Abstract
Objectives
To estimate the incidence of hypertension in people with and without prehypertension and determine the factors that predict progression to hypertension.
Methods
Data from a cohort of 25–74-year old residents of Spanish Town, Jamaica, were analysed. All participants completed a structured questionnaire and had blood pressure (BP), anthropometric measurements and venous blood sampling performed by trained personnel. Blood Pressure was classified using the Seventh Report of the Joint National Committee on the Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC-7) criteria.
Results
708 persons who had the required data and were not hypertensive at baseline were included in this analysis. Mean follow-up time was 4.1 years; 28.7% of prehypertensive participants developed hypertension compared to 6.2% of normotensive participants. The unadjusted incidence rate ratio (IRR [95% CI]) for progression among prehypertensive compared to normotensive participants was 4.62[2.96, 7.43].
Among males, the rate of progression to hypertension was significantly higher for those 45–64 years old and those who were current smokers. Among females, progression was higher for age groups 25–44 years, 45–64 years, those who were overweight (BMI ≥ 25), obese (BMI ≥ 30) and current smokers. In multivariate models, prehypertension, female gender, overweight status and older age remained significantly associated with progression to hypertension among the combined prehypertensive and normotensive groups. IRR [95% CI] were: prehypertension, 3.45 [2.18–5.45]; female gender, 1.81 [1.12, 2.94]; overweight, 1.87 [1.15, 2.94]; age 45–64 years, 1.73 [1.08, 2.76]; age ≥ 65 years 2.39 [1.31, 4.34].
Conclusions
Prehypertension is associated with a three-fold increase in the incidence of hypertension. Higher BMI, age and female gender also independently predict the development of hypertension.
Keywords: Caribbean, cardiovascular disease, incident hypertension, Jamaica, prehypertension
INTRODUCTION
The prevalence of prehypertension, as defined by the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure [JNC 7] (1), ranges between 30% and 47% in population-based studies (2–8). Prehypertension is also associated with cardiovascular risk factors such as diabetes mellitus, overweight/ obesity, hypercholesterolaemia, elevated C-reactive protein, left ventricular hypertrophy and increased carotid intima-media thickness (9–14).
Prior to the publication of the JNC 7, a number of studies reported an increased risk of cardiovascular disease and mortality among persons with blood pressure readings in the range now defined as prehypertension (15–17). In one study, Vasan and colleagues analysed data from over 9000 participants from the Framingham cohort who were between 35 and 94 years at baseline, and found that the rate of progression to hypertension over a four-year follow-up period was significantly higher among persons with blood pressure readings in the prehypertensive range, compared to those who had normal blood pressure (18). Among persons with blood pressure in the prehypertensive range, the cumulative incidence of hypertension over four years was between 17.6% and 49.5%, while among normotensive persons, the cumulative incidence was between 5.3% and 16.0% (18). More recently, Julius and colleagues found a cumulative incidence of 63% at four years among persons with prehypertension in the placebo arm of the Trial of Preventing Hypertension (TROPHY) study (19). To date, only a few other studies (19–24) have reported the rate of progression to hypertension among prehypertensive persons using JNC 7 criteria. All of these studies have examined the progression to hypertension among Caucasian or Asian populations in developed countries. Very little is known about the impact of this condition in a black population and how living in a developing country might affect the natural history of the disease.
The aim of this study was to estimate the incidence rate of hypertension among prehypertensive participants, compared to normotensive participants, in a predominantly black cohort from Spanish Town, Jamaica, and to evaluate whether prehypertension and other cardiovascular disease (CVD) risk factors, in particular, age, obesity and diabetes mellitus, would independently predict the development of hypertension in this population.
SUBJECTS AND METHODS
The study was conducted using the data from an ongoing cohort study in Spanish Town, Jamaica. This study was initiated in 1993 as part of an international study of hypertension, diabetes mellitus and chronic disease in people of African ancestry (25–27). Spanish Town was chosen because its population structure was considered as being most representative of urban Jamaica. The town lies 15 miles west of the capital city, Kingston and had a population of approximately 110 000 in 1993. A stratified sample of men and non-pregnant women, 25 to74 years old, were recruited by door-to-door solicitation of eligible residents in randomly selected enumeration districts. Enumeration districts were selected using a probability proportionate to size method with larger districts being more likely to be selected. From January 1993 to January 1998, two thousand and ninety-six (2 096) persons were enrolled in the study. The data for this report compares findings at initial recruitment and at first follow-up evaluation of 1131 persons seen up to December 2002. The protocol was reviewed and approved by the Ethics Committee of the Faculty of Medical Sciences, University of the West Indies/University Hospital of the West Indies, Kingston, Jamaica.
