Key Points
Intraaortic clusters contain pre-HSCs progressively maturing toward an HSC fate.
Abstract
Clusters of cells attached to the endothelium of the main embryonic arteries were first observed a century ago. Present in most vertebrate species, such clusters, or intraaortic hematopoietic clusters (IAHCs), derive from specialized hemogenic endothelial cells and contain the first few hematopoietic stem cells (HSCs) generated during embryonic development. However, some discrepancies remained concerning the spatio-temporal appearance and the numbers of IAHCs and HSCs. Therefore, the exact cell composition and function of IAHCs remain unclear to date. We show here that IAHCs contain pre-HSCs (or HSC precursors) that can mature into HSCs in vivo (as shown by the successful long-term multilineage reconstitution of primary neonates and secondary adult recipients). Such IAHC pre-HSCs could contribute to the HSC pool increase observed at midgestation. The novel insights in pre-HSC to HSC transition represent an important step toward generating transplantable HSCs in vitro that are needed for autologous HSC transplantation therapies.
Introduction
All blood cell production throughout adult life originates from hematopoietic stem cells (HSCs) that are initially produced during embryonic development. HSCs are first detected in the aorta of the aorta-gonad-mesonephros (AGM) region at embryonic day(E)10.5 of mouse development.1 They most likely reside in cell clusters—intra-aortic hematopoietic clusters (IAHCs)—tightly attached to the endothelium. Indeed, both HSCs and IAHC cells express similar markers (eg, c-kit2) and are absent in Runx1−/− embryos.3 IAHCs, first described a century ago,4 are present in most vertebrate species and believed to derive from the underlying endothelium.4 The so-called “hemogenic endothelial origin” of IAHCs and HSCs was shown in chicken5 and mouse embryos.6-9 It was definitively confirmed after we and others observed the endothelial to hematopoietic transition directly in the aorta by time-lapse confocal microscopy, ex vivo in thick mouse embryo slices,10 and in vivo in zebrafish embryos.11,12
Some discrepancies remain when HSCs and IAHCs are compared: (1) IAHCs appear 1 day before HSCs (E9.5 and E10.5, respectively)1,2; (2) the number of IAHC cells largely exceeds the number of HSCs estimated per AGM (∼600 IAHC cells and <0.1 HSC at E10.5; ∼500 IAHC cells and <2 HSCs at E11.51,2,13); and (3) although IAHCs are located in both sides of the aorta, HSCs are restricted to the ventral side.14 To determine the exact cell composition and function of IAHCs, we analyzed the phenotypic evolution and function of IAHC cells before and during HSC detection. Here we show that IAHCs contain pre-HSCs (or HSC precursors) capable of long-term multilineage reconstitution in newborn recipients at a time when HSCs are not yet detected. We demonstrate that IAHC pre-HSCs mature toward an HSC fate by performing secondary transplantations in adults and ex vivo time-lapse live confocal imaging.
Methods
IAHCs were analyzed by scanning electron microscopy or after immunostaining on embryos (sliced or whole). Sorted IAHC cells were tested in vitro in hematopoietic progenitor assays and in vivo after primary long-term transplantation in Rag2−/−γc−/− or wild-type (WT) newborns. Secondary transplantations were performed in adult Rag2−/−γc−/− or WT recipients. Donor chimerism was analyzed by flow cytometry 4 to 5 months upon transplantation.
