Abstract
Background
Neuraminidase (NA) inhibitors are the only licensed therapeutic option for human zoonotic H7N9 infections. An NA-R292K mutation that confers broad-spectrum resistance to NA inhibitors has been documented in H7N9 patients after treatment.
Methods
We evaluated the transmission potential of a human influenza A H7N9 isolate with a NA-R292K mutation in the ferret model followed by genotyping assay to monitor its competitive fitness in vivo.
Results
Plaque-purified A/Shanghai/1/2013 wild-type and NA-R292K viruses transmitted at comparable efficiency to direct or respiratory droplet contact ferrets. In ferrets inoculated with the plaque-purified A/Shanghai/1/2013 NA-R292K virus with dominant K292 (94%), the resistant K292 genotype was outgrown by the wild-type R292 genotype during the course of infection. Transmission of the resistant K292 genotype was detected in 3/4 direct contact and 3/4 respiratory droplet contact ferrets at early time points but was gradually replaced by the wild-type genotype. In the respiratory tissues of inoculated or infected ferrets, the wild-type R292 genotype dominated in the nasal turbinate, whereas the resistant K292 genotype was more frequently detected in the lungs.
Conclusions
The NA inhibitor-resistant H7N9 virus with the NA-R292K mutation may transmit among ferrets but showed compromised fitness in vivo while in competition with the wild-type virus.
Keywords: H7N9 influenza virus, R292K NA mutation, neuraminidase inhibitors, resistance, transmission, ferrets
With 2 waves of human infections in Spring and Winter 2013, the H7N9 avian influenza virus has led to over 440 confirmed cases since its emergence and is currently a major public health threat. Compared to the highly pathogenic H5N1 influenza that was first reported to cause human infections since 1997, H7N9 virus showed differences in epidemiological patterns [1], disease severity and symptomatic case fatality risk [2, 3], viral tropism in human respiratory tract [4, 5], and transmission potential in animal models [6–12]. Specifically, the H7N9 patients have significantly higher median age, higher proportion being the male gender, a longer duration of hospitalization, and a lower case fatality rate compared to the H5N1 patients [1–3]. Experimental ex vivo infections or virus attachment assays with H7N9 viruses demonstrated a broader tissue tropism ranging from upper to lower respiratory tract, which is distinct to the H5N1 viruses that target the epithelial cells and alveolar macrophages in the lungs [4, 5]. Furthermore, H7N9 showed moderate transmissibility among ferrets or guinea pigs in risk assessment studies [6–12], whereas the H5N1 viruses showed no or inefficient ferret-to-ferret transmission [13]. Although vaccines are being developed against H7N9 virus, their immunogenicity and availability remain uncertain in the event of H7N9 virus acquiring capacity for sustained human-to-human transmission [14]. The neuraminidase (NA) inhibitors have been the main therapeutic option for H7N9 patients but the emergence of resistance variants have been documented in 6 patients during the first wave of the epidemic, among which 3 were fatal [15–18].
We and others have previously characterized a human H7N9 isolate A/Shanghai/1/2013 containing a mixed population of R/K at NA residue 292 (N2 numbering from now on) and confirmed that the presence of an R292K mutation in the H7N9 viruses confers resistance to available NA inhibitors including oseltamivir carboxylate, peramivir, and zanamivir [8, 19–21]. Unlike the M2 ion channel blocker-resistant variants, the NA inhibitor resistant variants often lack sustained human-to-human transmissibility, with the exception of the A/Brisbane/59/2007-like seasonal H1N1 virus that emerged in the 2007–2008 influenza season [22]. The H3N2 seasonal influenza virus carrying the R292K mutation showed no [23, 24] or compromised [25] transmissibility to direct contact ferrets. However, it has been recently reported that clinical derived or recombinant H7N9 virus with the R292K mutation showed comparable pathogenicity in mice [20, 26] and a similarly inefficient airborne transmissibility in guinea pigs [20]. In the present study, we evaluated the transmission potential of plaque-purified A/Shanghai/1/2013 wild-type or its NA-R292K mutant counterpart in the ferret model followed by genotyping assay to monitor the fitness of the R292K mutation in vivo.
METHODS
Cells and Viruses
Madin-Darby canine kidney (MDCK) cells were obtained from the ATCC and were maintained in minimum essential medium supplemented with 10% fetal calf serum. The A/Shanghai/1/2013 (H7N9) virus was kindly provided by Dr Yuelong Shu at Chinese Center for Disease Control and Prevention. The plaque-purified A/Shanghai/1/2013 wild-type (WT-6) and NA-R292K mutant (MUT-6) viruses previously characterized in vitro [19] were used to evaluate their transmission potential in ferrets.