At baseline, participants completed an interviewer-administered questionnaire covering personal, medical, social and family history. All measurements were obtained by trained personnel using standardized procedures (25). Blood pressure (BP) was measured with a mercury sphygmomanometer to the nearest 2 mmHg using the first (systolic) and fifth (diastolic) Korotkoff phases. Three measurements were taken at one-minute intervals in the sitting position after the participant had been sitting for five minutes. The mean of the last two of the three readings was used for the analysis. Weight was measured in kilograms using digital scales which were calibrated daily. Height was measured in centimetres using a portable height rod. Waist circumference was measured at the smallest horizontal circumference between the ribs and the iliac crest, and hip circumference at the point of maximal extension of the buttocks. All anthropometric measurements were made without shoes and with the participant wearing only light clothing. Body mass index (BMI) was calculated as weight in kilograms (kg) divided by the square of the height in metres. Fasting venous blood was collected and a blood sample for glucose was obtained two hours after a 75 g oral glucose load.
A follow-up evaluation was conducted on average four years after the baseline visit. This included questionnaire administration and measurement of BP, height, weight, waist circumference and hip circumference performed as above.
Prehypertension was defined according to JNC 7 criteria as having either a systolic blood pressure of 120 to 139 mmHg and/or diastolic blood pressure of 80 to 89 mmHg in persons who were not on treatment for hypertension. Hypertension was also defined according to JNC 7 criteria as having an untreated systolic blood pressure (BP) of greater than or equal to 140 mmHg or diastolic BP greater than or equal to 90 mmHg or being on medication for hypertension. Normal blood pressure was defined as having both a systolic BP of < 120 mmHg and a diastolic BP of < 80 mmHg in the absence of antihypertensive medication.
Diabetes mellitus was defined according to the American Diabetes Association 1997 criteria (28) as fasting glucose ≥ 7.0 mmol/L or two-hour post challenge glucose of ≥ 11.1 mmol/L or taking medication for diabetes mellitus. Overweight was defined as a BMI greater than or equal to 25 kg/m2, while obesity was defined as BMI greater than or equal to 30 kg/m2 (29). Increased (high-risk) waist circumference was defined as recommended by Lean et al (30) as greater than or equal to 94 cm in men and greater than or equal to 80 cm in women. Increased waist-to-hip ratio was defined as greater than or equal to 0.95 for males and greater than or equal to 0.80 for females.
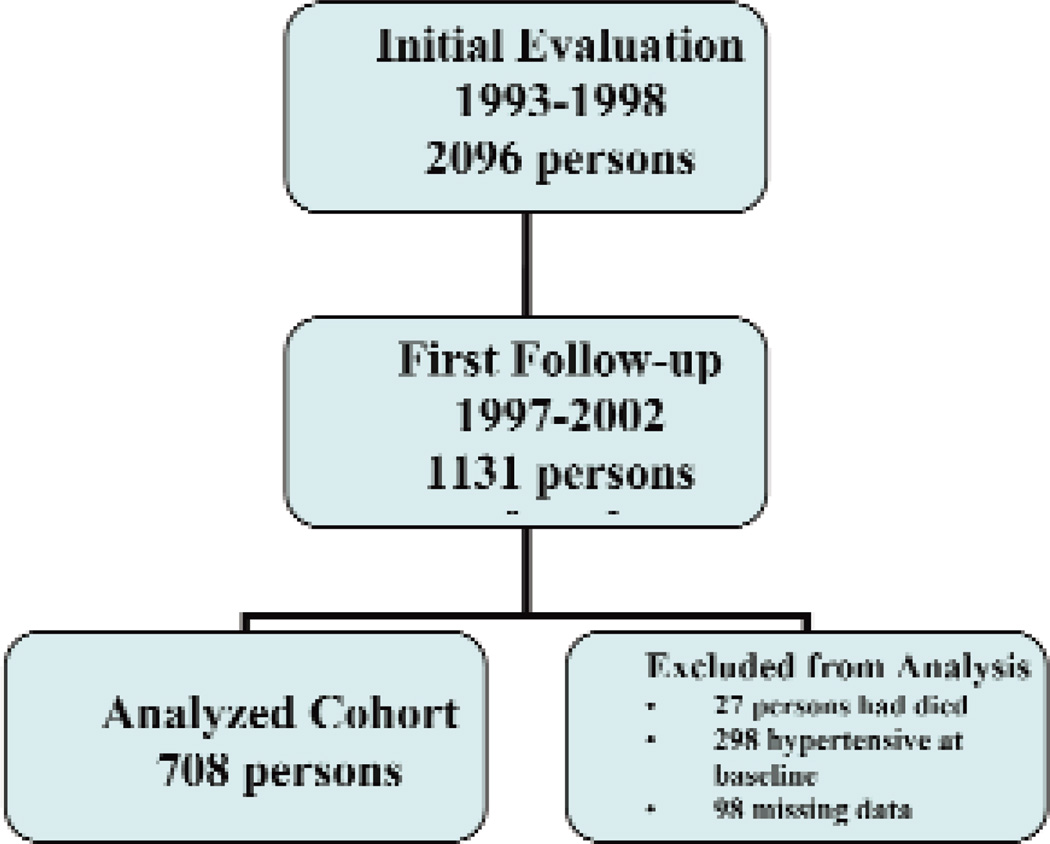
Statistical analyses were performed using Stata 10.0 (31). For this analysis, only persons with BP measurements at baseline and follow-up were included (Figure). Participants were classified into BP categories using the JNC 7 criteria as normotensive, prehypertensive or hypertensive based on their baseline BP. Participants who had hypertension at baseline were excluded from further analysis. Baseline characteristics of study participants by gender and BP categories were described using summary statistics. Time spent at risk was calculated as the time elapsed between the baseline and follow-up visit. Crude and category-specific incidence rates and rate ratios were calculated for progression to hypertension for participants who were normotensive and prehypertensive at baseline. Chi-squared tests, where appropriate, and Fisher’s exact tests were used to assess the statistical significance of the association of progression to hypertension with different baseline risk states. Poisson regression models were developed to determine factors which predicted the incidence rates for development of hypertension among study participants.
