Summary
The microsatellite instable (MSI) subset of colorectal cancer (CRC) exhibits an active Th1/CTL immune microenvironment probably due to recognition of a high number of tumor neoantigens. However, the high expression of checkpoint molecules PD-1, PD-L1, CTLA-4, LAG-3, and IDO in MSI CRC distinguishes MSI from microsatellite stable (MSS) CRC and creates an immunosuppressive microenvironment that may help MSI tumors evade immune destruction by the infiltrating immune cells. Though CRC does not have a good response rate to PD-1 pathway immunotherapy, these results suggest that the MSI subset of CRC is a particularly good candidate for checkpoint immunotherapy.
Microsatellite instable (MSI) colorectal cancer (CRC) comprises approximately 15% of sporadic CRC and most familial CRC while microsatellite stable (MSS) CRC comprises the remainder (1). MSI is typically diagnosed by the variable length of DNA microsatellites (mononucleotide and dinucleotide repeats) (1). This variation is a consequence of epigenetic silencing or mutation of DNA mismatch repair genes (1, 2). Cells with abnormal mismatch repair function accumulate DNA replication errors, and novel microsatellite lengths are created. Impaired DNA mismatch repair facilitates insertions or deletions that can be frame-shift mutations as well as single base mismatches that can be point mutations in coding regions. MSI allows mutations to be accumulated at many times the normal rate and facilitates MSI neoplastic progression (1) (Fig. 1A).
Figure 1.
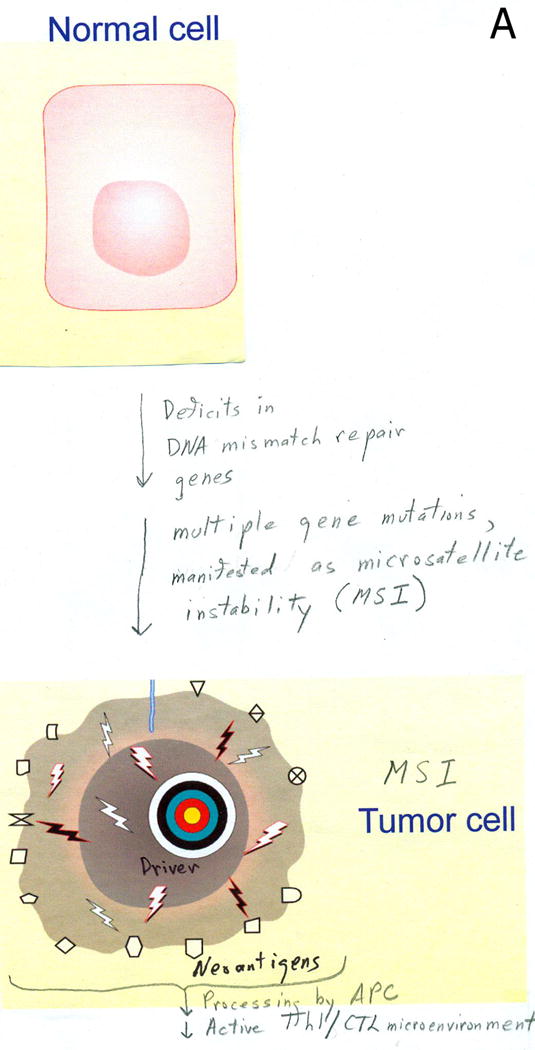

Immune microenvironment of MSI colorectal cancer. A. Deficits in DNA mismatch repair genes cause defective DNA mismatch repair, resulting in high levels of gene mutations manifested as MSI, which facilitate progression into an MSI CRC. Mutation-generated neoantigens are processed and presented on APCs and stimulate T cell activation, leading to an active Th1/CTL microenvironment; however, B. Upregulation of expression of checkpoint molecules such as PD-1, CTLA-4 and LAG-3 on T cells, PD-L1 on myeloid cells, and IDO expression in myeloid, APC, and tumor cells deliver inhibitory signals to suppress T cell activation, resulting in an immunosuppressive microenvironment. Green indicates activating and red inhibitory signals.
The high mutational load in MSI tumors also creates many tumor-specific neoantigens, typically 10–50 times that of MSS tumors (3). Some of these neoantigens will be processed, presented on MHC, and recognized as foreign by T cells (Fig. 1A). In particular, frame-shifted proteins should be a rich source of neoantigens. This high neoantigen burden might be one explanation for the high level of tumor-infiltrating lymphocytes (TILs) and lymphocytic reaction in MSI tumors observed in many previous studies (1). MSI tumors have a better prognosis than MSS (2) and the higher level of neoantigens in MSI may contribute to better survival via more robust immunoediting of MSI (4).
In this issue of Cancer Discovery, Llosa and colleagues (3) analyzed primary sporadic CRC from patients free of prior chemotherapy and found that a subset of primary sporadic CRC displayed high infiltration of activated CD8+ cytotoxic T lymphocytes (CTL) as well as activated Th1 cells with IFN-γ production and the Th1 transcription factor T-bet. Th17 or Th2 populations were not expanded. They determined that nearly all of the tumors of this subset were MSI CRC.
