Abstract
Resilience and the ability to mitigate the consequences of a nuclear incident are enhanced by (1) effective planning, preparation and training; (2) ongoing interaction, formal exercises, and evaluation among the sectors involved; (3) effective and timely response and communication; and (4) continuous improvements based on new science, technology, experience and ideas. Public health and medical planning require a complex, multi-faceted systematic approach involving federal, state, local, tribal and territorial governments, private sector organizations, academia, industry, international partners, and individual experts and volunteers. The approach developed by the U.S. Department of Health and Human Services Nuclear Incident Medical Enterprise (NIME) is the result of efforts from government and nongovernment experts. It is a “bottom-up” systematic approach built on the available and emerging science that considers physical infrastructure damage, the spectrum of injuries, a scarce resources setting, the need for decision making in the face of a rapidly evolving situation with limited information early on, timely communication and the need for tools and just-in-time information for responders who will likely be unfamiliar with radiation medicine and uncertain and overwhelmed in the face of the large number of casualties and the presence of radioactivity. The components of NIME can be used to support planning for, response to, and recovery from the effects of a nuclear incident. Recognizing that it is a continuous work-in-progress, the current status of the public health and medical preparedness and response for a nuclear incident is provided.
Keywords: National Council on Radiation Protection and Measurements, nuclear detonation, radiation emergency, improvised nuclear device, emergency preparedness and response, resilience
Introduction
Following the 11 September 2001 terrorist attacks, the United States began detailed preparation to address 15 National Planning Scenarios†††† (DHS 2007, 2011). Scenario #1 is a 10 kT improvised nuclear device, also called a nuclear detonation. Scenario #11, a radiological dispersal device has elements in common with a nuclear detonation but is not the subject of this report. The radiation research and sciences communities began working together to consider the science, tools and treatments available for acute radiation injury (Coleman et al. 2003), and efforts were initiated at the federal level to improve planning and preparedness for the health and medical response to such incidents which in the National Response Framework is a responsibility of the U.S. Department of Health and Human Services (DHHS) per Emergency Support Function #8 and the Nuclear/Radiological Incident Annex (FEMA 2008, 2013a).
A 2009 publication presented the systems approach being developed by DHHS and its interagency partners, which emphasized the importance of basing the response on the available and emerging science (Coleman et al. 2009; Dainiak et al. 2011a, 2011b). A number of guidance and planning documents incorporating input from subject matter experts (SMEs) inside and outside government have been published, including:
Planning Guidance for Response to a Nuclear Detonation (National Planning Guidance) (HSC 2010) coordinated by the Office of Science and Technology Policy that includes information on potential physical infrastructure damage, guidance for shelter and evacuation, and communication in addition to health and medical issues; and
Scarce Resources for a Nuclear Detonation Project coordinated by DHHS (Coleman et al. 2011a, Knebel et al. 2011), which addressed managing radiation casualties under conditions of resource scarcity (Coleman et al. 2011b).
Additionally, the U.S. government is supporting ongoing programs to develop medical countermeasures (MCM), diagnostics, and distribution systems. Formal collaborations with international partners have been established, and valuable experience has been gained from exercises and the response to the nuclear power plant disaster in Japan (Coleman et al. 2013, NA/IOM 2013). Current capabilities and experience have been distilled into the Nuclear Incident Medical Enterprise (NIME) which is described in this paper and addresses public health and medical planning and response.
When developing information, resources and tools for decision makers as well as public health and medical responders, planners make a number of core assumptions:
information needs to be in an understandable and useable format, with up-to-date content available just-in-time under a very compressed timeline (minutes) by a variety of audiences;
detonation of an nuclear device is thought to be such an overwhelming scenario that many localities do not expend scarce preparedness resources planning for it (GAO 2013); when, in fact,
although there would be catastrophic destruction near the epicenter, much infrastructure in the surrounding areas will remain intact and could provide meaningful support to affected populations; and, therefore,
while solid science, theory, law and policy underpinnings are critical, what is needed for responders and planners is the answer to the question “What do I DO??!!.”
While a consistent effort to share available information and tools has been made, recent workshops focusing on regional preparedness have shown that additional efforts are needed to bring the answers to this question to the public's attention (NA/IOM 2014).
As the individual tools and concepts in NIME were developed, they were published in the peer reviewed scientific literature so that the ideas and products benefit from review, broad discussion, and public dissemination. Most of these tools and capabilities can also be used for mass casualty radiation incidents other than a nuclear detonation.
Nuclear Incident Medical Enterprise
Fig. 1 illustrates the inter-related components of NIME. While there are various ways of presenting the content, the authors felt it is important to be able to visualize the components in a single chart in which their relationships could be understood. The enterprise is based on knowledge from science and medicine with the awareness that partnerships and senior leadership coordination will be essential for preparing for and mounting the response. Understanding the “nuclear scenario and its impact” is the basis for planning and response. Public health and medical concepts are the basis for developing resources that facilitate medical management and situational awareness. Built on these resources are response tools and capabilities which are assessed and modified in exercises and used during incidents including minor radiological incidents and the Fukushima Nuclear Power Plant accident. While there is overlap as to which NIME category in planning and response, resources and tools are developed, in the NIME chart they are placed into the five columns that occur in sequence following an incident: decision making and communication, organizing response, triage, medical management, and medical care. While “medical” is used in the title for simplicity, the enterprise addresses public health and medical needs. Some of the components have been specifically designed for or adapted to a nuclear incident, while most reflect general all-hazards capabilities available within the Office of the Assistant Secretary for Preparedness and Response (ASPR) with DHHS and the federal government.
Fig. 1.
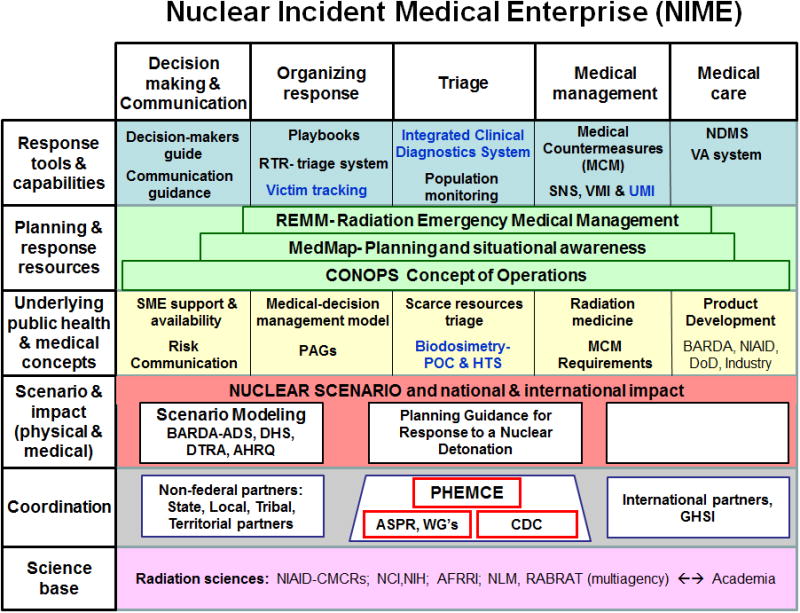
Nuclear Incident Medical Enterprise (NIME). NIME is a composite of the approach of DHHS and interagency partners, working with state, local, regional, territorial and tribal partners, and academia toward the public health and medical preparedness, planning and response to a nuclear detonation. It is a “bottom up” compilation with current and evolving science and collaboration as the underpinning of the enterprise. On this base are the scenario and models, concepts, resources, and lastly specific tools and capabilities. Working from left to right on the top three rows are how these will be used during the phases of preparedness and response. There are tools and resources that transcend all phases.
