Abstract
Generalized joint laxity and shoulder instability are common conditions that exhibit a wide spectrum of different clinical forms and may coexist in the same patient. Generalized joint laxity can be congenital or acquired. It is fundamental to distinguish laxity from instability. Laxity is a physiological condition that may predispose to the development of shoulder instability. A high prevalence of generalized joint laxity has been identified in patients with multidirectional instability of the shoulder. Multidirectional instability is defined as symptomatic instability in two or more directions. The diagnosis and treatment of this condition are still challenging because of complexities in its classification and etiology. These complexities are compounded when multidirectional instability and laxity exist in the same patient. With an improved understanding of the clinical symptoms and physical examination findings, a successful strategy for conservative and/or surgical treatments can be developed. Conservative treatment is the first-line option. If it fails, different surgical options are available. Historically, open capsular shift has been considered the gold standard in the surgical management of these patients. Nowadays, advanced arthroscopic techniques offer several advantages over traditional open approaches and have shown similar outcomes. The correct approach to the management of failed stabilization procedures has not been yet defined.
Keywords: arthroscopy, generalized joint laxity, multidirectional instability, open capsular shift, shoulder
Generalized joint laxity
Generalized joint laxity is characterized by increased length and elasticity of normal joint restraints, resulting in a greater degree of translation of the articular surfaces. This is detectable as an increased range of motion and increased distractibility (1).
This hyperlaxity can be congenital and acquired. Congenital hyperlaxity is usually caused by connective tissue disorders, such as Ehlers-Danlos syndrome, Marphan syndrome, osteogenesis imperfecta, and benign hypermobility syndrome (2, 3). However, it is not necessarily related to a pathological condition. The prevalence of non-pathological hyperlaxity in the general population is between 5 and 15% (4, 5). It becomes less common as individuals age and is slightly more prevalent in females than in males (6, 7). Acquired joint hyperlaxity is commonly observed in athletes (swimmers, gymnasts, pitchers, etc.) (8–10). In this specific population, repetitive microtrauma or repetitive use during training and competitions result in stretching of the normal capsuloligamentous restraints. Male and female athletes are equally affected (1).
Generalized joint laxity does not require any treatment.
Generalized joint laxity and unidirectional instability of the shoulder
Hyperlaxity must be distinguished from instability. Shoulder laxity is the physiological presence of asymptomatic translation of the shoulder joint. There is a wide spectrum of asymptomatic laxity in the anterior, posterior and inferior planes (11). Shoulder instability, on the other hand, is a pathological condition, characterized by the presence of symptoms in conjunction with abnormal laxity, which is indicative of deficient static and dynamic glenohumeral stabilizers (12, 13). Several studies suggest that individuals with generalized joint laxity are at risk of musculoskeletal injuries (14–17). A clear relationship has been demonstrated between generalized joint laxity and both knee (16, 17) and ankle (14, 15) injuries.
The association between generalized joint laxity and anterior shoulder instability continues to be debated. Although there is no gold standard to define hyperlaxity, numerous clinical scoring systems have been proposed. Chahal et al. (18) examined hyperlaxity and shoulder external rotation greater than 85° in 57 patients who sustained a primary traumatic anterior shoulder dislocation and 92 age-matched students without a history of shoulder or knee injuries. The Hospital Del Mar score (19) was used to assess hyperlaxity. It ranges from 0 to 10 and is derived by assigning one point for each of the following criteria:
passive hyperextension of the metacarpophalangeal joint of the little finger of 90° or more;
passive apposition of the thumb to the flexor aspect of the forearm at less than 21 mm;
passive elbow hyperextension of 10° or more;
passive shoulder external rotation of 85° or more;
passive hip abduction of 85° or more;
hyperextension of the first metatarsophalangeal joint beyond 90°;
patellar hypermobility, defined as excessive passive displacement medially and laterally as assessed by three or more quadrants of displacement;
excessive range of passive ankle dorsiflexion and eversion of the foot with the knee flexed to 90°;
passive knee hyperflexion, defined as ‘knee makes contact with the buttock’;
appearance of ecchymoses after hardly noticed, minimal trauma (historical datum).
A score of 4/10 or higher for men and 5/10 or higher for women suggests the presence of generalized joint laxity. The authors (18) showed that generalized joint laxity and increased external rotation are predisposing factors for anterior shoulder dislocation.
Cameron et al. (20), applying the Beighton criteria (21), confirmed the association between hyperlaxity and shoulder instability. The Beighton scale comprises five items:
passive dorsiflexion of the fifth finger beyond 90°;
passive thumb opposition to the forearm;
active elbow hyperextension beyond 10°;
active knee hyperextension beyond 10°;
forward flexion of the trunk with knees fully extended so that the palms of the hands rest flat on the floor.
Each item except for trunk flexion is scored bilaterally and the total score ranges from 0 to 9. The authors showed that patients with a Beighton score of 2 or greater were nearly 2.5 times more likely to have experienced an episode of shoulder instability than patients with lower scores.
The Beighton scale is the most popular scoring system for the clinical assessment of hyperlaxity, but unfortunately its cutoff point remains arbitrary.
A recent study by Ranalletta et al. (22) assessed hyperlaxity in 100 male patients affected by recurrent anterior dislocation and 100 age-matched males without a history of shoulder instability. A Beighton score greater than six was considered indicative of hyperlaxity. No differences were identified in the rate of generalized joint laxity between the two groups.
Shoulder instability occurs when the normal stabilizing mechanisms are disrupted. Patients with anterior traumatic shoulder instability without hyperlaxity can experience recurrent dislocations or subluxations due to a structural injury of the capsulolabral complex or secondary glenoid or humeral head bone loss. By contrast, patients affected by shoulder instability with hyperlaxity are more likely to experience recurrent subluxations than frank dislocations (9, 10, 23). They can develop structural lesions of the capsulolabral complex, but do not usually show any secondary osseous lesions.
A careful physical examination must be performed in order to ascertain the direction of the instability and the possible presence of shoulder hyperlaxity and generalized joint laxity.
