Abstract
Background.
Previous studies indicated that a single session of repeated-slip exposure can reduce over 40% of laboratory-induced falls among older adults. The purpose of this study was to determine to what degree such perturbation training translated to the reduction of older adults’ annual falls risk in their everyday living.
Methods.
Two hundred and twelve community-dwelling older adults (≥65 years old) were randomly assigned to either the training group (N = 109), who then were exposed to 24 unannounced repeated slips, or the control group (N = 103), who merely experienced one slip during the same walking in the same protective laboratory environment. We recorded their falls in the preceding year (through self-reported history) and during the next 12 months (through falls diary and monitored with phone calls).
Results.
With this single session of repeated-slip exposure, training cut older adults’ annual risk of falls by 50% (from 34% to 15%, p < .05). Those who experienced merely a single slip were 2.3 times more likely to fall during the same 12-month follow-up period (p < .05) than those who experienced the 24 repeated slips. Such training effect was especially prominent among those who had history of falls.
Conclusion.
A single session of repeated-slip exposure could improve community-dwelling older adults’ resilience to postural disturbances and, hence, significantly reduce their annual risk of falls.
Key Words: Postural disturbance, Learning-from-falling, Retention, Generalization, Inoculation.
Falls are a common and serious problem in older people. The cumulative effect of falls on older adults and on our health care system is enormous; the results are debilitating injuries, loss of independence, and transfer to an institution or even death (1,2). Perturbation-related falls from trips or slips are responsible for about 60% of outdoor falls among community-dwelling adults aged 70 or older (3). Even the healthiest older adults are not immune to idiopathic falls (with unknown cause) that can have devastating health consequences (4). It is therefore difficult, yet imperative, to develop and validate prophylactic approaches that can reduce the likelihood of falls among community-dwelling older adults.
Perturbation training is emerging as a viable option to reduce older adults’ risk of falls (5–7). This approach is novel because it focuses on improving a person’s resilience in response to externally induced perturbations for fall reduction rather than relying on performance-based exercises or other alternatives to improve one’s physical conditioning and control of balance (8–11). A person can modify, through training, the response to a postural perturbation and improve his or her control of stability between the center of mass and base of support (12,13). Such trial-and-error practice allows the central nervous system to make adaptive improvements in proactive and reactive control of stability to resist falls (5).
Adaptation to repeated-slip exposure experienced during perturbation training can occur rapidly—often in a single training session—as a person learns to shift his or her reliance on feedback-driven response for error correction to both incorporate proactive (feed-forward) control as well as improve reactive control of center-of-mass stability (5,14). Effects from a single session of repeated-slip exposure can be retained for many months when the participants were trained and retested in identical laboratory setting (5). Further, there is evidence that these effects can be generalized across different tasks or environments (15,16). Although these findings are promising, it is unknown whether such training effects can in fact translate into reducing older adults’ risk of falls in their everyday living.
This study was to determine to what degree a novel form of motor training, perturbation training provided in the laboratory, in fact translated to the reduction of community-dwelling older adults’ annual falls risk in their daily living. Based on the findings of perturbation-induced rapid adaptation (17), its carryover (15,16,18), and long-term retention (14,19) from previous laboratory studies, we hypothesized that such adaptation could indeed significantly reduce older adults’ annual risk of falls in daily living in comparison to their own history as well as to those of a randomly assigned control group, who received only a single slip (mimicking an occasional event) in the same initial session with an identical protective laboratory settings.
Methods
Study Design
We designed a randomized controlled trial to compare effects from systematic perturbation training (repeated slips) with those from merely an occasional (single) slip. Based on this design, all participants were randomly assigned to receive either 24 repeated slips (training group) or only a single slip (control group) in an identical protective laboratory settings. Their history of falls in the preceding 12 months and prospective falls in the 12 months following this initial session were compared to test the hypothesized training-induced reduction in falls.
Participants’ Recruitment
The recruitment was conducted within a 50-mile radius from the laboratory in the city and the neighboring suburbs of the Greater Chicago Area. These volunteers (paid) came from different senior centers, community exercise centers (eg, YMCA), independent senior living facilities, the Aging Research Registry of the Buehler Center on Aging at Northwestern University, or from affiliates of the Department on Aging, City of Chicago. All participants (≥65 years) had given written informed consent in this study approved by Institutional Review Board in the University of Illinois at Chicago.
All consented participants had no prior experience of any perturbation training. They completed a questionnaire for information on any neurological, musculoskeletal, and cardiopulmonary conditions. They were required to pass a cognition and memory test (>25 on the Folstein Mini Mental Status Exam) (20), a calcaneal ultrasound screening (T score > −1.5) (21), and a mobility test (Timed Up and Go score < 13.5 seconds) (22) and were presumably healthy.
