Abstract
The aim of the present study was to analyse the usefulness of the 6-20 rating of perceived exertion (RPE) scale for prescribing and self-regulating high-intensity interval training (HIT) in young individuals. Eight healthy young subjects (age = 27.5±6.7 years) performed maximal graded exercise testing to determine their maximal and reserve heart rate (HR). Subjects then performed two HIT sessions (20 min on a treadmill) prescribed and regulated by their HR (HR: 1 min at 50% alternated with 1 min at 85% of reserve HR) or RPE (RPE: 1 minute at the 9-11 level [very light-fairly light] alternated with 1 minute at the 15-17 level [hard-very hard]) in random order. HR response and walking/running speed during the 20 min of exercise were compared between sessions. No significant difference between sessions was observed in HR during low- (HR: 135±15 bpm; RPE: 138±20 bpm) and high-intensity intervals (HR: 168±15 bpm; RPE: 170±18 bpm). Walking/running speed during low- (HR: 5.7±1.2 km · h−1; RPE: 5.7±1.3 km · h−1) and high-intensity intervals (HR: 7.8±1.9 km · h−1; RPE: 8.2±1.7 km · h−1) was also not different between sessions. No significant differences were observed in HR response and walking/running speed between HIT sessions prescribed and regulated by HR or RPE. This finding suggests that the 6-20 RPE scale may be a useful tool for prescribing and self-regulating HIT in young subjects.
Keywords: exercise prescription, heart rate, high-intensity interval training, rating of perceived exertion
INTRODUCTION
It is well established that there is an association between regular aerobic exercise or intentional physical activity (performed in addition to the usual daily living activities) and reduced risk of cardiovascular disease and premature mortality in men and women [1–7]. Some of these studies suggest that vigorous-intensity physical activity is more effective than moderate-intensity physical activity for reducing cardiovascular disease and premature mortality, independent of its duration, frequency and energy expenditure [1, 3–7].
The role of physical activity intensity for its health-related benefits has been confirmed by recent interventional studies with high-intensity interval training (HIT). The studies have shown that short-term (≤ 16 weeks) HIT is superior to continuous moderate-intensity exercise (CME) for improving cardiorespiratory fitness [8–12] and other cardiometabolic biomarkers such as endothelial function and its markers [8, 11], blood lipoprotein and glucose [11], insulin sensitivity and fasting insulin [11, 13], markers of sympathetic activity [8, 9], arterial stiffness [8, 14], and muscle oxidative capacity [11]. These greater improvements have occurred in both healthy adults [8, 9, 13] and subjects with chronic diseases [10–12, 14, 15]. Moreover, several benefits of HIT have been shown to occur after just 2 weeks (6 sessions) of training [16, 17].
Although HIT models that involve maximal efforts have been used [18, 19], we [8, 9, 14] and others [10–12, 16, 17] have used HIT models that are more suitable for healthy sedentary and special populations (i.e. persons with cardiovascular or metabolic disease) and do not require any specialized ergometer. These HIT models consist of several bouts of high-intensity submaximal exercise (∼85% to 95% of maximal heart rate [HRMAX] or oxygen consumption [VO2MAX], or ∼80% to 90% of HRRESERVE) lasting 1 to 4 min interspersed with intervals of rest or active recovery [20]. The prescription of this type of training is based on HR, VO2 or ventilatory threshold response during cardiopulmonary exercise testing [8–12, 14, 16, 17], which requires expensive equipment and has measurements (VO2 or ventilatory thresholds) dependent on calibration procedures before testing [21, 22]. These limitations may reduce subjects’ access to exercise testing, and consequently access to HIT.
Rating of perceived exertion (RPE) is a simple and inexpensive measure that is associated with HR, VO2, and lactate and ventilatory thresholds [23–27]. Furthermore, the association of RPE with exercise intensity appears to remain stable regardless of training and health status [25, 27–29] and is sensitive to training-induced threshold changes [26]. These advantages make the RPE scale an attractive option for exercise prescription and self-regulation. In this regard, previous studies support the usefulness of RPE for prescribing and self-regulating CME in different populations [30–32]. Moreover, although the association between RPE and HR/blood lactate during an HIT session was previously reported [24], the usefulness of the RPE scale [33] to prescribe and self-regulate HIT has not been studied.
