Abstract
Background:
Spinal anaesthesia is the preferred technique to fix fracture of the femur. Extreme pain does not allow ideal positioning for this procedure. Intravenous fentanyl and femoral nerve block are commonly used techniques to reduce the pain during position for spinal anaesthesia however; results are conflicting regarding superiority of femoral nerve block over intravenous fentanyl.
Aims:
We conducted this study to compare the analgesic effect provided by femoral nerve block (FNB) and intra- venous (IV) fentanyl prior to positioning for central neuraxial block in patients undergoing surgery for femur fracture.
Patients and Methods:
In this randomized prospective study 60 patients scheduled for fracture femur operation under spinal were included. Patients were distributed in two groups through computer generated random numbers table; Femoral nerve block group (FNB) and Intravenous fentanyl group (FENT). In FNB group patients received FNB guided by a peripheral nerve stimulator (Stimuplex; B Braun, Melsungen, AG) 5 minutes prior to positioning. 20mL, 1.5% lidocaine with adrenaline (1:200,000) was injected incrementally after a negative aspiration test. Patients in the fentanyl group received injection fentanyl 1 μg/kg IV 5 mins prior to positioning. Spinal block was performed and pain scores before and during positioning were recorded. Statistical analysis was done with Sigmaplot version-10 computer software. Student t-test was applied to compare the means and P < 0.05 was taken as significant.
Results:
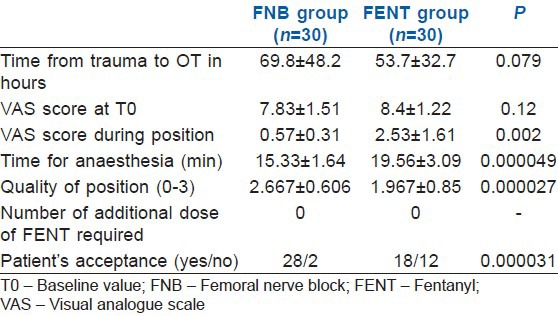
VAS during positioning in group FNB: 0.57 ± 0.31 versus FENT 2.53 ± 1.61 (P = 0.0020). Time to perform spinal anesthesia in group FNB: 15.33 ± 1.64 min versus FENT 19.56 ± 3.09 min (P = 0.000049). Quality of patient positioning for spinal anesthesia in group FNB 2.67± 0.606 versus FENT 1.967 ± 0.85 (P = 0.000027). Patient acceptance was less in group FENT (P = 0.000031).
Conclusion:
Femoral nerve block provides better analgesia, patient satisfaction and satisfactory positioning than IV fentanyl for position during spinal anaesthesia in patients of fracture femur.
Keywords: Anaesthesia, femoral nerve block, femur fracture, fentanyl, position for spinal, spinal
INTRODUCTION
Fracture of the femur is a common orthopaedic problem following trauma in patients of all ages and central neuraxial block such as spinal anaesthesia is the preferred technique for providing anaesthesia.[1] Correct positioning during central neuraxial block is the prerequisite for a successful procedure. However, limb immobility and extreme pain are the deterrents for an ideal positioning for this procedure. Various modalities like intravenous (IV) fentanyl (FENT), femoral nerve block (FNB) or fascia iliaca block with local anaesthetic have been advocated to reduce the pain pre-operatively and improve the positioning of these patients.[2,3] Results are conflicting regarding superiority of FNB on IV FENT. Previous studies have shown the superiority of the FNB as compared to the IV FENT.[4] However, recent studies have shown no benefit of FNB over IV FENT.[5] We conducted this study with the aim to compare the analgesic effect provided by FNB and IV FENT prior to positioning for central neuraxial block in patients undergoing surgery for femur fracture.