Outcome Measure and Other Potential Confounding Variables
Slips during walking were induced through the electromechanical unlocking of a pair of side-by-side low-friction, movable platforms embedded in a 7-m walkway (Figure 1a). During nonslip trials, the platforms were firmly locked in place. In a slip trial, they were released only after a foot contact was detected by force plates (AMTI, Newton, MA) located beneath, and they would then be free to slide forward (for up to 0.9 m) (23). A full-body harness and shock-absorbing suspension ropes, connected through a load cell to an overhead trolley on a track over the walkway, enabled participants to walk freely while protecting them against any harmful body impact with the floor surface (Figure 1a). A fall was defined by the harness support when it exceeded 30% of this person’s body weight (Figure 2a) (24). Participants’ other demographic characteristics and potential confounding factors, including age, gender, weight, height, Berg Balance scale, and Timed Up and Go score, were also recorded.
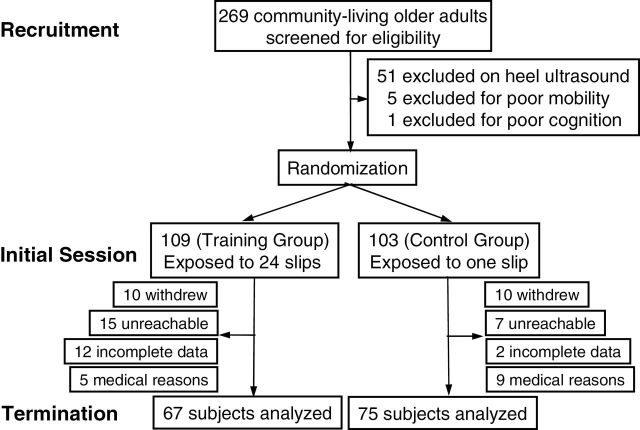
Figure 1.
(a) Schematics of the experimental setup used to induce an unannounced slip in the person traversing the walkway. A slip is induced by releasing two low-friction movable platforms embedded in the middle of this 7-m walkway. Each of the two moveable platforms is mounted to the walkway base frame with four low-friction linear bearings. The base frame is bolted to two force plates (not shown) that are used to measure ground reaction force; each platform is unlocked electronically after the force plates detect the landing of the corresponding foot. All participants wore a safety harness adjusted to prevent any part of the body (other than the feet) to come in contact with the ground. (b) The protocol of the initial session for (A) the training group and (B) the control group. Participants were never told the forthcoming trial condition; rather, they were only informed that a slip “may or may not occur.” To make the timing of the novel slip trial difficult to anticipate, the first 10 trials for everyone was unperturbed (regular) trials in which the low-friction platforms were firmly locked in place. The training group then experienced a total of 24 slips delivered in a block-and-mixed fashion. Two blocks of eight slip trials are shown in gray, intervening two blocks of three nonslip (NS) trials in white, and a final block of mixed eight slip and six nonslip trials in vertical lines. The control group only experienced the novel (single) slip.
Figure 2.

Video sequences show three possible slip outcomes: (a) a participant experienced a fall, the same participant recovered successfully in the subsequent slip trials, (b) with a skate-over strategy, and (c) with a walkover strategy (25). Three frames in a1–a3, b1–b3, and c1–c3 show the instants of foot touchdown that triggered the onset of the slip, postslip liftoff, and touchdown of trailing limb. The triangle on each frame marks the location of the heel at the onset of the slip.
Initial Session
The participants were instructed to walk with their preferred speed and manner. They were informed that a slip “may or may not” occur on any trial and that, if slipped, they should try to recover and keep walking forward. A novel slip was induced only after 10 trials of unperturbed walking to make it difficult for anticipation. As a result, participants did not know when, where, and how this novel first slip would occur. After this trial, those in the training group went on to have another 22 slip trials before the final slip (24 in total), arranged in blocks of eight slips, followed by three nonslip trials, and a final block of eight slips mixed with six nonslip trials (Figure 1b-A). Here again, no one was ever informed about the forthcoming trial condition (slip or nonslip). Those in the control group had the same amount of walking trials but did not experience any further slips in this initial session (Figure 1b-B) (14,26).
Falls Monitoring Program
A fall occurring in everyday living was defined when participants had experienced a sudden, unintended change in body position causing them to land on a lower surface, for example, an object, the floor, or the ground. Participants’ self-reported rate of falls experienced in the previous 12 months was recorded at the initial session. Over the next 12 months, falls experienced in their everyday living were recorded in a log (falls diary). An investigator would call each participant at 6-week intervals to retrieve the log. If a (prospective) fall(s) had occurred, this investigator would follow up with a 5- to 10-minute survey using standard questionnaire regarding the frequency, locations, and types of fall and associated injuries and/or treatment received (27).
Statistical Analysis
Preliminary analyses were performed to identify any confounding variables that could emerge from the baseline sample demographics and potential confounding factors and from dropout status by comparing experimental groups with t test for continuous variables and chi-square test for categorical variables. Rate of falls was compared using Fisher exact test between the training and the control groups. Kaplan–Meier survival method was used to compare the length of time (month) till the first fall during the 12-month falls monitoring program between the two experimental groups. For the final analysis, the generalized estimating equations model with a log link function was employed to assess the trajectory of outcome variable (history-to-prospective change in falls) and to determine if such within-group change (the time factor) differs as a result of training (the group factor that inspects between-group—that is, training vs. control—difference and group-by-time interaction).