Transmission Experiment in Ferrets
Transmissibility was tested in 4- to 6-month-old male ferrets obtained from Sangosho (Wuxi, China). All studies were conducted in the BSL3 facility at LKS Faculty of Medicine, University of Hong Kong, in compliance with all applicable laws and with the ethics approval from the Committee on the Use of Live Animals in Teaching and Research (CULATR) at the University of Hong Kong. Ferrets used in the study were confirmed to be seronegative for influenza A virus NP protein using ID Screen Influenza A Antibody Competition Enzyme-Linked Immunosorbent Assay (ELISA) kit (ID.vet) and have a hemagglutination inhibition titer ≤20 against a panel of selected influenza viruses. Virus transmission experiments used groups of inoculated donor ferrets, naive direct-contact ferrets, and naive respiratory droplet–contact ferrets as described elsewhere [27]. The transmission experiment was performed in replicate of 4 for each virus in 2 independent experiments. Donors were inoculated intranasally with 105 plaque-forming units (PFU) of virus in 0.5 mL media under isoflurane anesthesia. At 24 hours post-inoculation, we introduced naive ferrets to either co-house with the infected donor (direct contact) or house separately in an adjacent cage (by 4 cm) to the infected donor, separated by a perforated (0.5 cm holes separated by 1 cm) stainless steel divider (respiratory droplet contact). To monitor virus shedding, nasal washes were collected from all ferrets daily for 14 days and were titrated in MDCK cells. Ferret weight, temperature, and clinical signs were monitored daily. Post-exposure sera from naive direct contact or respiratory droplet contact ferrets were collected at 18 days post-contact to monitor seroconversion by using ID Screen Influenza A Antibody Competition ELISA kit (ID.vet). To monitor virus replication in the respiratory tract, tissues from the respiratory tract (nasal turbinate, upper trachea, middle trachea, whole right upper lung lobe, and whole left lower lung lobe) were collected on day 5 post-inoculation (day 4 post-contact) from 2 donors, 2 direct contacts, and 2 respiratory droplet contact ferrets for virus titration and genotyping assays. The respiratory tissues were also fixed in 10% neutral buffered formalin and embedded in paraffin for histology examination or immunohistochemistry [28].
Infectivity In Vitro
The 50% tissue culture infectious dose (TCID50) was determined in confluent MDCK cells in 96-well flat-bottom tissue culture plates. Prior to infection, cells were washed twice with phosphate-buffered saline and overlaid with infection media (MEM supplemented with 0.3% BSA and 1 µg/mL TPCK-trypsin). Cells were incubated with serial half-log diluted ferret nasal wash samples or supernatants from ferret respiratory tissue homogenate (replicates of 4 for each dilution) at 37°C for 72 hours. Hemagglutination assay using 5% turkey erythrocytes was performed to determine the endpoint of infection, and virus titers (log10 TCID50/mL) were calculated by the Reed-Muench method [29].
qRT-PCR Assay to Quantify the Ratio of R/K at NA Residue 292
Real-time polymerase chain reaction (PCR) with absolute quantitation (qPCR) was applied to monitor the percentage of the wide-type (R292) and mutant (K292) populations in ferret nasal washes or ferret respiratory tract tissues over the course of infection or transmission with the plaque-purified A/Shangahi/1/13 MUT-6 virus. In brief, 100 µL nasal wash or tissue homogenate supernatant was subjected to RNA extraction (RNeasy mini kit; Qiagen), with RNA eluted in 30 µL nuclease free water. SuperScript III First-Strand Synthesis System (Invitrogen) was used for complementary DNA (cDNA) synthesis (20 µL reaction) with 8 µL of the eluted RNA and Uni12 (AGCRAAAGCAGG) as primer. Amplification and qPCR measurements were performed using the LightCycler 480 Real-Time PCR System (Roche). Experiments were performed in 25 µL reactions with 5 µL cDNA and the LightCycler 480 Probes Master kit (Roche). The sequences of probes and primers were reported as described elsewhere [18]. Standard curves were established by serial 10-fold dilution of the control plasmids encoding the full length NA gene derived from A/Shanghai/1/2013 with either R (AGG) or K (AAG) at residue 292. Five spike-in plasmid controls with R292:K292 mixed at different ratios (90:10, 80:20, 50:50, 20:80, and 10:90) were included in each run.
Clonal Sequencing
Total RNA was extracted from the viral culture supernatants (RNeasy, Qiagen).The full-length HA and NA gene of the expanded plaques were amplified by RT-PCR using the universal primers [30] and sequenced by Sanger sequencing. To determine the ratio of R/K at residue 292, a 789 bp PCR product fragment spanning the region of residue 292 was amplified by RT-PCR (Qiagen) (Forward: 5′-AACACATGGGCCCGAAAC-3; Reverse: 5′-ATATCGTCTCGTATTAGTAGAAACAAGGGTCTT-3′) and cloned into the pCR4-TOPO vector (Invitrogen). Plasmid DNA were isolated (Miniprep, Qiagen) and were sequenced by Sanger sequencing using the amplification primers.
Statistical Analysis
The date of peak virus shedding from direct contact or respiratory droplet contact ferrets infected with the A/Shanghai/1/2013 wild-type or R292K variant strains were compared by the log–rank test. The total amount of virus shedding was estimated by calculating the area under the curve using the virus titers determined at different days post-inoculation or post-contact. The area under the curve from direct contact or respiratory droplet contact ferrets infected with the A/Shanghai/1/2013 wild-type or R292K variant strains was compared using the Wilcoxon rank-sum test.
RESULTS
Transmissibility of the A/Shanghai/1/2013 Wild-Type and NA-R292K Mutant Viruses in Ferrets
We previously reported the in vitro characterization of the A/Shanghai/1/2013 wild-type and its NA-R292K mutant counterpart derived from a H7N9 fatal case through plaque purification [19]. Specifically, plaque purification was used to derive 2 clones that share identical HA sequence by Sanger sequencing but differ by the R292K mutation in the NA glycoprotein. Further genetic analysis of the internal genes of the wild-type clone (WT-6) and the mutant clone (MUT-6) identified 2 amino acids differences in the PB1 and PA proteins; specifically, comparing to the A/Shanghai/1/2013 sequence deposited in Genbank, the WT-6 possessed the Q248L change in the PA (and a deletion of the last five amino acids of the PA-X) protein, whereas the MUT-6 possessed the Q687R change in the PB1 protein (Table 1). We previously reported that wild-type clone (WT-6) with dominant R292 (93%) and the mutant clone (MUT-6) with dominant K292 (94%) both replicated efficiently to comparable titers in the MDCK-SIAT1 cells, suggesting that the R292K mutation did not compromise viral fitness in vitro. Importantly, the K292 genotype was stably maintained in the MDCK-SIAT1 culture supernatant after infection with the mutant clone (MUT-6) at 50 hours post-infection (data not shown).
