INTRODUCTION
Emphysematous cystitis is a relatively rare complication of lower urinary tract infections (UTIs) characterized by the presence of air within the urinary bladder wall and/or the presence of intraluminal air within the bladder. Common symptoms include dysuria, hematuria, suprapubic pain, and, much less commonly, pneumaturia. Emphysematous cystitis is seen more frequently in elderly women, with underlying diabetes being a leading risk factor. The presence of intramural and intraluminal gas within the urinary bladder on computed tomography (CT) examination is diagnostic for emphysematous cystitis. Accurate and timely diagnosis coupled with appropriate treatment typically leads to a favorable prognosis.1-3
HISTORY
An 81-year-old female patient with medical history of stage II non–small cell lung cancer on chemotherapy, poorly controlled diabetes mellitus (in the setting of recent steroid administration), and chronic UTIs presented to the emergency department (ED) with acute onset of suprapubic pain following several days of episodic dysuria and hematuria. She reported no associated fever, chills, nausea, vomiting, or flank pain. Upon initial presentation to the ED, she was afebrile, and her vital signs were stable. Pertinent physical examination findings were positive for diffuse tenderness to palpation over the suprapubic region.
A complete blood count test revealed an abnormally high white blood cell count of 62,990/μL, confounded by recent Neulasta (pegfilgrastim) administration following chemotherapy. Initial glucose level was 226 mg/dL with hemoglobin A1c of 6.9%. The patient's lactic acid level was normal. Her blood urea nitrogen and creatinine test results were within normal limits. Urinalysis revealed >100 red blood cells and 79 white blood cells per high-powered field with significant bacteria presence and leukocyte esterase, protein, and glucose. Urine cultures were obtained and grew >100,000 colony-forming units per milliliter Escherichia coli. Her blood cultures were negative.
RADIOGRAPHIC APPEARANCE AND TREATMENT
The patient was admitted to the hospital following the diagnosis of UTI with leukocytosis. A Foley catheter was placed, appropriate hyperglycemic control was initiated, and she was started empirically on broad-spectrum antibiotics. Retroperitoneal ultrasound was performed because of the patient's significant suprapubic tenderness and to assess for possible bladder outlet obstruction. Ultrasound evaluation revealed a distended bladder with significant postvoid residual volume. The urinary bladder wall was diffusely echogenic in appearance with associated posterior dirty shadowing (Figure 1), raising concern for possible emphysematous cystitis.4 Contrast-enhanced CT examination of the abdomen and pelvis showed mild diffuse urinary bladder wall thickening and confirmed the presence of both intramural and intraluminal gas that was diagnostic for emphysematous cystitis (Figures 2 and 3).2 The kidneys were unremarkable in appearance with no evidence of perinephric stranding, hydronephrosis, or pyelonephritis.
Figure 1.

Longitudinal ultrasonographic image through the pelvis shows distended urinary bladder with diffuse hyperechoic appearance of the urinary bladder wall (arrows) with posterior shadowing. These findings are consistent with intramural air.
Figure 2.
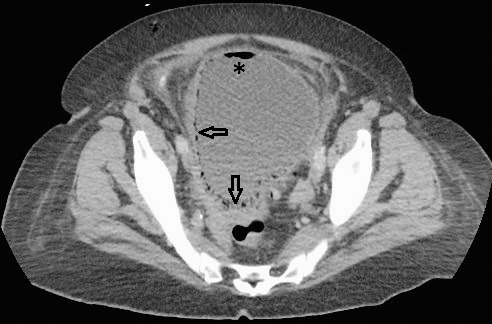
Contrast-enhanced axial computed tomography image through the pelvis reveals both intramural (arrows) and intraluminal (denoted by *) gas within the urinary bladder, confirming the diagnosis of emphysematous cystitis.
Figure 3.

Contrast-enhanced coronal computed tomography image through the abdomen and pelvis reveals air within the urinary bladder wall (arrow) consistent with emphysematous cystitis. Both kidneys (denoted by K) are visualized with no evidence of perinephric stranding, hydronephrosis, or pyelonephritis.
Urine cultures revealed E coli sensitive to piperacillin/tazobactam. During her hospital admission, the patient spiked occasional low-grade fevers for which she was kept on intravenous piperacillin/tazobactam for a total of 14 days. Repeat urine cultures revealed no bacteria growth, and blood cultures remained negative. The Foley catheter was discontinued after 5 days. The patient was afebrile at the time of eventual hospital discharge with complete resolution of her presenting symptoms.
