Abstract
Purpose
this study was conducted to assess the safety and efficacy of a new surgical technique for anatomical reconstruction of the coracoclavicular (CC) and acromioclavicular (AC) ligaments using one single-strand semitendinosus tendon graft.
Methods
eighteen patients affected by chronic type III–V AC joint dislocations were included in the present study between January 2010 and March 2012. All underwent the same surgical operation and rehabilitation protocol. The semitendinosus tendon was harvested from the ipsilateral knee. The CC and AC ligaments were reconstructed using the graft passed beneath the coracoid and through bone tunnels in the clavicle and in the acromion. The graft was secured with non-absorbable sutures. Radiographic recurrence of AC joint dislocation was the primary outcome. Clinical outcome was assessed using the DASH score and normalized Constant score. Wilcoxon’s signed-rank test was used for comparison between pre- and postoperative results. Significance was set at p ≤ 0.05.
Results
the mean follow-up duration was 26.4±2.3 months (range: 24–30 months). On X-ray evaluation, only two patients (11%) showed asymptomatic recurrence of AC joint instability. Comparison between pre- and postoperative DASH and Constant scores showed significant clinical improvement (p<0.001).
Conclusion
anatomical reconstruction of CC and AC ligaments using an autologous semitendinosus tendon graft for the treatment of AC joint dislocation provided good and reliable clinical and radiological results with a low failure rate at short-term follow-up.
Level of evidence
level IV, therapeutic case series.
Keywords: acromioclavicular, coracoclavicular, dislocation, reconstruction, semitendinosus
Introduction
Acromioclavicular (AC) joint injuries are common and account for about 12% of all shoulder injuries in clinical practice (1), a rate that increases to almost 40% in athletes participating in contact sports (2, 3). This may actually be an underestimation of the true prevalence of these injuries since many individuals with low-grade injuries, i.e. type I or II according to Rockwood et al. (4), may not seek medical attention (5). A recent longitudinal cohort study reported an incidence of 9.2/1000 AC joint injuries among young athletes. In particular, male athletes seem to be at greater risk than female athletes (6). This is most likely due to different patterns of risk-taking behavior and participation in contact sports, rather than to anatomical differences between the genders. Most AC joint injuries occur in the third decade of life and AC joint dislocations are commonly sustained as a result of participation in sports such as football, soccer, hockey, rugby, cycling and skiing (2, 3, 5, 7–9). The mechanism of injury leading to a dislocation can be direct or indirect. The most common cause is a direct blow to the shoulder with the arm in adduction. Due to the high strength of the sternoclavicular joint, the AC joint and the clavicle are weak points, particularly susceptible to injury (7,10). The AC capsule-ligamentous structures are first to fail, leading to increased loading of the coracoclavicular (CC) ligaments.
Despite the frequency of these injuries, many aspects of their treatment remain unresolved.
Conservative therapy is widely accepted as the gold standard for Rockwood type I and II injuries (4) and there is also consensus that type IV to VI dislocations should usually be treated surgically (11). Instead, treatment for type III lesions remains controversial (12, 13). Conservative treatment of type III AC joint dislocations is widespread and several promising results have been published (14, 15). However, some au thors have reported residual symptoms such as pain and weakness after conservative treatment of type III injuries; therefore, operative reconstruction has been recommended in young patients who have physically demanding occupations or participate in sports activities (16, 17).
Nowadays, there is huge variability in surgical indications and available surgical techniques in this setting. Because of the distinct functional anatomy of the two CC ligaments (the conoid and the trapezoid) there has been a tendency to focus on anatomical reconstruction of these structures to obtain improved function and stability (18–20). Open and arthroscopic techniques for reconstructing the conoid and trapezoid ligaments have been developed. Recently, several clinical studies reported promising results with procedures using biodegradable screw or cortical button fixation with or without the use of a tendon graft (21, 22). As this approach alone does not directly address the disrupted AC ligament complex, horizontal instability due to insufficient healing could result. While the CC ligaments are widely recognized to be responsible for vertical stability (23), horizontal stability is mainly attributed to the AC joint complex (24). Since it has been shown clinically that horizontal instability of the AC joint may result in severe chronic pain and functional shoulder impairment (25), there is growing interest in specific techniques thought to improve horizontal stability.
The purpose of the present study was to present a new technique for anatomical reconstruction of the CC and AC ligaments using an autologous semitendinosus tendon graft. Moreover, we report the functional and radiological outcome of this surgical procedure applied in 18 patients affected by chronic Rockwood type III–V AC joint dislocations.
Our starting hypothesis was that this technique would give equivalent or superior functional results compared with those reported in the literature for other surgical procedures and that the additional AC ligament reconstruction would lead to improved horizontal stability and radiological results with a lower rate of re-dislocation.
Methods
This study was designed as a prospective case series, to assess the safety and efficacy of a surgical technique for anatomical reconstruction of the CC and AC ligaments using one, single-strand semitendinosus tendon graft.
Inclusion and exclusion criteria
The indications for surgery were the presence of chronic type III–V AC joint dislocation with pain and discomfort at the affected shoulder with restriction of working activities and/or activities of daily living. AC joint dislocation was considered chronic when the interval from injury to our observation was longer than two months.