Table 1.
Amino Acid Differences Between Plaque-Purified A/Shanghai/1/2013 Wild-Type (WT-6) and Its NA-R292K Mutant (MUT-6) Before and After Transmission in Ferrets
| Viruses | PB2 | PB1 | PA | NA | |
|---|---|---|---|---|---|
| A/Shanghai/1/2013 | Genbank | D441 | Q687 | Q248 | K292 |
| A/Shanghai/1/2013 plaque-purified clone WT-6 | Inoculum | D441 | Q687 | L248 | R292 |
| WT-6: Respiratory droplet contact 3 | 5 dpca | D441 | Q687 | L248 | R292 |
| WT-6: Respiratory droplet contact 4 | 5 dpca | D441 | Q687 | L248 | R292 |
| A/Shanghai/1/2013 plaque-purified clone MUT-6 | Inoculum | D441 | R687 | Q248 | K292 |
| MUT-6: Donor 3 | 2 dpib | N441 | R687 | Q248 | R/K292 |
| MUT-6: Donor 4 | 2 dpib | N441 | R687 | Q248 | R/K292 |
| MUT-6: Respiratory droplet contact 3 | 4 dpca | N441 | R687 | Q248 | K292 |
| MUT-6: Respiratory droplet contact 4 | 5 dpca | N441 | R687 | Q248 | R292 |
Abbreviation: NA, neuraminidase.
a Ferret nasal wash collected on days post-contact (dpc).
b Ferret nasal wash collected on days post-inoculation (dpi).
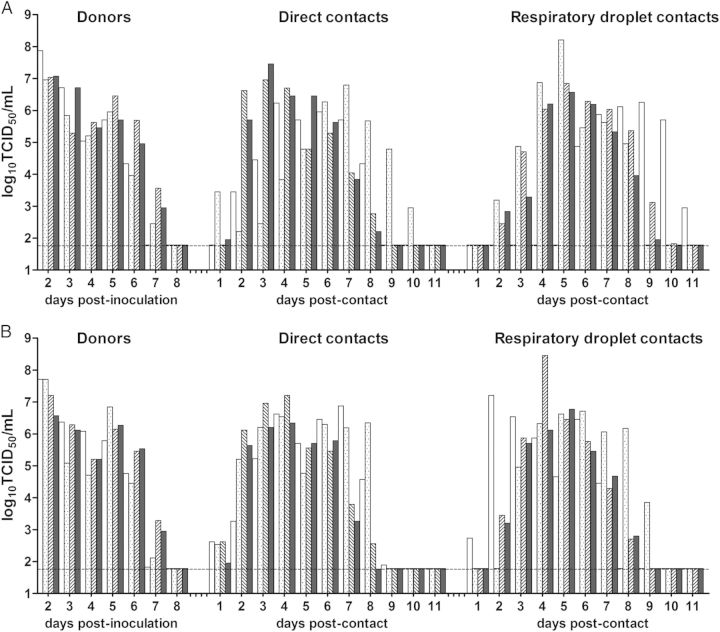
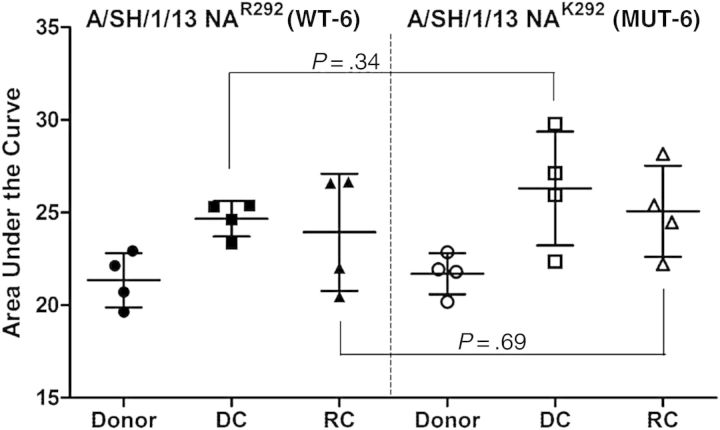
To further assess viral fitness and the transmission potential in vivo, we inoculated 4 donor ferrets intranasally with 105 TCID50 of the plaque-purified A/Shanghai/1/2013 wild-type (WT-6) or its NA-R292K mutant counterpart (MUT-6). Naive direct contact or respiratory droplet contact ferrets were introduced at 24 hours post-inoculation. Both the WT-6 (Figure 1A) and the MUT-6 (Figure 1B) viruses transmitted to 4/4 direct and 4/4 respiratory droplet contact ferrets at comparable efficiency. Virus shedding from direct contact ferrets was observed as early as at day 1 post-contact with the peak virus shedding detected on days 4, 7, 3, 3 and 7, 4, 4, 4 post-contact for WT-6 and MUT-6, respectively (P = .452, log–rank test). Peak virus shedding from respiratory droplet contact ferrets was detected on days 9, 5, 5, 5 and 2, 6, 4, 5 post-contact, respectively (P = .238, log–rank test). We calculated the area under the curve for the ferret nasal washes shed by each ferret. The amount of virus shedding estimated by the area under the curve, that represented the cumulative amount of virus shed during the course of infection was comparable between ferrets inoculated or infected by the plaque-purified A/Shanghai/1/2013 wild-type (WT-6) or its NA-R292K mutant counterpart (MUT-6; Figure 2). The transmission of the plaque-purified A/Shanghai/1/2013 wild-type (WT-6) or its NA-R292K mutant counterpart (MUT-6) were more efficient than that of the swine influenza viruses we reported previously under similar experimental settings [27].