The direction of instability can be determined by identifying the provocative position that reproduces instability symptoms. Several tests are commonly used: apprehension test, relocation test, anterior and posterior drawer, anterior and posterior load and shift (24). Inferior shoulder laxity is best evaluated using the sulcus sign test (25) and Gagey test (26). The sulcus sign test is performed with the arm in 0 to 20° of abduction, and both neutral and 30° of external rotation. Humeral head displacement greater than 1 cm from the acromion is considered indicative of a high degree of inferior laxity, but is not considered abnormal unless it reproduces the patient’s symptoms (pain and symptoms of instability). The same test with the arm in 30° of external rotation is specific for deficiency of the rotator interval.
The Gagey test is indicative of inferior laxity if the passive abduction is greater than 105° or if there is marked asymmetrical hyperabduction, i.e. a greater than 20° difference, when compared with the abduction on the contralateral side. Anterior laxity is defined by an excessive external rotation, greater than 85°, with the arm at the subject’s side (27, 28).
As mentioned above, there exist numerous clinical scoring systems for assessing generalized joint laxity. The most common is the Beighton scale. Although there is no formal consensus, a Beighton score of four or more is usually considered indicative of hyperlaxity (1).
Radiographs and computed tomography (CT) are commonly used to evaluate the presence of osseous defects or bony abnormalities; magnetic resonance imaging (MRI) and magnetic resonance arthrography (MRA) offer detailed information about capsulolabral structures, the long head of the biceps, and the rotator cuff. MRA is the most sensitive and specific imaging modality for assessing labral pathologies, capsular tears and volume.
Unidirectional shoulder instability with hyperlaxity always requires surgical treatment. Open and arthroscopic techniques showed comparable results in patients without osseous defects (29). The advantages of arthroscopic treatment include less surgical dissection, easier treatment of concomitant pathologies, and easier access to the posterior capsulolabral complex, if necessary. The aim is to create a stable joint by fixing labral lesions and reducing laxity and excessive volume through retensioning of the static capsulolabral stabilizers. A capsulolabral repair with anchors will be performed on the side of the instability and additional capsular plications on the opposite side may be also performed, depending on the degree of capsular laxity.
A high prevalence of hyperlaxity has been reported in recurrent instability after both open and arthroscopic stabilization procedures. The prevalence of hyperlaxity in failed open procedures, including Bankart repair, capsular shift, Latarjet procedures and bone block augmentation, ranges from 61 to 100% (28, 30–32).
Recent studies also showed a significant association between hyperlaxity and recurrence of instability after arthroscopic procedures (27, 33). Voos et al. (33) evaluated 83 patients who underwent arthroscopic Bankart repair with suture anchors at an average follow-up of 33 months (range, 24–49 months). They showed that patients with hyperlaxity have a 3.3-fold higher risk of recurrent instability than patients without hyperlaxity.
Multidirectional instability
In the 1980s, Neer and Foster coined the term “multidirectional instability” (25), defined as symptomatic involuntary instability of the glenohumeral joint in more than one direction (anterior and/or posterior, and inferior).
The first challenge is to identify and classify patients with multidirectional instability (MDI). Key points to consider in this regard are: the etiology (traumatic, atraumatic, microtraumatic) and the amount of symptomatic translation and volitional control (voluntary and involuntary instability). We classify MDI, as follows:
MDI without hyperlaxity;
MDI with hyperlaxity;
Voluntary instability with hyperlaxity.
Multidirectional instability without hyperlaxity
MDI without hyperlaxity is a very rare condition, usually associated with a traumatic onset. Physical examination will show shoulder instability in anterior and posterior directions. Tests for inferior laxity in the affected shoulder or anterior and inferior laxity in the contralateral shoulder will be negative. CT and MRI will be helpful in the detection of osseous and capsulolabral lesions, respectively. Patients without significant bony abnormalities will be eligible for an arthroscopic treatment. An anterior and posterior capsulolabral repair with anchors will be performed according to the extent of the capsulolabral lesions.
Multidirectional instability with hyperlaxity
The etiology of MDI in patients with hyperlaxity can be atraumatic or due to repetitive microtrauma.
Atraumatic MDI is usually characterized by pain and a sensation of instability. Symptoms develop gradually in these patients: at the beginning, pain during high-demand activities or provocative positions can be the only complaint; subsequently, instability symptoms may progress with subluxations and/or dislocations occurring during activities of daily living.
Repetitive microtrauma is the most common etiology in patients involved in repetitive overhead activities, particularly in sports such as volleyball, swimming and gymnastics. An accumulation of shear forces caused by persistent shoulder subluxation or microtrauma leads to a loss of chondrolabral containment with subsequent development of labral injuries (12, 13).
The prevalence of generalized joint laxity in patients with MDI and shoulder laxity ranges between 40 and 70% (12, 25, 34, 35).
Shoulder stability is guaranteed by the interaction of static and dynamic stabilizers. Bony and capsulolabral ligamentous structures are the primary static restraints of the shoulder. Insufficiency of these structures places higher demands on other shoulder stabilizers.
Dynamic stabilization is provided by the rotator cuff, long head of the biceps and scapula stabilizers.
MDI in patients with hyperlaxity is usually characterized by a patulous and redundant capsule, increased glenohumeral volume and labral injuries. Recent studies also reported abnormal scapular kinematics and an atypical pattern of muscle activity, suggesting that neuromuscular control is a contributing factor in the etiology of multidirectional instability (36–38).
The diagnosis of MDI is primarily clinical. Patients are usually young, between the second and the third decade of life. They may present with a frank history of instability or, more often, with an insidious onset and aspecific activity-related pain exacerbated by positions that can provoke instability such as throwing (anterior instability), carrying heavy loads (inferior instability) or pushing (posterior instability).
Decreased strength and declining athletic performance may also be reported. Inferior instability can be also be associated with numbness and tingling, secondary to traction on the brachial plexus, elicited when carrying heavy objects (39). Correlation of symptoms with the arm position is important to ensure the correct diagnosis. A comprehensive physical examination is one of the most important aspects. Both shoulders should be evaluated, observing any asymmetry, abnormal motion, muscle atrophy and scapular winging. Specific tests assessing the direction of instability and the degree of shoulder laxity must be performed. Moreover, generalized joint laxity must be also evaluated. Failure to address all the components of instability may result in treatment failure. Patients affected by MDI usually show positive instability tests in more than one direction, a positive sulcus sign and a positive Gagey sign. CT and MRI or MRA are helpful to further delineate structural injuries.