All the patients underwent a radiographic study (anteroposterior, axillary and Zanca views), to assess the type of AC joint dislocation, and a magnetic resonance imaging scan to rule out concomitant rotator cuff pathology and to evaluate degenerative changes of the articular surfaces of the AC joint and glenohumeral (GH) joint.
Exclusion criteria were: age under 18 years, concomitant rotator cuff tears (partial thickness or full-thickness), a history of previous ligament reconstruction procedures that had required harvesting of the semitendinosus tendon from the ipsilateral or contralateral knee, a history of traumatic injuries and/or previous surgery to the same shoulder, and degenerative changes of the GH joint.
Population
A total of 18 patients (1 woman and 17 men) affected by chronic type III–V AC joint dislocations were included in the present study between January 2010 and March 2012. They were aged between 21 and 49 years (mean age: 27.5±8.2 years) and they presented type III (8 cases), type IV (4 cases) or type V (6 cases) dislocations. In all cases the dislocation had been caused by a direct trauma to the shoulder, in six cases sustained in an accidental fall during working activities, in eight cases in a traffic accident, and in four cases while practicing sport. Eleven patients were manual workers and seven had sedentary occupations. The following types of sport were practiced: collision sport in two cases, contact sport in four cases, overhead sport in three cases, and non-contact sport in five cases. Four patients did not practice sports activities.
Intervention
In each case, a standard operating room table was set up in a beach chair position at 60° of flexion. The patient was positioned as laterally as was safely possible. A small pad was placed beneath the medial border of the scapula. This serves to stabilize the scapula, and also raises the shoulder away from the table thereby improving access to the clavicle, which is critical when drilling bone tunnels. The operating field was draped from the sternoclavicular joint to the neck; the draping also extended to several centimeters behind the posterior aspect of the clavicle, including the upper arm.
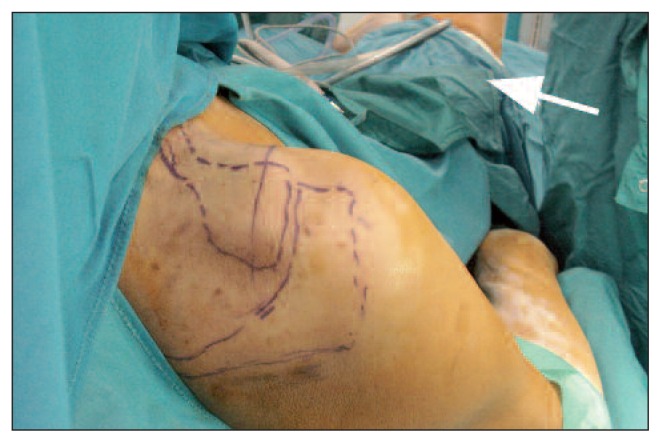
A second operating field was prepared for harvesting the semitendinosus tendon graft from the ipsilateral side. The leg was placed in a figure-of-four position and a side support was usually used. A tourniquet was then placed on the proximal thigh (Fig. 1).
Fig. 1.
Patient positioning for surgical procedure. The operating room table is set up in a beach chair position at 60° of flexion. The patient is positioned as laterally as possible. The draping extends to several centimeters behind the posterior aspect of the clavicle, including the upper arm. A second operating field is prepared for harvesting the semitendinosus tendon graft from the ipsilateral side (arrow).
Graft harvesting
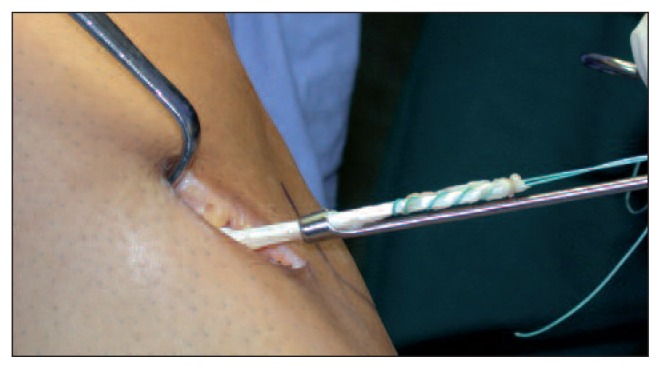
A 3-cm oblique skin incision was performed over the pes anserinus. An oblique incision was preferred to a vertical one to lessen the risk of injury to the infrapatellar branch of the saphenous nerve. The soft tissues were dissected down to the sartorial fascia, and the semitendinosus was visualized. The fascia was then incised, and the semitendinosus was identified and bluntly dissected with a right-angle clamp. Blunt dissection was continued medially to define the interval between the superficial medial collateral ligament and the semitendinosus tendon. The tendon was then sharply released from its insertion on the proximal tibia and whip-stitched with a No.2 FiberWire (Arthrex, Naples, FL, USA). Blunt dissection was used to identify any adhesions around the tendon and to separate the tendon from the fascia of the medial head of the gastrocnemius. The tendon was then released from its distal muscle-tendon junction by means of a tendon stripper and taken to the back table for preparation (Fig. 2). The fascia was closed with a No. 1 Vicryl suture (Ethicon, Somerville, NJ), whereas the subcutaneous tissue was closed with No. 2-0 Vicryl suture (Ethicon). A 3.0 Vycril suture was used for skin closure.
Fig. 2.
Graft harvesting. The tendon is released from its distal muscle-tendon junction by means of a tendon stripper.