Figure 1.
Transmission and nasal wash titers (log10TCID50/mL) detected in ferrets inoculated or infected by the plaque-purified A/Shanghai/1/2013 (H7N9) wild-type virus (A), or the plaque-purified A/Shanghai/1/2013 (H7N9) NA-R292K mutant virus (B). Nasal washes were collected daily from inoculated donor ferrets (days 2–8 post-inoculation), direct contact ferrets, and respiratory droplet contact ferrets (days 1–11 post-contact); the lower limit of detection was 1.789 log10TCID50/mL. Abbreviation: TCID50, 50% tissue culture infectious dose.
Figure 2.
Total amount of virus shedding was approximated by calculating the area under the curve for each ferret using the virus titers determined at different days post-inoculation or post-contact. The mean ± SD area under the curve were plotted for donors, direct contacts, or respiratory droplet contact ferrets infected with the A/Shanghai/1/2013 wild-type or NA-R292K mutant strains. P values showed the results from Wilcoxon rank-sum tests. Abbreviation: SD, standard deviation.
Ferrets inoculated or infected by the plaque-purified A/Shanghai/1/2013 wild-type (WT-6) or its NA-R292K mutant counterpart (MUT-6) exhibited comparable clinical signs, although ferrets in the MUT-6 group showed greater temperature elevation than those in the WT-6 group (Figure 3). The maximum elevated temperature was detected on day 2 post-inoculation in both WT-6 (1.50 ± 0.42°C, mean ± SD) and MUT-6 (1.80 ± 0.22°C) donor ferrets (P = .134, paired t-test) followed by a second peak detected on days 5 and 6 post-inoculation, respectively (Figure 3A). The maximum elevated temperature for direct contact ferrets infected by the WT-6 (0.70 ± 0.42°C) or MUT-6 (1.34 ± 0.71°C) were detected on day 7 post-contact (P = .185, paired t-test; Figure 3B). The maximum elevated temperature for respiratory droplet contact ferrets infected by the WT-6 (0.75 ± 0.25°C) or MUT-6 (1.20 ± 0.38°C) were significantly different (P = .037, paired t-test) and were detected on days 4 and 5 post-contact, respectively (Figure 3C). A greater temperature changes in the respiratory droplet contacts exposed to ferrets inoculated with A/Shanghai/1/2013 NA-K292 mutant clone (MUT-6) could be due to the 2 amino acid differences in the PB1 and PA genes observed between the plaque-purified wild-type (WT-6) and R292K mutant (MUT-6) inoculum viruses. It is interesting to note that although the virus shedding in the direct contact ferrets were detected earlier than that of the respiratory droplet contact ferrets, the maximum elevated temperatures were detected earlier in the respiratory droplet ferrets for both groups.
Figure 3.
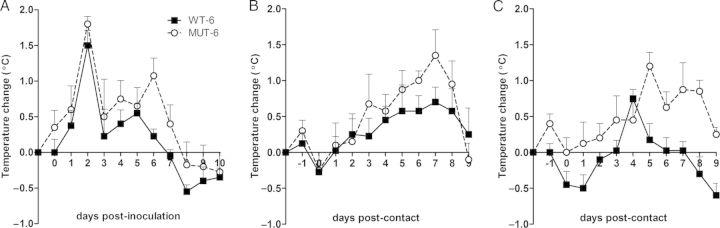
Temperature changes (°C, mean ± SD) of donors (A), direct contact ferrets (B), or respiratory droplet contact ferrets (C) over the course of transmission experiments with A/Shanghai/1/2013 wild-type or NA-R292K mutant viruses. The baseline temperature was determined at −1 day post-inoculation (−2 day post-contact). Abbreviation: SD, standard deviation.
To monitor potential amino acid changes during transmission, we analyzed viral sequences in the nasal washes of respiratory droplet contact ferrets (Table 1). The PA-Q248L mutation identified in the wild-type inoculum (WT-6) was maintained in the nasal washes of infected respiratory droplet contact ferrets. The PB1- Q687R mutation found in the mutant inoculum (MUT-6) was maintained in the nasal washes of the donor and respiratory droplet contact ferrets. Interestingly, an additional PB2-D441N mutation was found in the nasal washes of the donor and respiratory droplet contact ferrets infected with the mutant inoculum (MUT-6). It is possible that the PB2-D441N mutation may be present as a minor population in the mutant inoculum (MUT-6) and was rapidly selected in the donor ferrets after infection. Moreover, we observed mixed population of R/K at NA residue 292 from the nasal washes of 2 donors inoculated with the mutant inoculum (MUT-6). Among the 2 respiratory droplet contact ferrets analyzed, the R292K mutation was maintained in the nasal washes shed by 1 ferret, whereas the wild-type R292 genotype gained dominance in the nasal washes shed by the other ferret, suggesting the competitive fitness loss of the NA-R292K mutation in vivo.