Despite a robust Th1/CTL microenvironment, some MSI tumors are not naturally eradicated though some incipient MSI tumors may be eradicated and never seen as CRC patients. Llosa and colleagues determined the expression of immune checkpoint molecules by immunohistochemistry, laser capture microdissection of TIL, stroma and invasive front combined with quantitative RT-PCR, as well as multiparameter flow cytometry of fresh tumors (3). They show that compared to MSS, MSI tumors highly up-regulate expression of multiple immune checkpoints, including programmed death-1 (PD-1) and cytotoxic T lymphocyte–associated antigen 4 (CTLA-4) in TIL, stroma and invasive front compartments, lymphocyte activation gene 3 (LAG-3) in TIL and invasive front compartments, and indolamine 2,3-dioxygenase (IDO) in the TIL compartment (3) (Fig. 1B).
PD-1 is upregulated after T cell activation, but declines when antigen is cleared. If antigen is not cleared, as in chronic infection or cancer, PD-1 expression remains elevated and T cells can enter a state of decreased effector function and proliferative capacity, termed “T cell exhaustion”. PD-1 has two ligands, PD-L1 (B7-H1; CD274) and PD-L2 (B7-DC; CD273). Engagement of PD-1 by PD-L1 or PD-L2 results in inhibition of T-cell immune functions, as shown by decreased production of cytokines such as IFN-γ and IL-2, decreased expression of cell survival proteins, altered motility and duration of interaction with dendritic cells (DC) and target cells, and altered metabolic activity. CTLA-4 is a potent inhibitory molecule that exerts its function via binding to CD80 and CD86, keeping them from delivering positive signals through CD28. LAG-3 is a CD4 homolog that binds MHC class II with a higher affinity than CD4. LAG-3 is important in controlling CD8+ T cell activity within target organs. LAG-3 is also required for maximal Treg function and can inhibit DC function by engaging MHC II on DC. IDO is an enzyme that catalyzes the degradation of the essential amino acid tryptophan to kynurenine. Production and secretion of IDO is induced by IFN-γ and IL-10. In the tumor microenvironment, IDO is produced by tumor cells, antigen presenting cells (APCs), tumor associated myeloid derived suppressor cells (MDSC), and tumor-associated macrophages in response to these inflammatory signals. High levels of IDO reduce tryptophan levels and create kynurenine, both of which contribute to suppression of T cell activity and are a potential mechanism for immune tolerance to tumor antigens (5).
In melanoma and many tumor types, the interface between the wave of infiltrating lymphocytes and the tumor is characterized by PD-L1 expression on the tumor cells (6). This is believed to be a consequence of T cell recognition of the tumor leading to IFN-γ expression by the T cells that in turn stimulates PD-L1 expression on the tumor cells. This INF-γ and PD-L1 expression constitutes a feedback loop, inhibiting the T cell anti-tumor response via engagement of PD-1 by PD-L1. In contrast, in MSI the interface between tumor and T cells was characterized by little expression of PD-L1 on the tumor cells despite INF-γ expression by the T cells. Instead, the T cell infiltrate was interlaced with an abundant PD-L1 positive myeloid cell population (3). Presumably these PD-L1+ myeloid cells serve to inhibit the T cell response. These PD-L1 positive myeloid cells were characterized as CD11b+HLA−DRloCD15−CD14+CD33+ which some investigators would call monocytic MDSC (7); however, there is not general agreement on human MDSC markers and Llosa et al. did not pursue this point. They also explored the lack of PD-L1 expression on the MSI tumor cells and found that in response to IFN-γ, both MSI and MSS CRC cell lines modestly upregulated PD-L1 and HLA-DR in comparison to the robust upregulation on melanoma and other cancer cell lines (3). They speculated that this might be a consequence of impaired Stat1 signaling but changes in IFN-receptor might also be involved (3).
One mystery is why the high load of neoantigens does not lead to immune eradication of MSI. MSI most often arise on the right side of the body in the proximal colon and recent work has shown that the gut microbiota contributes to the development of CRC. The abundance of Fusobacterium species, particularly F. nucleatum, in tumor tissue has been shown to be associated with MSI CRC (8). Fusobacterium proteins can selectively recruit tumor-infiltrating myeloid cells and inhibit T-cell proliferation (9). Fusobacterium may facilitate up-regulation of checkpoint ligands such as PD-L1 in these recruited myeloid cells. We would speculate that Fusobacterium might be critically involved in suppressing the immune response at the time when MSI begins to generate a high burden of neoantigens that should facilitate immune eradication. Once the T cell population fails to eliminate the tumor, it lapses into a chronic response with high expression of exhaustion markers and susceptibility to immunoinhibitory signals.
