Abstract
A good outcome in total knee arthroplasty depends on many factors: joint alignment, range of motion, patellar tracking and ligament stability. A correct soft tissue balance keeps the joint aligned in flexion and extension, and therefore constitutes the most important factor for durability of the implant. Indeed, incorrect soft tissue balancing is the primary cause of early implant failure necessitating revision surgery. Soft tissue releases, serving to correct imbalances, are performed until the flexion and extension gaps appear symmetrical and balanced. A knee is considered perfectly balanced when the flexion and extension gaps are perfectly rectangular and all the measurements are absolutely equal.
Keywords: balance, ligament, total knee arthroplasty, valgus, varus
Introduction
A good outcome in total knee arthroplasty (TKA) depends on many factors: joint alignment, range of motion, patellar tracking and ligament stability. A correct soft tissue balance keeps the joint aligned in flexion and extension, and therefore constitutes the most important factor for durability of the implant; indeed, incorrect soft tissue balancing is the primary cause of early implant failure necessitating revision surgery.
In the osteoarthritic joint, instability can be symmetrical causing cartilaginous or bony erosion without ligament changes, or asymmetrical. Asymmetrical instability, which is typical of severe osteoarthritis (OA), is characterized by the inevitable occurrence of structural soft tissue changes, serving to compensate for the deformity caused by asymmetrical bone loss. Such joint instability cannot be corrected by bone resections and implant alignment alone (Fig. 1).
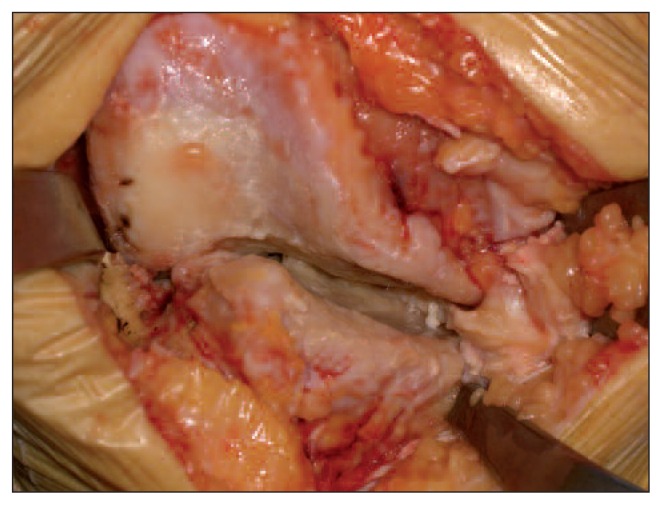
Fig. 1.
Severe varus knee deformity showing both ligament and bony alterations.
In the surgical correction of an asymmetrical joint deformity it can be necessary to perform additional procedures to ensure retention of the stretched ligamentous structures, or, if these are not sufficient, to opt for a constrained type of implant. In this regard, it is necessary to bear in mind the requirements of younger patients, in whom every effort should be made to avoid the use of constrained implants.
Each single patient should be evaluated carefully and treated individually. Accurate and thorough pre-operative planning with full-length standing radiographs of the lower limb in anteroposterior and lateral views, and axial view are indispensable for choosing the prosthesis design and tibial bone resection level (1, 2).
Testing for soft tissue balancing during TKA was introduced by Insall, who used spacer blocks and laminar spreaders intraoperatively to assess the extension and flexion gaps in varus and valgus stress (2).
It is recommended that all osteotomies of the tibia and femur be performed first, followed by excision of all osteophytes. Posterior femoral condylar osteophytes should be excised because they can prevent full extension and influence posterior soft tissue tension (Fig. 2). Before performing soft tissue release for balancing, it is important to remember the following points:
Fig. 2.
Osteophytes influence soft tissue tension and do not allow proper evaluation of balancing during surgery.
The position of the prosthesis components can serve a compensatory function in an extensive soft tissue release because the flexion gap dictates rotation of the femoral component. After soft tissue balancing, the flexion space is balanced by rotating the femoral component to equalize the filling effect of the femoral component in flexion (Fig. 3).
Femoral component malalignment leads to patella maltracking, flexion gap instability and anterior knee pain. In addition, a malrotated femoral component will result in an asymmetrical trapezoidal-shaped flexion gap which will increase polyethylene wear and might decrease the survival of the prosthesis.
Tibial cut performed neutrally in the coronal plane influences the ligament balance. A bone cut performed in a few degrees of valgus is tolerated better than one performed in varus.
In the sagittal plane, the slope can be increased to favor flexion and extension (3, 4).
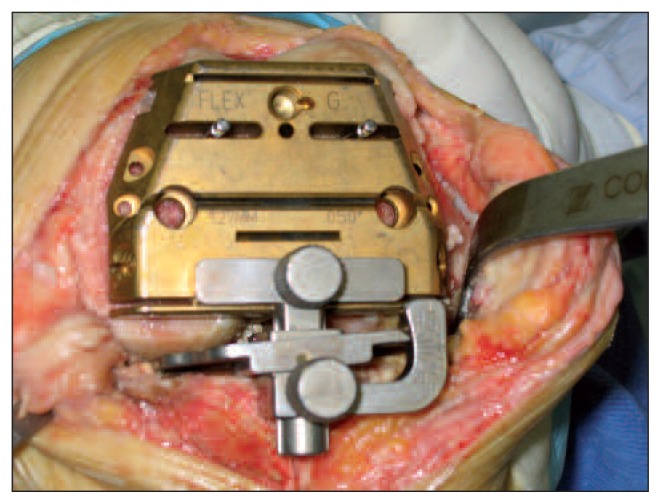
Fig. 3.
