Summary
The debate over the relative merits of substituting or retaining the posterior cruciate ligament in total knee arthroplasty is still ongoing. This article discusses the differences between the two procedures, considering the biomechanics and the surgical techniques involved.
Keywords: Total knee arthroplasty (TKA), cruciate-retaining (CR), posterior-stabilized (PS)
Introduction
Since the 1970s there has been an ongoing debate over the relative merits of substituting or retaining the posterior cruciate ligament (PCL) in total knee arthroplasty (TKA) and no general consensus has yet been reached. Numerous studies have evaluated long-term outcomes after both procedures (1) but, as with patella replacement or the use of cement, surgeons decide on the basis of their own training and experience. Advocates of PCL-retaining TKA claim that it offers a series of advantages: less bone sacrifice, better knee joint kinematics and proprioception, better femoral rollback in flexion, and, finally, better implant stabilization, which practically eliminates the risk of anterior translation of the femur on the tibia. They also argue that posterior-stabilized implants are prone to polyethylene wear due to overloading.
Proponents of cruciate-substituting TKA instead maintain that because the PCL is rarely intact in osteoarthritis, it is vulnerable to early tearing or progressive insufficiency. Often, the PCL needs to be released and the resulting reduced tension on the ligament leaves it exposed to the risk of increasing laxity. The post-cam mechanism in posterior-stabilized implants is claimed to be the optimal substitute for the PCL, as it reduces the risk of posterior instability while providing adequate rollback. Another point in favor of cruciate-substituting TKA is that the procedure is simpler and affords greater joint stability and a greater degree of flexion (2,3).
The two techniques present not only conceptual, but also technical differences, with which the surgeon should be well acquainted (4). The choice of one technique over the other must be based on sound knowledge rather than on dogmatic preconceptions or rigid preferences.
Indications and contraindications
In the approach to a patient scheduled for TKA, the first step is to perform a careful clinical evaluation of the stability of the knee joint. The finding of PCL insufficiency constitutes a contraindication to cruciate-retaining TKA, as does the presence of peripheral instability, especially instability of the posterolateral compartment, because of the stress placed on the PCL. In general, significant instability should prompt the surgeon to opt for cruciate-substituting TKA.
Another important clinical element is the degree of axial deviation: significant valgus or varus malalignment, predictive of difficulty balancing, often necessitates release of the PCL, which, however, impairs its function. An extension deficit may also create problems after cruciate-retaining TKA.
Radiographic studies can provide additional pointers: loss of bone substance or the need for augments are factors that do not favor cruciate-retaining TKA. We believe that cruciate-retaining TKA should not be performed as a revision procedure or in patients who have previously undergone a patellectomy.
Intraoperative assessment
The first consideration during the intraoperative evaluation is the tension and appearance of the PCL: if there are doubts over its quality, posterior-stabilized TKA must be preferred. Another important factor is that cruciate-retaining TKA will reduce the effective joint space in flexion, more than a cruciate-substituting TKA will. Cadaver studies have shown that cruciate-substituting TKA increases the gap in flexion from 1.8 to 4.8 mm (5) (Fig. 1), while it has an only minimal effect on the gap in extension. Since the ultimate objective is to have the same joint space in flexion and extension, the surgeon should consider resecting less distal femur in cruciate-retaining than in cruciate-substituting TKA (Fig. 2). Furthermore, in cruciate-substituting TKA, a medial or lateral release will further open the gap in flexion.
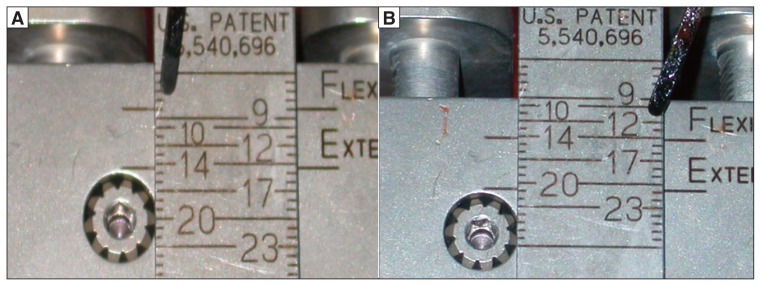
Figure 1.