Considering the above-mentioned greater HIT health-related benefits, the disadvantages of methods commonly used to prescribe HIT, and the convenience of using RPE, studies in this field are welcome. Thus, the purpose of the present study was to analyse the usefulness of the RPE scale [33] for prescribing and self-regulating HIT by comparing HR response and exercise intensity (walking/running speed) during a HIT session prescribed and regulated by HRRESERVE or RPE. We hypothesized that the HR response and exercise intensity would be similar between sessions, which would support the usefulness of the RPE scale for prescribing and self-regulating HIT in young sedentary subjects.
MATERIALS AND METHODS
Population and study design
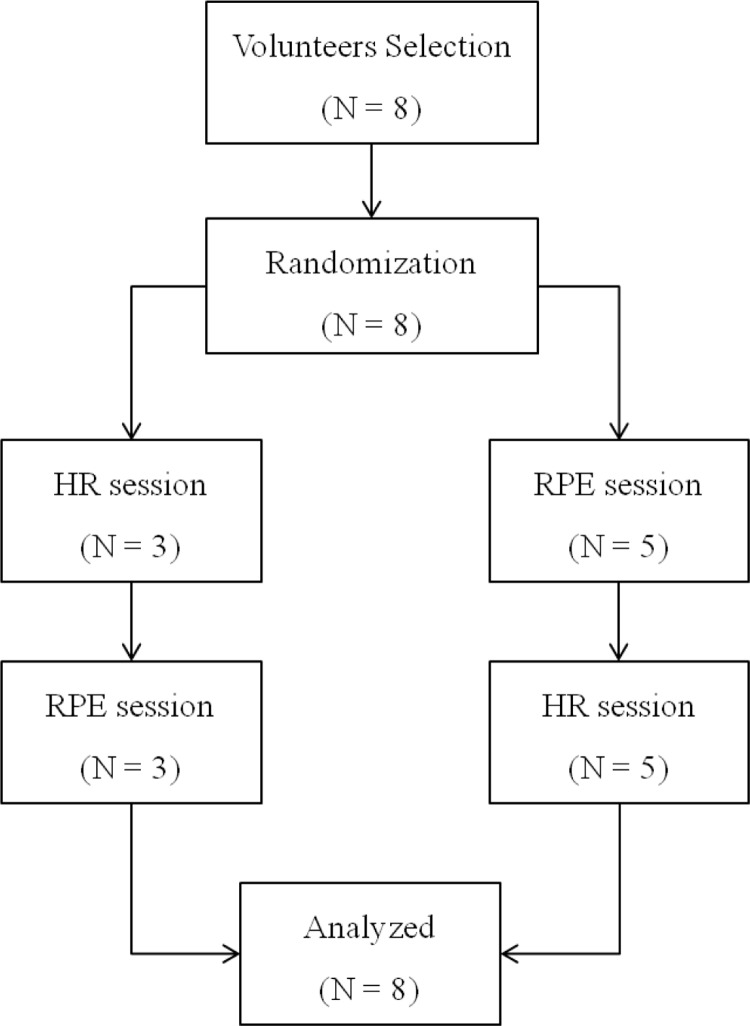
We studied 8 healthy young college subjects (5 women). A structured history, medical record review and physical evaluation were performed before study participation to document symptoms, history of chronic diseases, current medication, cardiac risk factors, and cardiac events and procedures. Subjects with musculoskeletal limitations to physical exercise, uncontrolled cardiovascular or metabolic disease, insulin-dependent diabetes, chronic psychological disorders, cardiac disease or taking any drug that could potentially influence cardiovascular response to exercise were excluded from the study. All volunteers were physically inactive (no involvement in regular physical activity or exercise programme during the previous 6 months) and had blood pressure below 130/80 mmHg (measures on two different occasions in triplicate at 2-minute intervals). Participants were then referred for maximal graded exercise testing (GXT) to determine HR dynamics. After GXT, volunteers were randomized one by one to a HIT session prescribed and regulated by HRRESERVE or RPE response. All volunteers performed the two HIT sessions between 3 and 7 days after the randomization, and there was an interval of at least 2 days between HIT sessions (Figure 1). HR and exercise intensity (walking/running speed) were collected throughout the 20 min of exercise and were compared between sessions. This study was approved by the ethics committee board at our institution. All volunteers read a detailed description of the protocol and provided their written informed consent. The characteristics of the subjects included in the study are summarized in Table 1.