Flexion space is balanced by rotating the femoral component to equalize the filling effect of the femoral component in flexion. Proper instruments are needed to reach a symmetrical gap.
Varus deformity
Varus deformity is often combined with medial soft tissue flexion contracture with lateral soft tissue laxity. Medial soft tissue serves a static stabilizing (superficial medial collateral ligament, posterior oblique ligament and posterior capsule) and a dynamic stabilizing (pes anserinus and semimembranosus tendon) function.
The critical structures on the medial side of the knee include the superficial medial collateral ligament (sMCL) fibers on the anterior aspect, and posterior structures such as the posterior oblique ligament (POL) and the semimembranosus (SM) tendon fibers that merge into the posterior capsule.
Release of the anterior structures tends to increase the flexion gap more than the extension gap, whereas release of the more posterior elements tends to affect the extension gap more than the flexion gap. The addition of a posterior cruciate ligament (PCL) release for a posterior stabilized prosthesis increases the flexion gap. The sMCL affects both the flexion and the extension gap; however, release of only the anterior portion affects the flexion gap more than the extension gap.
The POL should be the first structure released when the knee is tight only in extension and not in flexion. Another indication for release of the POL occurs when, after release of the SMCL, the knee remains tight in extension (Fig. 4). If the knee remains tight in full extension after release of the POL, then release of the SM tendon should be considered.
Fig. 4.
Balancing of varus knee after release of both anterior and posterior structures.
Release of the SM tendon is usually only necessary in knees with significant varus coronal deformity or combined varus and flexion contracture deformity. It allows the tibia to be externally rotated and allows easier access to the posteromedial aspect of the tibia.
The pes anserinus tendons should be released only in severe varus knees; their release affects extension more than flexion.
Osteotomy of the medial epicondyle has also been reported to aid in balancing and providing exposure of the varus knee with flexion contracture. Another option for the knee with a severe varus deformity involves resection of the bone along the medial tibial plateau, with downsizing and relative lateralization of the tibial baseplate. The final effect is a relative medialization of the tibial tubercle, which may enhance patellar tracking.
If, after complete release of medial-sided structures, imbalance persists and the medial gap is tight, the surgeon should consider advancing the lateral collateral ligament (LCL) to correct the imbalance. This can be accomplished on the fibular side of the joint by osteotomizing the proximal fibula and advancing it distally to tighten the LCL.
In the cruciate-retaining (CR) prosthesis the tension of the PCL reduces the tibiofemoral gap in flexion, therefore a tight PCL in the CR prosthesis can produce lift-off of the polyethylene insert in flexion.
In the varus knee with a mild flexion contracture it can be sufficient to perform a soft tissue release. The posterior capsule should be released when flexion contracture persists after soft tissue balancing has equalized the medial and lateral gaps.
The capsule must be released subperiosteally from the femur. Extensive release may lead to injuries to the superior geniculate arteries, which are very difficult to reach. When a severe flexion contracture is present it is often necessary to augment the distal femoral cut, bearing in mind that this increases the risk of mid-flexion instability. Indeed, raising the joint line can provoke laxity of the collateral ligaments in mid-flexion, causing instability and patella baja (5, 6).
Valgus deformity
Approximately 10% of patients requiring TKA have a valgus deformity. This deformity may include bone erosion and lateral soft tissue contracture with or without medial laxity.
The lateral structures involved in the process of balancing a valgus knee are the LCL, the popliteus tendon (PT), the posterolateral corner (PLC) and the iliotibial band (ITB).
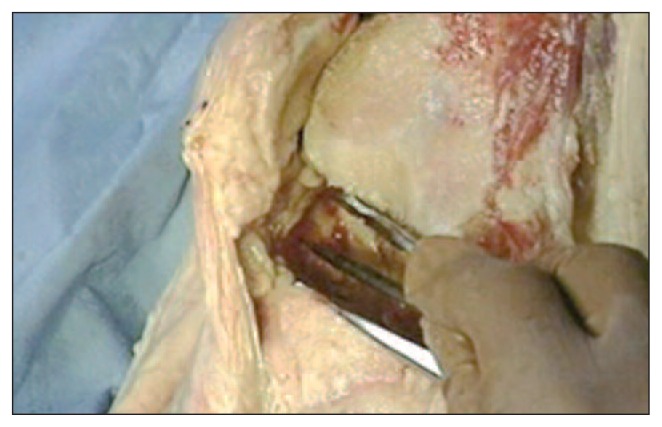
The LCL is a stabilizing structure both in flexion and in extension. It also influences the external rotation of the tibia (Fig. 5).