METHODS
Institutional approval and informed consent from the patient were taken prior to study. Patients of both sexes, 18–70 years, weight >50 kg, American Society of Anesthesiologists physical status I to III, scheduled for fracture femur operation under central neuraxial block, but unable to sit due to pain were included in the study. Patients who could sit comfortably refused for participation in the study or having any contraindication to spinal anaesthesia, FNB or use of local anaesthetic were excluded. Patients were distributed in two groups through computer generated random numbers table; FNB group and IV FENT group. Sample size was calculated based on an earlier study,[5] which showed in their pilot study that FNB was more effective to reduce pain, and the mean score was 2 in FNB group. Based on α =0.05, β =0.20 and considering a significant difference at mean difference of 2.2 in pain score, with standard deviation (SD) of 3.0, a sample size of 30 per group was required for one-tailed testing. Taking attrition at 10% due to conversion of technique (general anaesthesia), refusal on table, technical difficulties, total 68 patients were included (33 patients in each group). IV line was secured and fluid started, monitors attached and baseline parameters were recorded. In FNB group patients received FNB guided by a peripheral nerve stimulator (Stimuplex®; B Braun, Melsungen, AG, Germany) 5 min prior to positioning. FNB was performed by one of the two anaesthesiologists (AJ or SC). Entry point was infiltrated with 1 ml 1% lignocaine and then an insulated 50 mm 22 gauge needle (Stimuplex®; B Braun) was introduced 1 cm lateral to the femoral artery and 1.5 cm below the inguinal ligament. When a stimulating current at 0.3–0.5 mA elicited a quadriceps contraction 20 mL, 1.5% lignocaine with adrenaline (1:200,000) was injected (15 mL 2% lignocaine diluted with 5 ml distilled water) incrementally after a negative aspiration test. Patients in the FENT group received injection fentanyl 1 μg/kg IV 5 min prior to positioning. If any patient in either group reported pain scores ≥4 during positioning, IV fentanyl 0.5 μg/kg was given every 5 min until the pain score decreased to <4 or maximum dose of 3 μg/kg was given (whichever first); if pain score could not be achieved, patients were excluded from study. Thereafter a spinal block was performed in either the midline or paramedian approach at the L2/3 or L3/4 level, according to the anesthesiologist's decision. Pain scores before and during positioning were recorded. Pain assessment was done using visual analog scale (0 = no pain, 10 = maximal pain). Additional fentanyl requirement during positioning, time taken to achieve position and anaesthesiologist’ satisfaction with patient position maintained for spinal block (0 = not satisfactory, 1 = satisfactory, 2 = good, 3 = optimal) and patient satisfaction, e.g., like or dislike (yes or no) were also recorded. Vital parameters; heart rate (HR), mean arterial pressure (MAP) by non-invasive blood pressure and oxygen saturation (SpO2) were monitored. Statistical analysis was performed with SigmaPlot version-10 computer software. Parametric variables were described as mean ± SD; qualitative variables were described as number (percentage) and as median and range. Student's t-test, Chi-square test or Fisher exact test were used as appropriate to compare the two groups. P < 0.05 was considered as statistically significant.
RESULTS
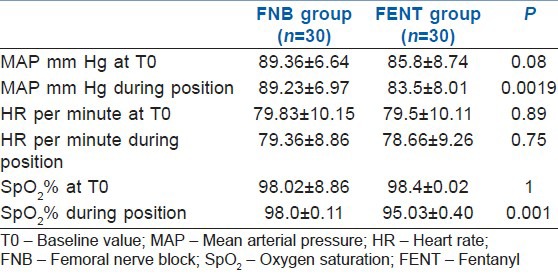
In two patients from each group, surgery was postponed due to infection at surgical site and change in surgical plan. One patient from each group was excluded due to refusal for spinal anaesthesia on table after initial consent. Therefore, six patients were subsequently excluded leaving 60 patients for final analysis. Demographic data and base line values for HRs, MAPs and type of surgery were comparable in both the groups [Tables 1 and 2]. There was no significant change noticed in HRs between two groups (P = 0.75); however, MAP was significantly lower in FENT group (P = 0.0019). Visual analog scale values during positioning (median ± SD) were lower in group FNB: 0.57 ± 0.31 versus FENT 2.53 ± 1.61 (P = 0.0020). Time to perform spinal anaesthesia (mean ± SD) was shorter in group FNB: 15.33 ± 1.64 min versus FENT 19.56 ± 3.09 min (P = 0.000049). Quality of patient positioning for spinal anesthesia) (median and SD) was higher in group FNB 2.67 ± 0.606 versus FENT 1.967 ± 0.85 (P = 0.000027). Patient acceptance was less in group FENT (P = 0.000031). SpO2 was significantly lower in FENT group (P = 0.001). However, no patient in both the groups had SpO2 <90% during the procedure [Table 2]. No patient required additional dose of fentanyl.
Table 1.
Demographic data
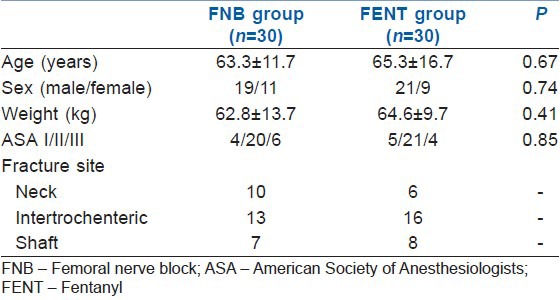
Table 2.
Vital clinical parameter before analgesia and during position
DISCUSSION
Spinal anaesthesia is universally accepted and preferred technique of anaesthesia for surgery of fracture femur.[1] This technique has many advantages over general anaesthesia like early mobility, less chances of deep vein thrombosis and mortality.[6,7] When considering the technique used to aid positioning patients for the spinal block, Sandby-Thomas et al.[1] reported that the most frequently used agents were midazolam, ketamine, and propofol. Alternative agents were fentanyl, remifentanil, morphine, nitrous oxide, and sevoflurane, whereas nerve blocks were infrequently used. Use of FNB to relieve pain from a fracture of the femur at various other situations[8,9] is well known and now, is being used for positioning during spinal anaesthesia.[2,4,5,10] In the present study visual analog scale values in FNB were significantly lower than fentanyl [Table 3]. Many other studies also reported significantly low pain scores with FNB compare to IV fentanyl.[2,10] Iamaroon et al. did not find any significant difference between FNB and fentanyl.[5] He used 0.3% bupivacaine for FNB and positioned the patients 15 min after block. The probable reason was the use of bupivacaine instead of lidocaine. The effect of lignocaine in FNB comes in 5 min[2,10] however; onset of analgesic effect of bupivacaine is variable and may take 25–30 min for full effect.[11,12]
Table 3.