Stability of the NA-R292K Mutation in Ferrets
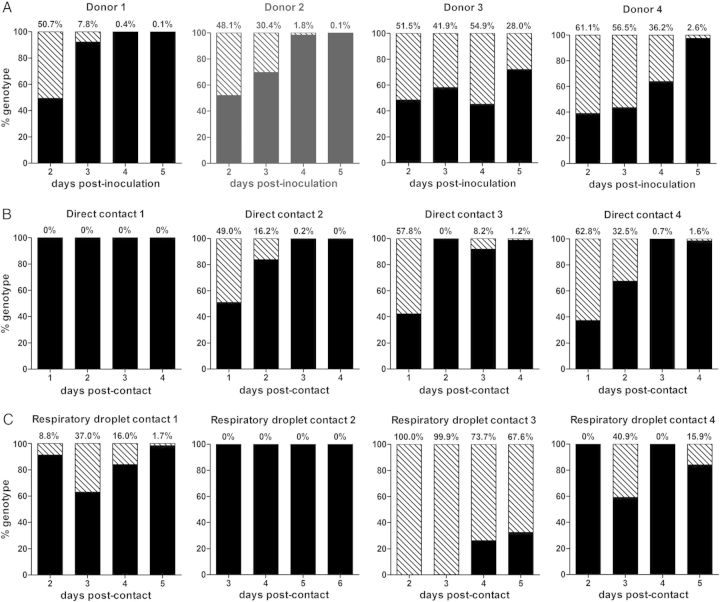
We applied the SNP qRT-PCR assay with specific probes to identify the R/K genotype at NA residue 292 [18]. Using clonal analysis, the plaque-purified R292K mutant virus (MUT-6) inoculum was dominated by K292 (94%, 15/16 clones) with minor presence of R292 (6%, 1/16 clones) [19]. In the nasal washes collected from donor ferrets inoculated with the plaque-purified MUT-6, we observed a gradual increase of the wild-type R292 genotype over the mutant K292 genotype over time (Figure 4A). On day 2 post-inoculation, the R292K mutation was detected at 48.1–61.1% in 4 donor ferrets; the percentage of the R292K mutation had dropped to <3% in 3/4 ferrets by day 5 post-inoculation, suggesting that the wild-type R292 genotype possess better fitness over the K292 genotype in vivo.
Figure 4.
Genotyping assay to determine the percentage of R292/ K292 in the nasal washes of donors (A), direct contact ferrets (B), and respiratory droplet contact ferrets (C) infected with the plaque-purified A/Shanghai/1/2013 NA-R292K mutant virus. The percentages of the mutant K292 genotype are shown using diagonally striped bars, and the percentages of the wild-type R292 genotype are shown using solid black bars.
We also monitored the R/K genotype that was transmitted to direct and respiratory droplet contact ferrets. In 3/4 direct contact ferrets, we can detect the mutant K292 genotype at 49.0%–62.8% on the first day post-contact, although the percentage of the K292 declined gradually over time (Figure 4B). In 3/4 respiratory droplet contact ferrets, we detected the mutant K292 genotype in the nasal washes (Figure 4C). Specifically, 100% of K292 genotype was detected in respiratory droplet contact 3 on days 2 and 3 post contact, demonstrating that the ability of the R292K mutant in conferring respiratory droplet transmission in ferrets. An increasing percentage of the wild-type R292 genotype was detected subsequently in this animal. Overall, the results suggest that the R292K mutant may transmit via direct contact or respiratory droplet contact routes but the mutation cannot be stably maintained in vivo while in competition with the wild-type virus.
Genotyping assay using ferret nasal washes suggests that the wild-type virus has greater replication fitness over the NA-R292K mutant in the upper respiratory tract. To monitor viral fitness of the mutant K292 genotype throughout the respiratory tract, we further collected respiratory tissues on day 5 post-inoculation (day 4 post-contact) from donor, direct contact, and respiratory droplet contact ferrets for virus titration and genotyping. Transmission of the MUT-6 virus to the 2 direct contact ferrets was confirmed by detecting viruses in the nasal washes on day 2 and day 3 post-contact, respectively. However, transmission to respiratory droplet contact ferret can only be confirmed in 1 of 2 respiratory droplet contact ferrets on day 3 post-contact. In donor ferrets inoculated with the MUT-6 virus, the H7N9 virus can be detected throughout the whole respiratory tract by virus titration (Table 2). Interestingly, immunohistochemistry detected virus antigens in the ferret submucosal glands at the bronchus. This observation was previously reported from ferrets inoculated with swine or pandemic H1N1 influenza viruses [27]. The wild-type R292 genotype gain dominance over the mutant K292 genotype in the majority of the donors' respiratory tissues on day 5 post-inoculation, although a significant percentage of the mutant K292 genotype can still be detected in the lung lobes of one donor. In direct contact ferrets infected by the MUT-6 virus, the H7N9 virus can be detected in different respiratory tissues at comparable titers to that of the inoculated donor ferrets (Table 2). The wild-type R292 genotype dominated in the nasal turbinate; however, a significant amount of the mutant K292 genotype can be detected in the lungs for both direct contact ferrets. In the respiratory droplet contact ferret infected by the MUT-6 virus, the H7N9 virus can only be detected in the nasal turbinate and 1 of 2 lung lobes by virus titration, suggesting these sites could be the initial sites of virus replication after airborne transmission (Table 2). The wild-type R292 genotype dominated at both locations. Overall, we observed a good correlation between the genotype detected in the ferret nasal washes and the genotype detected in the ferret nasal turbinate. The wild-type R292 genotype gain dominance over the mutant K292 genotype in the upper respiratory tract, whereas a significant percentage of the mutant K292 genotype can still be detected in the lung lobes of inoculated and infected direct contact ferrets. The detection of a significant percentage of NA-R292K mutation in the lung lobes suggests that the lung tissue may pose a lower selection pressure for the mutant virus while compared to the upper respiratory tract.