In patients without significant bony abnormalities, non-operative treatment is the mainstay of the therapeutic approach. The goal is to rehabilitate deficient structures to restore stability and alleviate symptoms. This form of treatment does not affect the static joint restraints, but it improves tone and proprioceptive control of the dynamic stabilizers. The focus is on strengthening of the rotator cuff and periscapular muscles in order to maximize the concavity-compression mechanism and stabilize the glenoid platform (40). The result is improved humeral head centering and more robust opposition to shear forces. A minimum of six months is a reasonable duration for a first-line treatment. Several studies showed variable results with success rates between 30 and 80% (41–43).
Surgical treatment should be considered after failure of conservative treatment or in the presence of bony abnormalities. It should be individualized in order to address the specific anatomical cause of the instability and reduce the shoulder hyperlaxity to obtain a more normal functional range of motion.
A recent study (44) compared the kinematic parameters and muscle activity of patients with MDI treated by physiotherapy or by surgical treatment and postoperative physiotherapy, before and after treatment. The authors showed that the significant alteration in shoulder kinematics observed in these patients cannot be restored by physiotherapy alone. Surgical treatment and physiotherapy allow bilinear scapulothoracic and glenohumeral rhythms and restoration of the normal relative displacement between the rotation centers of the scapula and humerus. Moreover, the duration of muscular activity was found to be almost normal, after surgery and postoperative rehabilitation.
Historically, open capsular shift has been the standard in the operative treatment of patients with multidirectional instability. A humeral-based (or lateral-based) capsular shift was first described by Neer and Foster in the 1980s (25). Subsequent cadaveric studies showed a significant capsular volume reduction, between 50 and 60% (45–47). Miller et al. (48) compared volume reduction of the glenohumeral joint using three different open capsular shift techniques: the humeral-based T-shaped capsular shift as described by Neer and Foster (25), the glenoid-based (or medial-based) T-shaped capsular shift as described by Altcheck et al. (34), and a vertical capsular imbrication as described by Wirth et al. (49). The humeral-based T-shaped capsular shift resulted in a greater significant reduction than the glenoid-based shift (48.9% vs 36.8%).
In recent years, attention has been focused on arthroscopic techniques. An arthroscopic inferior capsular shift is essentially an arthroscopic modification of the glenoid-based open inferior capsular shift described by Altcheck et al. (34). Cadaveric studies comparing open and arthroscopic capsular shift reported conflicting results. Cohen et al. (50) found that arthroscopic capsular plication using three 1-cm capsulolabral plication sutures resulted in a volume reduction of 22%, whereas humeral-based capsular shift reduced joint volume by nearly 50%. By contrast, Sekiya et al. (51) showed that arthroscopic plication resulted in a mean decrease of 58 ± 12%, whereas open inferior capsular shift resulted in a mean difference of 45 ± 11% (p=0.006). Subsequent studies showed that capsular volume reduction is related to the amount of capsular plication; therefore, the volume reduction increases when the arthroscopic capsulolabral plication is increased from 5 to 10 mm (52, 53). Yamamoto et al. (54) confirmed that the glenoid-based capsular shift decreases joint volume and increases responsiveness of intra-articular pressure to downward loading. Recently, Ponce et al. (55) noted that a 1-cm capsular plication stitch results in a roughly 10% volume reduction of the glenohumeral joint; therefore, five simple capsular plication stitches result in a volume reduction equivalent to an open humeral-based capsular shift.
Only one clinical study (56) reported joint volume reduction following arthroscopic capsular shift. The authors applied the same technique both in cadaveric specimens and in a clinical setting. They reported 37.9% of volume reduction in the cadaveric model and 58.8% of volume reduction in the clinical setting. However, clinical studies reported success rates of 80 to 97% after open capsular shift (25, 34, 35, 57). High success rates, ranging between 68 and 100%, have also been reported after arthroscopic capsular shift (58–60). A recent systematic review (61) comparing open capsular shift versus arthroscopic capsular plications showed that arthroscopic capsular plications yield comparable results to open capsular shift with regard to recurrent instability, return to sport, loss of external rotation, and overall complications.
Arthroscopic treatment is essentially based on the intraoperative findings and includes different techniques: pancapsular plications, capsulolabral repair with suture anchors, and rotator interval closure. Before the procedure is begun, the direction and magnitude of the glenohumeral translation are confirmed by examining the patient under anesthesia. A diagnostic arthroscopy is performed to identify the patulous capsule and possible labral injuries (Fig. 1). MDI may exist with or without labral tears (12), but large circumferential labral tears, termed the “triple labral lesion”, have been described (62). Therefore, a capsulolabral repair with suture anchors can sometimes be needed. Suture anchor repairs use the glenoid as the fixation point. By contrast, capsular plication, a surgical technique that imbricates and decreases the volume of the shoulder capsule with a suture, uses the labrum as the fixation point (63) (Fig. 2). It is generally believed that capsular plications are sufficient if the labrum is completely intact. However, although it has been shown that the labrum is a solid fixation point (64), concerns about shear stress, an unrecognized Kim lesion (Fig. 3) and suture breakage make anchor fixation preferable because it remains the strongest and most predictable repair construct. The sequence of repair is dictated by the primary direction of instability and the extent of the capsulolabral pathology. Considering that each plication decreases capsular volume and the size of the working area, inferior pathology is usually treated first. The final repair construct should produce a glenoid bumper providing sufficient tension along the tissue without capsular redundancy.