Resilience and the ability to mitigate the consequences are key goals. The concepts, resources, tools and capabilities for NIME can be applied to the all-hazards approach used for emergency planning and response. Responses begin at the local level with federal resources provided when requested. Description and essential information is presented in the text with the goal of having a single source that includes the information which is contained in a number of resources. Text in blue represents projects for which substantial development is necessary and in progress.
NIME recognizes that public health and medical responses begin at the local level and that federal resources are mobilized only when requested. It assumes that an incident of this magnitude will rapidly overwhelm the local, state and regional resources and that federal assistance will be requested. The items in Fig. 1 are next discussed by row from the bottom up.
Science Base
Radiation sciences
The information and resources developed for both planning and response are based on the best available science including knowledge of research and development in progress some of which may not yet be publicly available. There are experts in multiple federal agencies who share knowledge through research projects, seminars, and working groups. This includes a periodic informal exchange of information under Radiation Bioterrorism Research and Training Group (NCI 2013a). Collaboration and discussion among government, academic and industry scientists is conducted at meetings of scientific and professional societies, such as the Radiation Research Society (RRS 2014).
There is a present and growing national shortage of people with radiation biology expertise. For nuclear incident medical preparedness, this shortage was partially addressed through training and education provided in the National Institute of Allergy and Infectious Diseases (NIAID), Centers for Medical Countermeasures Against Radiation. However, these efforts are no longer available due to budget limitations. A more complete analysis of the national shortage of radiation experts is included in a report by the National Council on Radiation Protection and Measurements (NCRP 2013) entitled National Crisis: Where are the Radiation Professionals (WARP)?.
Coordination
ASPR, ASPR working groups, PHEMCE, CDC
The Public Health Emergency Medical Countermeasures Enterprise (PHEMCE) (ASPR 2013a) coordinates federal efforts to enhance the response to chemical, biological, radiological, nuclear, explosive threats from an MCM perspective. PHEMCE is led by ASPR and includes three primary DHHS internal agency partners: Centers for Disease Control and Prevention (CDC), Food and Drug Administration, and the National Institutes of Health, as well as several interagency partners: the U.S. Departments of Defense, Veterans Affairs, Homeland Security (DHS), and Agriculture. Working groups operating under the PHEMCE perform the wide range of functions, with integration of efforts across disciplines and departmental boundaries a major group being the Radiological/Nuclear Integrated Project Team. A key emphasis for all of U.S. government planning and response is working closely with partners, especially nonfederal U.S. partners, but also international partners. Given the magnitude of a nuclear detonation, this cooperation is particularly important.
Nonfederal partners: state/local/tribal/territorial
The ASPR Office of Emergency Management (OEM) works at the state and regional level through exercises and educational programs. There is substantial ongoing scientific participation by nongovernment SMEs, as illustrated in the authorship of the Scarce Resources for a Nuclear Detonation Project (Coleman et al. 2011a) and the medical planning guide (Coleman et al. 2012a).
International partnerships
Federal agencies, particularly ASPR collaborate with international partners for health and medical issues through multilateral forums such as the Global Health Security Initiative (ASPR 2013b) and with partners at the International Atomic Energy Agency and the World Health Organization including its BioDoseNet (2014) and the Radiation Emergency Medical Preparedness and Assistance Network (WHO 2014) components. Additionally, the NIAID Centers for Medical Countermeasures Against Radiation have established collaborations with international organizations to advance basic research and MCM development.
Scenario and Impact
Scenario modeling
A great deal of progress has been made in refining initial National Planning Scenario (DHS 2007) models. A wide range of robust, detailed, computer models have been built to describe many types and locations of nuclear detonations, including air and ground detonations, various sizes of detonations, and both meteorological and topographical factors, that could affect ground contamination, fires, the blast and the trajectory, deposition, and decay characteristics of the fallout cloud. The consequences of a detonation have also been modeled from human fatalities and injuries to impacts on infrastructure and the amount of debris generated. These models have been critical for characterizing a range of incident parameters for which plans have been developed and for which only limited data were available before the modeling.
Interagency partners-planning for the scope of nuclear detonation
The National Planning Guidance (HSC 2010) provides a structure from which the public health and medical response will occur. It describes four physical damage zones (severe, moderate, and light damage and dangerous fallout) and illustrates that there will be a wider area of radioactive fallout where people and responders can remain and work for varying periods of time.
The Interagency Modeling and Atmospheric Assessment Center (IMAAC) (DHS 2013) led by DHS produces, coordinates and disseminates dispersion modeling and hazard prediction products. This Center is a partnership among eight federal agencies to specifically address the integration necessary for atmospheric modeling. IMAAC information can be incorporated into MedMap (ASPR 2013c) for planning and situational awareness during a response as described below.
For a sense of scope of a nuclear detonation incident, general estimates of the numbers and types of casualties following an improvised nuclear device detonation are in Table 1 (Knebel et al. 2011, Coleman et al. 2012a).
Table 1.
Estimated casualties from nuclear detonation modeling for trauma only, radiation only injury, and combined injury (radiation plus trauma).
| Injury Type | Category | Compositea | ||
|---|---|---|---|---|
|
| ||||
| 50% | 85% | 95% | ||
| Trauma (injury severity score) | Mild (1–9) | 20,000 | 53,000 | 80,000 |
| Moderate (10–14) | 34,000 | 118,000 | 121,000 | |
| Severe (>15) | 14,000 | 63,000 | 143,000 | |
| Radiation only injury (radiation dose) | Mild 0.75–1.49 Gy | 4,000 | 23,000 | 72,000 |
| Moderate 1.5–5.29 Gy | 6,000 | 25,000 | 41,000 | |
| Severe 5.3–8.3 Gy | 3,000 | 6,000 | 12,000 | |
| Expectant >8.3 Gy | 5,000 | 16,000 | 47,000 | |
| Combined injury (radiation dose > 1.5 Gy) | Trauma and/or mild-severe burn | 2,000 | 20,000 | 45,000 |
The values in this table are estimates used for planning purposes and are derived from 185 different scenarios with various nuclear detonation yields (0.1–10 kT) in various cities under various conditions. Because of the range of possibilities, casualty numbers can vary by factors of 5 to ≥10 among cities and among detonation locations within cities. The percentiles used represent a mid-range (50th percentile), a moderately-high (85th percentile), and an estimate for a high-consequence scenario (95th percentile) (adapted from Knebel et al. 2011).