A: Example of joint space in flexion when the posterior cruciate ligament is retained (8 mm). B: Example of joint space in flexion when the posterior cruciate ligament is substituted (12 mm).
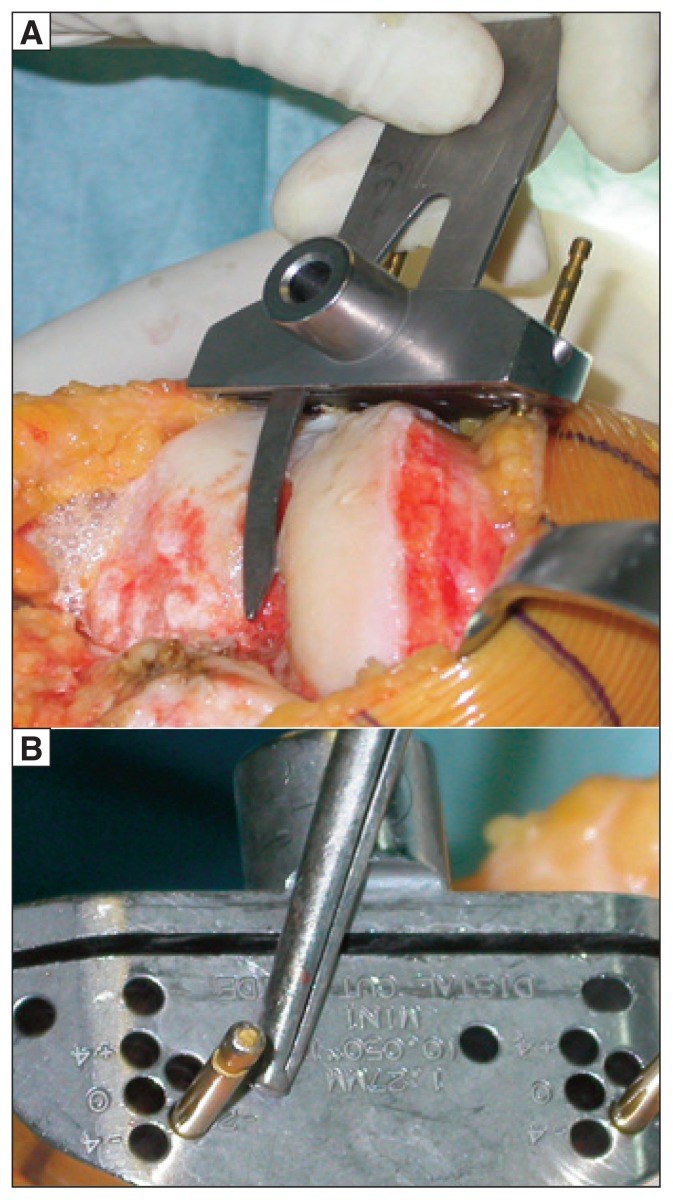
Figure 2.
A: Evaluation of the level of the femoral cut. B: Positioning of the resecting guide for the distal femoral cut in cruciate-retaining implants with a cut 2 mm less than the standard.
Failure to take these considerations into account when performing cruciate-retaining surgery invites the risk, if the distal femoral cut is excessive, of residual instability in extension, which cannot be corrected with a thicker polyethylene insert as this would produce a deficit in flexion. In such circumstances, the only options would be to switch to a posterior-stabilized procedure or to distalize the femur with augments. The increased joint space in flexion that is produced by a cruciate-substituting procedure must be balanced with an additional femoral distal cut. In such cases, it is useful to make sure that the first distal femoral cut is about 2 mm less than the standard cut. After the PCL has been sacrificed and the tibia prepared, balancing is evaluated and, if there is a deficit in extension, this may be corrected with a further distal femoral cut. In this case, simply increasing the poly-ethylene insert thickness to compensate for the space in flexion will produce a deficit in extension. Conversely, a thinner polyethylene insert will provide for better stability in extension, but result in instability in flexion which a post-cam mechanism cannot compensate for. In these cases, it should be remembered that a further tibial cut is not helpful as it influences both flexion and extension.
A final consideration is that because the post-cam mechanism is stressed in extension, hyperextension should be avoided, as it would lead to progressive polyethylene wear or even a rupture of the tibial post (5). In this context, one would also want to avoid an excessive femoral slope, since a curved femoral component predisposes to impingement of the post-cam mechanism.