Results and discussion
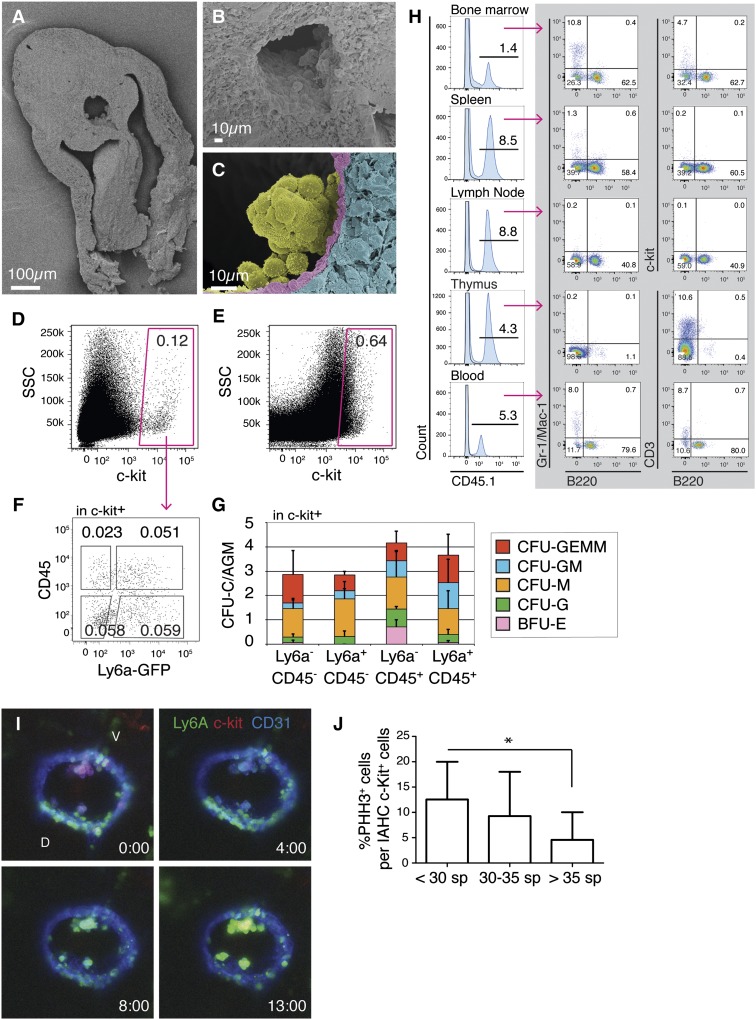
To observe in detail the structure of IAHCs, we imaged by scanning electron microscopy E10 (Figure 1A-C and supplemental Figure 1C-G, available on the Blood Web site) and E11 (supplemental Figure 1A-B) embryo slices. IAHCs, endothelium and subaortic mesenchyme were clearly visible (Figure 1C). In addition to observing single cells (supplemental Figure 1B), we observed spheroid (Figure 1C), stack (supplemental Figure 1C), and “mushroom” (supplemental Figure 1D) IAHC shapes. Most cells were spherical with surface microvilli (supplemental Figure 1E-G). As a control, no IAHCs were visible in Runx1−/− embryo slices (supplemental Figure 1H-I).
Figure 1.
Intraaortic hematopoietic clusters at E10 are phenotypically heterogeneous and contain very few progenitors but contain pre-HSCs able of long-term multilineage hematopoietic reconstitution after transplantation in WT neonates. (A-C) Scanning electron microscopy of E10 (28-34 somite pairs, sp) thick embryo slices. Before tissue fixation, the circulating blood was flushed out of the aorta to ascertain that attached IAHCs and not circulating cells were observed. (A) Whole E10 embryo slice. (B) Close-up view of the aorta where IAHCs are visible inside the aorta. (C) Close-up view of an IAHC with sphere shape in the aorta of E10 embryos. IAHC (yellow), endothelium (pink), and sub-aortic mesenchyme (blue) were artificially colored to show the delimitation between the structures. Top, dorsal side; bottom, ventral side. No morphologic heterogeneity was observed in the cells within single IAHCs or between IAHCs. (D-E) Flow cytometry analysis of AGM cells (E10 embryos) stained with c-kit antibody by intraaortic injection before AGM dissociation (D) or on dissociated AGM cells (E). (F) CD45 and Ly6a-GFP expression within c-kit+ AGM cells from E10 Ly6a-GFP embryos. Percentages of viable cells are indicated inside the gates. The absolute numbers of each population per ee are 216 ± 114 (c-kit+Ly6a-GFP–CD45–), 52 ± 16 (c-kit+Ly6a-GFP+CD45–), 37 ± 17 (c-kit+Ly6a-GFP–CD45+), and 49 ± 23 (c-kit+Ly6a-GFP+CD45+) (n = 4, mean ± standard deviation [SD]). (G) CFU-C assays for the 4 IAHC cell populations isolated from E10 AGMs (28-34 somite pairs) and sorted based on (F) (n = 3). Bars represent the mean ± SD. The number of CFU-C is indicated per flushed AGM. (H) Analysis of a WT neonate recipient (CD45.2) transplanted with 50 IAHC c-kit+ cells from mid-E10 (33-38 sp) AGM (CD45.1) up to 4 months posttransplantation. FACS analysis shows donor-cell contribution (CD45.1) in bone marrow, spleen, lymph nodes, thymus and blood, represented in the histogram on the left panel (CD45.1, blue; control, black line). Lines indicate the percentages of donor contribution in the whole tissue. Multilineage donor contribution (dot plots on gray background) was analyzed in all organs for myeloid (Gr-1/Mac-1) and B cells (B220) in the bone marrow and spleen for HSCs and progenitor cells (c-kit), and in blood and thymus for T cells (CD3). Percentages of each donor population are indicated per quadrant. The analyzed reconstituted mouse is shown in Table 1 (#). (I) Time-lapse series pictures from supplemental Movie 2 (Example 1) showing the maturation of IAHC cells. All CD31+c-kit+Ly6a-GFP– in IAHCs progressively