Underlying Concepts
SME support and availability
Should a nuclear incident occur, it will be essential for decision makers to have readily available expertise in the radiation sciences and in the management of radiological and nuclear emergencies. Public health and medical expertise is available from the Advisory Team for Environment, Food and Health, known as the A-Team (CDC 2014a) and from ASPR subject matter experts (SME). There is a proposed formalization of SMEs into a subject matter advisory resource team that would include government and nongovernment experts. Research scientists including clinicians and epidemiologists are available from federal agencies as noted above in Radiation Bioterrorism Research and Training. The Radiation Injury Treatment Network (RITN) is a nongovernment group that has world renowned oncology and hematology experts and capabilities to assist in planning, treatment-protocol development, and treatment for patients with acute radiation syndrome (Ross et al. 2011, NMDP 2014).
Risk communication
Risk communication experts are available during exercises and incidents from federal agencies. The importance of timely and effective communication was seen in the response to the Fukushima Nuclear Power Plant disaster. A set of prescripted messages for preparedness and response to a nuclear incident is available (FEMA 2013b) as noted in Response Tools and Capabilities of Fig. 1.
Medical-decision management model
Based on experience managing the Fukushima Nuclear Power Plant disaster in Japan, a medical decision-management model was proposed by a multi-agency group of experts who worked with the U.S. Embassy team in Tokyo during the crisis (Coleman et al. 2013). The underlying principles are that decisions must be made in real-time based on emerging information, as is done in rapidly evolving medical care such as emergency medicine and oncology, and that it is best done with SMEs on site with the senior decision makers. Reach-back expertise and consultation are necessary but should not delay critical decision making and communication.
PAGs
As defined on the EPA website:
“A PAG is defined ….. as the projected dose to an individual from a release of radioactive material at which a specific protective action to reduce or avoid that dose is recommended. PAGs are guides to help officials' select protective actions under emergency conditions during which exposures would occur for relatively short time periods. They are not meant to be applied as strict numeric criteria, but rather as guidelines to be considered in the context of incident-specific factors. PAGs do not establish an acceptable level of risk for normal, nonemergency conditions, nor do they represent the boundary between safe and unsafe conditions. The PAGs are not legally binding regulations or standards and do not supersede any environmental laws” (EPA 2013).
For the general public, the Protective Action Guide (PAG) dose, even if it is reached, is very low. It is below 0.05 Gy for radiation workers and lower for members of the public. Anyone receiving a dose below the PAG limit would be far below risk of acute radiation syndrome (EPA 2013) and would not need any medical intervention for radiation exposure per se. Response worker dose guides are higher (0.05–0.25 Gy or possibly higher) and require prior understanding and/or informed consent. In comparison to the PAG doses, symptoms from acute exposure begin to occur at ~0.75–1 Gy and screening for possible acute radiation syndrome begins at ~2 Gy.
In an evolving nuclear or major radiological incident response, the plume models and measured radiation data would be used to guide decision makers and responders as to where to deploy, who to evacuate and when, who should shelter in place, identify those individuals who are not affected, and for those who have evacuated when they might return. It is noteworthy that radioactive fallout decays rapidly following a nuclear detonation so that the boundary lines of where responders will be excluded due to the higher radiation exposures will shrink rapidly over the first few hours to days.
Scarce resources triage
Perhaps the most significant challenge for emergency responders and triage officers will be the possible need to alter triage assignment for individual victims from the usual “sickest first” model. The Scarce Resources for a Nuclear Detonation Project addressed the issue of scarce resource allocation and the possible need to alter triage (Casagrande et al. 2011, Coleman et al. 2011a, 2011b, Knebel et al. 2011). Performing medical triage in the field will pose a serious challenge to most emergency responders and healthcare facilities due to a lack of familiarity with the medical issues related to radiation exposure and/or contamination. To address this issue, the Radiation Emergency Medical Management (REMM) website (NLM 2014a) was developed for those unfamiliar with radiation exposure and/or contamination. REMM will be useful for symptoms such as time to vomiting but, the algorithms show the importance of laboratory support for biodosimetry, more accurate triage and medical management (NLM 2014b). A model of resource and time-based triage was developed by Casagrande, Coleman and colleagues (Casagrande et al. 2011, Coleman et al. 2011b) and an algorithm-based approach for triage (Coleman et al. 2011b) is available as triage cards and a web-based tool on the REMM website.
Biodosimetry
The ability to estimate the dose received by individuals will determine resource allocation and will aid in patient triage, emphasizing the importance of taking care of potentially fatal injuries first and considering the effect of radiation second. A diagnostic test that estimates radiation dose is called “biodosimetry.” A number of assays are used with the blood count (especially lymphocyte depletion kinetics) and cytogenetic changes (dicentric chromosome assay) being the most widely used techniques. As recently reviewed by Sullivan et al. (2013) newer approaches are being studied including point-of-care diagnostics that will sort people into broad dose groups (e.g., <2, 2–4, 4–6, and >6 Gy) for initial triage and secondary diagnostics high throughput screening that can provide a more accurate dose for definitive medical management.
Radiation medicine
Depending on the dose and presence of combined injury people with radiation exposure >2 Gy will require either immediate treatment or referral to a center with expertise in radiation injury. People with low doses (e.g., <2 Gy) and without physical injury will not require immediate care and might be among those monitored in long-term epidemiological studies, such as those conducted by the National Cancer Institute Division of Cancer Epidemiology and Genetics Radiation Epidemiology Branch (NCI 2013b). Determining who requires acute care in the immediate aftermath of the incident will be critical if medical resources are in short supply, as they are likely to be.
MCM requirements
The determination of what resources will be required for an incident is essential to effective planning. Resource requirements include the MCMs, clinical diagnostic tools, and supporting materiel needed for a range of emergencies, and the infrastructure for storing, accessing and dispensing MCMs. Determining what resources are required must take into account the ability to deliver and utilize them during the crisis. Organized by the ASPR Office of Policy and Planning, Division of Medical Countermeasure Strategy and Requirements (ASPR 2013d), requirements documents and processes are built on detailed modeling of:
the incident;
medical conditions anticipated;
patient illness and injury distribution;
treatments potentially available and their operating characteristics (e.g., intravenous, oral, temperature for storage, single packaging versus multi-dose, shelf-life, etc.);
whether the MCM is used in routine practice (called “dual-utility”);
quantity in routine use;
ease of administration (including self-administration); and
other factors.
Product development
While some aspects of MCM and diagnostic development are classified or confidential (due to business decisions or pending decisions on acquisitions), much is published in the peer review literature. The Biomedical Advanced Research and Development Authority (BARDA), which is a part of ASPR, partners with industry to facilitate advanced product development for MCMs that are guided by federal working groups. The products and concept of operations (CONOPS) for their use are continually evaluated to optimize what is available and also to develop products that could perform under the most likely scenarios.