Generalized estimating equations is a method for analyzing correlated data that can be modeled using specific covariance matrix. We employed the proportional odds method that is based on modeling cumulative logit functions. The correlations among the binary outcome (history and prospective falls) were modeled as exchangeable. Any confounding variables identified in the preliminary analyses were included in the final model. Throughout the article, both on-treatment (including only participants with complete data) and intention-to-treat (including all participants regardless of dropout) analyses were performed. All analyses were performed using SAS 9.3 (Cary, NC) with a significance level of .05.
Results
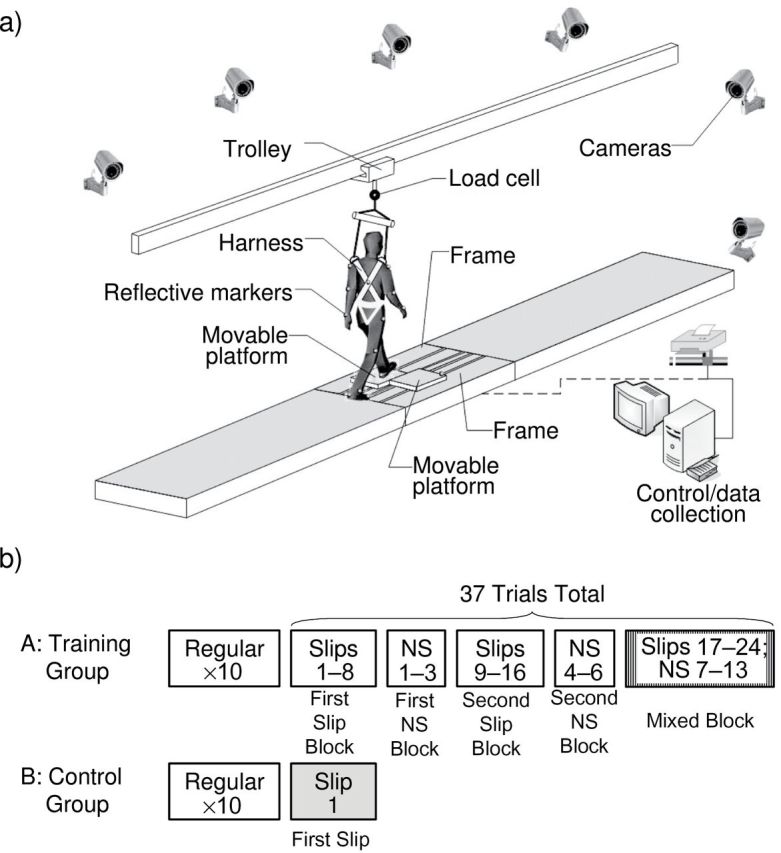
Fifty-one of those 269 community-dwelling older adults recruited initially did not participate in the initial sessiondue to poor bone density, five due to poor mobility, and one due to poor cognition/memory. The remaining 212 participants, having been randomly assigned into two groups (ie, the training and the control group), completed the initial session (Figure 3). There were no differences in age, body weight, history of falls, and risk for falls (Berg Balance Score) between the two groups at the time of the initial session, but more men (33.9% vs. 21.4%, p = .040) and higher level of mobility (Timed Up and Go score: 7.2±1.6 vs. 8.1±1.9 seconds, p < .001) were found in the training group than the control group. After the initial session, 42 participants from the training group and 28 from the control group failed to complete the entire falls monitoring program and were considered dropout based on our study protocol (Figure 3). However, these data were included in the intent-to-treat analysis. Participants who dropped out were older (74.6±5.2 vs. 72.0±5.5 years, p = .018) in the training group but were heavier (82.7±16.8 vs. 75.2±14.4kg, p = .027) in the control group than were those who completed the study (Table 1). When two groups were pooled together, however, those 70 people who dropped out did not differ in any of these confounding variables from those 142 participants who stayed in the study (Figure 3). The final analysis of 67 participants included in the training group were slightly younger (72.0±5.5 vs. 73.7±5.3, p = .077) more likely to be men (34.3% vs. 21.3%, p = .083) with better mobility (7.2±1.3 vs. 7.9±1.6, p = .006) than were 75 participants in the control group (Table 1). These confounding variables were adjusted in the final generalized estimating equations model.
Figure 3.
Flowchart of the number of the participants in various phases of the study. Of 269 older adults (≥65 years) recruited from communities around the Greater Chicago Area, 51 participants did not continue due to poor bone density, five due to poor mobility, and one due to poor cognition/memory. The remaining 212 were randomly assigned to one of the two groups. The intervention in the initial session consisted of repeated exposure to a total of 24 slips for the training group, whereas the control group only experienced a single slip. In the next 12 months, 142 of them completed the falls monitoring program, and the results from 67 and 75 participants were analyzed for the training group and the control group, respectively.
Table 1.
