Abstract
Aims:
To study precipitating factors, outcomes, and recurrence of diabetic ketoacidosis (DKA) at a University hospital at Damascus, the capital of Syria.
Patients and Methods:
Medical records between 2006 and 2012 were reviewed. One hundred and fifteen admissions for 100 patients with DKA were included. All fulfilled the American Diabetic Association DKA diagnostic criteria.
Results:
Of 115 admissions of DKA, there were 92 single admission and 23 recurrent admissions (eight patients). The order of precipitating factors of recurrent DKA or single admissions were the same with different percentage. The first and second factors were infection (74% and 48%) and treatment problems (17% and 24%), respectively. Complications rate was significantly higher in the intensive care unit (41.6%), compared to the ward admissions (14.2%). Overall in-hospital mortality rate was 11.3%. The severity of medical conditions that provoke DKA with aging, not the metabolic complications of hyperglycemia or ketoacidosis, were behind this high mortality rate. Patients who died were significantly (P = 0.004) older than patients who were discharged alive.
Conclusion:
Results concerning precipitating factor were similar to the results of many other studies. However, mortality rate was higher which might be explained by the severity of underlying precipitating illness.
Keywords: Diabetic ketoacidosis, DKA, DKA precipitating factor, DKA recurrence, DKA outcomes
INTRODUCTION
Diabetic ketoacidosis (DKA) is one of the acute metabolic complications of diabetes mellitus (DM) which is fatal if not accurately treated. Its biochemical characteristics are hyperglycemia, ketonemia, and academia.[1]
While DKA annual incidence is estimated between 4.6 and 8 episodes per 1,000 patient admissions with diabetes in the US population-based studies,[2] it is unknown in developing countries.[3] According to The Center for Disease Control and Prevention (CDC) - National Diabetes Surveillance Program, hospital discharges with DKA as the first-listed diagnosis increased from about 80,000 discharges in 1988 to about 140,000 in 2009.[4] However, mortality rate of DKA have fallen significantly in the last 20 years from 7.96% to 0.67% as reported by Lin et al.[5]; but in developing countries, it is still high.[6]
DKA occurs mainly in type 1 DM patients. However, type 2 DM patients might develop DKA under severe stress or illness with metabolic decompensation.[7]
Inadequate insulin therapy and infection are the most common DKA precipitating factors. Other factors, including underlying medical conditions (such as myocardial infarction, stroke, pancreatitis, and trauma), provoke the release of counter-regulatory hormones and might result in DKA. Another reason which may participate in DKA is carbohydrate metabolism affecting drugs such as corticosteroids.[8,9,10]
DKA patients can be managed either in the intensive care unit (ICU) or in the general medical ward. The decision where to manage DKA patients should be based on the local availability of hospital resources, the severity of DKA, and patients' comorbidities.[11]
The aim of this work was to study precipitating factors, outcome, and recurrence of DKA during 7 years in one of Damascus University hospitals.
PATIENTS AND METHODS
This retrospective study was carried out in Damascus, the capital of Syria. Syria is classified by the World Bank as a “lower middle income country.”[12] Damascus has an estimated population of 1,711,000 according to 2010 General Census.[13]
All medical records of patients who were admitted under the impression of DKA from January 2006 to December 2012 at Al-Assad University Hospital (AUH) were comprehensively analyzed. AUH is a teaching hospital that serves as one of major tertiary referral hospitals for a district (Mohafazat) Damascus. It has 645 beds, 50 of them are for intensive care (http://auhd.edu.sy/en). This hospital is usually for adults. However, children in some cases might be treated at it.
Patients were included if they fulfilled all of the American Diabetic Association DKA diagnostic criteria as follows: Serum glucose >250 mg/dl, serum bicarbonate concentration <18 mmol/l, arterial pH < 7.30, and positive serum/urine ketones.
All tests were performed in AUH clinical laboratory and analyzed immediately after collection by the same team of laboratory technicians. The same method was used throughout the study period, using kits provided by the same manufacturer.
Serum glucose, creatinine, potassium (K), sodium (Na), alanine transaminase (ALT), aspartate transaminase (AST), and albumin were measured by standard colorimetric methods using the Roche Hitachi 912 autoanalyzer (Roche Diagnostics, Mannheim, Germany). Arterial blood gasses and serum bicarbonate concentration were measured using Electrode-ABL 800 Felex Radiometer. Serum ketones were tested by Optium Xceed- Abbott) and urine ketones by Cortes Diagnostics, INC.
All patients were managed initially in the emergency department, then transferred to either ICU or endocrinology service according to ICU availability, as it is the policy at AUH to manage DKA in the ICU, unless an ICU bed is not available
Demographic characteristics, initial presentations, precipitating factors, admission laboratory/clinical data, treatment, and outcome of DKA for each admission were retrieved from medical records after full review. The study was ethically approved by the medical faculty review board.