Graft preparation
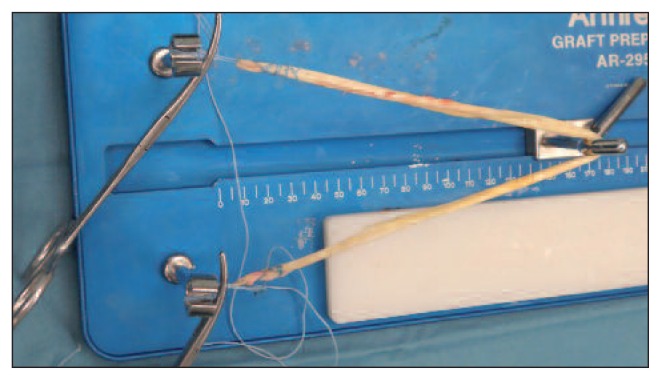
After freeing the graft from the remnant muscle tissue, the proximal end of the graft was whip-stitched with another No. 2 FiberWire (Arthrex). The stitches applied to the graft ends served to make the distal diameter of the graft as small as possible in order to facilitate its passage through small tunnels and prevent fraying of the graft edges. The graft length and diameter were then evaluated using a graft sizer. The graft was usually 20–25 cm in length and 4.5–5 mm in diameter. It was then mounted and fixed on a traction device (Arthrex) with clamps. Pre-tensioning was applied manually and maintained for at least 20 minutes (Fig. 3).
Fig. 3.
Graft preparation. The graft is whip-stitched with one No. 2 FiberWire at both ends and mounted on a traction device with clamps. Pre-tensioning is maintained for at least 20 minutes.
AC joint preparation
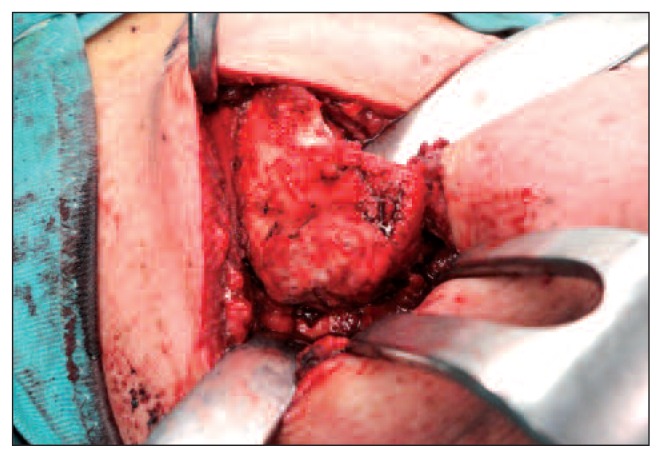
A perpendicular skin incision, 5–6 cm in length, was made, running about 1.5 cm medial to the AC joint, from the posterior edge of the clavicle to the tip of the coracoid (Fig. 4). The deltotrapezial fascia was incised along with the superior aspect of the clavicle, respecting the natural demarcation between the trapezius insertion onto the posterior aspect of the clavicle and the deltoid origin on the anterior clavicle. This incision extended medially beyond the conoid ligament insertion and laterally over the AC joint and the anterior third of the acromion. Needle tip electrocautery was used to begin raising flaps off the bone before using an elevator. In addition, tagging stitches were placed in the flaps to facilitate accurate re-approximation at closure. Retractors were used to retract the flaps. The exposure was completed by freeing the distal clavicle and AC joint of soft tissues that were preventing joint reduction (Fig. 5). The clavicle was also released from the trapezial fascia in type IV separations.
Fig. 4.
Surgical approach. A perpendicular skin incision, 5–6 cm in length, is made, running about 1.5 cm medial to the AC joint, from the posterior edge of the clavicle to the tip of the coracoid.
Fig. 5.
Surgical approach. The deltotrapezial fascia is incised along with the superior aspect of the clavicle, respecting the natural demarcation between the trapezius insertion onto the posterior aspect of the clavicle and the deltoid origin on the anterior clavicle. The exposure is completed by freeing the distal clavicle and AC joint of soft tissues that might prevent joint reduction.
The reducibility of the dislocation was assessed by pushing up on the elbow to elevate the scapulohumeral complex. Visual inspection was usually adequate for assessing reduction.
The clavicle was prepared by drilling bone tunnels in the anatomical locations of the CC ligaments. The conoid ligament tunnel was placed 40 mm medial to the AC joint and at the posterior aspect of the clavicle. Furthermore, the conoid tubercle was palpated on the undersurface of the clavicle and used as a secondary reference landmark. After placement of a 2.4-mm guide pin, a 5-mm tunnel was made using a cannulated reamer passed over the guide pin, with a “ream-in, pull out” technique. Next, the trapezoid ligament tunnel was prepared in the same manner. It was placed in the middle of the superior aspect of the clavicle and 20 mm lateral to the conoid tunnel. Then, a third tunnel in the medial end of the acromion was prepared in the same manner. It was placed 10 mm lateral to the medial aspect of the acromion, in line with the trapezoid ligament tunnel (Fig. 6).