express Ly6a-GFP during the time-lapse imaging (13 h). V, ventral; D, dorsal; Ly6a-GFP, green; c-kit, red; CD31, blue. (J) Percentages of proliferating (c-kit+PHH3+) cells per IAHC (c-kit+) cells (or mitotic index) in the aorta of early E10 (<30 sp), mid-E10 (30-35 sp), and late E10 (>35 sp) embryos. Bars represent means ± SD. *P < .05. To note, we controlled that the intraaortic staining procedure did not detach IAHCs by performing whole-embryo c-kit staining of flushed compared with nonflushed embryos. We found no significant differences in the number of c-kit+ (IAHC) cells in the aorta or in the shape of IAHCs (data not shown).
The functional characterization of IAHCs has been hindered by the difficulty to isolate IAHC cells to purity. All IAHC cells express c-kit, but contaminating c-kit+ cells are also present in the circulating blood and outside of the aorta.2,15 To circumvent this issue, directly-labeled antibodies against c-kit were injected inside the aorta of nonfixed E10 embryos before AGM dissection/dissociation. Our procedure allows flushing out the blood from the aorta, staining all IAHCs,10,16 and isolating IAHC cells only (Figure 1D). When the AGM is dissociated before staining, contaminating c-kit+ cells will also be stained (Figure 1E). Therefore, c-kit intraaortic staining allows IAHCs isolation to purity.
c-kit+ IAHC cells express several endothelial and hematopoietic surface markers (supplemental Figure 2A-D [E10] and 2E-H [E11]). Ly6a-GFP and CD45 were clearly differentially expressed in IAHCs.2,10,16,17 It revealed 4 phenotypically distinct populations (c-kit+Ly6a-GFP–CD45–, c-kit+Ly6a-GFP+CD45–, c-kit+Ly6a-GFP–CD45+, and c-kit+Ly6a-GFP+CD45+), as shown by flow cytometry or confocal microscopy at E10 (Figure 1F, supplemental Figure 3, and supplemental Movie 1) and E11 (supplemental Figure 4A).
To test whether IAHCs contain committed hematopoietic progenitors and whether these progenitors might be restricted to a particular phenotype, IAHC cells were tested in vitro in 3 different clonogenic assays for the presence of erythroid/myeloid progenitors, pre–B-lymphoid progenitors, or megakaryocyte progenitors (colony-forming unit [CFU-Mk]). We found that IAHCs contained very few erythroid/myeloid progenitors (13 ± 3 erythroid/myeloid progenitors/E10 AGM, n = 3, Figure 1G; 19 ± 4 erythroid/myeloid progenitors/E11 AGM, n = 3, supplemental Figure 4B), very few CFU-Mk (9 ± 2 CFU-Mk/E10 AGM, n = 2), and no pre–B progenitors (neither in E10 c-kit+ yolk sac sorted cells, data not shown). As a positive control, adult bone marrow cells produced pre–B progenitors in our culture system (data not shown). Of note, B progenitors were previously reported in the AGM, but only after a culture step on stromal cell lines.18 The number and types of myeloid progenitors were similar in the 4 sorted IAHC cell populations, indicating that a particular phenotype does not correlate with a specific type of progenitor at E10. Interestingly, most erythroid/myeloid progenitors at E10 and E11 were not present in IAHCs but in the AGM circulating blood (enriched in the c-kit+Ly6a-GFP–CD45+ fraction) (supplemental Figure 4C-D and 4E-F, respectively), most likely coming from the yolk sac.19 Altogether, our data show that HSCs and committed progenitors do not account for the high IAHC cell number.