Sample Demographics and Confounding Factors by Experimental Groups
| Baseline Characteristics | Training Group (N = 109) | Control Group (N = 103) |
p Value (A vs. C) |
||||
|---|---|---|---|---|---|---|---|
| (A) Complete (N = 67) | (B) Dropout (N = 42) | p Value (A vs. B) | (C) Complete (N = 75) | (D) Dropout (N = 28) | p Value (C vs. D) | ||
| Age (y) | 72.0±5.5 | 74.6±5.2 | .0184 | 73.7±5.3 | 74.4±6.0 | .5459 | .0765 |
| Gender (male) | 23 (34.3%) | 14 (33.3%) | .9150 | 16 (21.3%) | 6 (21.4%) | .9916 | .0833 |
| Mass (kg) | 75.6±13.0 | 75.3±14.3 | .9113 | 75.2±14.4 | 82.7±16.8 | .0265 | .8619 |
| History of falls (yes) | 23 (34.3%) | 13 (31.0%) | .6985 | 29 (38.7%) | 8 (28.6%) | .6383 | .5922 |
| Berg Balance Scale | 54.7±1.7 | 54.3±1.8 | .1858 | 54.4±1.8 | 53.6±2.3 | .0935 | .2668 |
| Timed Up and Go score | 7.2±1.3 | 7.2±1.9 | .8640 | 7.9±1.6 | 8.6±2.4 | .1768 | .0059 |
Upon the novel (first) slip in walking during the initial session, rate of falls was similar between these two groups (49% for the training group vs. 56% for the controls, p = .60, Figure 4). Those in the training group quickly learned fall-resisting skills after the repeated-slip exposure in the protective laboratory environment and were able to successfully reduce their rate of falls to 0% upon their final (24th) slip (p < .001, Figure 4). Subsequently, participants in the training group were able to reduce their falls outside of laboratory by 50%, down from 34% to 15%, over the next 12 months (p = .026). In contrast, one slip did not significantly change the control group’s risk of falls during the same 12-month period (39% vs. 32%, p = .35, Figure 4).
Figure 4.

(a) Rate of falls (%) during the first slip for the training group (filled circles) and the control group (open squares) and during the final (24th) slip in the initial session. (b) Annual rate of self-reported falls both groups experience in everyday living prior to the initial session (history) and in 12 months following the initial session (prospective). * indicates a significance level of p < .05, **p < .01, and ***p < .001.
Falls characteristics during the 12-month follow-up period were summarized in Table 2. For both on-treatment and intention-to-treat analyses, the control group illustrated significantly higher portion of participants with prospective falls during the 12-month period than the training group (32% vs. 15%, p = .0173 and 25% vs. 13%, p = .0193, respectively). There were no differences in frequency of falls, activities prior to falling, perceived cause of falling, and injuries sustained from a fall between the training and control groups.
Table 2.
Falls Characteristics During the 12-Month Fall-Monitoring Program by Experimental Groups
| Falls Characteristics | On-Treatment Analysis | p Value | Intention-to-Treat Analysis | p Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Training (N = 67) | Control (N = 75) | Training (N = 109) | Control (N = 103) | |||||||
| N | % | N | % | N | % | N | % | |||
| Prospective falls | ||||||||||
| Yes | 10 | 14.9 | 24 | 32.0 | .0173 | 14 | 12.8 | 26 | 25.2 | .0193 |
| No | 57 | 85.1 | 51 | 68.0 | 88 | 80.7 | 70 | 68.0 | ||
| Nonreport | — | — | — | — | 7 | 6.4 | 7 | 6.8 | ||
| Frequency of falls | ||||||||||
| 0 | 57 | 85.1 | 51 | 68.0 | .0990 | 88 | 80.7 | 70 | 68.0 | .1049 |
| 1 | 9 | 13.4 | 19 | 25.3 | 11 | 10.1 | 21 | 20.4 | ||
| 2 | 1 | 1.5 | 4 | 5.3 | 3 | 2.8 | 4 | 3.9 | ||
| 3 | 0 | 0.0 | 1 | 1.3 | 0 | 0.0 | 1 | 1.0 | ||
| Nonreport | — | — | — | — | 7 | 6.4 | 7 | 6.8 | ||
| Activities prior to falling | ||||||||||
| Ambulation | 2 | 20.0 | 9 | 37.5 | .9430 | 6 | 42.9 | 10 | 38.5 | .9815 |
| Transferring | 1 | 10.0 | 2 | 8.3 | 1 | 7.1 | 3 | 11.5 | ||
| Running | 0 | 0.0 | 1 | 4.2 | 0 | 0.0 | 1 | 3.8 | ||
| Sports | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | ||
| Stairs/curb | 1 | 10.0 | 1 | 4.2 | 2 | 14.3 | 1 | 3.8 | ||
| Others/unknown | 6 | 60.0 | 11 | 45.8 | 5 | 35.7 | 11 | 42.3 | ||
| Perceived cause of falling | ||||||||||
| Slips | 2 | 20.0 | 4 | 16.7 | .8269 | 4 | 28.6 | 4 | 15.4 | .3368 |
| Trips | 5 | 50.0 | 8 | 33.3 | 8 | 57.1 | 10 | 38.5 | ||
| ADL and transfers | 1 | 10.0 | 1 | 4.2 | 1 | 7.1 | 1 | 3.8 | ||
| External hazards | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | ||
| Others/unknown | 2 | 20.0 | 11 | 45.8 | 1 | 7.1 | 11 | 42.3 | ||
| Injuries sustained from falls | ||||||||||