FIG. 1.
Study design.
Note: HR: heart rate. RPE: rating of perceived exertion.
TABLE 1.
Subjects characteristics and graded exercise testing parameters.
| Variable (N = 8) | Mean | SD |
|---|---|---|
| Age (years) | 27.5 | 6.7 |
| Weight (kg) | 62.5 | 11.3 |
| Body Mass Index (kg·m−2) | 22.8 | 3.4 |
| Waist Circumference (cm) | 81.5 | 10.9 |
| Systolic Blood Pressure (mmHg) | 107 | 14 |
| Diastolic Blood Pressure (mmHg) | 74 | 5 |
| Exercise duration (min) | 10.2 | 1.5 |
| Resting Heart Rate (bpm) | 71.5 | 3.1 |
| Maximal Heart Rate (bpm) | 192.4 | 6.5 |
| % of Maximal Heart Rate Predicted (%) | 102 | 5.1 |
| Maximal Speed (km·h−2) | 11.1 | 1.2 |
| Rating of Perceived Exertion | 19.1 | 0.8 |
Graded exercise testing (GXT)
The volunteers performed a maximal, symptom-limited treadmill test (between 1600 and 1800 hours) using a Heck-modified protocol at controlled room temperature (20-23°C) before participation in HIT sessions as previously described [34]. Cardiac rhythm was continuously monitored by electrocardiogram in 12 derivations and recorded for 10 s at the end of rest, end of each warm-up and exercise stage, and at the end of each minute of the recovery phase. Subjects were told to avoid caffeine and alcoholic beverages for 24 hours and to have a light meal up to 2 hours before the GXT. Age-predicted maximal HR was determined using a standardized equation [35].
HIT sessions
The two HIT sessions (between 1600 and 1800 hours) were performed at controlled room temperature (20-23°C) and consisted of 20-min HIT controlled and regulated by HRRESERVE or RPE. Subjects were told to avoid caffeine and alcoholic beverages for 24 hours and to have a light meal up to 2 hours before each HIT session. The intensity of the HIT session prescribed and regulated by HRRESERVE was determined according to the HR dynamics during the GXT, and consisted of 20 min on a treadmill with intensity alternating between ∼50% (1 min) and ∼85% (1 min) of HRRESERVE [36]. The intensity of the HIT session prescribed and regulated by RPE was based on the association between RPE and HRRESERVE [37], and consisted of 20 min on a treadmill with intensity alternating 9-11 (1 min) and 15-17 (1 min) in the 15-point RPE scale [33]. The same 5 min warm-up and cool-down were performed and the individual's HR was monitored (Polar S810i, Polar Eletro, Kempele, Finland) throughout the two HIT sessions. The treadmill speed of the HRRESERVE HIT session was regulated by an exercise specialist according to the volunteers’ HR response during exercise. The treadmill speed of the RPE session was self-regulated by the volunteer according to the RPE perception during exercise. All volunteers were blinded to the treadmill speed during both the HR and the RPE session. The mean HR during the last 10 s of each interval and the speed at the end of the interval were used for comparisons between HIT sessions.
Statistical methods
All data are reported as mean ± SD. The statistical program SPSS 12.0 for Windows (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. The Kolmogorov–Smirnov test was applied to ensure a Gaussian distribution of the results. Paired Student's t test was used to analyse the differences between interventions (HRRESERVE vs. RPE). The significance level was set at p < 0.05.
RESULTS
All subjects achieved at least 95% of age-predicted maximal HR (102 ± 5.1%) and 18 points (19.1 ± 0.8) on the RPE scale during GXT (Table 1), suggesting that tests were maximal [38]. The 50% and 85% of HRRESERVE calculated for the training session were 131.9 ± 3.1 bpm and 174.2 ± 5.3 bpm, respectively. All volunteers performed the two HIT sessions, whereas three of them performed the first HIT session prescribed by HRRESERVE (Figure 1).
