobadilla JL, Haynes LD, Wilkes DS, Burlingham WJ, Greenspan DS. Interleukin-17-dependent autoimmunity to collagen type V in atherosclerosis. Circulation research. 2010;107:1106–1116. doi: 10.1161/CIRCRESAHA.110.221069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burlingham WJ, Love RB, Jankowska-Gan E, Haynes LD, Xu Q, Bobadilla JL, Meyer KC, Hayney MS, Braun RK, Greenspan DS, Gopalakrishnan B, Cai J, Brand DD, Yoshida S, Cummings OW, Wilkes DS. IL-17-dependent cellular immunity to collagen type V predisposes to obliterative bronchiolitis in human lung transplants. The Journal of clinical investigation. 2007;117:3498–3506. doi: 10.1172/JCI28031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bharat A, Saini D, Steward N, Hachem R, Trulock EP, Patterson GA, Meyers BF, Mohanakumar T. Antibodies to self-antigens predispose to primary lung allograft dysfunction and chronic rejection. The Annals of thoracic surgery. 2010;90:1094–1101. doi: 10.1016/j.athoracsur.2010.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haynes LD, Jankowska-Gan E, Sheka A, Keller MR, Hernandez-Fuentes MP, Lechler RI, Seyfert-Margolis V, Turka LA, Newell KA, Burlingham WJ. Donor-specific indirect pathway analysis reveals a B-cell-independent signature which reflects outcomes in kidney transplant recipients. American journal of transplantation: official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2012;12:640–648. doi: 10.1111/j.1600-6143.2011.03869.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rodriguez DS, Jankowska-Gan E, Haynes LD, Leverson G, Munoz A, Heisey D, Sollinger HW, Burlingham WJ. Immune regulation and graft survival in kidney transplant recipients are both enhanced by human leukocyte antigen matching. American journal of transplantation: official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2004;4:537–543. doi: 10.1111/j.1600-6143.2004.00385.x. [DOI] [PubMed] [Google Scholar]
- 18.Denlinger LC, Sommer JA, Parker K, Gudipaty L, Fisette PL, Watters JW, Proctor RA, Dubyak GR, Bertics PJ. Mutation of a dibasic amino acid motif within the C terminus of the P2X7 nucleotide receptor results in trafficking defects and impaired function. J Immunol. 2003;171:1304–1311. doi: 10.4049/jimmunol.171.3.1304. [DOI] [PubMed] [Google Scholar]
- 19.Denlinger LC, Shi L, Guadarrama A, Schell K, Green D, Morrin A, Hogan K, Sorkness RL, Busse WW, Gern JE. Attenuated P2X7 pore function as a risk factor for virus-induced loss of asthma control. American journal of respiratory and critical care medicine. 2009;179:265–270. doi: 10.1164/rccm.200802-293OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jankowska-Gan E, Hegde S, Burlingham WJ. Trans-vivo Delayed Type Hypersensitivity Assay for Antigen Specific Regulation. Journal of visualized experiments: JoVE. 2013 doi: 10.3791/4454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Keller MR, Haynes LD, Jankowska-Gan E, Sullivan JA, Agashe VV, Burlingham SR, Burlingham WJ. Epitope Analysis of the Collagen Type V-Specific T Cell Response in Lung Transplantation Reveals an HLA-DRB1*15 Bias in Both Recipient and Donor. PloS one. 2013;8:e79601. doi: 10.1371/journal.pone.0079601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hegde S, Jankowska-Gan E, Roenneburg DA, Torrealba J, Burlingham WJ, Gumperz JE. Human NKT cells promote monocyte differentiation into suppressive myeloid antigen-presenting cells. Journal of leukocyte biology. 2009;86:757–768. doi: 10.1189/jlb.0209059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yang C, Park AC, Davis NA, Russell JD, Kim B, Brand DD, Lawrence MJ, Ge Y, Westphall MS, Coon JJ, Greenspan DS. Comprehensive mass spectrometric mapping of the hydroxylated amino acid residues of the alpha1(V) collagen chain. The Journal of biological chemistry. 2012;287:40598–40610. doi: 10.1074/jbc.M112.406850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Surprenant A, Rassendren F, Kawashima E, North RA, Buell G. The cytolytic P2Z receptor for extracellular ATP identified as a P2X receptor (P2X7) Science. 1996;272:735–738. doi: 10.1126/science.272.5262.735. [DOI] [PubMed] [Google Scholar]