Statistical analysis
Statistical analysis was carried out using the Statistical Package for Social Sciences (SPSS, version 16). The results are presented as the mean ± standard deviation for continuous variables, and as the total number of patients (percentage of total patients) for categorical data. Chi-square test was used to analyze group differences for categorical variables.
A P value less than 0.05 was considered significant.
RESULTS
From the beginning of 2006 to the end of 2012, 1,405 patients with DM were admitted to AUH (to the endocrine floor and the ICU) for different reasons. DKA as an initial diagnosis was found in 158 admissions. Forty-three admissions were excluded due to incomplete data or incorrect diagnosis of DKA according to the American Diabetes Association criteria. We ended with 115 (8.18%) DKA admissions for 100 patients which were included in this study. Records were classified into two groups: 92 records of single admission and 23 records of recurrent admissions (eight patients).
Table 1 shows the demography of the 100 patients presented only once with DKA Sixty-three percent of the patients were adults. The Majority of them (69%) had type 1 diabetes.
Table 1.
Demography and diabetes status
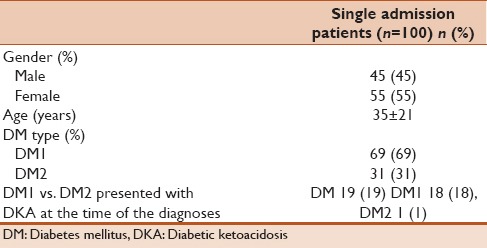
Table 2 shows the precipitating factor for DKA. The initial presentation [Table 2] (n = 115) were predominantly gastrointestinal symptoms.
Table 2.
DKA precipitating factors and initial presentation
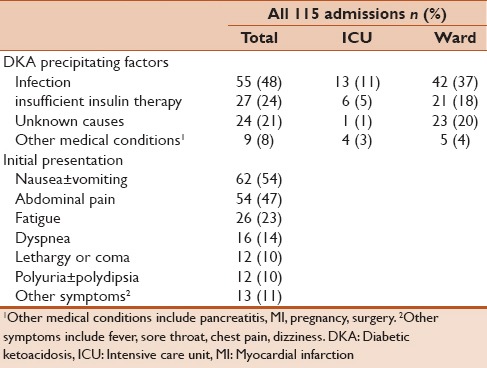
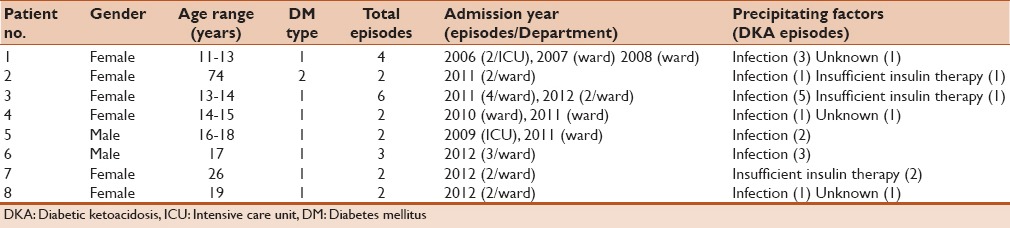
Table 3 shows the demography of the eight patients with 23 episodes of recurrent DKA admissions. Female to male ratio was 6:2, the majority of patients were type 1 DM and between 11 and 26 years old, except for patient No. 2 who was 74 years old and DM type 2. The precipitating causes of recurrent DKA in these 23 admissions were infection, treatment problems, then unknown causes. Two admissions were to the ICU, and 21 were to the ward (under the supervision of endocrine team).
Table 3.
Clinical data for patients with recurrent DKA admissions
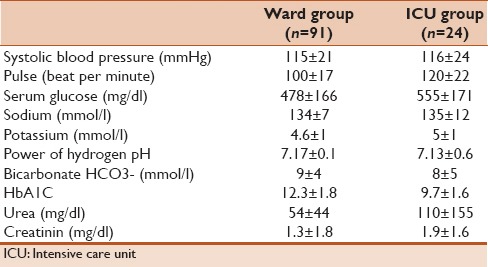
The majority of all 115 admissions were admitted to endocrinology service (91 admissions) and 24 admissions to the ICU (79% and 21%, respectively). Table 4 summarizes the clinical and laboratory characteristic of ward and ICU groups.
Table 4.