Figure.
Flow Diagram for persons included and excluded in the Spanish Town Prehypertension Progression Cohort.
RESULTS
Data from 708 persons, who were not hypertensive at baseline, had at least one follow-up visit and had complete data on the variables of interest, were analysed (Figure). The baseline characteristics of the participants according to gender are shown in Table 1. Men had higher mean age, while women had a higher mean weight, BMI, waist circumference, heart rate and two-hour post-challenge glucose. There were no significant gender differences in mean systolic blood pressure, diastolic blood pressure or fasting glucose. Baseline characteristics for participants included in the analysis and those excluded were also compared (data not shown). Except for a higher mean age (three years) and higher mean systolic blood pressure (2 mmHg), the baseline characteristics for participants used for the analysis were similar to those of the participants who were excluded.
Table 1.
Summary statistics for baseline characteristics of the participants included in the study by gender
| Males n = 275 |
Females n = 473 |
p-value M:F difference |
|||
|---|---|---|---|---|---|
| Baseline Characteristics | Mean | Standard Deviation |
Mean | Standard Deviation |
|
| Age (years) | 45.9 | 13.8 | 43.6 | 12.5 | 0.030 |
| BMI (kg/m2) | 23.3 | 4.0 | 27.6 | 6.4 | < 0.001 |
| Waist Circumference (cm) | 79.5 | 11.2 | 82.5 | 12.6 | 0.001 |
| Waist to Hip Ratio | 0.83 | 0.06 | 0.79 | 0.06 | < 0.001 |
| Weight (kg) | 69.4 | 13.4 | 71.7 | 17.4 | 0.048 |
| Systolic Blood Pressure (mmHg) | 114.8 | 12.1 | 113.0 | 12.6 | 0.053 |
| Diastolic Blood Pressure (mmHg) | 66.5 | 10.3 | 65.8 | 10.9 | 0.381 |
| Heart Rate (beats/minute) | 67.6 | 9.9 | 74.5 | 9.2 | < 0.001 |
| Fasting Glucose (mmol/L) | 5.2 | 1.7 | 5.4 | 2.2 | 0.233 |
| 2hr Post Challenge Glucose (mmol/L) | 6.1 | 3.1 | 7.1 | 3.6 | < 0.001 |
Table 2 shows the proportion of men and women with selected cardiovascular disease (CVD) risk factors. More women than men were grouped in the high CVD risk categories. For example, 63.5% of women were overweight or obese (BMI ≥ 25kg/m2) compared to 27.6% of men; similarly 10.9% of women had diabetes mellitus compared to 6.9% of men. Cigarette smoking was more frequent among men, with 34.9% being current smokers and 24% being past smokers, compared to 14.6% and 5.7% for females. Table 3 shows the proportions of the same CVD risk factors by blood pressure category for men and women separately. In both genders, participants with prehypertension had a higher prevalence of obesity (overall and central) as well as diabetes mellitus. There were no differences in smoking status by blood pressure category.
Table 2.
Proportions (%) of participants with selected cardiovascular disease risk factors at baseline by sex
| Males N = 275 |
Females N = 473 |
P-value M:F difference |
|||
|---|---|---|---|---|---|
| Baseline Characteristics | Proportion % |
Standard Error |
Mean | Standard Error |
|
| Overweight (BMI ≥ 25kg/m2) | 27.6 | 2.7 | 63.5 | 2.3 | < 0.001 |
| Obese (BMI ≥ 30kg/m2) | 6.9 | 1.5 | 28.2 | 2.2 | < 0.001 |
| High Waist Circumference* | 11.6 | 1.9 | 53.5 | 2.4 | < 0.001 |
| High Waist-to-Hip Ratio** | 4.3 | 1.2 | 43.4 | 2.3 | < 0.001 |
| Diabetes Mellitus | 6.9 | 1.5 | 10.9 | 1.5 | 0.078 |
| Cigarette Smoking (Current) | 34.9 | 2.9 | 14.6 | 1.7 | < 0.001 |
| Cigarette Smoking (Past) | 24.0 | 2.6 | 5.7 | 1.1 | |
High waist circumference: males ≥ 94 cm; females ≥ 80 cm
High waist-to-hip ratio: males ≥ 0.95; females ≥ 0.80
Table 3.