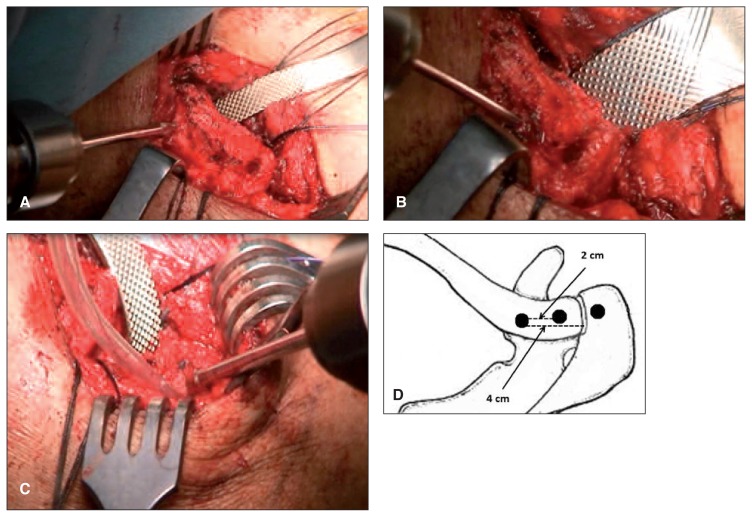
Fig. 6.
Tunnel placement. The conoid ligament tunnel is placed 40 mm medial to the AC joint and at the posterior aspect of the clavicle (A). The trapezoid ligament tunnel is placed in the middle of the superior aspect of the clavicle and 20 mm lateral to the conoid tunnel (B). A third tunnel in the medial end of the acromion is placed 10 mm lateral to the medial aspect of the acromion, in line with the trapezoid ligament tunnel (C). The line drawing shows the positioning of the three bone tunnels (D).
Graft passage and fixation
The graft was passed into the tunnels and beneath the coracoids, either using a shuttling PDS (Ethicon, Somerville, NJ, USA) stitch and a curved clamp or a flexible suture passing device. A No.2 FiberWire and a No. 2 TigerWire (Arthrex) were passed with the graft into the clavicular tunnels to provide additional initial non-biological fixation of the CC ligaments. The graft was passed from the conoid ligament tunnel beneath the coracoid (from medial to lateral) into the trapezoid ligament tunnel and over the acromion into the acromial tunnel and again into the trapezoid ligament tunnel like a loop. The AC joint was then manually reduced. Prior to fixation, the quality of reduction was examined visually. While an assistant maintained the reduction, the free ends of the FiberWire and TigerWire were first tensioned and then tied. Then, the sutures of the graft exiting the trapezoid tunnel were tensioned and tied over the graft in order to reconstruct the superior and inferior AC ligaments. Similarly, the other limb of the graft (exiting the conoid tunnel) was tensioned to secure the reduction and was fixed on the superior aspect of the clavicle to the part of the graft running from the trapezoid tunnel to the AC joint, for additional security and reinforcement of the repair (Fig. 7).
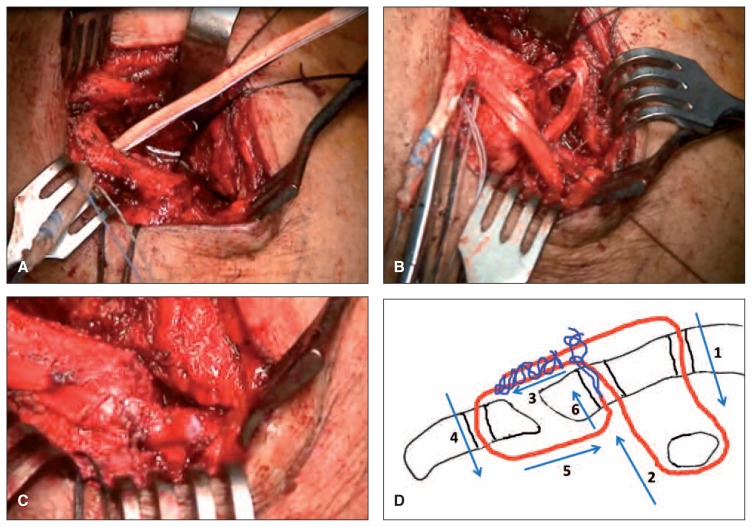
Fig. 7.
Graft passage and fixation. The graft is passed from the conoid ligament tunnel beneath the coracoid (from medial to lateral) (A). The graft is then passed into the trapezoid ligament tunnel and over the acromion into the acromial tunnel and again into the trapezoid ligament tunnel (B). The sutures of the graft exiting the trapezoid tunnel are tied over the graft in order to reconstruct the superior and inferior AC ligaments. The other limb of the graft (exiting the conoid tunnel) is fixed on the superior aspect of the clavicle to the part of the graft running from the trapezoid tunnel to the AC joint (C). The line drawing shows the steps of graft passage and fixation (D).
Closure
The deltotrapezial fascia was carefully closed with interrupted non-absorbable sutures (No. 2 Ethibond; Ethicon). Attachments of the anterior deltoid fascia and of the trapezius fascia were brought together with interrupted stitches. The knots were placed on the posterior side of the flap to minimize skin irritation. The subcutaneous layer was closed with 2.0 Vicryl (Ethicon) sutures, and a 3.0 Vycril suture was used for skin closure.
Postoperative rehabilitation
During the first six weeks, the patients wore a Kenny-Howard sling which provides support and protects the surgical repair against the pull of gravity. After removal of the sling, a rehabilitation program was undertaken, which was divided into three phases, each lasting four weeks:
Phase one: prevention of scar adhesions, full recovery of passive range of motion.