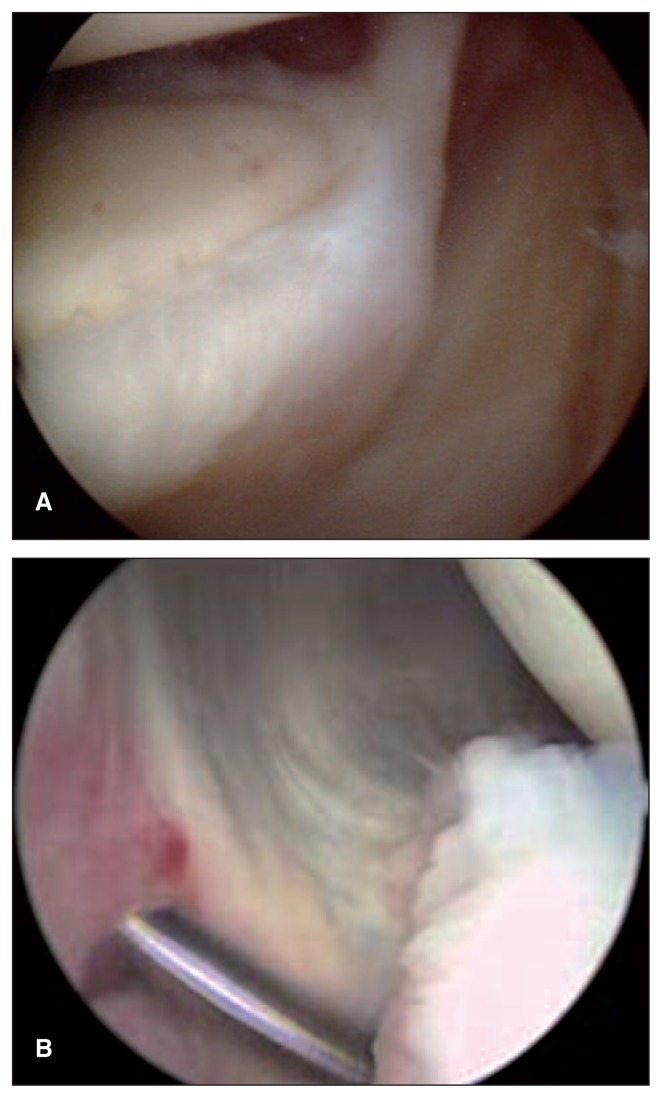
Fig. 1.
MDI of a left shoulder. Diagnostic arthroscopy identifies the patulous capsule at the superior (A) and inferior (B) aspect of the joint.
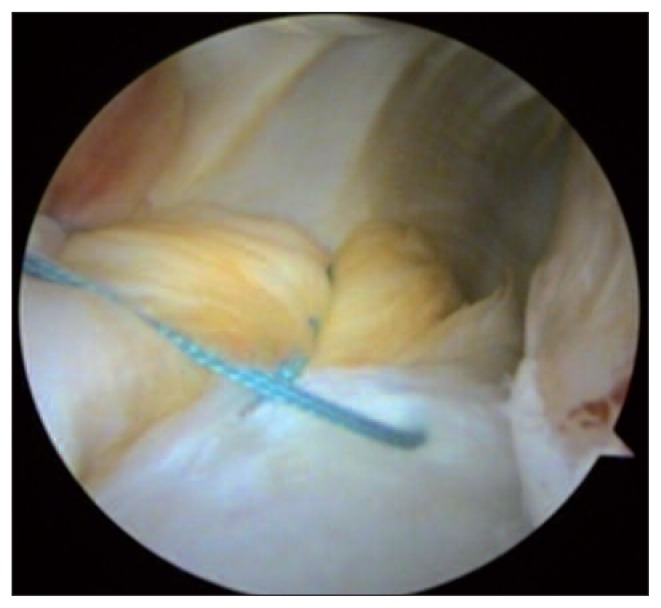
Fig. 2.
Capsular plications are performed to decreases the volume of the shoulder capsule using the labrum as the fixation point of the sutures.
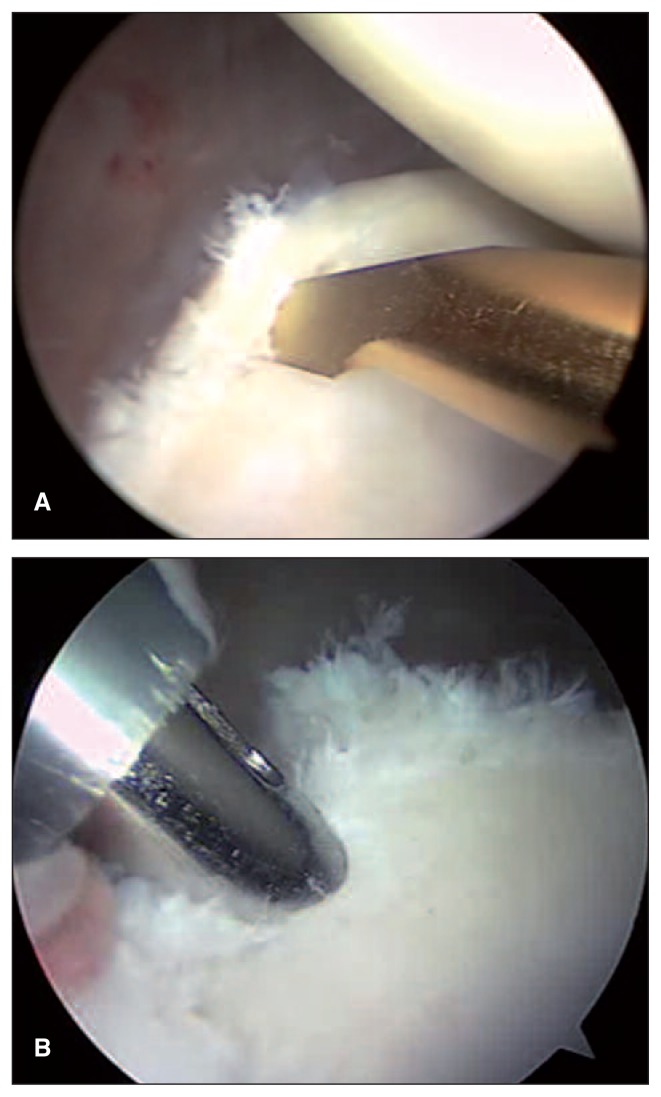
Fig. 3.