Sex-specific proportions of cardiovascular disease risk factors at baseline by blood pressure category
| Normal BP* n = 454 |
Prehypertension* n = 254 |
P-value Difference by BP category |
||||
|---|---|---|---|---|---|---|
| Baseline Characteristics | Proportion % |
Standard Error |
Proportion % |
Standard Error |
||
| Men | ||||||
| Overweight (BMI ≥25 kg/m2) | 21.0 | 3.2 | 38.0 | 4.6 | 0.002 | |
| Obese (BMI ≥ 30 kg/m2) | 4.7 | 1.6 | 10.1 | 2.9 | 0.085 | |
| High Waist Circumference | 8.3 | 2.2 | 16.7 | 3.6 | 0.036 | |
| High Waist-to-Hip Ratio | 2.4 | 1.1 | 7.4 | 2.5 | 0.047 | |
| Diabetes Mellitus | 3.0 | 1.3 | 13.0 | 3.2 | 0.001 | |
| Cigarette Smoking (Current) | 35.9 | 3.7 | 33.3 | 4.5 | 0.498** | |
| Cigarette Smoking (Past) | 21.6 | 3.2 | 27.8 | 4.3 | ||
| Women | ||||||
| Overweight (BMI ≥ 25 kg/m2) | 57.4 | 2.9 | 75.3 | 3.6 | < 0.001 | |
| Obese (BMI ≥ 30 kg/m2) | 23.7 | 2.5 | 37.0 | 4.0 | 0.004 | |
| High Waist Circumference | 47.7 | 2.9 | 65.1 | 4.0 | 0.001 | |
| High Waist-to-Hip Ratio | 38.0 | 2.8 | 54.1 | 4.1 | 0.001 | |
| Diabetes Mellitus | 7.0 | 1.5 | 18.5 | 3.2 | < 0.001 | |
| Cigarette Smoking (Current) | 15.6 | 2.1 | 12.3 | 2.7 | 0.638** | |
| Cigarette Smoking (Past) | 5.6 | 1.3 | 6.1 | 1.9 | ||
BP = Blood pressure
Normal BP ≤ 120/80 mmHg; Prehypertension = 120–139/80–89 mmHg
P-value for differences between BP groups for both current and past smokers
The mean time between the baseline and follow-up visit for the participants was 4.1 years (range, 1.3–6.4 years). The incidence rate for hypertension among persons who were prehypertensive was 70.4 per 1000 person-years while that for normotensive individuals was 15.2 per 1000 person-years. The cumulative incidence of hypertension over a mean follow-up period of four years among prehypertensive persons was 28.7% (95% confidence interval [CI] 23.2, 34.3) while cumulative incidence for normotensive persons was 6.2% (95% CI 3.9, 8.4).
Incidence rates and rate ratios for possible predictors of progression to hypertension in univariate analyses are shown in Table 4. Prehypertension was associated with a four-fold increase in risk of progression to hypertension compared to persons with normal blood pressure at baseline [incidence rate ratio (IRR) was 4.62 (95% CI 2.96,7.43, p < 0.001]. This was true for both genders, IRR 4.63 for males and 4.87 for females. Rates of progression to hypertension for prehypertensive persons compared to normotensive persons were also compared within sub-groups of age, BMI, diabetes mellitus and cigarette smoking. Among males, IRR for progression to hypertension was significantly higher for prehypertension compared to normal BP only for age category 45–64 years (IRR 4.13) and current smoking (IRR 6.09). Among females, the IRR for progression to hypertension was significantly higher for prehypertension compared to normal BP for age groups 25–44 years (IRR 7.85) and 45–64 years (IRR 3.36), overweight (IRR 3.46), obesity (IRR 2.56) and current smoking (IRR 20.66).
Table 4.