- 25.Sallusto F, Lenig D, Mackay CR, Lanzavecchia A. Flexible programs of chemokine receptor expression on human polarized T helper 1 and 2 lymphocytes. The Journal of experimental medicine. 1998;187:875–883. doi: 10.1084/jem.187.6.875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Duhen T, Duhen R, Lanzavecchia A, Sallusto F, Campbell DJ. Functionally distinct subsets of human FOXP3+ Treg cells that phenotypically mirror effector Th cells. Blood. 2012;119:4430–4440. doi: 10.1182/blood-2011-11-392324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Qin S, Rottman JB, Myers P, Kassam N, Weinblatt M, Loetscher M, Koch AE, Moser B, Mackay CR. The chemokine receptors CXCR3 and CCR5 mark subsets of T cells associated with certain inflammatory reactions. The Journal of clinical investigation. 1998;101:746–754. doi: 10.1172/JCI1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sallusto F, Lanzavecchia A, Mackay CR. Chemokines and chemokine receptors in T-cell priming and Th1/Th2-mediated responses. Immunology today. 1998;19:568–574. doi: 10.1016/s0167-5699(98)01346-2. [DOI] [PubMed] [Google Scholar]
- 29.Acosta-Rodriguez EV, Rivino L, Geginat J, Jarrossay D, Gattorno M, Lanzavecchia A, Sallusto F, Napolitani G. Surface phenotype and antigenic specificity of human interleukin 17-producing T helper memory cells. Nature immunology. 2007;8:639–646. doi: 10.1038/ni1467. [DOI] [PubMed] [Google Scholar]
- 30.Annunziato F, Cosmi L, Santarlasci V, Maggi L, Liotta F, Mazzinghi B, Parente E, Fili L, Ferri S, Frosali F, Giudici F, Romagnani P, Parronchi P, Tonelli F, Maggi E, Romagnani S. Phenotypic and functional features of human Th17 cells. The Journal of experimental medicine. 2007;204:1849–1861. doi: 10.1084/jem.20070663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Singh SP, Zhang HH, Foley JF, Hedrick MN, Farber JM. Human T cells that are able to produce IL-17 express the chemokine receptor CCR6. J Immunol. 2008;180:214–221. doi: 10.4049/jimmunol.180.1.214. [DOI] [PubMed] [Google Scholar]
- 32.Zhao F, Hoechst B, Gamrekelashvili J, Ormandy LA, Voigtlander T, Wedemeyer H, Ylaya K, Wang XW, Hewitt SM, Manns MP, Korangy F, Greten TF. Human CCR4+ CCR6+ Th17 cells suppress autologous CD8+ T cell responses. J Immunol. 2012;188:6055–6062. doi: 10.4049/jimmunol.1102918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Turtle CJ, Delrow J, Joslyn RC, Swanson HM, Basom R, Tabellini L, Delaney C, Heimfeld S, Hansen JA, Riddell SR. Innate signals overcome acquired TCR signaling pathway regulation and govern the fate of human CD161(hi) CD8alpha(+) semi-invariant T cells. Blood. 2011;118:2752–2762. doi: 10.1182/blood-2011-02-334698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lasiglie D, Traggiai E, Federici S, Alessio M, Buoncompagni A, Accogli A, Chiesa S, Penco F, Martini A, Gattorno M. Role of IL-1 beta in the development of human T(H)17 cells: lesson from NLPR3 mutated patients. PloS one. 2011;6:e20014. doi: 10.1371/journal.pone.0020014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gu BJ, Zhang WY, Bendall LJ, Chessell IP, Buell GN, Wiley JS. Expression of P2X(7) purinoceptors on human lymphocytes and monocytes: evidence for nonfunctional P2X(7) receptors. American journal of physiology. Cell physiology. 2000;279:C1189–1197. doi: 10.1152/ajpcell.2000.279.4.C1189. [DOI] [PubMed] [Google Scholar]