The NIAID Radiation and Nuclear Countermeasures Program (NIAID 2013) has a research and development program addressing radiation-induced normal tissue injury and biodosimetry, with a focus on post-exposure treatment, mitigation, and public health emergency needs. As part of this program, the NIAID Centers for Medical Countermeasures against Radiation and the Radiation and Nuclear MCM Product Development Support Services engage academic and industrial/biotechnology companies in early stage research and product development that can serve as a source of potential new products for BARDA's advanced development. Earlier stage research and discovery is supported by the National Institutes of Health basic and translational research grants. The Armed Forces Radiobiology Research Institute (AFRRI) has long-standing research and development programs for radiation MCM and biodosimetry (AFRRI 2014). While NIAID and BARDA focus on post-exposure mitigation, the U.S. Department of Defense supports pre-exposure, prophylactic MCM research at AFRRI and the Defense Advanced Research Projects Agency.
Plannng and Response Resources
REMM
Development of the Radiation Emergency Medical Management (REMM) website was initiated early on, as the first versions of playbooks were written (NLM 2014a). REMM is a collaboration of ASPR, the National Cancer Institute, the National Library of Medicine (NLM), and SMEs from within and outside the federal government. REMM reflects evidence-based, peer-reviewed literature, and is updated frequently as medical science and official planning documents evolve. REMM uses an algorithm-based approach similar to that used in advanced cardiac life support. It provides guidance for both responders who manage an incident as well as individual health care providers who manage patients. REMM can be used as a just-in-time resource or pre-incident for training and education. “Mobile REMM” is a smart-phone app and can be downloaded for multiple platforms (ASPR 2014a). Both REMM and Mobile REMM have an interactive tool which uses the absolute lymphocyte count from one or more complete blood counts to estimate whole-body dose (NLM 2014c). The algorithm was developed by AFRRI.
MedMap
A nuclear scenario will evolve rapidly over time and location. In order to maintain situational awareness and provide a common operating picture for responders, MedMap was developed by ASPR to specifically respond to a nuclear detonation. However, MedMap is now used for all hazards and continues to grow in capacity and capability. MedMap is a secure, Geographic Information Systems-based application that combines data from multiple federal and public agencies and sources into a single mapping environment, with individual layers reflecting details about the incident as well as many kinds of response resources and analytical tools. With consultation from chemical, biological, radiological, nuclear, or explosive SMEs (ASPR 2013e, CDC 2013a) data can be integrated and interpreted as an incident unfolds. MedMap can be updated iteratively in real-time as new data arrive to provide incident managers with big picture situational awareness. It displays areas with damage and fallout, and shows the locations of resources for planning and responses including medical care sites and mobilization points. Access to MedMap can be shared by request to ASPR when needed.
CONOPS
DHHS and other federal agencies have developed their own specific CONOPS for a nuclear detonation response that describes in detail the agency's planned overall response. The DHHS CONOPS, prepared by OEM while working with intra- and interagency experts, focuses on the DHHS role and how other agencies and state/local responders will interact with the federal response. What is key in the NIME approach is that MCM use and delivery must be realistically executable within the CONOPS (Sullivan et al. 2013). CONOPS are modified to accommodate the characteristics of the necessary supplies and their distribution. Thus, CONOPS are constantly evolving and are operationalized within playbooks and guidance documents.
Response Tools and Resources
Decision-makers' guide
After seeing first-hand the scope of and immediate need for information in the real-time management of the Fukushima Nuclear Power Plant disaster, a decision-makers' guide was developed to enable better informed decisions by primary decision makers (who may be an elected official without a science or medical background). The decision-makers' guide contains critical information on aspects of a radiation or nuclear incident that can be used until SME support is available (Coleman et al. 2012a, Koerner et al. 2014). A web-based electronic version is in preparation.
Communication guidance
Effective and timely messaging is critical. Resources have been developed to aid responders in providing information and life-saving instructions to the public (FEMA 2013b, CDC 2014b, Koerner et al. 2014). The resources have been reviewed and tested by state and local responders and communications experts.
Playbooks
Considerable energy is devoted to the development of plans and playbooks that become the basis for training and exercises so that responders can prepare for and respond quickly to events they have never experienced before, except to some extent in exercises. These may be incident-specific documents or an annex to an all-hazards plan. DHHS playbooks and plans are produced by planning and operations SMEs within OEM. Other federal agencies have internal plans that detail their responsibilities and how they will interact with others (FEMA 2008).
There are a number of plans, playbook, and other resources available on the ASPR website [http://www.phe.gov (ASPR 2014b)]. While the federal response has much in common with state/local/tribal/territorial responses, ASPR has worked with state/local/tribal/territorial experts to develop a playbook template for a nuclear detonation and which uses both a time- and sector-oriented response (Murrain-Hill et al. 2011).
The Radiation Triage, Treatment, and Transport System
As described in Planning Guidance for Response to a Nuclear Detonation (HSC 2010), there will be locations after a nuclear detonation where there will be some people with combined injury (e.g., radiation, mechanical trauma, and/or burn) as well as many people with either isolated physical injury or isolated radiation exposure. Triage will be based first on standard triage systems in use by the local/regional responders. Radiation exposure will be assessed based on the person's location at the time of the detonation and during the period of fallout deposition and by symptoms and laboratory measurement. In that the responders need a system to account for the presence of radiation, the Radiation Triage, Treatment, and Transport System was developed to help manage radiation injury and has been used in a number of exercises and regional planning efforts (Hrdina et al. 2009).
Victim tracking
The ability to reunite displaced people after an incident of this magnitude will present a complex challenge. A common process for tracking patients, fatalities and responders remains a significant gap. State and local agencies should establish a registry as early as possible that can be used to contact people who require short-term medical follow-up and/or long-term health monitoring; assistance is available from CDC and the Agency for Toxic Substances and Disease Registry (CDC 2014c). The Agency's Rapid Response Registry is available to assist state and local personnel with epidemiological investigations. Other examples of registry and epidemiological tracking forms are available from the National Alliance for Radiation Readiness (NY DOH 2014) or as part of the Virtual Community Reception Center training program (CDC 2014d, NLM 2014c).
Integrated clinical diagnostics system
For a nuclear detonation, various techniques will be used to estimate an individual's whole-body radiation dose from external exposure. There may be physical radiation dose levels from monitors in fixed locations (e.g., police and fire stations) and from responders in the field. Computer models (DHS 2013) will analyze doses reported from various venues, and create geographic dose maps that evolve over time. With these maps, responders can “bin” members of the public into groups based on their physical location(s) and estimate likely dose from radiation exposure to prompt radiation and subsequent fallout.
Physical dosimetry (field measurements) and models will be helpful but for medical management biodosimetry will be necessary to estimate doses received by an individual as noted above. SMEs have proposed an architecture that will allow for a massive, immediate national biodosimetry surge (HSC 2010, Grace et al. 2011, Hatchett 2011, NA/IOM 2013) and the concepts for an Integrated Clinical Diagnostics System (ICDS) are under development (Coleman et al. 2009, Sullivan et al. 2013, Blumenthal et al. 2014). The ICDS concept recognizes that the role of clinical diagnostics will change based on the location of testing and over time after the incident. Physical and clinical biodosimetry would be used initially for triage, then to inform medical management, and still later for long-term epidemiology and risk assessment. The establishment of ICDS is a work in progress. This system has a unique focus on radiation and its special requirements and is not a component of the CDC Laboratory Response Network (CDC 2013b), although there are potential processes in common.