Crude and sex-specific incidence rates and rate ratios for progression to hypertension from prehypertension or normal blood pressure within and across categories of cardiovascular disease risk factors
| From Normal Blood Pressure* n = 454 |
From Prehypertension* n = 254 |
Rate Ratio (Confidence Intervals) |
p-value | ||
|---|---|---|---|---|---|
| Males | |||||
| 25–44 year-olds | 5.1 | 6.4 | 1.26 (0.02 – 24.36) | 0.855 | |
| 45–64year-olds | 14.1 | 58.1 | 4.13 (1.09 – 23.05 | 0.032 | |
| 65 yrs and older | 14.4 | 63.6 | 4.42 (0.54 – 203.34) | 0.150 | |
| Overweight (BMI ≥ 25.0 kg/m2) | 13.8 | 48.0 | 3.46 (0.69 – 33.47) | 0.104 | |
| Obese (BMI ≥ 30 kg/m2) | 31.2 | – | – | – | |
| Diabetes Mellitus | 51.2 | 88.5 | 1.73 (0.19 – 81.77) | 0.686 | |
| Cigarette Smoking (Current) | 7.9 | 48.3 | 6.09 (1.15 – 60.06) | 0.016 | |
| Cigarette Smoking (Past) | 21.0 | 8.2 | 0.39 (0.01 – 4.89) | 0.462 | |
| All Males | 8.9 | 41.0 | 4.63 | 0.001 | |
| Females | |||||
| 25–44 year-olds | 10.6 | 83.5 | 7.85 (3.28 – 20.73) | < 0.001 | |
| 45–64year-olds | 28.9 | 94.4 | 3.36 (1.52 – 7.58) | 0.001 | |
| 65 yrs and older | 61.1 | 105.7 | 1.73 (0.50 – 7.56) | 0.367 | |
| Overweight (BMI ≥ 25.0 kg/m2) | 28.6 | 99.2 | 3.46 (1.99 – 6.28) | < 0.001 | |
| Obese (BMI ≥ 30 kg/m2) | 39.6 | 101.6 | 2.56 (1.19 – 5.82) | 0.009 | |
| Diabetes Mellitus | 100.5 | 95.4 | 0.95 (0.35 – 2.72) | 0.902 | |
| Cigarette Smoking (Current) | 5.4 | 113.6 | 20.66 (2.77 – 916.76) | < 0.001 | |
| Cigarette Smoking (Past) | 14.8 | 85.4 | 5.79 (0.46 – 303.78) | 0.132 | |
| All Females | 18.9 | 92.0 | 4.87 (2.92 – 8.38) | < 0.001 | |
| Total (males and females) | 15.2 | 70.4 | 4.62 (2.96 – 7.43) | < 0.001 | |
Incidence Rate per 1000 person-years
Normal BP ≤ 120/80 mmHg; Prehypertension = 120–139/80–89 mmHg
Poisson regression models were used to evaluate factors which were independent predictors of progression to hypertension among the combined prehypertension and normal blood pressure groups. Baseline blood pressure category, age-group in 20-year bands, gender, BMI, diabetes mellitus and cigarette smoking were hypothesized potential predictors and were included in the initial models. The final model excluded smoking, based on post-estimation model statistics. Estimates presented were adjusted for blood pressure, age, gender, overweight status and diabetes mellitus (Table 5). After adjustments, prehypertension was associated test indicates that the proportion who returned to normal BP was significantly lower (p = 0.005) than the proportion who progressed to hypertension.
Table 5.
Factors, determined from Poisson regression models*, which predict the rate of progression to hypertension
| Incidence Rate Ratio |
95% Confidence Interval |
p-Value | ||
|---|---|---|---|---|
| Blood Pressure (compared to normal BP) | ||||
| Prehypertension | 3.45 | 2.18 – 5.45 | < 0.001 | |
| Age Group (compared to 15–34 Years) | ||||
| 45–64 Years | 1.73 | 1.08 – 2.76 | 0.022 | |
| ≥ 65 Years | 2.39 | 1.31 – 4.34 | 0.004 | |
| Body Mass Index (compared to not overweight) | ||||
| Overweight (BMI ≥ 25) | 1.87 | 1.15 – 3.03 | 0.011 | |
| Sex (compared to males) | ||||
| Females | 1.81 | 1.12 – 2.94 | 0.016 | |
| Diabetes Mellitus (compared to not diabetic at baseline) | ||||
| Diabetic at baseline | 1.58 | 0.98 – 2.57 | 0.058 | |
All variables in the table were includes in a single model; incidence rate ratios are adjusted for all other variables in the table.
DISCUSSION
Higher systolic and/or diastolic blood pressure have been reported to predict the future development of hypertension in a number of studies (18, 32–35). We report similar findings in this study and found that the incidence of hypertension in persons with prehypertension is more than three times higher with a greater than three-fold increase in the risk of progression to hypertension (IRR 3.45, p < 0.001) compared to persons with normal blood pressure. Older age was also associated with increased risk of progression to hypertension, IRR 1.73 for age 45–64 years and 2.39 for age ≥ 65 years respectively, compared to age group 25–44 years. In addition, female gender (IRR 1.81) and overweight status (IRR 1.87) were also predictors of progression to hypertension. The IRR for diabetes mellitus was 1.58 but this did not achieve statistical significance.
Approximately 21% of persons who where prehypertensive at baseline had their blood pressure reverting to normal at follow-up. Table 6 shows the blood pressure outcome status with proportions and 95% confidence intervals for prehypertensive persons in the study. The absence of considerable overlap between the confidence intervals suggests that the proportions differ significantly. The exact binomial than in persons with normal blood pressure and is independent of the effect of other CVD risk factors. Age, female gender and overweight status also independently predicted the development of hypertension. Persons with prehypertension had a greater burden of CVD risk factors than persons with normal blood pressure in this study.
Table 6.