Correct intramedullary alignment of the femoral component is essential to avoid bending: in this regard, correct preoperative radiological planning is useful to optimize entry of the intramedullary rod.
The tibial cut will differ depending on whether a cruciate-retaining or a cruciate-substituting implant is used. An important element is the degree of the tibial slope which tends to open joint space in flexion. In cruciate-retaining implants, a slight increase in the slope will reduce tension on the PCL and facilitate flexion. However, a large slope in such implants can hinder insertion of the PCL at the tibia, leading to instability in flexion.
In the majority of cruciate-substituting implants, a very small slope is recommended. As already mentioned, with posterior-stabilized implants, we have, by definition, an increase of joint space in flexion; in the presence of an excessive tibial slope this space would be further increased, leading to the risk of significant instability in flexion. Furthermore, a large slope in cruciate-substituting implants would also lead to impingement of the post-cam mechanism.
Ligament balancing can also be influenced by the presence or absence of the PCL. When the PCL is cut, its release significantly increases joint space in extension and flexion, particularly in varus deformities.
Another important factor, given the problems with reestablishing effective joint space in flexion and extension, is the choice of femoral component size. In view of the reduced space in flexion that characterizes cruciate-retaining implants, one should, in the presence of an intermediate femoral size, choose the smallest component to avoid creating too much tension on the PCL, which would require release of the ligament and thus increase the risk of relative instability in flexion. Conversely, in posterior-stabilized implants, where there is greater space in flexion, a larger component size is preferable to compensate for the space created by having substituted the PCL.
In recent years, there has been increasing interest in the concept of posterior femoral offset. It has been demonstrated that creating correct femoral offset provides for good flexion. Published data show that posterior condyle offset (which should always be restored) has a greater effect on flexion after cruciate-retaining TKA (for each 2 mm less offset there is approximately a 12° reduction in flexion) (2,7,8).
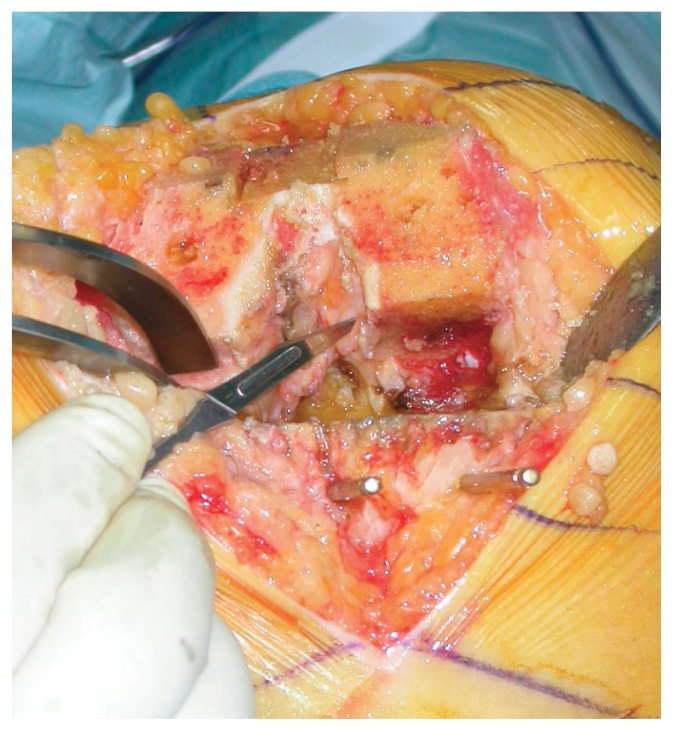
If flexion is difficult due to PCL retraction or excessive tension, the ligament should be released at either its proximal or distal insertion. Personal experience has shown that a useful initial step is to detach the posterior tibial island at the level of the most proximal fibers of the tibial insertion of the PCL (Fig. 3). Often, this step will suffice. Sometimes, however, it is necessary to gradually detach the ligament fibers from the tibia (Fig. 4) or to resect fibers of the ligament at its insertion on the femur (Fig. 5). Extreme care should be taken when releasing the ligament to avoid intra-operative insufficiency or postoperative insufficiency due to progressive weakening. Before deciding whether or not to release the ligament, the bone cuts and correct implant positioning should be carefully evaluated. Often, tension on the PCL is the result of a technical error. If posterior capsule release is necessary, due to residual deficit in extension, this will be more difficult when the PCL is present as it restricts vision and access to the central distal femoral portion (Fig. 6).