Kim Lesion (A) is contraindicated for capsular plications. Anchor fixation (B) is preferable because the repair construct is stronger and more predictable.
The role of the rotator interval in the pathoanatomy of MDI has long been debated. It has been suggested that the capsule and the structures of the rotator interval can limit the postero-inferior translation (65), therefore a rotator interval closure can be an additional procedure performed in the treatment of MDI (Fig. 4). Biomechanical studies reported a reduction of anterior translation and external rotation (66, 67). Only one recent study (68), which compared a superior-inferior closure with an arthroscopic medial-lateral closure, reported a reduction of posterior translation after medial-lateral closure. Clinical studies showed high success rates when rotator interval closure was associated with capsular plications or Bankart repair (69, 70). Although the results of operative treatment show high success rates, treatment of a failed stabilization procedure is still challenging, as there exists no clear algorithm. Two recent reviews suggest simply performing a new comprehensive review of the patient’s history, physical examination and diagnostic imaging (71, 72); therefore, reassessment of the direction of instability, shoulder laxity, generalized joint laxity, sports activities and presence of glenoid and humeral head osseous defects. Arthroscopic techniques could still be appropriate, in patients without osseous defects, to treat residual capsular laxity or labral injuries. However, there is also a role for the open capsular shift. It is usually indicated for patients with specific soft-tissue pathology, including humeral avulsion of the glenohumeral ligaments, midsubstance capsular rupture and capsular deficiency. Moreover, although uncommon in traumatic instability or multidirectional instability, in the presence of significant osseous defects, open reconstructive techniques, such as Latarjet or bone block procedures, must be performed in addition to an open capsular shift.
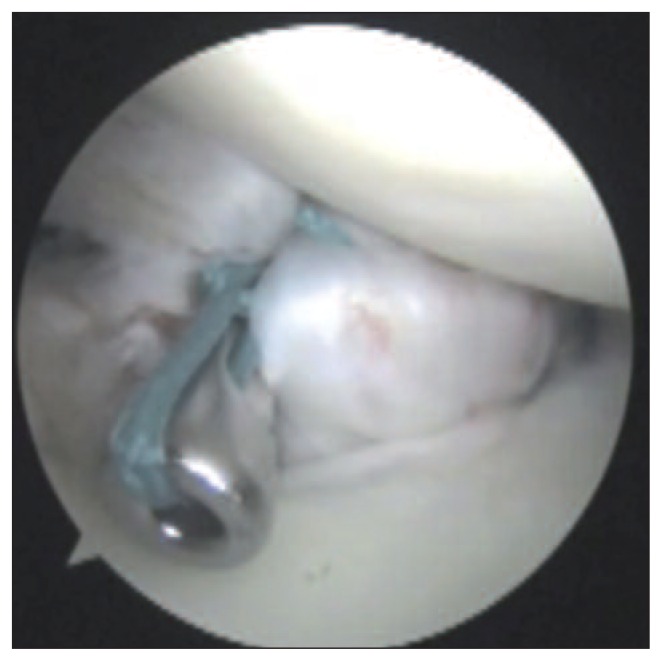
Fig. 4.
Rotator interval closure can be an additional procedure performed in the treatment of MDI.
Voluntary instability with hyperlaxity
Voluntary shoulder instability is characterized by a patient’s ability to subluxate or dislocate her/his shoulder using selective muscle contraction and relaxation. This pathological entity was first described by Rowe in 1973 (73). Most of the patients in that report had ligamentous laxity.
The clinical signs and symptoms of voluntary instability and the treatment algorithm for affected patients have not yet been clearly defined. Conservative treatment, based on strengthening of the rotator cuff and periscapular muscles, is usually the first-line treatment. Surgical treatment is recommended after failure of non-operative treatment. Only two studies reported the outcome of surgical treatment (74, 75). Fuchs et al. (74) reported the results of a posterior capsular shift procedure in a consecutive series of twenty-six shoulders affected by involuntary as well as voluntary posterior instability. Seven shoulders had previously been operated on. At an average follow up of 7.6 years (range, 1.8 to 14.6 years) subjective results were excellent for sixteen shoulders, good for eight, and fair for two. Recently, Greiwe et al. (75) reported good and excellent results after arthroscopic capsular shift in a group of ten patients with voluntary instability.