Fig. 5.
Lateral collateral ligament release using the pie crusting technique in a valgus knee.
The PT plays a crucial stabilizing role and is an important part of the PLC of the knee. It is considered one of the main structures contributing to posterolateral rotatory stability of the knee. It helps to unlock the knee, rotates the tibia internally on the femur, and prevents excessive external rotation of the tibia during knee flexion, among other functions. The PT should be protected because it acts as an important lateral stabilizer in higher degrees of flexion. When using a posterior substitute (PS) prosthesis, this function of the PT is critical, as it is believed to help resist dislocation of the cam-and-post mechanism when the leg is flexed and a varus force is applied.
The PLC stabilizes the knee in flexion and extension. The ITB is perpendicular to the joint line and is therefore an important lateral stabilizer only in extension. Release of the ITB must be performed only when contraction is present in extension.
In order to balance a valgus knee in extension, we first remove peripheral osteophytes and then extend the knee and distract with a laminar spreader; after this we palpate the PCL, the PLC, and the ITB with a finger or with a small Cobb elevator to identify tight structures. At this point, we can release any remnants of the PCL and release the posterolateral capsule intra-articularly using electrocautery at the level of the tibial cut surface from the PCL to the posterior border of the ITB.
If possible, the PT should be preserved, unless it is too tight, in which case we can use the so-called pie-crusting technique. This consists of transverse cutting of the arcuate ligament at the level of the tibial bone cut, and progressive lengthening of the ITB, LCL, and lateral capsule through multiple transverse stab incisions.
The gaps are then measured with a laminar spreader placed in the flexion gap. If the gaps are asymmetrical the femoral jig can be rotated, lowered or raised to create equal gaps because, when using the balanced flexion gap technique, the femoral component is rotated according to ligament tension. Therefore, bone cuts should be used to balance the knee in flexion, and controlled soft-tissue lengthening to balance the knee in extension (7–10).
According to many authors in recent years, there exists, in addition to the “measured resection technique” and the “gap balancing methodology”, a third solution for alignment and soft tissue balancing, namely computer assisted surgery. CAOS (computer assisted orthopaedic surgery) can be used to balance the gaps intraoperatively, according to Insall’s technique.
In conclusion, soft tissue releases, serving to correct imbalances, are performed until the flexion and extension gaps appear symmetrical and balanced. A knee is considered perfectly balanced when the flexion and extension gaps are perfectly rectangular and all the measurements are absolutely equal (7–10).
References
- 1.Sharkey PF, Hozack WJ, Rothman RH, et al. Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;404:7–13. doi: 10.1097/00003086-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Griffin FM, Insall JN, Scuderi GR. Accuracy of soft tissue balancing in total knee arthroplasty. J Arthroplasty. 2000;15:970–973. doi: 10.1054/arth.2000.6503. [DOI] [PubMed] [Google Scholar]
- 3.Kaipel M, Gergely I, Sinz K, et al. Femoral rotation in ligament balanced knee arthroplasty; a prospective clinical study. J Arthroplasty. 2013;28:1103–1106. doi: 10.1016/j.arth.2013.02.031. [DOI] [PubMed] [Google Scholar]
- 4.Mihalko WM, Whiteside LA, Krackow KA. Comparison of ligament-balancing techniques during total knee arthroplasty. J Bone Joint Surg. 2003;85A(Suppl 4):132–135. doi: 10.2106/00004623-200300004-00018. [DOI] [PubMed] [Google Scholar]
- 5.Ahn JH, Back YW. Comparative study of two techniques for ligament balancing in total knee arthroplasty for severe varus knee: medial soft tissue release vs. bony resection of proximal medial tibia. Knee Surg Relat Res. 2013;25:13–18. doi: 10.5792/ksrr.2013.25.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mihalko MW, Saleh KJ, Krackow KA, et al. Soft-tissue balancing during total knee arthroplasty in the varus knee. J Am Acad Orthop Surg. 2009;17:766–774. doi: 10.5435/00124635-200912000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Whiteside LA. Correction of ligament and bone defects in total arthroplasty of the severely valgus knee. Clin Orthop Relat Res. 1993;288:234–245. [PubMed] [Google Scholar]
- 8.Miyasaka KC, Ranawat CS, Mullaji A. 10- to 20-year follow up of total knee arthroplasty for valgus deformities. Clin Orthop Relat Res. 1997;345:29–37. [PubMed] [Google Scholar]
- 9.Ranawat AS, Ranawat CS, Elkus M, Rasquinha VJ, Rossi R, Babhulkar S. Total knee arthroplasty for severe valgus deformity: surgical technique. J Bone Joint Surg Am. 2005;87( Suppl 1):271–284. doi: 10.2106/JBJS.E.00308. [DOI] [PubMed] [Google Scholar]
- 10.Rajgopal A, Dahiya V, Vasdev A, et al. Long-term results of total knee arthroplasty for valgus knees: soft-tissue release technique and implant selection. J Orthop Surg (Hong Kong) 2011;19:60–63. doi: 10.1177/230949901101900114. [DOI] [PubMed] [Google Scholar]