We then tested whether IAHCs contained pre-HSCs (HSC precursors). Pre-HSCs were previously reported in precultured E8 para-aortic splanchnopleura (P-Sp) (prospective AGM area),20 E9.0 yolk sac, and P-Sp.21,22 These cells, unable to reconstitute adult, irradiated WT recipients, could reconstitute more permissive recipients (eg, busulfan-conditioned WT neonates, immunodeficient adult). Secondary transplantations performed in WT adult recipients also confirmed the self-renewal potential of the pre-HSCs.21 Pre-HSCs were also identified after an in vitro AGM-dissociated/reaggregated culture.23,24 We performed transplantations of c-kit+ IAHC cells isolated from early E10 (before HSC detection) and mid-E10 (beginning of HSC detection) AGMs into the liver of Rag2−/−γc−/− or WT neonates (Table 1). Early E10 IAHC cells reconstituted at long-term both Rag2−/−γc−/− and WT neonate recipients after the minimum injection of 100 and 200 cells, respectively. Mid-E10 IAHC cells reconstituted both types of recipients with as few as 50 cells. All reconstitutions were multilineage with donor contribution in myeloid, T-, and B-lymphoid lineages (Figure 1H and supplemental Figure 5). Thus, IAHCs contain pre-HSCs, and their frequency increases between early and mid-E10. Based on the number of c-kit+ cells (∼200 and 600 c-kit+ cells/aorta at early E10 and mid-E10, respectively)2 and our neonate transplantation data (all recipients reconstituted when injected with 100 and 50 c-kit+ cells from early E10 and mid-E10 embryos, respectively), we estimate that there is an average of 2 pre-HSCs per aorta at early E10. This number increases to 12 pre-HSCs at mid-E10, which largely exceeds the number of HSCs estimated at this stage (∼0.1 HSC).1,13 All 4 c-kit+ IAHC subpopulations reconstituted Rag2−/−γc−/− neonates (Table 1). Therefore, pre-HSCs in IAHCs are not restricted to a specific phenotype at E10, based on Ly6a-GFP and CD45 expression. Both markers are thus not useful to enrich in pre-HSCs at E10 but are indicative of pre-HSC maturation into an HSC fate (because all HSCs are Ly6a-GFP+CD45+ at E11.5).
Table 1.
Intraaortic hematopoietic clusters contain pre-HSCs
| Cell number | Neonate recipients§ | |||
|---|---|---|---|---|
| Embryo stage | Sorted cells | injected/recipient | Rag2−/−γc−/− | WT |
| Early E10 (25-32 sp) | c-kit+* | 10 | 0/1 | 0/9 |
| 50 | — | 0/4 | ||
| 100 | 2/2 | 0/2 | ||
| 150 | — | — | ||
| 200 | — | 3‖/5 | ||
| 750 | 1¶/1 | — | ||
| 1350 | 1/1 | — | ||
| c-kit+GFP–CD45–†‡ | 1000-2500 | 3/3 | — | |
| c-kit+GFP+CD45– | 250-550 | 3/4 | — | |
| c-kit+GFP–CD45+ | 150-350 | 1/4 | — | |
| c-kit+GFP+CD45+ | 250-650 | 3/4 | — | |
| Mid-E10 (33-38 sp) | c-kit+* | 10 | 0/1 | 0/6 |
| 50 | 2/2 | 2¶#/12 | ||
| 100 | — | 1/3 | ||
| 150 | 2/2 | — | ||
| 200 | — | 1/1 | ||
—, Not done.
n = 5 independent experiments.
n = 3 independent experiments.