References
- 1.Johnson SM, Robinson CM. Shoulder instability in patients with joint hyperlaxity. J Bone Joint Surg Am. 2010;92:1545–1557. doi: 10.2106/JBJS.H.00078. [DOI] [PubMed] [Google Scholar]
- 2.Maltz SB, Fantus RJ, Mellett MM, et al. Surgical complications of Ehlers-Danlos syndrome type IV: case report and review of the literature. J Trauma. 2001;51:387–390. doi: 10.1097/00005373-200108000-00029. [DOI] [PubMed] [Google Scholar]
- 3.Zweers MC, Hakim AJ, Grahame R, et al. Joint hypermobility syndromes: the pathophysiologic role of tenascin-X gene defects. Arthritis Rheum. 2004;50:2742–2749. doi: 10.1002/art.20488. [DOI] [PubMed] [Google Scholar]
- 4.Juul-Kristensen B, Røgind H, Jensen DV, et al. Inter-examiner reproducibility of tests and criteria for generalized joint hypermobility and benign joint hypermobility syndrome. Rheumatology (Oxford) 2007;46:1835–1841. doi: 10.1093/rheumatology/kem290. [DOI] [PubMed] [Google Scholar]
- 5.Remvig L, Jensen DV, Ward RC. Epidemiology of general joint hypermobility and basis for the proposed criteria for benign joint hypermobility syndrome: review of the literature. J Rheumatol. 2007;34:804–809. [PubMed] [Google Scholar]
- 6.Didia BC, Dapper DV, Boboye SB. Joint hypermobility syndrome among undergraduate students. East Afr Med J. 2002;79:80–81. doi: 10.4314/eamj.v79i2.8906. [DOI] [PubMed] [Google Scholar]
- 7.Seçkin U, Tur BS, Yilmaz O, et al. The prevalence of joint hypermobility among high school students. Rheumatol Int. 2005;25:260–263. doi: 10.1007/s00296-003-0434-9. [DOI] [PubMed] [Google Scholar]
- 8.Jansson A, Saartok T, Werner S, et al. Evaluation of general joint laxity, shoulder laxity and mobility in competitive swimmers during growth and in normal controls. Scand J Med Sci Sports. 2005;15:169–176. doi: 10.1111/j.1600-0838.2004.00417.x. [DOI] [PubMed] [Google Scholar]
- 9.Smith R, Damodaran AK, Swaminathan S, et al. Hypermobility and sports injuries in junior netball players. Br J Sports Med. 2005;39:628–631. doi: 10.1136/bjsm.2004.015271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caplan J, Julien TP, Michelson J, et al. Multidirectional instability of the shoulder in elite female gymnasts. Am J Orthop (Belle Mead NJ) 2007;36:660–665. [PubMed] [Google Scholar]
- 11.Lintner SA, Levy A, Kenter K, et al. Glenohumeral translation in the asymptomatic athlete’s shoulder and its relationship to other clinically measurable anthropometric variables. Am J Sports Med. 1996;24:716–720. doi: 10.1177/036354659602400603. [DOI] [PubMed] [Google Scholar]
- 12.Provencher MT, Romeo AA. Posterior and multidirectional instability of the shoulder: challenges associated with diagnosis and management. Instr Course Lect. 2008;57:133–152. [PubMed] [Google Scholar]
- 13.Gaskill TR, Taylor DC, Millett PJ. Management of multidirectional instability of the shoulder. J Am Acad Orthop Surg. 2011;19:758–767. doi: 10.5435/00124635-201112000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Decoster LC, Bernier JN, Lindsay RH, et al. Generalized joint hypermobility and its relationship to injury patterns among NCAA lacrosse players. J Athl Train. 1999;34:99–105. [PMC free article] [PubMed] [Google Scholar]
- 15.Beynnon BD, Murphy DF, Alosa DM. Predictive factors for lateral ankle sprains: a literature review. J Athl Train. 2002;37:376–380. [PMC free article] [PubMed] [Google Scholar]
- 16.Ramesh R, Von Arx O, Azzopardi T, et al. The risk of anterior cruciate ligament rupture with generalised joint laxity. J Bone Joint Surg Br. 2005;87:800–803. doi: 10.1302/0301-620X.87B6.15833. [DOI] [PubMed] [Google Scholar]
- 17.Myer GD, Ford KR, Paterno MV, et al. The effects of generalized joint laxity on risk of anterior cruciate ligament injury in young female athletes. Am J Sports Med. 2008;36:1073–1080. doi: 10.1177/0363546507313572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chahal J, Leiter J, McKee MD, et al. Generalized ligamentous laxity as a predisposing factor for primary traumatic anterior shoulder dislocation. J Shoulder Elbow Surg. 2010;19:1238–1242. doi: 10.1016/j.jse.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 19.Bulbena A, Duró JC, Porta M, et al. Clinical assessment of hypermobility of joints: assembling criteria. J Rheumatol. 1992;19:115–122. [PubMed] [Google Scholar]
- 20.Cameron KL, Duffey ML, DeBerardino TM, et al. Association of generalized joint hypermobility with a history of glenohumeral joint instability. J Athl Train. 2010;45:253–258. doi: 10.4085/1062-6050-45.3.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beighton P, Horan F. Orthopaedic aspects of the Ehlers-Danlos syndrome. J Bone Joint Surg Br. 1969;51:444–453. [PubMed] [Google Scholar]
- 22.Ranalletta M, Bongiovanni S, Suarez F, et al. Do patients with traumatic recurrent anterior shoulder instability have generalized joint laxity? Clin Orthop Relat Res. 2012;470:957–960. doi: 10.1007/s11999-011-1992-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.An YH, Friedman RJ. Multidirectional instability of the glenohumeral joint. Orthop Clin North Am. 2000;31:275–285. doi: 10.1016/s0030-5898(05)70147-4. [DOI] [PubMed] [Google Scholar]
- 24.Moen MH, de Vos RJ, Ellenbecker TS, et al. Clinical tests in shoulder examination: how to perform them. Br J Sports Med. 2010;44:370–375. doi: 10.1136/bjsm.2010.071928. [DOI] [PubMed] [Google Scholar]
- 25.Neer CS, 2nd, Foster CR. Inferior capsular shift for involuntary inferior and multidirectional instability of the shoulder. A preliminary report. J Bone Joint Surg Am. 1980;62:897–908. [PubMed] [Google Scholar]
- 26.Gagey OJ, Gagey N. The hyperabduction test. J Bone Joint Surg Br. 2001;83:69–74. doi: 10.1302/0301-620x.83b1.10628. [DOI] [PubMed] [Google Scholar]