VAS scores, performance time, quality of position and patient acceptance
The most important finding of our study was that femoral nerve blockade offered superior analgesia compared to IV fentanyl during position for spinal anaesthesia in cases of fracture femur. In addition, FNB was associated with greater patient satisfaction. Iamaroon et al.[5] used 0.5 μg/kg fentanyl as the initial dose and average additional dose of fentanyl in FENT group was 17.1 ± 18.4. The total doses required by IVfentanyl group are similar to our study. In our study, initial doses of FENT 1.0 μg/kg was given. We planned to give the additional dose with a 5 min interval because titration of the dose of fentanyl may reduce any serious side-effects, such as hypoventilation or apnea. However, no patient required additional dose possibly because, most of our patients were elderly [Table 1]. In addition in patients of FENT group drowsiness was observed which required more persons for holding the patient during positioning.
CONCLUSION
Femoral nerve block provides better analgesia, patient satisfaction, less time for anaesthesia and satisfactory positioning than IV fentanyl for central neuraxial block in patients undergoing surgery for femur fractures.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Sandby-Thomas M, Sullivan G, Hall JE. A national survey into the peri-operative anaesthetic management of patients presenting for surgical correction of a fractured neck of femur. Anaesthesia. 2008;63:250–8. doi: 10.1111/j.1365-2044.2007.05328.x. [DOI] [PubMed] [Google Scholar]
- 2.Sia S, Pelusio F, Barbagli R, Rivituso C. Analgesia before performing a spinal block in the sitting position in patients with femoral shaft fracture: A comparison between femoral nerve block and intravenous fentanyl. Anesth Analg. 2004;99:1221–4. doi: 10.1213/01.ANE.0000134812.00471.44. [DOI] [PubMed] [Google Scholar]
- 3.Mosaffa F, Esmaelijah A, Khoshnevis H. Analgesia before performing a spinal block in the lateral decubitus position in patients with femoral neck fracture: A comparison between fascia iliaca block and IV fentanyl. Reg Anesth Pain Med. 2005;30(Suppl 1):61. [Google Scholar]
- 4.Szucs S, Iohom G, O’Donnell B, Sajgalik P, Ahmad I, Salah N, et al. Analgesic efficacy of continuous femoral nerve block commenced prior to operative fixation of fractured neck of femur. Perioper Med (Lond) 2012;1:4. doi: 10.1186/2047-0525-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iamaroon A, Raksakietisak M, Halilamien P, Hongsawad J, Boonsararuxsapong K. Femoral nerve block versus fentanyl: Analgesia for positioning patients with fractured femur. Local Reg Anesth. 2010;3:21–6. doi: 10.2147/lra.s8600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parker MJ, Handoll HH, Griffiths R. Anaesthesia for hip fracture surgery in adults. Cochrane Database Syst Rev. 2004:CD000521. doi: 10.1002/14651858.CD000521.pub2. [DOI] [PubMed] [Google Scholar]
- 7.Urwin SC, Parker MJ, Griffiths R. General versus regional anaesthesia for hip fracture surgery: A meta-analysis of randomized trials. Br J Anaesth. 2000;84:450–5. doi: 10.1093/oxfordjournals.bja.a013468. [DOI] [PubMed] [Google Scholar]
- 8.Stanley I. The anaesthetic management of upper femoral fracture. Curr Anaesth Crit Care. 2005;16:23–33. [Google Scholar]
- 9.Schiferer A, Gore C, Gorove L, Lang T, Steinlechner B, Zimpfer M, et al. A randomized controlled trial of femoral nerve blockade administered preclinically for pain relief in femoral trauma. Anesth Analg. 2007;105:1852–4. doi: 10.1213/01.ane.0000287676.39323.9e. [DOI] [PubMed] [Google Scholar]
- 10.Gosavi CP, Chaudhari LS, Poddar R. Use of femoral nerve block to help positioning during conduct of regional anesthesia (Abstract) [Last accessed on 2013 Dec 29]. Available from: http://www.bhj.org/journal/2001_4304_oct/org_531.htm .
- 11.Urbanek B, Duma A, Kimberger O, Huber G, Marhofer P, Zimpfer M, et al. Onset time, quality of blockade, and duration of three-in-one blocks with levobupivacaine and bupivacaine. Anesth Analg. 2003;97:888–92. doi: 10.1213/01.ANE.0000072705.86142.5D. [DOI] [PubMed] [Google Scholar]
- 12.Marhofer P, Oismüller C, Faryniak B, Sitzwohl C, Mayer N, Kapral S. Three-in-one blocks with ropivacaine: Evaluation of sensory onset time and quality of sensory block. Anesth Analg. 2000;90:125–8. doi: 10.1097/00000539-200001000-00028. [DOI] [PubMed] [Google Scholar]