Blood pressure status, at first follow-up of subjects who were prehypertensive at baseline
| Blood Pressure Outcome | Frequency | Percent | 95% CI | |
|---|---|---|---|---|
| Remained Prehypertensive | 128 | 50.4 | 44.2 – 56.7 | |
| Returned to Normotension | 53 | 20.9 | 15.8 – 25.9 | |
| Progressed to Hypertension | 73 | 28.7 | 23.1 – 34.3 | |
| Total | 254 | 100 | ||
These findings are generally consistent with the current literature, including studies using JNC 7 criteria for blood pressure classification, and are among the first studies to demonstrate this in a black population in a developing country. Grossman and colleagues (22) reported an odds ratio of 3.7 for progression to hypertension among prehypertensive male aviators when compared to those with normal BP. In another study, using JNC 6 criteria (18), “normal BP” (systolic BP 120–129 mm Hg and diastolic BP 80–84 mm Hg) was associated with a two-fold to four-fold increase in the risk of hypertension; while “high normal BP” (systolic BP 130–139 mm Hg and diastolic BP 85–89 mm Hg) was associated with a five-fold to twelve-fold increase in the risk of hypertension. With regards to predictors of progression, age and obesity have been consistently found to predict future development of hypertension. Female gender has been found to predict development of hypertension in some studies (33, 35) but others have found no gender differences (18, 36). The finding of a three-fold increased risk of hypertension among persons in the prehypertension category supports the JNC 7 definition of normal BP and the need to consider persons in the prehypertension category as being at higher cardiovascular risk, especially in light of previous studies which have reported an increased prevalence of cardiovascular risk factors and cardiovascular morbidity (5, 9, 11) among prehypertensive persons.
Most of the studies reporting on the incidence of hypertension have used the cumulative incidence as the main measure of risk. The periods of follow-up in these studies varied widely, from four up to twenty-six years. In the present study, incidence rate was used as the main measure or risk. This measure was chosen as there was a relatively wide variation in the duration of follow-up (1.3–6.4 years). However, the estimates of relative risk obtained in this study was still similar to that reported in other studies supporting the validity of the findings. In addition, the estimated incidence rate ratio using the four-year cumulative incidence was similar to that obtained using the incidence rate. It is noteworthy that the cumulative incidence figures for this study were generally similar to those for persons 35 to 64 years in a report from the Framingham Study (18).
This study is limited by the fact that in both baseline and follow-up studies, the categorization of blood pressure was based on a single encounter. However, any misclassification due to this single encounter measurement is likely to be non-differential and thus would bias towards no effect being seen. This would result in a reduction of the estimated relative risk. The finding of a statistically significant association is therefore likely to be valid. The study is also limited by the fact that there was follow-up data on only 54% of the original cohort and data could only be analysed for only 45% of those who were not hypertensive at baseline. However, except for marginally higher age and blood pressure, participants used for the analysis had similar baseline characteristics to those excluded. Any bias introduced by this loss to follow-up is likely to be small and would likely not significantly alter the findings. The consistency of the findings with other studies also supports their validity.
The finding of 21% reversion to normal blood pressure from the prehypertensive group is noteworthy and may have more than one explanation. Of note, a similar finding was reported by Chiu and colleagues (21). This may represent natural phenomenon as seen in pre-diabetes (37) and would raise the provocative question as to whether these persons should be left alone. Such a position must be weighed against the demonstrated significantly increased risk of target organ damage among persons with prehypertension (11, 14, 38). The higher proportion of persons progressing to hypertension compared to those reverting to normal BP supports the view that this prehypertension category connotes a net increase in risk. Another possible explanation derives from the inadequacy of classifying individuals’ BP based on a single measurement encounter and supports the recommendation that clinical decision-making should be based on measurements of BP on at least two encounters.
In summary, prehypertension is associated with a threefold increase in the incidence of hypertension over an average four-year follow-up period. Overweight status, older age and female gender were also significant predictors for the development of hypertension. This study supports the recommendation that persons with prehypertension should be considered as having an increased risk of cardiovascular disease and should be targeted for lifestyle or other interventions to reduce this risk.
ACKNOWLEDGEMENTS
This study was funded by grants from the NIH (PHS Grant #R01 HL53353), the European Commission and the Wellcome Trust. The authors wish to acknowledge the contributions of the research nurses, laboratory staff and administrative staff of the TMRI and the study participants, to this study.