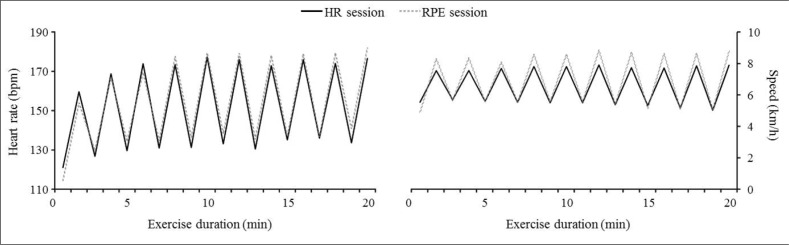
No significant differences in HR were observed between HIT sessions prescribed and regulated by HRRESERVE or RPE (Figure 2). HR values at low-intensity intervals (∼50% of HRRESERVE or 9-11 points on the RPE scale) were 135 ± 15 bpm and 138 ± 20 bpm (P = 0.36), whereas HR values at high-intensity intervals (∼85% of HRRESERVE or 15-17 points on the RPE scale) were 168 ± 15 bpm and 170 ± 18 bpm (P = 0.38) during HIT sessions prescribed and regulated by HRRESERVE or RPE, respectively.
FIG. 2.
Heart rate (left panel) and walking/running speed (right panel) during HIT session prescribed and regulated by heart rate (HR session) or rating of perceived exertion (RPE session) response. No significant differences were observed between sessions.
No significant differences in walking/running speed were also observed between HIT sessions prescribed and regulated by HRRESERVE or RPE (Figure 2). Walking speed at low-intensity intervals (∼50% of HRRESERVE or 9-11 points on the RPE scale) were 5.7 ± 1.2 km · h−1 and 5.7 ± 1.3 km · h−1 (P > 0.81), whereas running speed at high-intensity intervals (∼85% of HRRESERVE or 15-17 points on the RPE scale) were 7.8 ± 1.9 km · h−1 and 8.2 ± 1.7 km · h−1 (P = 0.25) during HIT sessions prescribed and regulated by HRRESERVE or RPE, respectively.
DISCUSSION
To the best of our knowledge, this is a pioneering study in analysing the usefulness of the 6-20 RPE scale [33] for prescribing and self-regulating HIT in young sedentary individuals. The data analyses showed no significant differences in HR response and walking/running speed between HIT sessions prescribed and regulated by HR or RPE. This finding suggests that the RPE scale is a simple, inexpensive and useful tool for prescribing and self-regulating HIT in young subjects.
Independent of the method of exercise training, the prescription of adequate intensity is crucial to obtain both an acceptable training stimulus and reasonable control of the exercise-related risk [37]. Although HIT models that involve maximal efforts have been used [18, 19], most studies with healthy sedentary individuals and populations with chronic diseases have used HIT models with bouts of high-intensity submaximal exercise (∼85% to 95% of maximal heart rate [HRMAX] or oxygen consumption [VO2MAX], or ∼80% to 90% of HRRESERVE), with the HR response being the tool used to guide the exercise session [8–12, 16, 17, 24]. However, the use of HR to guide HIT has limitations that include the use of cardiopulmonary testing to prescribe exercise intensity, which requires expensive equipment and has measurements (VO2 or ventilatory thresholds) dependent on calibration procedures [21, 22] and the use of HR monitors to regulate exercise intensity, devices that are not accessible to the general population, especially in developing countries. Although digitalis palpation of superficial arteries may be an alternative and less expensive tool to the use of HR monitors, most individuals have shown poor ability to self-monitor and self-regulate their exercise intensity by this method, which has partially contributed to the high rate of dropout from exercise programmes [39]. In contrast, the lack of difference in HR and walking/running speed during HIT prescribed and regulated by HR or RPE observed in the present study makes the RPE scale an alternative and attractive option to prescribe and self-regulate HIT in healthy individuals, and is corroborated by its association with HR, VO2, and lactate and ventilatory thresholds during exercise testing [23–27].