Anti-PD-1 and anti-PD-L1 antibodies have demonstrated significantly durable efficacy in patients with melanoma, renal cancer and non-small cell lung cancer (3). However, CRC appeared to be a poor responder to antibody blockade of PD-1 or PD-L1 in clinical trials (3). Since most MSI CRC typically present with lower stage disease than MSS CRC, the MSI subtype represents only 5–6% of the stage IV CRC population (10) and likely there were few MSI patients in PD-1 and PD-L1 clinical trials, with 18 and 19 advanced CRC patients, respectively.
All of the five checkpoint molecules upregulated in MSI tumors are currently being targeted clinically with inhibitors (3). The FDA approved a CTLA4 mAb (ipilumumab) in 2010 and a PD-1 mAb (pembrolizumab) in 2014 for melanoma treatment and multiple other pathway agents are in clinical trials and approaching approval. Multiple LAG-3 mAbs and small molecule IDO pathway inhibitors are in development or clinical trials. Based on Llosa et al.’s findings of high expression of PD-1 and PD-L1 in MSI CRC, two clinical trials have been initiated to test PD-1 blockade in MSI CRC patients (3). Combinations with IDO, LAG-3, CTLA-4 and other checkpoints will likely follow.
This still leaves a great need for effective immunotherapies in the remaining 95% of stage IV CRC. As the checkpoint blockade molecules were discovered by their effects on immune tolerance, this suggests we need to deepen our understanding of the specialized mechanisms of gut immune tolerance in order to identify additional targets for CRC immunotherapy.
Acknowledgments
Grant Support:
This work was supported by NIH grants P01AI056299, U54CA163125, P50CA101942 and HHSN272201100018C (GF).
Footnotes
Disclosure of Potential Conflicts of Interest
G.J. Freeman has patents and receives patent royalties on the PD-1 pathway from Bristol-Myers-Squibb, Merck, Roche, EMD-Serono, Boehringer-Ingelheim, Amplimmune, and Novartis. Y. Xiao is an inventor on a patent application for PD-L2 interaction with repulsive guidance molecule b which has been licensed to Novartis.
References
- 1.Smyrk TC, Watson P, Kaul K, Lynch HT. Tumor-infiltrating lymphocytes are a marker for microsatellite instability in colorectal carcinoma. Cancer. 2001;91:2417–22. [PubMed] [Google Scholar]
- 2.Ogino S, Nosho K, Kirkner GJ, Kawasaki T, Meyerhardt JA, Loda M, et al. CpG island methylator phenotype, microsatellite instability, BRAF mutation and clinical outcome in colon cancer. Gut. 2009;58:90–6. doi: 10.1136/gut.2008.155473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Llosa NJ, Cruise M, Tam A, Wick EC, Hechenbleikner EM, Taube JM, et al. The vigorous immune microenvironment of microsatellite instable colon cancer is balanced by multiple counter-inhibitory checkpoints. Cancer Discov. 2014 doi: 10.1158/2159-8290.CD-14-0863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gubin MM, Zhang X, Schuster H, Caron E, Ward JP, Noguchi T, et al. Checkpoint blockade cancer immunotherapy targets tumour-specific mutant antigens. Nature. 2014 doi: 10.1038/nature13988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prendergast GC, Smith C, Thomas S, Mandik-Nayak L, Laury-Kleintop L, Metz R, et al. Indoleamine 2,3-dioxygenase pathways of pathogenic inflammation and immune escape in cancer. Cancer Immunol Immunother. 2014;63:721–35. doi: 10.1007/s00262-014-1549-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taube JM, Anders RA, Young GD, Xu H, Sharma R, McMiller TL, et al. Colocalization of inflammatory response with B7-h1 expression in human melanocytic lesions supports an adaptive resistance mechanism of immune escape. Sci Transl Med. 2012;4:127ra37. doi: 10.1126/scitranslmed.3003689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rudolph BM, Loquai C, Gerwe A, Bacher N, Steinbrink K, Grabbe S, et al. Increased frequencies of CD11b(+) CD33(+) CD14(+) HLA-DR(low) myeloid-derived suppressor cells are an early event in melanoma patients. Exp Dermatol. 2014;23:202–4. doi: 10.1111/exd.12336. [DOI] [PubMed] [Google Scholar]
- 8.Tahara T, Yamamoto E, Suzuki H, Maruyama R, Chung W, Garriga J, et al. Fusobacterium in colonic flora and molecular features of colorectal carcinoma. Cancer Res. 2014;74:1311–8. doi: 10.1158/0008-5472.CAN-13-1865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kostic AD, Chun E, Robertson L, Glickman JN, Gallini CA, Michaud M, et al. Fusobacterium nucleatum potentiates intestinal tumorigenesis and modulates the tumor-immune microenvironment. Cell Host Microbe. 2013;14:207–15. doi: 10.1016/j.chom.2013.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lochhead P, Kuchiba A, Imamura Y, Liao X, Yamauchi M, Nishihara R, et al. Microsatellite instability and BRAF mutation testing in colorectal cancer prognostication. J Natl Cancer Inst. 2013;105:1151–6. doi: 10.1093/jnci/djt173. [DOI] [PMC free article] [PubMed] [Google Scholar]