Figure 3.
Detachment of the posterior tibial island.
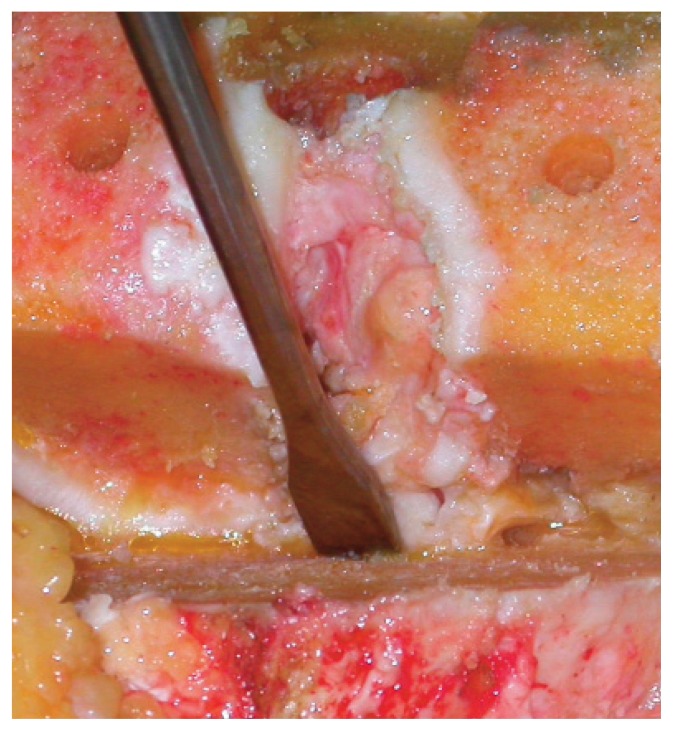
Figure 4.
Distal release of the posterior cruciate ligament.
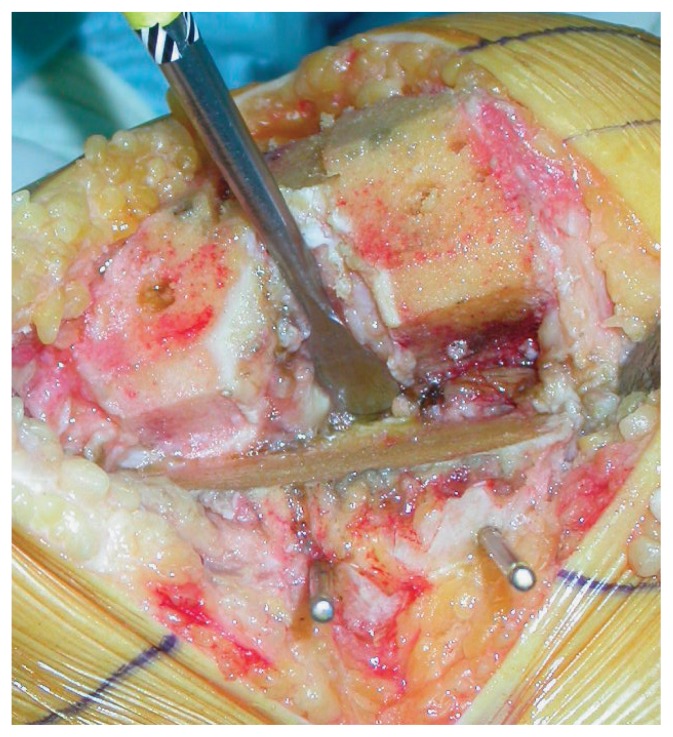
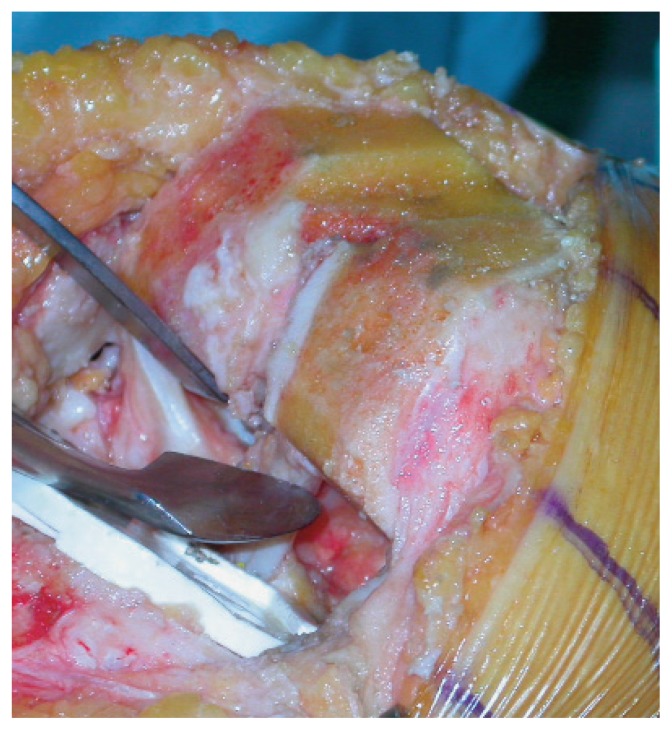
Figure 5.