The usefulness of RPE for prescribing and self-regulating CME in different populations has been shown in previous studies [30–32]. For example, in a study with 44 chronic heart failure patients, the RPE scale proved to be useful for prescribing and self-regulating land and water based CME [30]. In another study analysing HR, blood lactate and speed during treadmill and field running at three different intensities monitored and regulated by the RPE scale showed that this tool is effective and reproducible for monitoring and regulating steady-state running in physically active individuals [31]. The results of the present study are consistent with the above-mentioned studies with CME and confirm our hypothesis that the RPE scale may be a useful tool for prescribing and self-regulating HIT in young sedentary subjects.
The body of evidence showing the fitness and health-related benefits of aerobic exercise training for adults is indisputable [1–7, 37]. Although HIT has been used for several decades by athletes and coaches to improve exercise performance [40], its ability to improve health-related variables in healthy subjects and in individuals with chronic diseases has recently generated new interest. In this context, we and others have shown that HIT is more effective than CME for improving endothelial function in healthy subjects [8] and individuals with metabolic syndrome [11] or chronic heart failure [12], for reducing arterial stiffness in hypertensive [14] and normotensive individuals at high risk for hypertension [8], for improving insulin sensitivity and fasting insulin in healthy [13] and metabolic syndrome subjects [11], for reversing left ventricular remodelling in heart failure patients [12], for improving markers of sympathetic activity in normotensive individuals at high risk for hypertension [8, 9], and for inducing fat loss and reducing central body fat (despite lower total energy expenditure during an exercise session) in healthy women [13]. In addition, the greater efficiency of HIT over CME in improving cardiorespiratory fitness in healthy [8, 9] and chronic disease populations [10–12] may have important implications for preventing premature mortality in the general population and in patients with cardiometabolic diseases [8, 10, 12], because out of all established risk factors, low cardiorespiratory fitness seems to be the strongest predictor of mortality [41].
In this context, the results of the present study may have important clinical implications. The lack of significant differences observed in HR response and walking/running speed between HIT sessions prescribed and regulated by HR or RPE suggests that RPE may be a useful tool for prescribing and self-regulating HIT. Given the high cost and low access of the methods commonly used to prescribe HIT [8–12, 14, 16, 17], and the above-mentioned higher health-related benefits of HIT, the use of the simple and inexpensive tool that is the RPE scale to prescribe and self-regulate HIT may increase access and adherence to this exercise modality and, consequently, increase benefits to the general population. In this context, future multicenter randomized controlled trials focused on analysing adherence and health-related benefits of RPE-prescribed and self-regulated HIT in healthy subjects and populations with chronic diseases are welcome.
The main limitations of the present study include its design, where the use of a single session of RPE-prescribed and self-regulated HIT does not allow one to state that the present results would persist after a long period of training. However, the initial step to evaluate the response to any exercise intervention is to analyse the acute responses that this intervention produces, and training studies may not be justified without demonstrating an efficient acute response first. Moreover, a number of studies have shown that RPE association with exercise intensity remains stable regardless of training and health status [25, 27–29] and is sensitive to training-induced threshold changes [26], suggesting that the results of the present study may persist after periods of training. Another limitation is that only sedentary, young and healthy subjects were studied, which does not guarantee similar results in older individuals or populations with chronic disease, mainly populations under use of medications that affect the cardiovascular and/or respiratory response to exercise. Future studies with these populations are thus necessary.
CONCLUSIONS
In summary, no significant differences were observed in HR response and walking/running speed between HIT sessions prescribed and regulated by HR or RPE in sedentary young subjects. This finding suggests that the 6-20 RPE scale may be a useful tool for prescribing and self-regulating HIT in this population.
Acknowledgements
Dr. Ciolac was funded by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP #2012/ 02409-0) and Fundação Nacional de Desenvolvimento do Ensino Superior Particular (FUNADESP # 5500261) during this project.
Conflict of interests
The authors declared no conflict of interests regarding the publication of this manuscript.