| Fracture | 0 | 0.0 | 2 | 8.3 | .9876 | 1 | 7.1 | 2 | 7.7 | .8673 |
| Treated injury | 0 | 0.0 | 2 | 8.3 | 1 | 7.1 | 2 | 7.7 | ||
| Untreated injury | 2 | 20.0 | 4 | 16.7 | 2 | 14.3 | 4 | 15.4 | ||
| No injury | 8 | 80.0 | 16 | 66.7 | 10 | 71.4 | 18 | 69.2 | ||
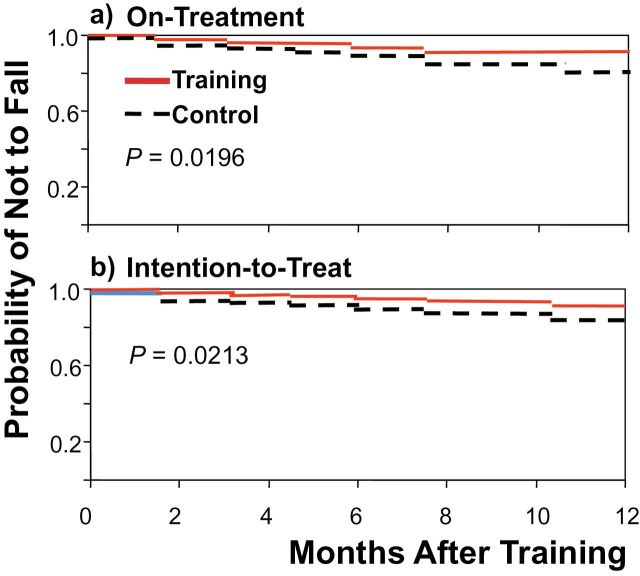
Kaplan–Meier survival analysis showed that the control group had a greater likelihood of falls during the 12-month follow-up period than the training group using both on-treatment (Figure 5a) and intention-to-treat analyses (Figure 5b). The multivariable analysis with generalized estimating equations model further confirmed these findings with significant time (history vs. prospective falls) and group-by-time interaction effects (Table 3). There was an overall reduction in the risk of falls (odds ratio = 0.31, 95% confidence interval: 0.16–0.64, p = .002), but most of the reductions were from the training group as illustrated by the significant group-by-time interaction. Participants in the control group were 2.3 times more likely to experience falls in the next 12 months than did those in the training group (odds ratio = 2.30, 95% confidence interval: 1.04–5.49, p = .033, Table 3). The intention-to-treat analysis yielded a similar result.
Figure 5.
(a) On-treatment analysis of Kaplan–Meier survival curves of falls during the 12-month fall-monitoring program. (b) Intention-to-treat analysis of Kaplan–Meier survival curves of falls during the 12-month fall-monitoring program.
Table 3.
Generalized Estimating equations Model on Change in Rate of Falls in Everyday Living
| Parameter | On-Treatment Analysis | Intention-to-Treat Analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p Value | OR | 95% CI | p Value | |
| Group (control) | 1.12 | 0.60–2.08 | .6610 | 1.07 | 0.54–2.14 | .7023 |
| Time (12 mo vs. pre) | 0.31 | 0.16–0.64 | .0018 | 0.42 | 0.18–0.68 | .0036 |
| Group × Time | 2.30 | 1.04–5.49 | .0339 | 2.00 | 1.01–5.76 | .0481 |
| Gender (female) | 1.35 | 0.72–2.52 | .1089 | 1.23 | 0.68–2.56 | .1211 |
| Age | 0.97 | 0.92–1.02 | .1714 | 0.98 | 0.91–1.02 | .1824 |
| Timed Up and Go score | 0.99 | 0.84–1.17 | .8556 | 0.99 | 0.85–1.19 | .8577 |
Note: 95% CI = 95% confidence interval; OR = odds ratio.
Further analysis suggested that perturbation training had more profound effect on participants with history of falls than it did to those without such history (Table 4). More than half of the fallers (55%) in the control group continued to experience falls in the same duration of 12 months. In contrast, only 26% of the previous fallers in the training group experienced further falls in their everyday living (between-group p = .035, Table 4), although they still appeared to fall more frequently than did those without previous history of falls after receiving the same training (9.1%, p = .064). Interestingly, those participants without previous history of falls in the training group (9.1%) also appear to be less likely to fall in comparison to their counterpart in the control group (17.4%, Table 4), though such difference did not reach a significant level (p = .2469, Table 4).
Table 4.
Prospective Falls During 12-Month Follow-up Period by Experimental Groups
| Baseline History of Falls | Training (N = 67) | Control (N = 75) | p Value | ||
|---|---|---|---|---|---|
| Faller/Total | % | Faller/Total | % | ||
| Yes | 6/23 | 26.1 | 16/29 | 55.2 | .0350 |
| No | 4/44 | 9.1 | 8/46 | 17.4 | .2469 |
| Total | 10/67 | 14.9 | 24/75 | 32.0 | .0173 |
Discussion
The novel approach of perturbation training by letting older adults learn from falling in a safe and well-controlled environment puts slips into good use. Such perturbation training could improve older adults’ proactive and reactive control of stability and their limb support against collapse in a laboratory setting (14,26). When older adults were retested in the same laboratory settings 6 months (14,26) or even 12 months (19) after the initial session, they also showed significantly greater retention of such training effects. These laboratory observations have enabled us to hypothesize that perturbation training may reduce older adults’ annual fall risk in everyday living outside of the laboratory. Now, the results indeed further confirmed that such training benefits can be retained and be generalized to reduce these older adults’ likelihood of annual fall risk by 50% in their daily living (Table 2 and Figures 4 and 5).