Population monitoring
CDC prepared Population Monitoring in Radiation Emergencies: A Guide for State and Local Public Health Planners (CDC 2014e) which has been used in the design and conduct of drills and exercises at local, state and federal levels (NLM 2014c). States are beginning to incorporate population monitoring into their radiation emergency response plans. The operational concept of the community reception center is also being incorporated in radiation emergency response plans across the country. To support these efforts, CDC has developed a number of training and planning tools and resources specifically related to population monitoring and community reception center operations.
MCM
The effective and efficient use of medical countermeasures (MCM) requires a CONOPS for managing and co-locating the staff and resources with the victims who need assessment and treatment. As a nuclear detonation response will require a national and, indeed, an international response expanding the current planning and utilization of MedMap for a “national CONOPS” is a work in progress by ASPR. MCM's included medicines and supplies which may be common across hazards. Examples for a nuclear detonation include bone marrow cytokines, antibiotics, antiemetics, intravenous fluids, and burn kits. There is a DHHS Blood and Tissue Working Group looking at these products. The special needs for at-risk populations and pediatric patients, such as liquid formulations and alternate dosing schedules, are considered during MCM development and dispensing. Product development of novel radiation countermeasures is supported by NIAID and BARDA.
Managed inventory approaches for MCMs
The CDC Division of Strategic National Stockpile ensures the availability of critical MCMs that can be rapidly integrated into a public health response when needed. The Division of Strategic National Stockpile uses multiple managed-inventory systems to ensure inventory of available MCM. A new User-Managed Inventory approach (Coleman et al. 2012b), currently under consideration, could enhance the capability of local responders to have MCMs in the first 24 h before major outside resources can reach the incident. The User-Managed Inventory approach would stockpile and store inventory in local care facilities, and is under discussion or development by a few cities and RITN. Table 2 compares various kinds of actual and potential storage and stockpiling methods.
Table 2.
Medical countermeasure storage and stockpiling methods.
| Current SNS Strategies | Emerging Strategy | ||||
|---|---|---|---|---|---|
|
| |||||
| Vendor-Managed Inventory | Stockpile-Managed Inventory | Forward Deployed Stockpile-Managed Inventory | Contingency Contract | User-Managed Inventory | |
| Source of additional capacity | Manufacturer or vendor maintains guaranteed level of needed supplies rotating regularly to fill commercial orders; supplies are kept in a warehouse the vendor controls. | Inventory is purchased and stored in a commercial warehouse location such as a warehouse and is replaced as it reaches expiry or is used. | A stockpile of inventory is kept onsite, or close by so that it can be used in a very short time period after an incident. | Pre-existing contracts allow access to manufacturer or prime vendor's existing inventory on an “as available” basis. | Dual-utilitya product normally stored onsite. After the one time creation of a bolus of supply, routine use could allow supply to be rotated and replenished at reduced per dose cost. |
| Responsible party | Manufacturer or vendor under SNS oversight | Third party logistics provider under SNS oversight | Local hospital or emergency medical services under remote SNS oversight | Manufacturer or prime vendor | User of product; hospitals, specialty clinics, care facilities, etc. |
| An example | Anti-neutropenic cytokines | Antibiotics, vaccines, IV fluids | Nerve agent antidotes | Medical/surgical supplies for blast and trauma | Anti-emetics |
| Expected timeframe for delivery | Dependent on contractual terms. <24 h | Varies by item. <12–24 h | <1 h. Product must be at the site of need or very close. | 24–48 h | Immediate use in facility where stored. |
This is in contrast to dual-use research in which knowledge, products or technologies could potentially be misapplied in a harmful manner.
Medical care
The number of individuals seeking medical attention will likely rapidly and significantly overwhelm the local/regional capacity which will have a substantial ripple effect throughout the region and country. During an emergency, most deployable federal medical resources other than the SNS are coordinated through the OEM, which oversees assets such as the National Disaster Medical System. In a nuclear disaster, these assets will supplement an integrated national medical response capability by assisting state and local authorities (ASPR 2013f). The U.S. Public Health Service and local Medical Reserve Corps teams located across the United States will also support this “whole medical community” response, and these assets are connected at the federal level both to ASPR and the DHHS Office of the Surgeon General and the Assistant Secretary of Health. Very few of these teams, however, are equipped to operate in a contaminated environment or have the ability to treat contaminated patients. Additionally, current local and state efforts supported by the Hospital Preparedness Program (ASPR 2014c) grants for developing hospital surge models and regional healthcare coalitions will be essential to meeting medical surge requirements.
RITN, working through the National Marrow Donor Program, established a network of over 60 U.S. academic medical centers to assist in patient management (Ross et al. 2011) by providing direct care for radiation injury and guidance to other professionals (Davids et al. 2010a). In an exercise, RITN demonstrated how the capacity to care for those who need management of radiation injury can be greatly enhanced by modifying the triage and medical care criteria (Davids et al. 2010b).
Summary and Conclusions
A nuclear incident would have devastating consequences. If prevention fails, an effective response could save tens to hundreds of thousands of lives. NIME describes a systematic approach with various interrelated and interdependent concepts, resources, tools and capabilities designed to facilitate such a response.
The critical impact of reducing radiation injury by sheltering in place for the first day or until authorities can provide evacuation guidance is a key primary response that can markedly reduce radiation casualty numbers (HSC 2010).
Medical interventions can be effective if implemented in a timely, strategic way. The science and technology for detection, diagnosis, MCMs and treatment will continually improve and CONOPS will be modified to take advantage of advances.
Given the catastrophic nature of a nuclear detonation, the entire country will be impacted and will need to respond. Responding effectively will include transferring patients to centers where expert care can be provided (e.g., RITN), sharing resources, recognizing and treating the intense psychological trauma that such an event will cause, and monitoring and supporting dislocated populations. The NIME systematic approach and enhanced models under development will enhance the effectiveness and capability for planners, responders and researchers and provide some assurance to members of the public that this complex incident has been considered.
Acknowledgments
The authors acknowledge the many individuals who have contributed to the programs that are a part of nuclear and radiological incident emergency management. These include subject matter experts and supporting staff from within and outside government, many of whom are co-authors of the papers describing the components and projects of the Nuclear Incident Medical Enterprise (NIME) that are in the references. The support of sequential Assistant Secretaries of Public Health Emergency Preparedness and Assistant Secretaries for Preparedness and Response has been essential: Stewart Simonson, Rear Admiral Craig Vanderwagen, and Rear Admiral Nicole Lurie. Particular thanks goes to Rear Admiral Ann Knebel whose leadership, vision, experience, tireless support, direct contributions, and enthusiasm were indispensable to the realization of many facets of NIME. Alicia Livinski from NIH Library for editorial assistance.
Footnotes
National Planning Scenarios remain “For Official Use Only.”
Conflicts of Interest: The authors report no conflicts of interest.