REFERENCES
- 1.Lee IM, Hsieh CC, Paffenbarger RS., Jr Exercise intensity and longevity in men: The Harvard Alumni Health Study. JAMA. 1995;273(15):1179–1184. [PubMed] [Google Scholar]
- 2.Lee IM, Rexrode KM, Cook NR, Manson JE, Buring JE. Physical activity and coronary heart disease in women: is „no pain, no gain” passe? JAMA. 2001;285(11):1447–1454. doi: 10.1001/jama.285.11.1447. [DOI] [PubMed] [Google Scholar]
- 3.Lee IM, Sesso HD, Oguma Y, Paffenbarger RS., Jr Relative intensity of physical activity and risk of coronary heart disease. Circulation. 2003;107(8):1110–1116. doi: 10.1161/01.cir.0000052626.63602.58. [DOI] [PubMed] [Google Scholar]
- 4.Slattery ML, Jacobs DR, Jr, Nichaman MZ. Leisure time physical activity and coronary heart disease death: The US Railroad Study. Circulation. 1989;79(2):304–311. doi: 10.1161/01.cir.79.2.304. [DOI] [PubMed] [Google Scholar]
- 5.Swain DP, Franklin BA. Comparison of cardioprotective benefits of vigorous versus moderate intensity aerobic exercise. Am J Cardiol. 2006;97(1):141–147. doi: 10.1016/j.amjcard.2005.07.130. [DOI] [PubMed] [Google Scholar]
- 6.Tanasescu M, Leitzmann MF, Rimm EB, Willett WC, Stampfer MJ, Hu FB. Exercise type and intensity in relation to coronary heart disease in men. JAMA. 2002;288(16):1994–2000. doi: 10.1001/jama.288.16.1994. [DOI] [PubMed] [Google Scholar]
- 7.Wisloff U, Nilsen TI, Droyvold WB, Morkved S, Slordahl SA, Vatten LJ. A single weekly bout of exercise may reduce cardiovascular mortality: how little pain for cardiac gain? ‚The HUNT study, Norway’. Eur J Cardiov Prev Rehabil. 2006;13(5):798–804. doi: 10.1097/01.hjr.0000216548.84560.ac. [DOI] [PubMed] [Google Scholar]
- 8.Ciolac EG, Bocchi EA, Bortolotto LA, Carvalho VO, Greve JMD, Guimaraes GV. Effects of high-intensity aerobic interval training vs. moderate exercise on hemodynamic, metabolic and neuro-humoral abnormalities of young normotensive women at high familial risk for hypertension. Hypert Res. 2010;33(8):836–843. doi: 10.1038/hr.2010.72. [DOI] [PubMed] [Google Scholar]
- 9.Ciolac EG, Bocchi EA, Greve JM, Guimaraes GV. Heart rate response to exercise and cardiorespiratory fitness of young women at high familial risk for hypertension: effects of interval vs continuous training. Eur J Cardiov Prev Rehabil. 2011;18(6):824–830. doi: 10.1177/1741826711398426. [DOI] [PubMed] [Google Scholar]
- 10.Rognmo O, Hetland E, Helgerud J, Hoff J, Slordahl SA. High intensity aerobic interval exercise is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary artery disease. Eur J Cardiov Prev Rehabil. 2004;11(3):216–222. doi: 10.1097/01.hjr.0000131677.96762.0c. [DOI] [PubMed] [Google Scholar]
- 11.Tjonna AE, Lee SJ, Rognmo O, Stølen TO, Bye A, Haram PM, Loennechen JP, Al-Share QY, Skogvoll E, Slørdahl SA, Kemi OJ, Najjar SM, Wisløff U. Aerobic interval training versus continuous moderate exercise as a treatment for the metabolic syndrome: A pilot study. Circulation. 2008;118(4):346–354. doi: 10.1161/CIRCULATIONAHA.108.772822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wisloff U, Stoylen A, Loennechen JP, Bruvold M, Rognmo Ø, Haram PM, Tjønna AE, Helgerud J, Slørdahl SA, Lee SJ, Videm V, Bye A, Smith GL, Najjar SM, Ellingsen Ø, Skjaerpe T. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: A randomized study. Circulation. 2007;115(24):3086–3094. doi: 10.1161/CIRCULATIONAHA.106.675041. [DOI] [PubMed] [Google Scholar]
- 13.Trapp EG, Chisholm DJ, Freund J, Boutcher SH. The effects of high-intensity intermittent exercise training on fat loss and fasting insulin levels of young women. Int J Obes. 2008;32(4):684–691. doi: 10.1038/sj.ijo.0803781. [DOI] [PubMed] [Google Scholar]