REFERENCES
- 1.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 2.Wang Y, Wang QJ. The prevalence of prehypertension and hypertension among US adults according to the new joint national committee guidelines: new challenges of the old problem. Arch Intern Med. 2004;164:2126–2134. doi: 10.1001/archinte.164.19.2126. [DOI] [PubMed] [Google Scholar]
- 3.Yu D, Huang J, Hu D, Chen J, Cao J, Li J, et al. Prevalence and risk factors of prehypertension among Chinese adults. J Cardiovasc Pharmacol. 2008;52:363–368. doi: 10.1097/FJC.0b013e31818953ac. [DOI] [PubMed] [Google Scholar]
- 4.Tsai PS, Ke TL, Huang CJ, Tsai JC, Chen PL, Wang SY, et al. Prevalence and determinants of prehypertension status in the Taiwanese general population. J Hypertens. 2005;23:1355–1360. doi: 10.1097/01.hjh.0000173517.68234.c3. [DOI] [PubMed] [Google Scholar]
- 5.Ferguson TS, Younger NO, Tulloch-Reid MK, Lawrence Wright MB, Ward EM, Ashley DE, et al. Prevalence of prehypertension and its relationship to risk factors for cardiovascular disease in Jamaica: analysis from a cross-sectional survey. BMC Cardiovasc Disord. 2008;8:20. doi: 10.1186/1471-2261-8-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choi KM, Park HS, Han JH, Lee JS, Lee J, Ryu OH, et al. Prevalence of prehypertension and hypertension in a Korean population: Korean National Health and Nutrition Survey 2001. J Hypertens. 2006;24:1515–1521. doi: 10.1097/01.hjh.0000239286.02389.0f. [DOI] [PubMed] [Google Scholar]
- 7.Agyemang C, Owusu-Dabo E. Prehypertension in theAshanti region of Ghana, West Africa: An opportunity for early prevention of clinical hypertension. Public Health. 2008;122:19–24. doi: 10.1016/j.puhe.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 8.Sun Z, Zheng L, Wei Y, Li J, Zhang X, Zhang X, et al. Prevalence and risk factors of the rural adult people prehypertension status in Liaoning Province of China. Circ J. 2007;71:550–553. doi: 10.1253/circj.71.550. [DOI] [PubMed] [Google Scholar]
- 9.Greenlund KJ, Croft JB, Mensah GA. Prevalence of heart disease and stroke risk factors in persons with prehypertension in the United States, 1999–2000. Arch Intern Med. 2004;164:2113–2118. doi: 10.1001/archinte.164.19.2113. [DOI] [PubMed] [Google Scholar]
- 10.Manios E, Tsivgoulis G, Koroboki E, Stamatelopoulos K, Papamichael C, Toumanidis S, et al. Impact of Prehypertension on Common Carotid Artery Intima-Media Thickness and Left Ventricular Mass. Stroke. 2009 doi: 10.1161/STROKEAHA.108.528174. [DOI] [PubMed] [Google Scholar]
- 11.Liszka HA, Mainous AG, King DE, III, Everett CJ, Egan BM. Prehypertension and cardiovascular morbidity. Ann Fam Med. 2005;3:294–299. doi: 10.1370/afm.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.King DE, Egan BM, Mainous AG, Geesey ME., III Elevation of C-reactive protein in people with prehypertension. J Clin Hypertens (Greenwich) 2004;6:562–568. doi: 10.1111/j.1524-6175.2004.03577.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lawrence Wright MB, Devereux RB, Roman MJ, Chinali M, Best LG, Galloway J, et al. Association of Prehypertension by Joint National Committee 7 Criteria with Left Ventricular Structure and Function: The Strong Heart Study. J Am Coll Cardiol. 2004 Mar 3;43(5) Supplement A:513A. [Google Scholar]
- 14.Washio M, Tokunaga S, Yoshimasu K, Kodama H, Liu Y, Sasazuki S, et al. Role of prehypertension in the development of coronary atherosclerosis in Japan. J Epidemiol. 2004;14:57–62. doi: 10.2188/jea.14.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 16.MacMahon S, Peto R, Cutler J, Collins R, Sorlie P, Neaton J, et al. Blood pressure, stroke, and coronary heart disease. Part 1, Prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet. 1990;335:765–774. doi: 10.1016/0140-6736(90)90878-9. [DOI] [PubMed] [Google Scholar]
- 17.Vasan RS, Larson MG, Leip EP, Evans JC, O’Donnell CJ, Kannel WB, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med. 2001;345:1291–1297. doi: 10.1056/NEJMoa003417. [DOI] [PubMed] [Google Scholar]
- 18.Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet. 2001;358:1682–1686. doi: 10.1016/S0140-6736(01)06710-1. [DOI] [PubMed] [Google Scholar]
- 19.Julius S, Nesbitt SD, Egan BM, Weber MA, Michelson EL, Kaciroti N, et al. Feasibility of treating prehypertension with an angiotensin-receptor blocker. N Engl J Med. 2006;354:1685–1697. doi: 10.1056/NEJMoa060838. [DOI] [PubMed] [Google Scholar]
- 20.Tomiyama H, Matsumoto C, Yamada J, Yoshida M, Odaira M, Shiina K, et al. Predictors of Progression From Prehypertension to Hypertension in Japanese Men. Am J Hypertens. 2009 doi: 10.1038/ajh.2009.49. [DOI] [PubMed] [Google Scholar]