Disclaimer: The paper is the opinion of the authors and does not represent policy or conclusions of the National Cancer Institute, the National Institutes of Health, the Office of the Assistant Secretary for Preparedness and Response, the U.S. Department of Health and Human Services or the U.S. government.
References
- Armed Forces Radiobiology Research Institute. Bethesda, MD: AFRRI; [Accessed 10 March 2014]. 2014. [online]. Available at: http://www.afrri.usuhs.mil/ [Google Scholar]
- Assistant Secretary for Preparedness and Response. Washington, DC: ASPR; [Accessed 10 March 2014]. 2013a. Public health emergency medical countermeasures enterprise (PHEMCE) [online]. Available at: http://www.phe.gov/preparedness/mcm/phemce/Pages/default.aspx. [Google Scholar]
- Assistant Secretary for Preparedness and Response. Washington, DC: ASPR; [Accessed 10 March 2014]. 2013b. Global health security initiative (GHSI) [online]. Available at: http://www.phe.gov/preparedness/international/ghsi/pages/default.aspx. [Google Scholar]
- Assistant Secretary for Preparedness and Response. Washington, DC: ASPR; [Accessed 12 March 2014]. 2013c. ASPR fusion tools. [online]. Available at: https://www.phe.gov/about/oem/fusion/Pages/tools.aspx. [Google Scholar]
- Assistant Secretary for Preparedness and Response. Washington, DC: ASPR; [Accessed 3 March 2014]. 2013d. Office of policy and planning. [online]. Available at: https://www.phe.gov/about/opp/Pages/default.aspx. [Google Scholar]
- Assistant Secretary for Preparedness and Response, Office of Emergency Management. Washington, DC: ASPR; [Accessed 13 March 2014]. 2013e. CBRNE branch. [online]. Available at: https://www.phe.gov/about/oem/cbrne/pages/default.aspx. [Google Scholar]
- Assistant Secretary for Preparedness and Response. Washington, DC: ASPR; [Accessed 4 March 2014]. 2013f. National disaster medical system. [online]. Available at: http://www.phe.gov/preparedness/responders/ndms/pages/default.aspx. [Google Scholar]
- Assistant Secretary for Preparedness and Response. Washington, DC: ASPR; [Accessed 28 April 2014]. 2014a. Radiation emergency medical management: Download mobile REMM. [online]. Available at: http://www.remm.nlm.gov/downloadmremm.htm. [Google Scholar]
- Assistant Secretary for Preparedness and Response. Washington, DC: ASPR; [Accessed 2 September 2014]. 2014b. [online]. Available at: http://www.phe.gov. [Google Scholar]
- Assistant Secretary for Preparedness and Response. Washington, DC: ASPR; [Accessed 11 April 2014]. 2014c. Hospital preparedness program (HPP) [online]. Available at: http://www.phe.gov/PREPAREDNESS/PLANNING/HPP/Pages/default.aspx. [Google Scholar]
- BioDoseNet. Geneva: World Health Organization; [Accessed 10 March 2014]. 2014. Global biodosimetry laboratories network for radiation emergencies. [online]. Available at: http://www.who.int/ionizing_radiation/a_e/biodosenet/en/ [Google Scholar]
- Blumenthal DJ, Sugarman SL, Christensen DM, Wiley AL, Livingston GK, Glassman ES, Koerner JF, Sullivan JM, Hinds S. Role of dicentric analysis in an overarching biodosimetry strategy for use following a nuclear detonation in an urban environment. Health Phys. 2014;106:516–522. doi: 10.1097/HP.0b013e3182a5f94f. [DOI] [PubMed] [Google Scholar]
- Casagrande R, Wills N, Kramer E, Sumner L, Mussante M, Kurinsky R, McGhee P, Katz L, Weinstock DM, Coleman CN. Using the model of resource and time-based triage (MORTT) to guide scarce resource allocation in the aftermath of a nuclear detonation. Disaster Med Public Health Prep. 2011;5:S98–S110. doi: 10.1001/dmp.2011.16. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Atlanta, GA: CDC; [Accessed 10 March 2014]. 2013a. Radiation and your health. [online]. Available at: http://www.cdc.gov/nceh/radiation/ [Google Scholar]
- Centers for Disease Control and Prevention. Atlanta, GA: CDC; [Accessed 5 March 2014]. 2013b. Emergency preparedness and response. The laboratory response network partners in preparedness. [online]. Available at: http://www.bt.cdc.gov/lrn/ [Google Scholar]
- Centers for Disease Control and Prevention. Atlanta, GA: CDC; [Accessed 2 August 2014]. 2014a. Advisory team for environment, food, and health. [online]. Available at: http://www.crcpd.org/ATeam/Ateam.htm. [Google Scholar]
- Centers for Disease Control and Prevention. Atlanta, GA: CDC; [Accessed 2 August]. 2014b. Emergency preparedness and response. Resource library: communications and public information. [online]. Available at: http://www.bt.cdc.gov/radiation/resourcelibrary/communications.asp. [Google Scholar]
- Centers for Disease Control and Prevention. Atlanta, GA: CDC; [Accessed 27 April 2014]. 2014c. Agency for Toxic Substances and Disease Registry. Rapid response registry. [online]. Available at: http://www.atsdr.cdc.gov/rapidresponse/ [Google Scholar]
- Centers for Disease Control and Prevention. Atlanta, GA: CDC; [Accessed 10 April 2014]. 2014d. Emergency preparedness and response. Virtual community reception center. [online]. Available at: http://www.bt.cdc.gov/radiation/crc/vcrc.asp. [Google Scholar]
- Centers for Disease Control and Prevention, National Center for Environmental Health, Division of Environmental Hazards and Health Effects, Radiation Studies Branch. 2nd. Atlanta, GA: CDC; [Accessed 10 April 2014]. 2014e. Population monitoring in radiation emergencies: a guide for state and local public health planners. [online] Available at: http://emergency.cdc.gov/radiation/pdf/population-monitoring-guide.pdf. [Google Scholar]
- Coleman CN, Blakely WF, Fike JR, MacVittie TJ, Metting NF, Mitchell JB, Moulder JE, Preston RJ, Seed TM, Stone HB, Tofilon PJ, Wong RS. Molecular and cellular biology of moderate-dose (1–10 Gy) radiation and potential mechanisms of radiation protection: report of a workshop at Bethesda, Maryland, December 17–18, 2001. Radiat Res. 2003;159:812–834. doi: 10.1667/rr3021. [DOI] [PubMed] [Google Scholar]
- Coleman CN, Hrdina C, Bader JL, Norwood A, Hayhurst R, Forsha J, Yeskey K, Knebel A. Medical response to a radiologic/nuclear event: integrated plan from the office of the assistant secretary for preparedness and response, department of health and human services. Ann Emerg Med. 2009;53:213–222. doi: 10.1016/j.annemergmed.2007.12.021. [DOI] [PubMed] [Google Scholar]