- 14.Guimaraes GV, Ciolac EG, Carvalho VO, D'Avila VM, Bortolotto LA, Bocchi EA. Effects of continuous vs. interval exercise training on blood pressure and arterial stiffness in treated hypertension. Hypert Res. 2010;33(6):627–632. doi: 10.1038/hr.2010.42. [DOI] [PubMed] [Google Scholar]
- 15.Beauchamp MK, Nonoyama M, Goldstein RS, Hill K, Dolmage TE, Mathur S, Brooks D. Interval versus continuous training in individuals with chronic obstructive pulmonary disease--a systematic review. Thorax. 2010;65(2):157–164. doi: 10.1136/thx.2009.123000. [DOI] [PubMed] [Google Scholar]
- 16.Earnest CP, Lupo M, Thibodaux J, Hollier C, Butitta B, Lejeune E, Johannsen NM, Gibala MJ, Church TS. Interval training in men at risk for insulin resistance. Int J Sports Med. 2013;34(4):355–363. doi: 10.1055/s-0032-1311594. [DOI] [PubMed] [Google Scholar]
- 17.Little JP, Gillen JB, Percival ME, Safdar A, Tarnopolsky MA, Punthakee Z, Jung ME, Gibala MJ. Low-volume high-intensity interval training reduces hyperglycemia and increases muscle mitochondrial capacity in patients with type 2 diabetes. J Appl Physiol. 2011;111(6):1554–1560. doi: 10.1152/japplphysiol.00921.2011. [DOI] [PubMed] [Google Scholar]
- 18.Gibala MJ, Little JP, van Essen M, Wilkin GP, Burgomaster KA, Safdar A, Raha S, Tarnopolsky MA. Short-term sprint interval versus traditional endurance training: similar initial adaptations in human skeletal muscle and exercise performance. J Physiol. 2006;575(3):901–911. doi: 10.1113/jphysiol.2006.112094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Richards JC, Johnson TK, Kuzma JN, Lonac MC, Schweder MM, Voyles WF, Bell C. Short-term sprint interval training increases insulin sensitivity in healthy adults but does not affect the thermogenic response to beta-adrenergic stimulation. J Physiol. 2010;588(15):2961–2972. doi: 10.1113/jphysiol.2010.189886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ciolac EG. High-intensity interval training and hypertension: maximizing the benefits of exercise? Am J Cardiov Dis. 2012;2(2):102–110. [PMC free article] [PubMed] [Google Scholar]
- 21.Atkinson G, Davison RC, Nevill AM. Performance characteristics of gas analysis systems: what we know and what we need to know. IntJ Sports Med. 2005;26:S2–S10. doi: 10.1055/s-2004-830505. [DOI] [PubMed] [Google Scholar]
- 22.Meyer T, Lucia A, Earnest CP, Kindermann W. A conceptual framework for performance diagnosis and training prescription from submaximal gas exchange parameters--theory and application. Int J Sports Med. 2005;26:S38–S48. doi: 10.1055/s-2004-830514. [DOI] [PubMed] [Google Scholar]
- 23.Green JM, Crews TR, Bosak AM, Peveler WW. Overall and differentiated ratings of perceived exertion at the respiratory compensation threshold: effects of gender and mode. Eur J Appl Physiol. 2003;89(5):445–450. doi: 10.1007/s00421-003-0869-4. [DOI] [PubMed] [Google Scholar]
- 24.Green JM, McLester JR, Crews TR, Wickwire PJ, Pritchett RC, Lomax RG. RPE association with lactate and heart rate during high-intensity interval cycling. Med Sci Sports Exerc. 2006;38(1):167–172. doi: 10.1249/01.mss.0000180359.98241.a2. [DOI] [PubMed] [Google Scholar]
- 25.Hetzler RK, Seip RL, Boutcher SH, Pierce E, Snead D, Weltman A. Effect of exercise modality on ratings of perceived exertion at various lactate concentrations. Med Sci Sports Exerc. 1991;23(1):88–92. [PubMed] [Google Scholar]
- 26.Hill DW, Cureton KJ, Grisham SC, Collins MA. Effect of training on the rating of perceived exertion at the ventilatory threshold. Eur J Appl Physiol. 1987;56(2):206–211. doi: 10.1007/BF00640645. [DOI] [PubMed] [Google Scholar]