The doses of c-Kit+GFP–CD45–, c-kit+GFP+CD45–, c-kit+GFP–CD45+, and c-kit+GFP+CD45+ cells injected per recipient correspond to 5 to 12, 5 to 11, 4 to 9, and 5 to 13 ee injected per recipient, respectively.
Number of repopulated recipients per injected neonate recipients 4 to 5 months postinjection. Mice were considered repopulated when donor-derived cells (>0.01%) were detected in both the bone marrow and spleen by flow cytometry of the H2kk and Ly6a-GFP donor markers (for Rag2−/−γc−/− recipients) or of the CD45.1 donor marker (for WT recipients).
‖Multilineage reconstitution is shown in supplemental Figure 5.
Primary recipients used for secondary transplantations (see supplemental Table 1).
Multilineage reconstitution is shown in Figure 1H.
Our data show that pre-HSCs not only derive from Ly6a-GFP+ hemogenic endothelial cells25 but also from Ly6a-GFP– hemogenic endothelial cells (not visible by fluorescent live confocal imaging10). Ly6a-GFP is thus very unlikely to be an exclusive marker of hemogenic endothelial cells. To date, only Runx1 seems to mark endothelial cells endowed with the potential of producing blood cells.6 To determine whether IAHC pre-HSC maturation occurs in vivo, secondary transplantations were performed in adult recipients (Rag2−/−γc−/− and/or WT), with bone marrow and spleen cells isolated from primary reconstituted recipients (identified by the paragraph symbol [¶] in Table 1) (supplemental Table 1). In both cases, long-term multilineage reconstitution was observed in the bone marrow, spleen, and peripheral blood of the recipients. Therefore, IAHC pre-HSCs can mature into fully potent HSCs in vivo. Time-lapse confocal microscopy of E10 Ly6a-GFP embryo slices (stained with CD31 and c-kit antibodies before imaging) revealed that, although most IAHC cells were Ly6a-GFP–, they all began to express GFP during the course of imaging (Figure 1I and supplemental Movie 2), indicative of maturation toward an HSC fate (all HSCs are Ly6a-GFP+).17 To test whether cell proliferation occurred in IAHCs, embryo slices were stained for phospho-histone H3.3 (PHH3), CD31, and c-kit (supplemental Figure 6A-B), and proliferating IAHC cells (c-kit+PHH3+) were counted to determine the mitotic index (percentage of IAHC proliferating cells per total IAHC cells; Figure 1J). Few IAHC cells proliferated at the early, mid, and late E10 stages. Thus, the majority of IAHC cells mature toward a putative HSC state with low proliferation.
The hemogenic endothelium does not directly form fully potent HSCs but an intermediate cell population organized in IAHCs. Concomitant to HSC detection (mid-E10), IAHCs already contain an average of 12 pre-HSCs and 22 committed progenitors. The vast majority of IAHC cells is therefore not yet identified but could be very immature pre-HSCs not yet able to reconstitute neonate recipients. We hypothesize that IAHC cells will progressively become pre-HSCs, maturing toward an HSC fate via successive steps initiated inside the aorta and possibly completed in the fetal liver (main HSC reservoir at midgestation) (supplemental Figure 8). We indeed observed 3 phenotypically defined IAHC pre-HSC populations in E12 fetal liver (supplemental Figure 7A-B). To which extent the pre-HSC populations described thus far in different hematopoietic sites are related remains to be determined.
Acknowledgments
The authors thank the experimental animal center (Experimental Dieren Centrum, Erasmus University Medical Center) for mouse care and the Optical Imaging Center of the Erasmus MC for confocal microscope access, Reinier van der Linden and Julien Karrich for help with cell sorting, Elize Haasdijk for initial help with the vibratome, Niels Galjart (Erasmus University Medical Center) for access to the Volocity software, Fanny Sage for her help in editing the movies, and Jacqueline Deschamps (Hubrecht Institute) for careful reading of the manuscript.