Phase two: closed kinetic chain exercises to strengthen the rotator cuff, the subscapularis tendon and the scapular stabilizers.
Phase three: open kinetic chain exercises, proprioceptive and plyometric exercises, postural rehabilitation of the kinetic chain (lumbopelvic, lumbar thoracic, scapulothoracic).
Return to sports activities and heavy manual work was allowed 4–6 months after surgery.
Outcome measurements
Radiographic recurrence of AC dislocation was considered the primary outcome of the study. Secondary outcomes included: assessment of disability-related quality of life and evaluation of global functional status of the operated shoulder.
All patients underwent a radiographic study (anteroposterior, axillary and Zanca views) to assess recurrence of AC joint instability, defined as subluxation or frank re-dislocation. The outcome was dichotomized (yes or no) according to the presence of a complete anatomical reduction of the AC joint in both the coronal and the axial plane.
Disability-related quality of life was assessed using the national validated version of the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire (26). This is a self-administered questionnaire which measures physical ability and symptoms of the upper extremity and explores the impact of functional impairment and pain on daily living tasks as well as on social and recreational activities, work and sleep. The scoring system of the questionnaire is based on a metric scale, ranging from 0 (minimum disability, best result) to 100 points (maximum disability, poorest result).
Functional evaluation of the shoulder was performed using the Constant-Murley shoulder outcome score (herein referred to as the Constant score), which is recommended by the European Society of Shoulder and Elbow Surgery (SECEC/ESSE) for assessing shoulder disorder treatment outcomes. The scoring system is based on subjective (sleep, work, recreational activities) and objective (range of motion and strength) components, adjusted for age and gender, according to normative data reported by Yian et al. (27). The summary score ranges from 0 (worst result) to 100 (best result). A final radiographic and clinical follow-up was scheduled for all the patients at two years after surgery. Secondary outcome measures were collected at baseline and at follow-up visits by an investigator blind to the treatment undertaken.
Statistical analysis
Statistical analysis was performed by an independent data analyst using the SPSS version 17.0 software (SPSS, Chicago, Illinois). The Wilcoxon signed-rank test was used for comparison between pre- and postoperative results. Spearman’s rank correlation coefficient was calculated for subgroup analysis according to the following predictors of outcome: age, type of dislocation, type of work, and type of sport. The significance level was set at p ≤ 0.05.
Results
All the patients were available for follow-up. The mean follow-up duration was 26.4±2.3 months (range: 24–30 months).
On the basis of the radiological findings, only two patients (11%) showed recurrence of AC joint instability. Specifically, they had asymptomatic AC joint subluxation in the coronal plane.
Clinically, significant differences were found (p<0.001) between the mean pre- and postoperative overall DASH (89.3±5.7 preop vs 6.6±8.4 postop) and Constant (58.5±7.2 preop vs 90.3±4.9 postop) scores. Subgroup analysis revealed no differences in outcomes according to age, type of dislocation, type of work, and type of sport practiced (Tab. 1).
Table 1.
Subgroup analysis according to predictors of outcome.
| Predictors of outcome | DASH score | Constant score | ||
|---|---|---|---|---|
|
| ||||
| rho coefficient | p | rho coefficient | p | |
| Age | 0.027 | 0.916 | 0.341 | 0.166 |
| Type of dislocation | 0.111 | 0.661 | −0.113 | 0.654 |
| Type of work | 0.308 | 0.214 | −0.253 | 0.311 |
| Type of sport | 0.002 | 0.995 | −0.182 | 0.471 |
Discussion
Surgical treatment of AC joint dislocations has been performed since 1861 (28). To date, over 80 different surgical techniques have been described. This is likely due to a general dissatisfaction with available treatment options. Historically, primary fixation of the AC joint consisted of pin fixation using either smooth or threaded Kirschner wires after a closed or open reduction. In 1941, Bosworth popularized the use of a percutaneous screw for CC fixation (29). In 1976, Balser (30) first introduced the hook plate for stabilization of AC dislocations. This plate was fixed, with screws, on the top of the distal end of the clavicle and ensured AC reduction by means of a transarticular hook engaging at the undersurface of the acromion. Unfortunately, these techniques were often associated with hardware-related complications that required implant removal. Subsequently, a multitude of soft tissue surgeries were described, whose aim was to recreate the function of the disrupted CC and/or AC ligaments. Transfer of the coracoacromial (CA) ligament from the acromion into the resected distal clavicle was first suggested by Cadenat in 1917 (31) and reported in 1972 by Weaver and Dunn (32). Since then, a large number of modifications have been described. However, many of these modified Weaver-Dunn procedures have since been abandoned because of their high re-dislocation rates (33–35), which are probably due to the fact that the transferred ligaments are not as strong as the native CC ligaments and cannot reproduce their normal anatomy. As a result, anatomical CC ligament reconstructions, which aim to recreate the anatomy of the CC ligaments utilizing stronger autogenic, allogeneic or synthetic graft materials, have been developed in the hope of decreasing complication rates and improving stability and functional outcomes. Over the past decades, the management of the distal clavicle in the setting of AC dislocations has also evolved. In 1941 Mumford (36) popularized the isolated distal clavicle excision (DCE) for the treatment of AC dislocations. Even though this technique gave poor results because it failed to address the instability (37), DCE has been incorporated into many subsequent procedures used to treat AC instability, especially chronic instability, in order to remove a potential pain generator and prevent AC joint osteoarthritis.