Table 2.
Virus Titers and R292/ K292 Genotypes in the Upper and Lower Respiratory Tract of Ferrets Inoculated or Infected With the A/Shanghai/1/2013 NA-R292K Mutant Virus
| Nasal Washa |
Nasal Turbinateb |
Trachea (Upper)b |
Trachea (Middle)b |
Right Upper Lung Lobeb |
Left Lower Lung Lobeb |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Virus Titerc | % K292 (%R292) | Virus Titerc | % K292 (%R292) | Virus Titerc | % K292 (%R292) | Virus Titerc | % K292 (%R292) | Virus Titerc | % K292 (%R292) | Virus Titerc | % K292 (%R292) | |
| Donor 5 | 6.57 | 11.64% (88.36%) | 6.46 | 21.52% (78.48%) | 4.79 | 0% (100%) | 4.71 | 0% (100%) | 5.79 | 57.69% (42.31%) | 4.58 | 33.59% (66.41%) |
| Donor 6 | 6.37 | 3.95% (96.05%) | 6.87 | 4.49% (95.51%) | 5.21 | 10.60% (89.40%) | 4.21 | 0% (100%) | 8.29 | 3.31% (96.69%) | 7.14 | 3.34% (96.66%) |
| Direct contact 5 | 6.96 | 0.06% (99.94%) | 6.74 | 3.55% (96.45%) | 4.62 | 53.75% (46.25%) | 3.46 | 0% (100%) | 4.96 | 0% (100%) | 4.79 | 99.85% (0.15%) |
| Direct contact 6 | 6.21 | 0.27% (99.73%) | 6.69 | 2.18% (97.82%) | 3.07 | 0% (100%) | 2.37 | 0.23% (99.77%) | 5.62 | 48.17% (51.83%) | 7.21 | 1.16% (98.84%) |
| Respiratory droplet contact 5 | 5.71 | 0% (100%) | 6.71 | 2.39% (97.61%) | <d | …e | <d | …e | <d | 0% (100%) | 3.84 | 0% (100%) |
| Respiratory droplet contact 6 | <d | …e | <d | …e | <d | …e | <d | …e | <d | …e | <d | …e |
Abbreviations: MDCK, Madin-Darby canine kidney; PCR, polymerase chain reaction; TCID50, 50% tissue culture infectious dose.
a Ferret nasal washes were collected on day 4 post-inoculation (day 3 post-contact).
b Tissues from ferret upper and lower respiratory tracts were collected on day 5 post-inoculation (day 4 post-contact).
c Virus titers were determined in MDCK cells and are expressed as log10 TCID50/mL.
d Below the detection limit of 1.79 log10 TCID50/mL by TCID50 assay.
e Below the detection limit of 10 copies of influenza M gene by quantitative real-time PCR assay.
DISCUSSION
We report here that the NA inhibitor-resistant H7N9 virus with an NA-R292K mutation may transmit at comparable efficiency as the wild-type virus in the ferret model; however, the mutant K292 genotype was outcompeted by the wild-type R292 genotype in upper respiratory tract of inoculated donors or infected contact ferrets. The compromised fitness of the NA-R292K mutant virus in vivo could be a result of decreased NA enzyme activity in the H7N9 virus [19–21] as has been demonstrated previously using seasonal H3N2 influenza virus [24]. Dominance of the wild-type R292 genotype over the K292 genotype was reported from donor ferrets co-infected with H3N2 seasonal influenza containing mixtures of wild-type and the NA-R292K mutant viruses [24]. Furthermore, only the wild-type R292 genotype was transmitted to direct contact ferrets co-housed with donors inoculated with mixtures of the wild-type and the NA-R292K mutant H3N2 viruses [24]. Similarly, we observed that the K292 genotype was gradually outgrown by the wild-type R292 genotype in the nasal washes of donor ferrets inoculated with the plaque-purified A/Shanghai/1/2013 (H7N9) NA-R292K mutant virus. However, in contrast to H3N2 seasonal influenza virus, the plaque-purified A/Shanghai/1/2013 (H7N9) NA-R292K mutant virus was transmissible to naive direct contact or respiratory droplet contact ferrets as the K292 genotype can be detected early in the nasal washes. The mutant K292 genotype remained dominant in 1 respiratory droplet contact ferret on day 5 post-contact further supported the transmission potential of the NA-R292K mutant virus (Figure 3). Overall, our results demonstrated the transmission potential of the NA inhibitor-resistant A/Shanghai/1/2013 NA-R292K mutant virus in ferrets, a unique trait not seen previously with seasonal H3N2 viruses carrying the R292K mutation. However, the wild-type R292 genotype gain dominance in the majority of the ferret respiratory tissues, which indicated the competitive fitness loss for the R292K mutant virus.