- 27.Boileau P, Villalba M, Héry JY, et al. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006;88:1755–1763. doi: 10.2106/JBJS.E.00817. [DOI] [PubMed] [Google Scholar]
- 28.Boileau P, Richou J, Lisai A, et al. The role of arthroscopy in revision of failed open anterior stabilization of the shoulder. Arthroscopy. 2009;25:1075–1084. doi: 10.1016/j.arthro.2009.04.073. [DOI] [PubMed] [Google Scholar]
- 29.Petrera M, Patella V, Patella S, et al. A meta-analysis of open versus arthroscopic Bankart repair using suture anchors. Knee Surg Sports Traumatol Arthrosc. 2010;18:1742–1747. doi: 10.1007/s00167-010-1093-5. [DOI] [PubMed] [Google Scholar]
- 30.Zabinski SJ, Callaway GH, Cohen S, et al. Revision shoulder stabilization: 2- to 10-year results. J Shoulder Elbow Surg. 1999;8:58–65. doi: 10.1016/s1058-2746(99)90057-5. [DOI] [PubMed] [Google Scholar]
- 31.Levine WN, Arroyo JS, Pollock RG, et al. Open revision stabilization surgery for recurrent anterior glenohumeral instability. Am J Sports Med. 2000;28:156–160. doi: 10.1177/03635465000280020401. [DOI] [PubMed] [Google Scholar]
- 32.Meehan RE, Petersen SA. Results and factors affecting outcome of revision surgery for shoulder instability. J Shoulder Elbow Surg. 2005;14:31–37. doi: 10.1016/j.jse.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 33.Voos JE, Livermore RW, Feeley BT, et al. Prospective evaluation of arthroscopic bankart repairs for anterior instability. Am J Sports Med. 2010;38:302–307. doi: 10.1177/0363546509348049. [DOI] [PubMed] [Google Scholar]
- 34.Altchek DW, Warren RF, Skyhar MJ, et al. T-plasty modification of the Bankart procedure for multidirectional instability of the anterior and inferior types. J Bone Joint Surg Am. 1991;73:105–112. [PubMed] [Google Scholar]
- 35.Cooper RA, Brems JJ. The inferior capsular-shift procedure for multidirectional instability of the shoulder. J Bone Joint Surg Am. 1992;74:1516–1521. [PubMed] [Google Scholar]
- 36.Morris AD, Kemp GJ, Frostick SP. Shoulder electromyography in multidirectional instability. J Shoulder Elbow Surg. 2004;13:24–29. doi: 10.1016/j.jse.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 37.Barden JM, Balyk R, Raso VJ, et al. Atypical shoulder muscle activation in multidirectional instability. Clin Neurophysiol. 2005;116:1846–1857. doi: 10.1016/j.clinph.2005.04.019. [DOI] [PubMed] [Google Scholar]
- 38.Ogston JB, Ludewig PM. Differences in 3-dimensional shoulder kinematics between persons with multidirectional instability and asymptomatic controls. Am J Sports Med. 2007;35:1361–1370. doi: 10.1177/0363546507300820. [DOI] [PubMed] [Google Scholar]
- 39.Bahu MJ, Trentacosta N, Vorys GC, et al. Multidirectional instability: evaluation and treatment options. Clin Sports Med. 2008;27:671–689. doi: 10.1016/j.csm.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 40.Schenk TJ, Brems JJ. Multidirectional instability of the shoulder: pathophysiology, diagnosis, and management. J Am Acad Orthop Surg. 1998;6:65–72. doi: 10.5435/00124635-199801000-00007. [DOI] [PubMed] [Google Scholar]
- 41.Burkhead WZ, Jr, Rockwood CA., Jr Treatment of instability of the shoulder with an exercise program. J Bone Joint Surg Am. 1992;74:890–896. [PubMed] [Google Scholar]
- 42.Kiss J, Damrel D, Mackie A, et al. Non-operative treatment of multidirectional shoulder instability. Int Orthop. 2001;24:354–357. doi: 10.1007/s002640000202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Misamore GW, Sallay PI, Didelot W. A longitudinal study of patients with multidirectional instability of the shoulder with seven- to ten-year follow-up. J Shoulder Elbow Surg. 2005;14:466–470. doi: 10.1016/j.jse.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 44.Kiss RM, Illyés A, Kiss J. Physiotherapy vs. capsular shift and physiotherapy in multidirectional shoulder joint instability. J Electromyogr Kinesiol. 2010;20:489–501. doi: 10.1016/j.jelekin.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 45.Lubowitz J, Bartolozzi A, Rubinstein D, et al. How much does inferior capsular shift reduce shoulder volume? Clin Orthop Relat Res. 1996;328:86–90. doi: 10.1097/00003086-199607000-00015. [DOI] [PubMed] [Google Scholar]
- 46.Luke TA, Rovner AD, Karas SG, et al. Volumetric change in the shoulder capsule after open inferior capsular shift versus arthroscopic thermal capsular shrinkage: a cadaveric model. J Shoulder Elbow Surg. 2004;13:146–149. doi: 10.1016/j.jse.2003.11.008. [DOI] [PubMed] [Google Scholar]
- 47.Wiater JM, Vibert BT. Glenohumeral joint volume reduction with progressive release and shifting of the inferior shoulder capsule. J Shoulder Elbow Surg. 2007;16:810–814. doi: 10.1016/j.jse.2007.02.117. [DOI] [PubMed] [Google Scholar]
- 48.Miller MD, Larsen KM, Luke T, et al. Anterior capsular shift volume reduction: an in vitro comparison of 3 techniques. J Shoulder Elbow Surg. 2003;12:350–354. doi: 10.1016/s1058-2746(02)86805-7. [DOI] [PubMed] [Google Scholar]
- 49.Wirth MA, Blatter G, Rockwood CA., Jr The capsular imbrication procedure for recurrent anterior instability of the shoulder. J Bone Joint Surg Am. 1996;78:246–259. doi: 10.2106/00004623-199602000-00012. [DOI] [PubMed] [Google Scholar]
- 50.Cohen SB, Wiley W, Goradia VK, et al. Anterior capsulorrhaphy: an in vitro comparison of volume reduction - arthroscopic plication versus open capsular shift. Arthroscopy. 2005;21:659–664. doi: 10.1016/j.arthro.2005.02.014. [DOI] [PubMed] [Google Scholar]
- 51.Sekiya JK, Willobee JA, Miller MD, et al. Arthroscopic multi-pleated capsular plication compared with open inferior capsular shift for reduction of shoulder volume in a cadaveric model. Arthroscopy. 2007;23:1145–1151. doi: 10.1016/j.arthro.2007.05.019. [DOI] [PubMed] [Google Scholar]