The surgical technique described in this paper is based on knowledge of the anatomy and biomechanics of the AC joint as well as of the history of previous techniques used to address AC dislocations. It includes an anatomical reconstruction of the CC and AC ligaments using a free tendon graft without any fixation device, only high-strength non-absorbable sutures, and it conserves the AC joint.
A body of biomechanical (38–41) and clinical (42) data has shown anatomical CC ligament reconstruction using autologous semitendinosus tendon to be superior to the Weaver-Dunn procedure and also to more closely reproduce the function of the native CC ligaments. Recently, several anatomical techniques using different fixation devices, such as biotenodesis screws (21, 43) or buttons (44, 45), have been described. Despite good clinical outcomes (43), complications related to clavicle fractures and hardware failure have been reported (46–48). In an attempt to minimize complications and favor a biological environment, we decided not to use any fixation device, but rather sutures.
The decision to retain the AC joint is somewhat controversial. A recent biomechanical study showed that resection of the distal clavicle leads to increased horizontal translation, therefore, only sparing resection of the distal clavicle should be performed, and only if strictly indicated (49).
Moreover, there is no strong clinical evidence to support routinely performing a concomitant DCE. Some authors (50) did not report any additional improvement after a concomitant DCE. Others (51, 52) reported that when the AC joint is retained, some patients will develop symptomatic osteoarthritis that can require future treatment. However, none of the patients included in our series complained of AC joint pain, even at two years after surgery. We decided to retain the AC joint because it has been shown to improve the horizontal stability of the repair.
Our case series underwent a single reconstructive technique and further studies are required to allow direct comparisons of this technique with different operations. However, only two of our patients showed asymptomatic subluxation, a result which compares favorably with previous studies.
The main goal of the surgical approach is to reduce the dislocation and create an environment for proper soft tissue healing and, subsequently, persistent AC joint stability. Reviewing the current literature, it remains uncertain which technique provides best restoration of the AC joint anatomy and whether postoperative radiological alterations of the AC joint anatomy influence the functional outcome. The technique described in the present study allows an anatomical and biological reconstruction of the CC and AC ligaments because it uses autografts without any additional fixation device, only sutures, in order to minimize the risk of complications already encountered after using screws or metal implants.
In conclusion, anatomical reconstruction of CC and AC ligaments using an autologous semitendinosus tendon graft for the treatment of AC joint dislocation provided good and reliable clinical and radiological results with a low failure rate at short-term follow-up.
References
- 1.Emery R. Acromioclavicular and sternoclavicular joints. In: Copeland S, editor. Shoulder Surgery. WB Saunders; London: 1997. [Google Scholar]
- 2.Stuart MJ, Smith A. Injuries in Junior A ice hockey. A three-year prospective study. Am J Sports Med. 1995;23:458–461. doi: 10.1177/036354659502300415. [DOI] [PubMed] [Google Scholar]
- 3.Headey J, Brooks JH, Kemp SP. The epidemiology of shoulder injuries in English professional rugby union. Am J Sports Med. 2007;35:1537–1543. doi: 10.1177/0363546507300691. [DOI] [PubMed] [Google Scholar]
- 4.Rockwood C, Williams G, Young D. Disorders of the acromioclavicular joint. In: Rockwood CJ, Matsen FA, editors. The Shoulder. 2nd edition. WB Saunders; Philadelphia: 1998. pp. 483–553. [Google Scholar]
- 5.Fraser-Moodie JA, Shortt NL, Robinson CM. Injuries to the acromioclavicular joint. J Bone Joint Surg Br. 2008;90:697–707. doi: 10.1302/0301-620X.90B6.20704. [DOI] [PubMed] [Google Scholar]
- 6.Pallis M, Cameron KL, Svoboda SJ, et al. Epidemiology of acromioclavicular joint injury in young athletes. Am J Sports Med. 2012;40:2072–2077. doi: 10.1177/0363546512450162. [DOI] [PubMed] [Google Scholar]
- 7.Mazzocca AD, Arciero RA, Bicos J. Evaluation and treatment of acromioclavicular joint injuries. Am J Sports Med. 2007;35:316–329. doi: 10.1177/0363546506298022. [DOI] [PubMed] [Google Scholar]
- 8.Willimon SC, Gaskill TR, Millett PJ. Acromioclavicular joint injuries: anatomy, diagnosis, and treatment. Phys Sportsmed. 2011;39:116–122. doi: 10.3810/psm.2011.02.1869. [DOI] [PubMed] [Google Scholar]