- 21.Chiu YH, Wu SC, Tseng CD, Yen MF, Chen TH. Progression of prehypertension, stage 1 and 2 hypertension (JNC 7): a population-based study in Keelung, Taiwan (Keelung Community-based Integrated Screening No. 9) J Hypertens. 2006;24:821–828. doi: 10.1097/01.hjh.0000222750.82820.19. [DOI] [PubMed] [Google Scholar]
- 22.Grossman A, Grossman C, Barenboim E, Azaria B, Goldstein L, Grossman E. Pre-hypertension as a predictor of hypertension in military aviators: a longitudinal study of 367 men. Aviat Space Environ Med. 2006;77:1162–1165. [PubMed] [Google Scholar]
- 23.Onat A, Yazici M, Can G, Kaya Z, Bulur S, Hergenc G. Predictive Value of Prehypertension for Metabolic Syndrome, Diabetes, and Coronary Heart Disease Among Turks. Am J Hypertens. 2008;21:890–895. doi: 10.1038/ajh.2008.212. [DOI] [PubMed] [Google Scholar]
- 24.De Marco M, de Simone G, Roman MJ, Chinali M, Lee ET, Russell M, et al. Cardiovascular and metabolic predictors of progression of prehypertension into hypertension: the Strong Heart Study. Hypertension. 2009;54:974–980. doi: 10.1161/HYPERTENSIONAHA.109.129031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ataman SL, Cooper R, Rotimi C, McGee D, Osotimehin B, Kadiri S, et al. Standardization of blood pressure measurement in an international comparative study. J Clin Epidemiol. 1996;49:869–877. doi: 10.1016/0895-4356(96)00111-4. [DOI] [PubMed] [Google Scholar]
- 26.Cooper R, Rotimi C, Ataman S, McGee D, Osotimehin B, Kadiri S, et al. The prevalence of hypertension in seven populations of west A frican origin. Am J Public Health. 1997;87:160–168. doi: 10.2105/ajph.87.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wilks R, Rotimi C, Bennett F, McFarlane-Anderson N, Kaufman JS, Anderson SG, et al. Diabetes in the Caribbean: results of a population survey from Spanish Town, Jamaica. Diabet Med. 1999;16:875–883. doi: 10.1046/j.1464-5491.1999.00151.x. [DOI] [PubMed] [Google Scholar]
- 28.Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 1997;20:1183–1197. doi: 10.2337/diacare.20.7.1183. [DOI] [PubMed] [Google Scholar]
- 29.Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1995;854:1–452. [PubMed] [Google Scholar]
- 30.Lean ME, Han TS, Morrison CE. Waist circumference as a measure for indicating need for weight management. BMJ. 1995;311:158–161. doi: 10.1136/bmj.311.6998.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stata Statistical Software: Release 10. College Station, Texas: Stata Corporation; 2007. [Google Scholar]
- 32.Dyer AR, Liu K, Walsh M, Kiefe C, Jacobs DR, Jr, Bild DE. Ten-year incidence of elevated blood pressure and its predictors: the CARDIA study. Coronary Artery Risk Development in (Young) Adults. J Hum Hypertens. 1999;13:13–21. doi: 10.1038/sj.jhh.1000740. [DOI] [PubMed] [Google Scholar]
- 33.Leitschuh M, Cupples LA, Kannel W, Gagnon D, Chobanian A. High-normal blood pressure progression to hypertension in the Framingham Heart Study. Hypertension. 1991;17:22–27. doi: 10.1161/01.hyp.17.1.22. [DOI] [PubMed] [Google Scholar]
- 34.Thomas J, Semenya KA, Neser WB, Thomas DJ, Green DR, Gillum RF. Risk factors and the incidence of hypertension in black physicians: the Meharry Cohort Study. Am Heart J. 1985;110:637–645. doi: 10.1016/0002-8703(85)90087-0. [DOI] [PubMed] [Google Scholar]
- 35.Bakx JC, van den Hoogen HJ, van den Bosch WJ, van Schayck CP, van Ree JW, Thien T, et al. Development of blood pressure and the incidence of hypertension in men and women over an 18-year period: results of the Nijmegen Cohort Study. J Clin Epidemiol. 1999;52:531–538. doi: 10.1016/s0895-4356(99)00023-2. [DOI] [PubMed] [Google Scholar]
- 36.Echeverria RF, Carbajal HA, Salazar MR, Riondet B, Rechifort V, Quaini M. Prevalence of high normal blood pressure and progression to hypertension in a population sample of La Plata. Medicina (B Aires) 1992;52:145–149. [PubMed] [Google Scholar]
- 37.Santaguida PL, Balion C, Hunt D, Morrison K, Gerstein H, Raina P, et al. Diagnosis, prognosis, and treatment of impaired glucose tolerance and impaired fasting glucose. Evid Rep Technol Assess (Summ) 2005;128:1–11. [PMC free article] [PubMed] [Google Scholar]
- 38.Pletcher MJ, Bibbins-Domingo K, Lewis CE, Wei GS, Sidney S, Carr JJ, et al. Prehypertension during Young Adulthood and Coronary Calcium Later in Life. Ann Intern Med. 2008;149:91–99. doi: 10.7326/0003-4819-149-2-200807150-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]