This work was supported in part by a European Research Council grant (project number 220-H75001 EU/HSCOrigin-309361); an Innovational Research Incentives Scheme (NWO-VIDI) grant (917-76-345) (C.R., J.-C.B.), and Landsteiner Foundation for Blood Transfusion Research (LSBR 1025) (T. Clapes).
Footnotes
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: C.R. and J.-C.B. conceived ideas and designed the research; J.-C.B. performed most experiments with the help of C.R., T. Clapes, and A.K.; J.O. performed scanning electron microscopy, supervised by M.M.; N.P. performed the initial neonate transplantations, supervised by T. Cupedo; J.-C.B. and C.R. analyzed the data, interpreted the experiments, created the figures, and wrote the paper; and all authors discussed the results and commented on the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Catherine Robin, Hubrecht Institute–KNAW & and University Medical Center Utrecht, Uppsalalaan 8, 3584 CT, Utrecht, The Netherlands; e-mail: c.robin@hubrecht.eu.
References
- 1.Müller AM, Medvinsky A, Strouboulis J, Grosveld F, Dzierzak E. Development of hematopoietic stem cell activity in the mouse embryo. Immunity. 1994;1(4):291–301. doi: 10.1016/1074-7613(94)90081-7. [DOI] [PubMed] [Google Scholar]
- 2.Yokomizo T, Dzierzak E. Three-dimensional cartography of hematopoietic clusters in the vasculature of whole mouse embryos. Development. 2010;137(21):3651–3661. doi: 10.1242/dev.051094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cai Z, de Bruijn M, Ma X, et al. Haploinsufficiency of AML1 affects the temporal and spatial generation of hematopoietic stem cells in the mouse embryo. Immunity. 2000;13(4):423–431. doi: 10.1016/s1074-7613(00)00042-x. [DOI] [PubMed] [Google Scholar]
- 4.Dantschakoff V. Untersuchungen über die Entwickelung von Blut und Bindegewebe bei Vogeln. Das lockere Bindegewebe des Hühnchens im fetalen Leben. Arch f mikr Anat. 1909;73:117–181. [Google Scholar]
- 5.Jaffredo T, Gautier R, Eichmann A, Dieterlen-Lièvre F. Intraaortic hemopoietic cells are derived from endothelial cells during ontogeny. Development. 1998;125(22):4575–4583. doi: 10.1242/dev.125.22.4575. [DOI] [PubMed] [Google Scholar]
- 6.Chen MJ, Yokomizo T, Zeigler BM, Dzierzak E, Speck NA. Runx1 is required for the endothelial to haematopoietic cell transition but not thereafter. Nature. 2009;457(7231):887–891. doi: 10.1038/nature07619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eilken HM, Nishikawa S, Schroeder T. Continuous single-cell imaging of blood generation from haemogenic endothelium. Nature. 2009;457(7231):896–900. doi: 10.1038/nature07760. [DOI] [PubMed] [Google Scholar]
- 8.Lancrin C, Sroczynska P, Stephenson C, Allen T, Kouskoff V, Lacaud G. The haemangioblast generates haematopoietic cells through a haemogenic endothelium stage. Nature. 2009;457(7231):892–895. doi: 10.1038/nature07679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zovein AC, Hofmann JJ, Lynch M, et al. Fate tracing reveals the endothelial origin of hematopoietic stem cells. Cell Stem Cell. 2008;3(6):625–636. doi: 10.1016/j.stem.2008.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boisset JC, van Cappellen W, Andrieu-Soler C, Galjart N, Dzierzak E, Robin C. In vivo imaging of haematopoietic cells emerging from the mouse aortic endothelium. Nature. 2010;464(7285):116–120. doi: 10.1038/nature08764. [DOI] [PubMed] [Google Scholar]
- 11.Bertrand JY, Chi NC, Santoso B, Teng S, Stainier DY, Traver D. Haematopoietic stem cells derive directly from aortic endothelium during development. Nature. 2010;464(7285):108–111. doi: 10.1038/nature08738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kissa K, Herbomel P. Blood stem cells emerge from aortic endothelium by a novel type of cell transition. Nature. 2010;464(7285):112–115. doi: 10.1038/nature08761. [DOI] [PubMed] [Google Scholar]