In this study, we have applied the overlearning principle in a total of 24 slips in randomized-block design, which is known to augment both the retention and the generalization (28). Although an occasional slip could in itself be a learning experience, experimental evidence suggests that a single session of 24 slips can be superior than a single slip (29). The learning (retention and its generalization) may be further reinforced by the perceived or real penalties that could result from errors in failed recovery. In real life, such falls can lead to severe or even life-threatening injuries. Thus, consequences of an inappropriate response to slip (and a fall) may implicitly (albeit subconsciously) motivate the central nervous system to quickly learn and remember the improved movement strategies for an extended period. Fear-conditioning studies in mice have demonstrated that a single session is sufficient for long-term retention of the acquired stimulus–response behavior (30). Notably, our training effect was especially prominent among those at-risk of falls (who had a history of falls). The fear resulting from previous falls might have further accentuated (consciously or unconsciously) their learning.
Because relatively few people in both groups fell in everyday living (30% or less) and even fewer in each category of falls, the findings of this study can only be preliminary that require further verification. It remains unclear, for instance, whether such training-induced benefits can be generalizable or would be more specific to slip-related falls in everyday living. In Table 2, the percentage of trips and slips, which accounts for up to 60% of falls by older adults, was quantitatively greater in the trained group. Indeed, the largest number of falls in the untrained group was from unknown causes. This is not trivial. Arguably, the significant between-group difference in prospective falls may have been driven by the rather large difference in falls due to unknown causes, for which any explanation can only be speculative. Therefore, any attempt to link perturbation training to specific type of fall outcome (eg, slip or trip) could be misled due to this and other data limitations. Nonetheless, a combined all-cause falls is still an acceptable endpoint (from data logistics perspective) to provide evidence on outcome evaluation for this novel approach of perturbation training among the elderly people.
We are only at the beginning of understanding the potential benefits or the limitations of perturbation training in terms of its generalizability and specificity. We first investigated that repeated-slip training-induced interlimb transfer effects, that is, to what degree young adults could withstand a novel slip applied to the untrained contralateral limb during walking (31). We subsequently investigated generalization across different environmental conditions and found that after being trained with moveable platform induced slips, young adults were able to resist falling when exposed to a slippery vinyl floor (16). We then looked at young adults’ ability to generalize skills across different tasks (intertask) and demonstrated that they could resist slip-induced falls during walking after being given repeated-slip training during a sit-to-stand task (15). We also studied the generalizability from repeated-slip training on a computer-controlled treadmill to a novel over-ground slip during level walking (7).
Moreover, we investigated how repeated-slip training would affect recovery from a novel trip, which is a diametrically opposing type of perturbation (18). The results indicated that although adaptation to slips did interfere with the proactive control of stability (negative effect) just as one would have expected, the adaptive improvements in reactive control were able to generalize to the trip response (positive effect). The latter (the generalization) was sufficient to mitigate such interference. All evidence seems to point to the conclusion that, in general, training will improve both proactive and reactive control of stability (7,15,16,31) and that one or both mechanisms may be generalizable across conditions outside of the training context or even crossover to opposing types of perturbation as seen in the slip-to-trip study (18). Although it is not clear whether the current perturbation-training paradigm would result in the largest effects only on slip-related falls in real life (though it is theoretically logical), our findings are still promising given the highly debilitating fractures associated with these falls among the elderly people.
Perturbation training is different from the conventional performance-based, self-initiated, and self-motivated training in several respects. Unlike conventional training, such as muscle strengthening and standing balance training, perturbation training mimics naturalistic environments. It induces gross errors (32,33) and improves the effectiveness of protective stepping that can be generalized to untrained activities, from sit-to-stand to walking for instance (15), and that is involuntary in nature, which do not exist in self-initiated performance or exercise. Experiencing such errors is essential for the central nervous system to recalibrate an existing internal representation of the environment (34,35)—in this case, pertaining to the stability limits—which provides the basis required in order to make adaptive adjustments in protective stepping and in both proactive and reactive control of stability. Training that focuses only on self-initiated (and in essence, volitional and self-motivated) performance may not provide the opportunity for someone to improve his or her reaction to unexpected or unpreventable postural disturbances.
Further, the recalibration process appears to take place in just a few perturbation trials (25,36) that does not require the same length of training as developing a new motor program. We have shown that “skate-over” or “walkover” movement strategies can quickly emerge when older adults traverse across the same slippery surface (Figure 2b and c) (25). In contrast to the conventional performance-based training that could require at least 50 hours/sessions of training (37), a single session of perturbation-based training may improve their resilience to postural disturbances year-round. Does that sound “too good to be true”? Studies conducted by independent investigative groups may provide additional verification or confirmation.