- 52.Schneider DJ, Tibone JE, McGarry MH, et al. Biomechanical evaluation after five and ten millimeter anterior glenohumeral capsulorrhaphy using a novel shoulder model of increased laxity. J Shoulder Elbow Surg. 2005;14:318–323. doi: 10.1016/j.jse.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 53.Flanigan DC, Forsythe T, Orwin J, et al. Volume analysis of arthroscopic capsular shift. Arthroscopy. 2006;22:528–533. doi: 10.1016/j.arthro.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 54.Yamamoto N, Itoi E, Tuoheti Y, et al. The effect of the inferior capsular shift on shoulder intra-articular pressure: a cadaveric study. Am J Sports Med. 2006;34:939–944. doi: 10.1177/0363546505283834. [DOI] [PubMed] [Google Scholar]
- 55.Ponce BA, Rosenzweig SD, Thompson KJ, et al. Sequential volume reduction with capsular plications: relationship between cumulative size of plications and volumetric reduction for multidirectional instability of the shoulder. Am J Sports Med. 2011;39:526–531. doi: 10.1177/0363546510391634. [DOI] [PubMed] [Google Scholar]
- 56.Lubiatowski P, Ogrodowicz P, Wojtaszek M, et al. Arthroscopic capsular shift technique and volume reduction. Eur J Orthop Surg Traumatol. 2012;22:437–441. doi: 10.1007/s00590-011-0865-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lebar RD, Alexander AH. Multidirectional shoulder instability. Clinical results of inferior capsular shift in an active-duty population. Am J Sports Med. 1992;20:193–198. doi: 10.1177/036354659202000217. [DOI] [PubMed] [Google Scholar]
- 58.Duncan R, Savoie FH., 3rd Arthroscopic inferior capsular shift for multidirectional instability of the shoulder: a preliminary report. Arthroscopy. 1993;9:24–27. doi: 10.1016/s0749-8063(05)80340-8. [DOI] [PubMed] [Google Scholar]
- 59.Gartsman GM, Roddey TS, Hammerman SM. Arthroscopic treatment of multidirectional glenohumeral instability: 2- to 5-year follow-up. Arthroscopy. 2001;17:236–243. doi: 10.1053/jars.2001.21529. [DOI] [PubMed] [Google Scholar]
- 60.Fleega BA, El Shewy MT. Arthroscopic inferior capsular shift: long-term follow-up. Am J Sports Med. 2012;40:1126–1132. doi: 10.1177/0363546512438509. [DOI] [PubMed] [Google Scholar]
- 61.Jacobson ME, Riggenbach M, Wooldridge AN, et al. Open capsular shift and arthroscopic capsular plication for treatment of multidirectional instability. Arthroscopy. 2012;28:1010–1017. doi: 10.1016/j.arthro.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 62.Lo IK, Burkhart SS. Triple labral lesions: pathology and surgical repair technique - report of seven cases. Arthroscopy. 2005;21:186–193. doi: 10.1016/j.arthro.2004.09.022. [DOI] [PubMed] [Google Scholar]
- 63.Hewitt M, Getelman MH, Snyder SJ. Arthroscopic management of multidirectional instability: pancapsular plication. Orthop Clin North Am. 2003;34:549–557. doi: 10.1016/s0030-5898(03)00094-4. [DOI] [PubMed] [Google Scholar]
- 64.Provencher MT, Verma N, Obopilwe E, et al. A biomechanical analysis of capsular plication versus anchor repair of the shoulder: can the labrum be used as a suture anchor? Arthroscopy. 2008;24:210–216. doi: 10.1016/j.arthro.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 65.Harryman DT, 2nd, Sidles JA, Harris SL, et al. The role of the rotator interval capsule in passive motion and stability of the shoulder. J Bone Joint Surg Am. 1992;74:53–66. [PubMed] [Google Scholar]
- 66.Yamamoto N, Itoi E, Tuoheti Y, et al. Effect of rotator interval closure on glenohumeral stability and motion: a cadaveric study. J Shoulder Elbow Surg. 2006;15:750–758. doi: 10.1016/j.jse.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 67.Shafer BL, Mihata T, McGarry MH, et al. Effects of capsular plication and rotator interval closure in simulated multidirectional shoulder instability. J Bone Joint Surg Am. 2008;90:136–144. doi: 10.2106/JBJS.F.00841. [DOI] [PubMed] [Google Scholar]
- 68.Farber AJ, El Attrache NS, Tibone JE, et al. Biomechanical analysis comparing a traditional superior-inferior arthroscopic rotator interval closure with a novel medial-lateral technique in a cadaveric multidirectional instability model. Am J Sports Med. 2009;37:1178–1185. doi: 10.1177/0363546508330142. [DOI] [PubMed] [Google Scholar]
- 69.Chechik O, Maman E, Dolkart O, et al. Arthroscopic rotator interval closure in shoulder instability repair: a retrospective study. J Shoulder Elbow Surg. 2010;19:1056–1062. doi: 10.1016/j.jse.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 70.Moon YL, Singh H, Yang H, et al. Arthroscopic rotator interval closure by purse string suture for symptomatic inferior shoulder instability. Orthopedics. 2011;34:269. doi: 10.3928/01477447-20110228-02. [DOI] [PubMed] [Google Scholar]
- 71.Forsythe B, Ghodadra N, Romeo AA, et al. Management of the failed posterior/multidirectional instability patient. Sports Med Arthrosc. 2010;18:149–161. doi: 10.1097/JSA.0b013e3181ec4397. [DOI] [PubMed] [Google Scholar]
- 72.Bois AJ, Wirth MA. Revision open capsular shift for atraumatic and multidirectional instability of the shoulder. J Bone Joint Surg Am. 2012;94:748–756. doi: 10.2106/JBJS.L00090. [DOI] [PubMed] [Google Scholar]
- 73.Rowe CR, Pierce DS, Clark JG. Voluntary dislocation of the shoulder. A preliminary report on a clinical, electromyographic, and psychiatric study of twenty-six patients. J Bone Joint Surg Am. 1973;55:445–460. [PubMed] [Google Scholar]
- 74.Fuchs B, Jost B, Gerber C. Posterior-inferior capsular shift for the treatment of recurrent, voluntary posterior subluxation of the shoulder. J Bone Joint Surg Am. 2000;82:16–25. doi: 10.2106/00004623-200001000-00003. [DOI] [PubMed] [Google Scholar]
- 75.Greiwe RM, Galano G, Grantham J, et al. Arthroscopic stabilization for voluntary shoulder instability. J Pediatr Orthop. 2012;32:781–786. doi: 10.1097/BPO.0b013e31826b6ee1. [DOI] [PubMed] [Google Scholar]