- 27.Seip RL, Snead D, Pierce EF, Stein P, Weltman A. Perceptual responses and blood lactate concentration: Effect of training state. Med Sci Sports Exerc. 1991;23(1):80–87. [PubMed] [Google Scholar]
- 28.Demello JJ, Cureton KJ, Boineau RE, Singh MM. Ratings of perceived exertion at the lactate threshold in trained and untrained men and women. Med Sci Sports Exerc. 1987;19(4):354–362. [PubMed] [Google Scholar]
- 29.Kunitomi M, Takahashi K, Wada J, Suzuki H, Miyatake N, Ogawa S, Ohta S, Sugimoto H, Shikata K, Makino H. Re-evaluation of exercise prescription for Japanese type 2 diabetic patients by ventilatory threshold. Diabetes Res Clin Pr. 2000;50(2):109–115. doi: 10.1016/s0168-8227(00)00170-4. [DOI] [PubMed] [Google Scholar]
- 30.Carvalho VO, Bocchi EA, Guimares GV. The Borg scale as an important tool of self-monitoring and self-regulation of exercise prescription in heart failure patients during hydrotherapy - A randomized blinded controlled trial. Circulation J. 2009;73(10):1871–1876. doi: 10.1253/circj.cj-09-0333. [DOI] [PubMed] [Google Scholar]
- 31.Ceci R, Hassmen P. Self-monitored exercise at 3 different RPE intensities in treadmill vs field running. Med Sci Sports Exerc. 1991;23(6):732–738. [PubMed] [Google Scholar]
- 32.Chen MJ, Fan XT, Moe ST. Criterion-related validity of the Borg ratings of perceived exertion scale in healthy individuals: a meta-analysis. J Sport Sci. 2002;20(11):873–899. doi: 10.1080/026404102320761787. [DOI] [PubMed] [Google Scholar]
- 33.Borg GAV. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–381. [PubMed] [Google Scholar]
- 34.Ciolac EG, Greve JM. Exercise-induced improvements in cardiorespiratory fitness and heart rate response to exercise are impaired in overweight/obese postmenopausal women. Clinics. 2011;66(4):583–589. doi: 10.1590/S1807-59322011000400011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tanaka H, Monahan KD, Seals DR. Age-predicted maximal heart rate revisited. J Am Coll Cardiol. 2001;37(1):153–156. doi: 10.1016/s0735-1097(00)01054-8. [DOI] [PubMed] [Google Scholar]
- 36.Karvonen MJ, Kentala E, Mustala O. The effects of training on heart rate - a longitudinal study. Ann Med Exp Biol Fenn. 1957;35(3):307–315. [PubMed] [Google Scholar]
- 37.Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, Nieman DC, Swain DP, American College of Sports Medicine Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 38.Fletcher GF, Balady GJ, Amsterdam EA, Chaitman B, Eckel R, Fleg J, Froelicher VF, Leon AS, Piña IL, Rodney R, Simons-Morton DA, Williams MA, Bazzarre T. Exercise standards for testing and training: A statement for healthcare professionals from the American Heart Association. Circulation. 2001;104(14):1694–1740. doi: 10.1161/hc3901.095960. [DOI] [PubMed] [Google Scholar]
- 39.Ekkekakis P, Hall EE, Petruzzello SJ. Practical markers of the transition from aerobic to anaerobic metabolism during exercise: rationale and a case for affect-based exercise prescription. Prev Med. 2004;38(2):149–159. doi: 10.1016/j.ypmed.2003.09.038. [DOI] [PubMed] [Google Scholar]
- 40.Laursen PB, Jenkins DG. The scientific basis for high-intensity interval training - Optimising training programmes and maximising performance in highly trained endurance athletes. Sports Med. 2002;32(1):53–73. doi: 10.2165/00007256-200232010-00003. [DOI] [PubMed] [Google Scholar]
- 41.Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. New Engl J Med. 2002;346(11):793–801. doi: 10.1056/NEJMoa011858. [DOI] [PubMed] [Google Scholar]