This study did not include a “pure” control group who walked on the same walkway for the same number of trials and the same length of time but did not experience any slip. Evidence suggests that even a single slip (as experienced by the control group) may yield some training effects (29). The rationale to use such a control group was that a single slip would better prepare participants against future falls than using a control group who had never experienced any slip in the same laboratory setting. Hence, demonstrating that repeated-slip training is better than a single slip would provide a higher order evidence than to merely demonstrate that such training is better than a “pure” control group without any slip exposure. The results indeed suggest that repeated-slip exposure is better than an occasional incident of a single slip that an untrained person could otherwise naturally experience in real-life situations (Figure 4).
This study has limitations. It did not explore the optimum dose–response (numbers of slip exposure) relationship that is required for providing efficiency and optimal outcome. The monitoring of falls in everyday living was conducted through falls diary, which could be influenced by many factors including the accuracy of recall and participation adherence, although this approach is still one of the most commonly applied methods for such studies (9,10,38–41). Any systematic, methodological-related bias would, however, likely have affected both the training group and the control group similarly. Although our findings suggest that training could be especially helpful to those who previously had a history of falls, the sample size for such analyses on subgroups is still small. Finally, these findings are relevant only for healthy and active older adults, who presumably are more likely to have the neuromotor plasticity and to respond safely and develop subsequent fall response strategies than the more impaired older adults.
In conclusion, the results lend support to our hypothesis that perturbation training can reduce community-dwelling older adults’ annual risk of falls in their everyday living. Based on the evidence presented here, it is conceivable that a future intervention strategy may also include a “vaccination-like” component to boost older adults’ resilience in response to postural disturbances.
Funding
This work was supported by the National Institutes of Health (2R01-AG16727, R01-AG029616 to Y.-C.P.).
Acknowledgments
The authors thank Debbie Espy, PhD, and Ms. Yiru Wang for assisting in data collection and processing.
References
- 1. Kannus P, Sievanen H, Palvanen M, Jarvinen TLN, Parkkari J. Prevention of falls and consequent injuries in elderly people. Lancet. 2005;336:1885–1893. [DOI] [PubMed] [Google Scholar]
- 2. Alexander BH, Rivara FP, Wolf ME. The cost and frequency of hospitalization for fall-related injuries in older adults. Am J Public Health. 1992;82:1020–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Luukinen H, Herala M, Koski K, Honkanen R, Laippala P, Kivelä SL. Fracture risk associated with a fall according to type of fall among the elderly. Osteoporos Int. 2000;11:631–634. [DOI] [PubMed] [Google Scholar]
- 4. Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(suppl 2):ii37–ii41. [DOI] [PubMed] [Google Scholar]
- 5. Pai YC, Bhatt TS. Repeated-slip training: an emerging paradigm for prevention of slip-related falls among older adults. Phys Ther. 2007;87:1478–1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shimada H, Obuchi S, Furuna T, Suzuki T. New intervention program for preventing falls among frail elderly people: the effects of perturbed walking exercise using a bilateral separated treadmill. Am J Phys Med Rehabil. 2004;83:493–499. [DOI] [PubMed] [Google Scholar]
- 7. Yang F, Bhatt T, Pai YC. Generalization of treadmill-slip training to prevent a fall following a sudden (novel) slip in over-ground walking. J Biomech. 2013;46:63–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rubenstein LZ, Josephson KR. Falls and their prevention in elderly people: what does the evidence show? Med Clin North Am. 2006;90:807–824. [DOI] [PubMed] [Google Scholar]
- 9. Wolf SL, Sattin RW, Kutner M, O’Grady M, Greenspan AI, Gregor RJ. Intense tai chi exercise training and fall occurrences in older, transitionally frail adults: a randomized, controlled trial. J Am Geriatr Soc. 2003;51:1693–1701. [DOI] [PubMed] [Google Scholar]
- 10. Shumway-Cook A, Silver IF, LeMier M, York S, Cummings P, Koepsell TD. Effectiveness of a community-based multifactorial intervention on falls and fall risk factors in community-living older adults: a randomized, controlled trial. J Gerontol A Biol Sci Med Sci. 2007;62:1420–1427. [DOI] [PubMed] [Google Scholar]
- 11. Tinetti ME, Baker DI, McAvay G, et al. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med. 1994;331:821–827. [DOI] [PubMed] [Google Scholar]
- 12. Pai YC, Patton J. Center of mass velocity-position predictions for balance control. J Biomech. 1997;30:347–354. [DOI] [PubMed] [Google Scholar]
- 13. Pai YC, Iqbal K. Simulated movement termination for balance recovery: can movement strategies be sought to maintain stability in the presence of slipping or forced sliding? J Biomech. 1999;32:779–786. [DOI] [PubMed] [Google Scholar]