Although the wild-type R292 genotype rapidly gain dominance in the nasal washes or in the upper respiratory tract of ferrets inoculated or infected with the plaque-purified R292K mutant virus, the detection of a significant percentage of the mutant K292 genotype in the lung lobes suggests a lower selection pressure for the NA-R292K mutant in the lungs. Comparing to the trachea or bronchus, the lung parenchyma does not contain submucosal glands that secrete mucus rich in sialylated glycoproteins. It is not clear if the mucus layer poses a higher selection pressure for the NA-R292K mutant virus, which possess approximately 25% of the NA activity to that of the wild-type virus [19].
The fitness of NA inhibitor-resistant H7N9 virus has been characterized in vitro [19, 20], as well as in mice and guinea pigs [20, 26]. Plaque-purified wild-type and NA-R292K variants derived from human H7N9 isolates—A/Shanghai/1/2013 and A/Taiwan/1/2013—showed comparable pathogenicity in BALB/c mice, although additional HA mutations were identified in the plaque-purified NA-R292K mutant viruses [26]. Recombinant reassortant H7N9 virus with and without the R292K mutation showed comparable lethality in the BALB/c mouse model (50% mouse lethal dose at 32 and 42 PFU, respectively) and replicated to comparable titers in the mouse lungs. The recombinant reassortant H7N9 virus with and without the R292K mutation were transmitted to 2/4 and 1/4 respiratory droplet contact guinea pigs. Although the H7N9 virus with the NA-R292K mutation may show comparable virulence and transmissibility as the wild-type virus, monitoring the R/K genotype during the course of infection clearly demonstrated the compromised viral fitness of the R292K mutant in competition with the wild-type virus in the ferret model. Our study applied the A/Shanghai/1/2013 virus, which differed by 7 amino acids in the HA1 compared to the A/Shanghai/2/2013-like viruses. Further studies are required to address the competitive fitness of the NA-R292K mutants using the A/Shanghai/2/2013-like viruses in vivo.
Notes
Acknowledgments. This work was supported by the Area of Excellence Scheme of the University Grants Committee (AoE/M-12/06), Hong Kong SAR and contract HHSN27220140006C from the National Institute of Allergy and Infectious Disease, National Institutes of Health, USA. The authors thank Dr Yuelong Shu at Chinese Center for Disease Control and Prevention for providing the A/Shanghai/1/2013 virus, the Laboratory Animal Unit at The University of Hong Kong for the animal experiment support, and Michael Liman for the technical support in the BSL3 laboratory.
Financial support. This work was supported by the Area of Excellence Scheme of the University Grants Committee (AoE/M-12/06), Hong Kong SAR and contract HHSN27220140006C from the National Institute of Allergy and Infectious Disease, National Institutes of Health, USA.
Potential conflicts of interest. B. J. C. and J. S. M. P. have consulted for Crucell NV. B. J. C. reports receipt of research funding from Sanofi Pasteur and MedImmune Inc. H. L. Y. reports receipt of research funding from Celltrion and Visterra. All other authors report no potential conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Cowling BJ, Jin L, Lau EH, et al. Comparative epidemiology of human infections with avian influenza A H7N9 and H5N1 viruses in China: a population-based study of laboratory-confirmed cases. Lancet. 2013;382:129–37. doi: 10.1016/S0140-6736(13)61171-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang C, Yu H, Horby PW, et al. Comparison of patients hospitalized with influenza A subtypes H7N9, H5N1, and 2009 pandemic H1N1. Clin Infect Dis. 2014;58:1095–103. doi: 10.1093/cid/ciu053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yu H, Cowling BJ, Feng L, et al. Human infection with avian influenza A H7N9 virus: an assessment of clinical severity. Lancet. 2013;382:138–45. doi: 10.1016/S0140-6736(13)61207-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chan MC, Chan RW, Chan LL, et al. Tropism and innate host responses of a novel avian influenza A H7N9 virus: an analysis of ex-vivo and in-vitro cultures of the human respiratory tract. Lancet Respir Med. 2013;1:534–42. doi: 10.1016/S2213-2600(13)70138-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Riel D, Leijten LM, de Graaf M, et al. Novel avian-origin influenza A(H7N9) virus attaches to epithelium in both upper and lower respiratory tract of humans. Am J Pathol. 2013;183:1137–43. doi: 10.1016/j.ajpath.2013.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Belser JA, Gustin KM, Pearce MB, et al. Pathogenesis and transmission of avian influenza A(H7N9) virus in ferrets and mice. Nature. 2013;501:556–9. doi: 10.1038/nature12391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Richard M, Schrauwen EJ, de Graaf M, et al. Limited airborne transmission of H7N9 influenza A virus between ferrets. Nature. 2013;501:560–3. doi: 10.1038/nature12476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Watanabe T, Kiso M, Fukuyama S, et al. Characterization of H7N9 influenza A viruses isolated from humans. Nature. 2013;501:551–5. doi: 10.1038/nature12392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xu L, Bao L, Deng W, et al. Novel avian-origin human influenza A(H7N9) can be transmitted between ferrets via respiratory droplets. J Infect Dis. 2014;209:551–6. doi: 10.1093/infdis/jit474. [DOI] [PubMed] [Google Scholar]