- 9.Millett PJ, Braun S, Gobezie R, et al. Acromioclavicular joint reconstruction with coracoacromial ligament transfer using the docking technique. BMC Musculoskelet Disord. 2009;10:6. doi: 10.1186/1471-2474-10-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iannotti JP, Williams GR. Disorders of the Shoulder: Diagnosis and Management. Lippincott Williams & Wilkins; Philadelphia: 1999. [Google Scholar]
- 11.Simovitch R, Sanders B, Ozbaydar M, et al. Acromioclavicular joint injuries: diagnosis and management. J Am Acad Orthop Surg. 2009;17:207–219. doi: 10.5435/00124635-200904000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Murena L, Canton G, Vulcano E, et al. Scapular dyskinesis and SICK scapula syndrome following surgical treatment of type III acute acromioclavicular dislocations. Knee Surg Sports Traumatol Arthrosc. 2013;21:1146–1150. doi: 10.1007/s00167-012-1959-9. [DOI] [PubMed] [Google Scholar]
- 13.Rios CG, Mazzocca AD. Acromioclavicular joint problems in athletes and new methods of management. Clin Sports Med. 2008;27:763–788. doi: 10.1016/j.csm.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 14.Fremerey RW, Lobenhoffer P, Ramacker K, et al. Acute acromioclavicular joint dislocation – operative or conservative therapy? Unfallchirurg. 2001;104:294–299. doi: 10.1007/s001130050730. [DOI] [PubMed] [Google Scholar]
- 15.Glick JM, Milburn LJ, Haggerty JF, et al. Dislocated acromioclavicular joint: follow- up study of 35 unreduced acromioclavicular dislocations. Am J Sports Med. 1977;5:264–270. doi: 10.1177/036354657700500614. [DOI] [PubMed] [Google Scholar]
- 16.Gstettner C, Tauber M, Hitzl W, et al. Rockwood type III acromioclavicular dislocation: surgical versus conservative treatment. J Shoulder Elbow Surg. 2008;17:220–225. doi: 10.1016/j.jse.2007.07.017. [DOI] [PubMed] [Google Scholar]
- 17.Rawes ML, Dias JJ. Long-term results of conservative treatment for acromioclavicular dislocation. J Bone Joint Surg Br. 1996;78:410–412. [PubMed] [Google Scholar]
- 18.Debski RE, Parsons IM, Woo SL, et al. Effect of capsular injury on acromioclavicular joint mechanics. J Bone Joint Surg Am. 2001;83:1344–1351. doi: 10.2106/00004623-200109000-00009. [DOI] [PubMed] [Google Scholar]
- 19.Lee KW, Debski RE, Chen CH, et al. Functional evaluation of the ligaments at the acromioclavicular joint during anteroposterior and superoinferior translation. Am J Sports Med. 1997;25:858–862. doi: 10.1177/036354659702500622. [DOI] [PubMed] [Google Scholar]
- 20.Mazzocca AD, Spang JT, Rodriguez RR, et al. Biomechanical and radiographic analysis of partial coracoclavicular ligament injuries. Am J Sports Med. 2008;36:1397–1402. doi: 10.1177/0363546508315200. [DOI] [PubMed] [Google Scholar]
- 21.Beitzel K, Cote MP, Apostolakos J, et al. Current concepts in the treatment of acromioclavicular joint dislocations. Arthroscopy. 2013;29:387–397. doi: 10.1016/j.arthro.2012.11.023. [DOI] [PubMed] [Google Scholar]
- 22.Tauber M. Management of acute acromioclavicular joint dislocations: current concepts. Arch Orthop Trauma Surg. 2013;133:985–995. doi: 10.1007/s00402-013-1748-z. [DOI] [PubMed] [Google Scholar]
- 23.Yoo YS, Tsai AG, Ranawat AS, et al. A biomechanical analysis of the native coracoclavicular ligaments and their influence on a new reconstruction using a coracoid tunnel and free tendon graft. Arthroscopy. 2010;26:1153–1161. doi: 10.1016/j.arthro.2009.12.031. [DOI] [PubMed] [Google Scholar]
- 24.Klimkiewicz JJ, Williams GR, Sher JS, et al. The acromioclavicular capsule as a restraint to posterior translation of the clavicle: a biomechanical analysis. J Shoulder Elbow Surg. 1999;8:119–124. doi: 10.1016/s1058-2746(99)90003-4. [DOI] [PubMed] [Google Scholar]
- 25.Scheibel M, Dröschel S, Gerhardt C, et al. Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations. Am J Sports Med. 2011;39:1507–1516. doi: 10.1177/0363546511399379. [DOI] [PubMed] [Google Scholar]
- 26.Padua R, Padua L, Ceccarelli E, et al. Italian version of the Disability of the Arm, Shoulder and Hand (DASH) questionnaire. Cross-cultural adaptation and validation. J Hand Surg Br. 2003;28:179–186. doi: 10.1016/s0266-7681(02)00303-0. [DOI] [PubMed] [Google Scholar]
- 27.Yian EH, Ramappa AJ, Arneberg O, et al. The Constant score in normal shoulders. J Shoulder Elbow Surg. 2005;14:128–133. doi: 10.1016/j.jse.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 28.Cooper E. New method of treating long standing dislocations of the scapuloclavicular articulation. Am J Med Sci. 1861;41:389–392. [Google Scholar]
- 29.Bosworth B. Acromioclavicular separation: new method of repair. Surg Gynecol Obstet. 1941;73:866–871. [Google Scholar]
- 30.Balser D. Eine neue Methode zur operative Behandlung der akromioklavikularen Luxation. Chir Prax. 1976;24:275. [Google Scholar]
- 31.Cadenat F. The treatment of dislocations and fractures of the outer end of the clavicle. Int Clin. 1917;1:145–169. [Google Scholar]
- 32.Weaver JK, Dunn HK. Treatment of acromioclavicular injuries, especially complete acromioclavicular separation. J Bone Joint Surg Am. 1972;54:1187–1194. [PubMed] [Google Scholar]