- Coleman CN, Knebel AR, Hick JL, Weinstock DM, Casagrande R, Caro JJ, DeRenzo EG, Dodgen D, Norwood AE, Sherman SE, Cliffer KD, McNally R, Bader JL, Murrain-Hill P. Scarce resources for nuclear detonation: project overview and challenges. Disaster Med Public Health Prep. 2011a;5:S13–S19. doi: 10.1001/dmp.2011.15. [DOI] [PubMed] [Google Scholar]
- Coleman CN, Weinstock DM, Casagrande R, Hick JL, Bader JL, Chang F, Nemhauser JB, Knebel AR. Triage and treatment tools for use in a scarce resources-crisis standards of care setting after a nuclear detonation. Disaster Med Public Health Prep. 2011b;5:S111–S121. doi: 10.1001/dmp.2011.22. [DOI] [PubMed] [Google Scholar]
- Coleman CN, Adams S, Adrianopoli C, Ansari A, Bader JL, Buddemeier B, Caro JJ, Casagrande R, Case C, Jr, Caspary K, Chang AS, Chang HF, Chao N, Cliffer KD, Confer D, Deitchman S, Derenzo EG, Dobbs A, Dodgen D, Donnelly EH, Gorman S, Grace MB, Hatchett R, Hick JL, Hrdina C, Jones R, Kane E, Knebel A, Koerner JF, Laffan AM, Larson L, Livinski A, Mackinney J, Maidment BW, Manning R, Marinissen MJ, Martin C, Michael G, Murrain-Hill P, Nemhauser JB, Norwood AE, Nystrom S, Raheem M, Redlener I, Sheehan K, Simon SL, Taylor TP, Toner E, Wallace KS, Wieder J, Weinstock DM, Wiley AL, Jr, Yeskey K. Medical planning and response for a nuclear detonation: a practical guide. Biosecur Bioterror. 2012a;10:346–371. doi: 10.1089/bsp.2012.1025. [DOI] [PubMed] [Google Scholar]
- Coleman CN, Hrdina C, Casagrande R, Cliffer KD, Mansoura MK, Nystrom S, Hatchett R, Caro JJ, Knebel AR, Wallace KS, Adams SA. User-managed inventory: an approach to forward-deployment of urgently needed medical countermeasures for mass-casualty and terrorism incidents. Disaster Med Public Health Prep. 2012b;6:408–414. doi: 10.1001/dmp.2012.46a. [DOI] [PubMed] [Google Scholar]
- Coleman CN, Blumenthal DJ, Casto CA, Alfant M, Simon SL, Remick AL, Gepford HJ, Bowman T, Telfer JL, Blumenthal PM, Noska MA. Recovery and resilience after a nuclear power plant disaster: a medical decision model for managing an effective, timely, and balanced response. Disaster Med Public Health Prep. 2013;7:136–145. doi: 10.1017/dmp.2013.5. [DOI] [PubMed] [Google Scholar]
- Dainiak N, Gent RN, Carr Z, Schneider R, Bader J, Buglova E, Chao N, Coleman CN, Ganser A, Gorin C, Hauer-Jensen M, Huff LA, Lillis-Hearne P, Maekawa K, Nemhauser J, Powles R, Schunemann H, Shapiro A, Stenke L, Valverde N, Weinstock D, White D, Albanese J, Meineke V. First global consensus for evidence-based management of the hematopoietic syndrome resulting from exposure to ionizing radiation. Disaster Med Public Health Prep. 2011a;5:202–212. doi: 10.1001/dmp.2011.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dainiak N, Gent RN, Carr Z, Schneider R, Bader J, Buglova E, Chao N, Coleman CN, Ganser A, Gorin C, Hauer-Jensen M, Huff LA, Lillis-Hearne P, Maekawa K, Nemhauser J, Powles R, Schunemann H, Shapiro A, Stenke L, Valverde N, Weinstock D, White D, Albanese J, Meineke V. Literature review and global consensus on management of acute radiation syndrome affecting nonhematopoietic organ systems. Disaster Med Public Health Prep. 2011b;5:183–201. doi: 10.1001/dmp.2011.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davids MS, Case C, Jr, Confer DL, Weisdorf DJ, Weinstock DM. Medical management of radiation victims in the United States. Health Phys. 2010a;98:833–837. doi: 10.1097/01.HP.0000346701.04476.0d. [DOI] [PubMed] [Google Scholar]
- Davids MS, Case C, Jr, Hornung R, 3rd, Chao NJ, Chute JP, Coleman CN, Weisdorf D, Confer DL, Weinstock DM. Assessing surge capacity for radiation victims with marrow toxicity. Biol Blood Marrow Transplant. 2010b;16:1436–1441. doi: 10.1016/j.bbmt.2010.04.007. [DOI] [PubMed] [Google Scholar]
- Department of Homeland Security. Washington, DC: DHS; [Accessed 13 March 2014]. 2007. National preparedness guidelines. [online]. Available at: http://www.fema.gov/pdf/emergency/nrf/National_Preparedness_Guidelines.pdf. [Google Scholar]
- Department of Homeland Security. Washington, DC: DHS; [Accessed 13 March 2014]. 2011. The strategic national risk assessment in support of PPD 8: a comprehensive risk-based approach toward a secure and resilient nation. [online]. Available at: http://www.dhs.gov/xlibrary/assets/rma-strategic-national-risk-assessment-ppd8.pdf. [Google Scholar]
- Department of Homeland Security. Washington, DC: DHS; [Accessed 20 March 2014]. 2013. Interagency modeling and atmospheric assessment center (IMAAC) [online]. Available at: http://www.dhs.gov/imaac. [Google Scholar]
- Environmental Protection Agency. Washington, DC: EPA; [Accessed 2 August 2014]. 2013. PAG manual: Protective action guides and planning guidance for radiological incidents. [online]. Available at: http://www.epa.gov/radiation/docs/er/pag-manual-interim-public-comment-4-2-2013.pdf. [Google Scholar]
- Federal Emergency Management Agency. Washington, DC: FEMA; [Accessed 10 March 2014]. 2008. Nuclear/radiological incident annex. [online]. Available at: http://www.fema.gov/pdf/emergency/nrf/nrf_nuclearradiologicalincidentannex.pdf. [Google Scholar]
- Federal Emergency Management Agency. Washington, DC: FEMA; [Accessed 10 March 2014]. 2013a. Emergency support function #8 - public health and medical services annex. [online]. Available at: http://www.fema.gov/media-library/assets/documents/32198?id=7359. [Google Scholar]
- Federal Emergency Management Agency, Nuclear/Radiological Communications Working Group. Washington, DC: FEMA; [Accessed 2 August 2014]. 2013b. Improvised nuclear device response and recovery: communicating in the immediate aftermath. [online]. Available at: http://www.fema.gov/media-library/assets/documents/33036?id=7659. [Google Scholar]
- Government Accountability Office. Washington, DC: GAO; [Accessed 2 August 2014]. 2013. Nuclear terrorism response plans: Major cities could benefit from federal guidance on responding to nuclear and radiological attacks. [online]. Available at: http://www.gao.gov/assets/660/658336.pdf. [Google Scholar]