- 10.Zhang Q, Shi J, Deng G, et al. H7N9 influenza viruses are transmissible in ferrets by respiratory droplet. Science. 2013;341:410–4. doi: 10.1126/science.1240532. [DOI] [PubMed] [Google Scholar]
- 11.Zhu H, Wang D, Kelvin DJ, et al. Infectivity, transmission, and pathology of human-isolated H7N9 influenza virus in ferrets and pigs. Science. 2013;341:183–6. doi: 10.1126/science.1239844. [DOI] [PubMed] [Google Scholar]
- 12.Gabbard JD, Dlugolenski D, Van Riel D, et al. Novel H7N9 influenza virus shows low infectious dose, high growth rate, and efficient contact transmission in the guinea pig model. J Virol. 2014;88:1502–12. doi: 10.1128/JVI.02959-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maines TR, Chen LM, Matsuoka Y, et al. Lack of transmission of H5N1 avian-human reassortant influenza viruses in a ferret model. Proc Natl Acad Sci U S A. 2006;103:12121–6. doi: 10.1073/pnas.0605134103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Osterholm MT, Ballering KS, Kelley NS. Major challenges in providing an effective and timely pandemic vaccine for influenza A(H7N9) JAMA. 2013;309:2557–8. doi: 10.1001/jama.2013.6589. [DOI] [PubMed] [Google Scholar]
- 15.Gao R, Cao B, Hu Y, et al. Human infection with a novel avian-origin influenza A(H7N9) virus. N Engl J Med. 2013;368:1888–97. doi: 10.1056/NEJMoa1304459. [DOI] [PubMed] [Google Scholar]
- 16.Hu Y, Lu S, Song Z, et al. Association between adverse clinical outcome in human disease caused by novel influenza A H7N9 virus and sustained viral shedding and emergence of antiviral resistance. Lancet. 2013;381:2273–9. doi: 10.1016/S0140-6736(13)61125-3. [DOI] [PubMed] [Google Scholar]
- 17.Lin PH, Chao TL, Kuo SW, et al. Virological, serological, and antiviral studies in an imported human case of avian influenza A(H7N9) virus in Taiwan. Clin Infect Dis. 2014;58:242–6. doi: 10.1093/cid/cit638. [DOI] [PubMed] [Google Scholar]
- 18.Wang W, Song Z, Guan W, et al. PCR for detection of oseltamivir resistance mutation in influenza A(H7N9) virus. Emerg Infect Dis. 2014;20:847–9. doi: 10.3201/eid2005.131364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yen HL, McKimm-Breschkin JL, Choy KT, et al. Resistance to neuraminidase inhibitors conferred by an R292K mutation in a human influenza virus H7N9 isolate can be masked by a mixed R/K viral population. MBio. 2013;4:pii:e00396–13. doi: 10.1128/mBio.00396-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hai R, Schmolke M, Leyva-Grado VH, et al. Influenza A(H7N9) virus gains neuraminidase inhibitor resistance without loss of in vivo virulence or transmissibility. Nat Commun. 2013;4:2854. doi: 10.1038/ncomms3854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sleeman K, Guo Z, Barnes J, Shaw M, Stevens J, Gubareva LV. R292K substitution and drug susceptibility of influenza A(H7N9) viruses. Emerg Infect Dis. 2013;19:1521–4. doi: 10.3201/eid1909.130724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dharan NJ, Gubareva LV, Meyer JJ, et al. Infections with oseltamivir-resistant influenza A(H1N1) virus in the United States. JAMA. 2009;301:1034–41. doi: 10.1001/jama.2009.294. [DOI] [PubMed] [Google Scholar]
- 23.Herlocher ML, Carr J, Ives J, et al. Influenza virus carrying an R292K mutation in the neuraminidase gene is not transmitted in ferrets. Antiviral Res. 2002;54:99–111. doi: 10.1016/s0166-3542(01)00214-5. [DOI] [PubMed] [Google Scholar]
- 24.Hurt AC, Nor'e SS, McCaw JM, et al. Assessing the viral fitness of oseltamivir-resistant influenza viruses in ferrets, using a competitive-mixtures model. J Virol. 2010;84:9427–38. doi: 10.1128/JVI.00373-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yen HL, Herlocher LM, Hoffmann E, et al. Neuraminidase inhibitor-resistant influenza viruses may differ substantially in fitness and transmissibility. Antimicrob Agents Chemother. 2005;49:4075–84. doi: 10.1128/AAC.49.10.4075-4084.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marjuki H, Mishin VP, Chesnokov AP, et al. An investigational antiviral drug, DAS181, effectively inhibits replication of zoonotic influenza A virus subtype H7N9 and protects mice from lethality. J Infect Dis. 2014;210:435–40. doi: 10.1093/infdis/jiu105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yen HL, Liang CH, Wu CY, et al. Hemagglutinin-neuraminidase balance confers respiratory-droplet transmissibility of the pandemic H1N1 influenza virus in ferrets. Proc Natl Acad Sci U S A. 2011;108:14264–9. doi: 10.1073/pnas.1111000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nicholls JM, Wong LP, Chan RW, et al. Detection of highly pathogenic influenza and pandemic influenza virus in formalin fixed tissues by immunohistochemical methods. J Virol Methods. 2012;179:409–13. doi: 10.1016/j.jviromet.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 29.Reed LJ, Muench H. A simple method of estimating fifty percent endpoints. Am J Hyg. 1938;27:493–7. [Google Scholar]
- 30.Hoffmann E, Stech J, Guan Y, Webster RG, Perez DR. Universal primer set for the full-length amplification of all influenza A viruses. Arch Virol. 2001;146:2275–89. doi: 10.1007/s007050170002. [DOI] [PubMed] [Google Scholar]