DISCUSSION
Emphysematous cystitis can be seen as a rare complication of lower UTIs. Typical symptoms are similar to those of uncomplicated UTIs, including dysuria, hematuria, urinary frequency, fever, and possible suprapubic pain. Pneumaturia, although more specific, is a much less common presenting symptom. Some patients may be completely asymptomatic at the time of incidental diagnosis.1,2 Although the overall incidence of emphysematous cystitis is unknown, it is seen more commonly in females than males (>2:1).1,3 Diabetes mellitus is the leading risk factor and is present in more than half of reported cases. Other predisposing risk factors include being elderly or debilitated, bladder outlet obstruction, chronic UTIs, neurogenic bladder, chronic indwelling bladder catheters, and immune deficiency.1,2,5 The majority of emphysematous cystitis cases (>60%-70%) are caused by E coli, as in our case.1,2 Other common bacterial pathogens include Enterobacter species, Klebsiella pneumoniae, Staphylococcus aureus, Proteus mirabilis, Pseudomonas aeruginosa, and Streptococcus species. Fungal agents such as Candida species are a less common cause.1,6,7 Laboratory and urinalysis findings in the setting of emphysematous cystitis often mimic those seen in uncomplicated UTI cases, including leukocytosis, microscopic or gross hematuria, leukocyturia, and bacteriuria.
Radiologic imaging is essential for diagnosis because of common overlap of clinical and laboratory findings. Conventional radiography and ultrasound may at times be useful in aiding with diagnosis, although CT examination is the preferred imaging technique for establishing the presence of intramural and/or intraluminal gas, thus confirming the diagnosis of emphysematous cystitis.2 Isolated air within the urinary bladder lumen is not diagnostic on its own, as this finding may be seen in the setting of recent catheterization/instrumentation, surgery, trauma, colovesical fistula, or vesicovaginal fistula.8 Other key radiographic findings include diffuse urinary bladder wall thickening and possible pericystic inflammatory change that are best appreciated on CT.7,8
Clinical presentations of emphysematous cystitis can vary greatly, ranging from patients in severe sepsis to asymptomatic patients who are incidentally diagnosed at the time of unrelated abdominal imaging.1 Treatment typically includes broad-spectrum antibiotic coverage until the organism and antibiotic sensitivity are established from the urine culture. Long-term antibiotic therapy may be needed for 10 days to 6 weeks.3 Infectious disease consultation may be sought for determining the duration of treatment. Other management recommendations include proper glycemic control for diabetic patients. Adequate bladder drainage via catheterization may be needed in the setting of bladder outlet obstruction. Patients should also be closely monitored to ensure clinical improvement with medical management and for potential development of peritoneal signs at which point surgical consultation may be warranted.1,8 Emphysematous cystitis is generally associated with good prognosis if accurately diagnosed and treated in a timely manner. If not properly or timely managed, emphysematous cystitis may have mortality as high as 7%-10%.1,3
REFERENCES
- 1.Thomas AA, Lane BR, Thomas AZ, Remer EM, Campbell SC, Shoskes DA. Emphysematous cystitis: a review of 135 cases. BJU Int. 2007 Jul;100(1):17–20. doi: 10.1111/j.1464-410X.2007.06930.x. [DOI] [PubMed] [Google Scholar]
- 2.Eken A, Alma E. Emphysematous cystitis: the role of CT imaging and appropriate treatment. Can Urol Assoc J. 2013 Nov-Dec;7(11-12):E754–E756. doi: 10.5489/cuaj.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grupper M, Kravtsov A, Potasman I. Emphysematous cystitis: illustrative case report and review of the literature. Medicine (Baltimore) 2007 Jan;86(1):47–53. doi: 10.1097/MD.0b013e3180307c3a. [DOI] [PubMed] [Google Scholar]
- 4.Tublin M, Thurston W, Wilson SR. The kidney and urinary tract. In: Rumack CM, Wilson SR, Charboneau JW, Levine D, editors. Diagnostic Ultrasound. 4th ed. Philadelphia, PA: Elsevier Mosby;; 2011. pp. 317–391. In. eds. [Google Scholar]
- 5.Asada S, Kawasaki T. Images in clinical medicine. Emphysematous cystitis. N Engl J Med. 2003 Jul 17;349(3):258. doi: 10.1056/NEJMicm020703. [DOI] [PubMed] [Google Scholar]
- 6.Quint HJ, Drach GW, Rappaport WD, Hoffmann CJ. Emphysematous cystitis: a review of the spectrum of disease. J Urol. 1992 Jan;147(1):134–137. doi: 10.1016/s0022-5347(17)37160-4. [DOI] [PubMed] [Google Scholar]
- 7.Federle MP. Federle MP, Jeffrey RB, Woodard PJ, Borhani AA. Diagnostic Imaging: Abdomen. 2nd ed. Salt Lake City, UT: Amirsys;; 2010. Cystitis. In. IV.5.8-IV.5.9. [Google Scholar]
- 8.Grayson DE, Abbott RM, Levy AD, Sherman PM. Emphysematous infections of the abdomen and pelvis: a pictorial review. Radiographics. 2002 May-Jun;22(3):543–545. doi: 10.1148/radiographics.22.3.g02ma06543. [DOI] [PubMed] [Google Scholar]