- 36.Schenk U, Westendorf AM, Radaelli E, Casati A, Ferro M, Fumagalli M, Verderio C, Buer J, Scanziani E, Grassi F. Purinergic control of T cell activation by ATP released through pannexin-1 hemichannels. Science signaling. 2008;1:ra6. doi: 10.1126/scisignal.1160583. [DOI] [PubMed] [Google Scholar]
- 37.Vittal R, Fan L, Greenspan DS, Mickler EA, Gopalakrishnan B, Gu H, Benson HL, Zhang C, Burlingham W, Cummings OW, Wilkes DS. IL-17 induces type V collagen overexpression and EMT via TGF-beta-dependent pathways in obliterative bronchiolitis. American journal of physiology. Lung cellular and molecular physiology. 2013;304:L401–414. doi: 10.1152/ajplung.00080.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hyman MC, Petrovic-Djergovic D, Visovatti SH, Liao H, Yanamadala S, Bouis D, Su EJ, Lawrence DA, Broekman MJ, Marcus AJ, Pinsky DJ. Self-regulation of inflammatory cell trafficking in mice by the leukocyte surface apyrase CD39. The Journal of clinical investigation. 2009;119:1136–1149. doi: 10.1172/JCI36433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Peng W, Cotrina ML, Han X, Yu H, Bekar L, Blum L, Takano T, Tian GF, Goldman SA, Nedergaard M. Systemic administration of an antagonist of the ATP-sensitive receptor P2X7 improves recovery after spinal cord injury. Proceedings of the National Academy of Sciences of the United States of America. 2009;106:12489–12493. doi: 10.1073/pnas.0902531106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rassendren F, Buell GN, Virginio C, Collo G, North RA, Surprenant A. The permeabilizing ATP receptor, P2X7. Cloning and expression of a human cDNA. The Journal of biological chemistry. 1997;272:5482–5486. doi: 10.1074/jbc.272.9.5482. [DOI] [PubMed] [Google Scholar]
- 41.Martinon F, Mayor A, Tschopp J. The inflammasomes: guardians of the body. Annual review of immunology. 2009;27:229–265. doi: 10.1146/annurev.immunol.021908.132715. [DOI] [PubMed] [Google Scholar]
- 42.Qu Y, Franchi L, Nunez G, Dubyak GR. Nonclassical IL-1 beta secretion stimulated by P2X7 receptors is dependent on inflammasome activation and correlated with exosome release in murine macrophages. J Immunol. 2007;179:1913–1925. doi: 10.4049/jimmunol.179.3.1913. [DOI] [PubMed] [Google Scholar]
- 43.Jankovic D, Ganesan J, Bscheider M, Stickel N, Weber FC, Guarda G, Follo M, Pfeifer D, Tardivel A, Ludigs K, Bouazzaoui A, Kerl K, Fischer JC, Haas T, Schmitt-Graff A, Manoharan A, Muller L, Finke J, Martin SF, Gorka O, Peschel C, Ruland J, Idzko M, Duyster J, Holler E, French LE, Poeck H, Contassot E, Zeiser R. The Nlrp3 inflammasome regulates acute graft-versus-host disease. The Journal of experimental medicine. 2013;210:1899–1910. doi: 10.1084/jem.20130084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Haque MA, Mizobuchi T, Yasufuku K, Fujisawa T, Brutkiewicz RR, Zheng Y, Woods K, Smith GN, Cummings OW, Heidler KM, Blum JS, Wilkes DS. Evidence for immune responses to a self-antigen in lung transplantation: role of type V collagen-specific T cells in the pathogenesis of lung allograft rejection. J Immunol. 2002;169:1542–1549. doi: 10.4049/jimmunol.169.3.1542. [DOI] [PubMed] [Google Scholar]
- 45.Yasufuku K, Heidler KM, O’Donnell PW, Smith GN, Jr, Cummings OW, Foresman BH, Fujisawa T, Wilkes DS. Oral tolerance induction by type V collagen downregulates lung allograft rejection. American journal of respiratory cell and molecular biology. 2001;25:26–34. doi: 10.1165/ajrcmb.25.1.4431. [DOI] [PubMed] [Google Scholar]
- 46.Lubberts E, Koenders MI, van den Berg WB. The role of T-cell interleukin-17 in conducting destructive arthritis: lessons from animal models. Arthritis research & therapy. 2005;7:29–37. doi: 10.1186/ar1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.