- 14. Bhatt T, Yang F, Pai YC. Learning to resist gait-slip falls: long-term retention in community-dwelling older adults. Arch Phys Med Rehabil. 2012;93:557–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wang TY, Bhatt T, Yang F, Pai YC. Generalization of motor adaptation to repeated-slip perturbation across tasks. Neuroscience. 2011;180:85–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bhatt T, Pai YC. Generalization of gait adaptation for fall prevention: from moveable platform to slippery floor. J Neurophysiol. 2009;101:948–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pai YC, Bhatt T, Wang E, Espy D, Pavol MJ. Inoculation against falls: rapid adaptation by young and older adults to slips during daily activities. Arch Phys Med Rehabil. 2010;91:452–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bhatt T, Wang TY, Yang F, Pai YC. Adaptation and generalization to opposing perturbations in walking. Neuroscience. 2013;246:435–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pai Y-C, Yang F, Bhatt T, Wang E. Learning from laboratory-induced falling: long-term motor retention among older adults. Age (Dordr). 2014 March 26. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Folstein MF, Folstein SE, McHugh PR. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. [DOI] [PubMed] [Google Scholar]
- 21. Thompson PW, Taylor J, Oliver R, Fisher A. Quantitative ultrasound (QUS) of the heel predicts wrist and osteoporosis-related fractures in women age 45–75 years. J Clin Densitom. 1998;1:219–225. [DOI] [PubMed] [Google Scholar]
- 22. Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–148. [DOI] [PubMed] [Google Scholar]
- 23. Yang F, Pai YC. Correction of the inertial effect resulting from a plate moving under low-friction conditions. J Biomech. 2007;40:2723–2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Yang F, Pai YC. Automatic recognition of falls in gait-slip training: harness load cell based criteria. J Biomech. 2011;44:2243–2249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bhatt T, Wang E, Pai YC. Retention of adaptive control over varying intervals: prevention of slip-induced backward balance loss during gait. J Neurophysiol. 2006;95:2913–2922. [DOI] [PubMed] [Google Scholar]
- 26. Bhatt T, Yang F, Pai YC. Learning from falling: retention of fall-resisting behavior derived from one episode of laboratory-induced slip training. J Am Geriatr Soc. 2011;59:2392–2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Talbot LA, Musiol RJ, Witham EK, Metter EJ. Falls in young, middle-aged and older community dwelling adults: perceived cause, environmental factors and injury. BMC Public Health. 2005;5:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Schmidt RA, Lee TD. Conditions of practice. In: Schmidt RA, Lee TD, eds. Motor Control and Learning: A Behavioral Emphasis. Champaign, IL: Human Kinetics Publishers; 1999:285–318. [Google Scholar]
- 29. Bhatt T, Pai YC. Prevention of slip-related backward balance loss: the effect of session intensity and frequency on long-term retention. Arch Phys Med Rehabil. 2009;90:34–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sacchetti B, Scelfo B, Tempia F, Strata P. Long-term synaptic changes induced in the cerebellar cortex by fear conditioning. Neuron. 2004;42:973–982. [DOI] [PubMed] [Google Scholar]
- 31. Bhatt T, Pai YC. Immediate and latent interlimb transfer of gait stability adaptation following repeated exposure to slips. J Mot Behav. 2008;40:380–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Scheidt RA, Dingwell JB, Mussa-Ivaldi FA. Learning to move amid uncertainty. J Neurophysiol. 2001;86:971–985. [DOI] [PubMed] [Google Scholar]
- 33. Tseng YW, Diedrichsen J, Krakauer JW, Shadmehr R, Bastian AJ. Sensory prediction errors drive cerebellum-dependent adaptation of reaching. J Neurophysiol. 2007;98:54–62. [DOI] [PubMed] [Google Scholar]
- 34. Blakemore SJ, Goodbody SJ, Wolpert DM. Predicting the consequences of our own actions: the role of sensorimotor context estimation. J Neurosci. 1998;18:7511–7518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Shadmehr R, Mussa-Ivaldi FA. Adaptive representation of dynamics during learning of a motor task. J Neurosci. 1994;14(5 Pt 2):3208–3224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Karniel A, Mussa-Ivaldi FA. Does the motor control system use multiple models and context switching to cope with a variable environment? Exp Brain Res. 2002;143:520–524. [DOI] [PubMed] [Google Scholar]
- 37. Sherrington C, Tiedemann A, Fairhall N, Close JC, Lord SR. Exercise to prevent falls in older adults: an updated meta-analysis and best practice recommendations. N S W Public Health Bull. 2011;22:78–83. [DOI] [PubMed] [Google Scholar]
- 38. Banz DA, Higashi T, Rubenstein LZ. Monitoring falls in cohort studies of community-dwelling older people: effect of the recall interval. J Am Geriatr Soc. 2005;53:2190–2194. [DOI] [PubMed] [Google Scholar]
- 39. Buchner DM, Cress ME, de Lateur BJ, et al. The effect of strength and endurance training on gait, balance, fall risk, and health services use in community-living older adults. J Gerontol A Biol Sci Med Sci. 1997;52:M218–M224. [DOI] [PubMed] [Google Scholar]
- 40. Rubenstein LZ, Josephson KR, Trueblood PR, et al. Effects of a group exercise program on strength, mobility, and falls among fall-prone elderly men. J Gerontol A Biol Sci Med Sci. 2000;55:M317–M321. [DOI] [PubMed] [Google Scholar]
- 41. Fitzharris MP, Day L, Lord SR, Gordon I, Fildes B. The Whitehorse NoFalls trial: effects on fall rates and injurious fall rates. Age Ageing. 2010;39:728–733. [DOI] [PubMed] [Google Scholar]