Proximal release of the posterior cruciate ligament.
Figure 6.
Posterior cruciate ligament hindering visualization and access to the central distal portion of the femur.
Situations can arise in which it is necessary to convert from a cruciate-retaining to a cruciate-substituting implant during the operation. In such circumstances, an additional distal femoral cut will balance the increased joint space in flexion.
Finally, in posterior-stabilized TKAs, it is essential to ensure accurate hemostasis of the ligament vessels, especially when a tourniquet is used, owing to the difficulties with visualizing these vessels after the definitive implant has been positioned.
In conclusion, one should have a clear idea of the technical differences between cruciate-retaining and cruciate-substituting implants. The distal femoral cut and the tibial slope are particularly crucial. Unless they are meticulously executed, residual instability or reduced range of motion will ensue, which can be notoriously difficult to resolve afterwards. One should also remember that excessive stress on the post-cam mechanism will increase the risk of poly-ethylene wear.
References
- 1.Han CW, Yang IH, Lee WS, et al. Evaluation of postoperative range of motion and functional outcomes after cruciate-retaining and posterior-stabilized high-flexion total knee arthroplasty. Yonsei Med J. 2012;53:794–800. doi: 10.3349/ymj.2012.53.4.794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Luo SX, Zhao JM, Su W, et al. Posterior cruciate substituting versus posterior cruciate retaining total knee arthroplasty prostheses: a meta-analysis. Knee. 2012;19:246–252. doi: 10.1016/j.knee.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 3.Yagishita K, Muneta T, Ju YJ, et al. High-flex posterior cruciate-retaining vs posterior cruciate-substituting designs in simultaneous bilateral total knee arthroplasty: a prospective, randomized study. J Arthroplasty. 2012;27:368–374. doi: 10.1016/j.arth.2011.05.008. [DOI] [PubMed] [Google Scholar]
- 4.Emodi GJ, Callaghan JJ, Pedersen DR, et al. Posterior cruciate ligament function following total knee arthroplasty: the effect of joint line elevation. Iowa Orthop J. 1999;19:82–92. [PMC free article] [PubMed] [Google Scholar]
- 5.Sierra RJ, Berry DJ. Surgical technique differences between posterior-substituting and cruciate-retaining total knee arthroplasty. J Arthroplasty. 2008;23( 7 Suppl):20–23. doi: 10.1016/j.arth.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 6.Li G, Papannagari R, Most E, et al. Anterior tibial post impingement in a posterior stabilized total knee arthroplasty. J Orthop Res. 2005;23:536–541. doi: 10.1016/j.orthres.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 7.Arabori M, Matsui N, Kuroda R, et al. Posterior condylar offset and flexion in posterior cruciate-retaining and posterior stabilized TKA. J Orthop Sci. 2008;13:46–50. doi: 10.1007/s00776-007-1191-5. [DOI] [PubMed] [Google Scholar]
- 8.Bellemans J, Banks S, Victor J, et al. Fluoroscopic analysis of the kinematics of deep flexion in total knee arthroplasty. Influence of posterior condylar offset. J Bone Joint Surg. 2002;84B:50–53. doi: 10.1302/0301-620x.84b1.12432. [DOI] [PubMed] [Google Scholar]