- 33.Boileau P, Old J, Gastaud O, et al. All-arthroscopic Weaver-Dunn-Chuinard procedure with double-button fixation for chronic acromioclavicular joint dislocation. Arthroscopy. 2010;26:149–160. doi: 10.1016/j.arthro.2009.08.008. [DOI] [PubMed] [Google Scholar]
- 34.Millett PJ, Braun S, Gobezie R, et al. Acromioclavicular joint reconstruction with coracoacromial ligament transfer using the docking technique. BMC Musculoskelet Disord. 2009;10:6. doi: 10.1186/1471-2474-10-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Spencer EE., Jr Treatment of grade III acromioclavicular joint injuries: a systematic review. Clin Orthop Relat Res. 2007;455:38–44. doi: 10.1097/BLO.0b013e318030df83. [DOI] [PubMed] [Google Scholar]
- 36.Mumford E. Acromioclavicular dislocation. J Bone Joint Surg Am. 1941;23:799–802. [Google Scholar]
- 37.Rockwood CAJ, Guy DK, Griffin JL. Treatment of chronic, complete acromioclavicular dislocation. Orthop Trans. 1988;12:735. [Google Scholar]
- 38.Costic RS, Labriola JE, Rodosky MW, et al. Biomechanical rationale for development of anatomical reconstructions of coracoclavicular ligaments after complete acromioclavicular joint dislocations. Am J Sports Med. 2004;32:1929–1936. doi: 10.1177/0363546504264637. [DOI] [PubMed] [Google Scholar]
- 39.Grutter PW, Petersen SA. Anatomical acromioclavicular ligament reconstruction: a biomechanical comparison of reconstructive techniques of the acromioclavicular joint. Am J Sports Med. 2005;33:1723–1728. doi: 10.1177/0363546505275646. [DOI] [PubMed] [Google Scholar]
- 40.Lee SJ, Nicholas SJ, Akizuki KH, et al. Reconstruction of the coracoclavicular ligaments with tendon grafts: a comparative biomechanical study. Am J Sports Med. 2003;31:648–655. doi: 10.1177/03635465030310050301. [DOI] [PubMed] [Google Scholar]
- 41.Mazzocca AD, Santangelo SA, Johnson ST, et al. A biomechanical evaluation of an anatomical coracoclavicular ligament reconstruction. Am J Sports Med. 2006;34:236–246. doi: 10.1177/0363546505281795. [DOI] [PubMed] [Google Scholar]
- 42.Tauber M, Gordon K, Koller H, et al. Semitendinosus tendon graft versus a modified Weaver-Dunn procedure for acromioclavicular joint reconstruction in chronic cases: a prospective comparative study. Am J Sports Med. 2009;37:181–190. doi: 10.1177/0363546508323255. [DOI] [PubMed] [Google Scholar]
- 43.Carofino BC, Mazzocca AD. The anatomic coracoclavicular ligament reconstruction: surgical technique and indications. J Shoulder Elbow Surg. 2010;19:37–46. doi: 10.1016/j.jse.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 44.Schliemann B, Roßlenbroich SB, Schneider KN, et al. Why does minimally invasive coracoclavicular ligament reconstruction using a flip button repair technique fail? An analysis of risk factors and complications. Knee Surg Sports Traumatol Arthrosc. 2013 Oct; doi: 10.1007/s00167-013-2737-z. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 45.Beris A, Lykissas M, Kostas-Agnantis I, et al. Management of acute acromioclavicular joint dislocation with a double-button fixation system. Injury. 2013 Jan; doi: 10.1016/j.injury.2013.01.002. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 46.Motta P, Maderni A, Bruno L, et al. Suture rupture in acromioclavicular joint dislocations treated with flip buttons. Arthroscopy. 2011;27:294–298. doi: 10.1016/j.arthro.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 47.Milewski MD, Tompkins M, Giugale JM, et al. Complications related to anatomic reconstruction of the coracoclavicular ligaments. Am J Sports Med. 2012;40:1628–1634. doi: 10.1177/0363546512445273. [DOI] [PubMed] [Google Scholar]
- 48.Martetschläger F, Horan MP, Warth RJ, et al. Complications after anatomic fixation and reconstruction of the coracoclavicular ligaments. Am J Sports Med. 2013;41:2896–2903. doi: 10.1177/0363546513502459. [DOI] [PubMed] [Google Scholar]
- 49.Beitzel K, Sablan N, Chowaniec DM, et al. Sequential resection of the distal clavicle and its effects on horizontal acromioclavicular joint translation. Am J Sports Med. 2012;40:681–685. doi: 10.1177/0363546511428880. [DOI] [PubMed] [Google Scholar]
- 50.Browne JE, Stanley RF, Tullos HS. Acromioclavicular joint dislocations. Comparative results following operative treatment with and without primary distal clavisectomy. Am J Sports Med. 1977;5:258–263. doi: 10.1177/036354657700500613. [DOI] [PubMed] [Google Scholar]
- 51.Park JP, Arnold JA, Coker TP, et al. Treatment of acromioclavicular separations. A retrospective study. Am J Sports Med. 1980;8:251–256. doi: 10.1177/036354658000800407. [DOI] [PubMed] [Google Scholar]
- 52.Weinstein DM, McCann PD, McIlveen SJ, et al. Surgical treatment of complete acromioclavicular dislocations. Am J Sports Med. 1995;23:324–331. doi: 10.1177/036354659502300313. [DOI] [PubMed] [Google Scholar]