- 13.Gekas C, Dieterlen-Lièvre F, Orkin SH, Mikkola HK. The placenta is a niche for hematopoietic stem cells. Dev Cell. 2005;8(3):365–375. doi: 10.1016/j.devcel.2004.12.016. [DOI] [PubMed] [Google Scholar]
- 14.Taoudi S, Medvinsky A. Functional identification of the hematopoietic stem cell niche in the ventral domain of the embryonic dorsal aorta. Proc Natl Acad Sci USA. 2007;104(22):9399–9403. doi: 10.1073/pnas.0700984104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zovein AC, Turlo KA, Ponec RM, et al. Vascular remodeling of the vitelline artery initiates extravascular emergence of hematopoietic clusters. Blood. 2010;116(18):3435–3444. doi: 10.1182/blood-2010-04-279497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boisset JC, Andrieu-Soler C, van Cappellen WA, Clapes T, Robin C. Ex vivo time-lapse confocal imaging of the mouse embryo aorta. Nat Protoc. 2011;6(11):1792–1805. doi: 10.1038/nprot.2011.401. [DOI] [PubMed] [Google Scholar]
- 17.de Bruijn MF, Ma X, Robin C, Ottersbach K, Sanchez MJ, Dzierzak E. Hematopoietic stem cells localize to the endothelial cell layer in the midgestation mouse aorta. Immunity. 2002;16(5):673–683. doi: 10.1016/s1074-7613(02)00313-8. [DOI] [PubMed] [Google Scholar]
- 18.Ohmura K, Kawamoto H, Fujimoto S, Ozaki S, Nakao K, Katsura Y. Emergence of T, B, and myeloid lineage-committed as well as multipotent hemopoietic progenitors in the aorta-gonad-mesonephros region of day 10 fetuses of the mouse. J Immunol. 1999;163(9):4788–4795. [PubMed] [Google Scholar]
- 19.Lux CT, Yoshimoto M, McGrath K, Conway SJ, Palis J, Yoder MC. All primitive and definitive hematopoietic progenitor cells emerging before E10 in the mouse embryo are products of the yolk sac. Blood. 2008;111(7):3435–3438. doi: 10.1182/blood-2007-08-107086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cumano A, Ferraz JC, Klaine M, Di Santo JP, Godin I. Intraembryonic, but not yolk sac hematopoietic precursors, isolated before circulation, provide long-term multilineage reconstitution. Immunity. 2001;15(3):477–485. doi: 10.1016/s1074-7613(01)00190-x. [DOI] [PubMed] [Google Scholar]
- 21.Yoder MC, Hiatt K, Dutt P, Mukherjee P, Bodine DM, Orlic D. Characterization of definitive lymphohematopoietic stem cells in the day 9 murine yolk sac. Immunity. 1997;7(3):335–344. doi: 10.1016/s1074-7613(00)80355-6. [DOI] [PubMed] [Google Scholar]
- 22.Yoder MC, Hiatt K, Mukherjee P. In vivo repopulating hematopoietic stem cells are present in the murine yolk sac at day 9.0 postcoitus. Proc Natl Acad Sci USA. 1997;94(13):6776–6780. doi: 10.1073/pnas.94.13.6776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Taoudi S, Gonneau C, Moore K, et al. Extensive hematopoietic stem cell generation in the AGM region via maturation of VE-cadherin+CD45+ pre-definitive HSCs. Cell Stem Cell. 2008;3(1):99–108. doi: 10.1016/j.stem.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 24.Rybtsov S, Sobiesiak M, Taoudi S, et al. Hierarchical organization and early hematopoietic specification of the developing HSC lineage in the AGM region. J Exp Med. 2011;208(6):1305–1315. doi: 10.1084/jem.20102419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen MJ, Li Y, De Obaldia ME, et al. Erythroid/myeloid progenitors and hematopoietic stem cells originate from distinct populations of endothelial cells. Cell Stem Cell. 2011;9(6):541–552. doi: 10.1016/j.stem.2011.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]