- Grace MB, Cliffer KD, Moyer BR, Coleman CN, Prasher JM, Hatchett R, Mercier J, Manning RG, Bader JL, Disbrow GL, Kovacs GR. The U.S. government's medical countermeasure portfolio management for nuclear and radiological emergencies: Synergy from interagency cooperation. Health Phys. 2011;101:238–247. doi: 10.1097/HP.0b013e3182135fba. [DOI] [PubMed] [Google Scholar]
- Hatchett RJ. Slow progress in preparing for radiological and nuclear emergencies. Disaster Med Public Health Prep. 2011;5:180–182. doi: 10.1001/dmp.2011.70. [DOI] [PubMed] [Google Scholar]
- Homeland Security Council, Interagency Policy Coordination Subcommittee for Preparedness and Response to Radiological and Nuclear Threats. 2nd. Bethesda, MD: HSC, U.S. Department of Health and Human Services; [Accessed 7 March 2014]. 2010. Planning guidance for response to a nuclear detonation. [online]. Available at: http://www.remm.nlm.gov/PlanningGuidanceNuclearDetonation.pdf. [Google Scholar]
- Hrdina CM, Coleman CN, Bogucki S, Bader JL, Hayhurst RE, Forsha JD, Marcozzi D, Yeskey K, Knebel AR. The “RTR” medical response system for nuclear and radiological mass-casualty incidents: a functional triage-treatment-transport medical response model. Prehosp Disaster Med. 2009;24:167–178. doi: 10.1017/s1049023x00006774. [DOI] [PubMed] [Google Scholar]
- Knebel AR, Coleman CN, Cliffer KD, Murrain-Hill P, McNally R, Oancea V, Jacobs J, Buddemeier B, Hick JL, Weinstock DM, Hrdina CM, Taylor T, Matzo M, Bader JL, Livinski AA, Parker G, Yeskey K. Allocation of scarce resources after a nuclear detonation: setting the context. Disaster Med Public Health Prep. 2011;5:S20–S31. doi: 10.1001/dmp.2011.25. [DOI] [PubMed] [Google Scholar]
- Koerner JF, Coleman CN, Murrain-Hill P, FitzGerald DJ, Sullivan JM. The medical decision model and decision maker tools for management of radiological and nuclear incidents. Health Phys. 2014;106(6):645–651. doi: 10.1097/HP.0000000000000053. [DOI] [PubMed] [Google Scholar]
- Murrain-Hill P, Coleman CN, Hick JL, Redlener I, Weinstock DM, Koerner JF, Black D, Sanders M, Bader JL, Forsha J, Knebel AR. Medical response to a nuclear detonation: creating a playbook for state and local planners and responders. Disaster Med Public Health Prep. 2011;5:S89–S97. doi: 10.1001/dmp.2011.13. [DOI] [PubMed] [Google Scholar]
- National Academies/Institute of Medicine, Board on Health Sciences Policy. Nationwide response issues after an improvised nuclear device attack: medical and public health considerations for neighboring jurisdictions: an Institute of Medicine workshop. Washington, DC: National Academies Press; 2013. [PubMed] [Google Scholar]
- National Academies/Institute of Medicine. Nationwide response issues after an improvised nuclear device attack: medical and public health considerations for neighboring jurisdictions: Workshop summary. Washington, DC: National Academies Press; 2014. [PubMed] [Google Scholar]
- National Cancer Institute, Division of Cancer Treatment and Diagnosis. Bethesda, MD: NCI; [Accessed 2 March 2014]. 2013a. Radiation research program. [online]. Available at: http://dctd.cancer.gov/programpages/rrp/partnerships_radiation_bioterrorism.htm. [Google Scholar]
- National Cancer Institute, Division of Cancer Epidemiology and Genetics, Radiation Epidemiology Branch. Bethesda, MD: NCI; [Accessed 10 March 2014]. 2013b. Understanding the link between radiation exposure and cancer. [online]. Available at: http://dceg.cancer.gov/about/organization/programs-ebp/reb. [Google Scholar]
- National Council on Radiation Protection and Measurements. Bethesda, MD: NCRP; [Accessed 2 August 2014]. 2013. National crisis: Where are the radiation professionals (WARP)? [online]. Available at: http://www.ncrponline.org/PDFs/2013/WARP_Workshop_Summary.pdf. [Google Scholar]
- National Institute of Allergy and Infectious Diseases. Bethesda, MD: NIAID; [Accessed 4 March 2014]. 2013. Radiation and nuclear countermeasures program. [online]. Available at: http://www.niaid.nih.gov/topics/radnuc/pages/default.aspx. [Google Scholar]
- National Library of Medicine. Bethesda, MD: NLM; [Accessed 20 March 2014]. 2014a. Radiation emergency medical management: REMM. [online]. Available at: http://remm.nlm.gov. [Google Scholar]
- National Library of Medicine. Bethesda, MD: NLM; [Accessed 30 April 2014]. 2014b. Radiation emergency medical management: exposure: diagnose/manage acute radiation syndrome. [online]. Available at: http://www.remm.nlm.gov/exposureonly.htm#skip. [Google Scholar]
- National Library of Medicine. Bethesda, MD: NLM; [Accessed 27 April 2014]. 2014c. Radiation emergency medical management: Dose estimator for exposure: 3 biodosimetry tools. [online]. Available at: http://www.remm.nlm.gov/ars_wbd.htm. [Google Scholar]
- National Marrow Donor Program. Knoxville, TN: NMDP; [Accessed 4 March 2014]. 2014. Radiation Injury Treatment Network. [online]. Available at: http://www.ritn.net/ [Google Scholar]
- New York State Department of Health. Bethesda, MD: National Library of Medicine; [Accessed 27 April 2014]. 2014. Community reception center (CRC) form. [online]. Available at: http://www.remm.nlm.gov/Empire-09-Tracking-and-Epi-form-FINAL.pdf. [Google Scholar]
- Bozeman, MT: RRS; [Accessed 2 August 2014]. 2014. Radiation Research Society. [online]. Available at: http://www.radres.org. [Google Scholar]
- Ross JR, Case C, Confer D, Weisdorf DJ, Weinstock D, Krawisz R, Chute J, Wilhauk J, Navarro W, Hartzman R, Norman Coleman C, Hatchett R, Chao N. Radiation Injury Treatment Network (RITN): healthcare professionals preparing for a mass casualty radiological or nuclear incident. Int J Radiat Biol. 2011;87:748–753. doi: 10.3109/09553002.2011.556176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan JM, Prasanna PG, Grace MB, Wathen LK, Wallace RL, Koerner JF, Coleman CN. Assessment of biodosimetry methods for a mass-casualty radiological incident: medical response and management considerations. Health Phys. 2013;105:540–554. doi: 10.1097/HP.0b013e31829cf221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, Ionizing Radiation Programme. Geneva: WHO; [Accessed 4 March 2014]. 2014. REMPAN collaborating centres and liaision institutions. [online]. Available at: http://www.who.int/ionizing_radiation/a_e/rempan/en/ [Google Scholar]