Admission clinical and laboratory data
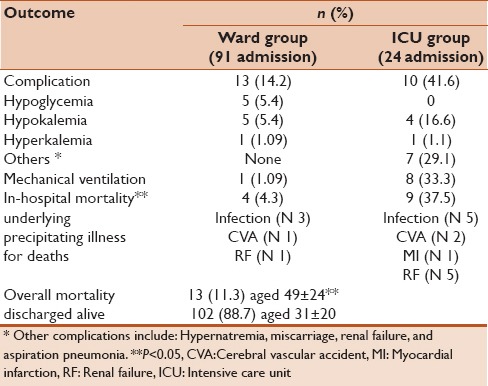
Complications rate was significantly (P < 0.05) higher in the ICU (41.6%, n = 10), compared to the ward (14.2%, n = 13). One of the ward patients (1.09%) needed mechanical ventilation compared to eight patients (33.3%) in the ICU. Overall in-hospital mortality rate was 11.3% (n = 13). Pearson Chi-square test showed that mortality rate in the ICU is significantly higher than it in the medical wards P < 0.05 [Table 5]. While three (7%) out of 43 child died, ten (13.9%) out of 72 adults died. Although it seems that mortality rate is higher in adults, it is statistically insignificant using Pearson Chi-square (P = 0.257). However, mortality rate was significantly higher in DM type 2 patients (P = 0.01).
Table 5.
In-hospital clinical outcomes
DISCUSSION
This is the first published paper, to our knowledge, about the precipitating factors, recurrence, and outcomes of DKA in Damascus.
Gender did not seem to have effect on the frequency of DKA which is consistent with what has been reported in the literature.[14]
The number of DM patients who presented with DKA at the time of the diagnoses differs among countries. For instance, it is 12.8% in the United Arab Emirate and 80% in Sweden.[15] In our study, it is 19% of patients, 95% of them were children with DM type 1. In the literature, the frequency of DKA at type 1 diabetes onset is high in children (16–54%).[16]
Patients with type 2 diabetes were 31% in this study. Unfortunately, there was no follow-up to distinguish if they were latent autoimmune diabetes in adults (LADA), or atypical ketosis-prone type 2 DM.[17,18]
Infections were the predominant precipitating factors for DKA in all admissions, followed by insulin-related problems. Similar results were reported in studies from the US,[2] Pakistan,[9] and India.[19] However, some recent studies suggested that omission of insulin or under-treatment with insulin may be the most important precipitating factor as in Saudi Arabia[20] and in a Brazilian study.[21] In our study, there was misunderstanding among 24% of patients who intended to minimize insulin dose or stop it with illness to prevent hypoglycemia [Table 2].
The policy at AUH is to admit DKA cases to the ICU. However, because of limited availability severe DKA cases might hospitalized in medical wards and mild-moderate cases might managed in the ICU. Having a predefined local guideline for referral to either ICU or medical ward was reported to save time, resources, up to 30% of hospitalization cost,[2,22] and might lead to better outcomes.
The in-hospital mortality rate in this study was 11.3%. This figure is higher than that reported in other developing countries such as India,[3] Pakistan, and Thailand[23] (7.1%, 7.15%, and 8.4%, respectively). Most patients who died were in the ICU and on mechanical ventilation. They came with sever precipitating illness: Nearly 62% of them had severe infection, and 46% had renal failure. This is compatible with other reports of DKA fatality that is primarily due to the underlying precipitating illness and rarely due to the metabolic complications of hyperglycemia or ketoacidosis.[24] Aging increased mortality rate and patients who died were significantly older than patients who were discharged alive (P = 0.004) which is consistent with what has been reported in the literature.[25]
DKA complications were high at AUH (20%). This might be explained in part by some mis-management particularly when endocrinology consultation was not requested. Less complications significantly were seen among ward group who were seen by the endocrinology team (P = 0.001). Although being treated by endocrinologist significantly reduce complications rate in repeated DKA that admitted to the ward (P = 0.001), it did not stop DKA recurrence. Another reason that might have participated in such higher complication rate, is absent of a detailed defined protocol or guideline for DKA management at AUH which.
Limitations
This study has several limitations. Firstly, it was a retrospective review of records, performed at one hospital which cares mainly for adults. Longitudinal studies indicated that pediatric patients account for 80% of all admissions for DKA;[26] such cases are usually referred to Damascus University Children Hospital. Secondly, lactate level was not measured in ICU patients, which might contribute to acidosis. Finally, selection bias was resulted from the lack of good documentations in the patients charts (many patients files were excluded). This was one of the important limitations.
Future work
We implemented a DKA protocol at AUH. Adherence to this protocol and further study on its effects on patients care and outcomes will be carried out. What is more, we are planning to work more on patients' education on DM to improve their understanding and knowledge.
ACKNOWLEDGMENTS
The authors wish to thank Dr. Mohammad Almohammad and Dr, Dani Markabawi for assistance in data collecting. They appreciate Miss Hend Alkabbani, and all members of medical record department at AUH for their help. They also thank Dr. Younes Kabalan and Dr. Mohammad Salem Alhalabi for helpful notes.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Wolfsdorf J, Craig ME, Daneman D, Dunger D, Edge J, Lee W, et al. Diabetic ketoacidosis in children and adolescents with diabetes. Pediatr Diabetes. 2009;10(Suppl 12):118–33. doi: 10.1111/j.1399-5448.2009.00569.x. [DOI] [PubMed] [Google Scholar]
- 2.Savage MW, Dhatariya KK, Kilvert A, Rayman G, Rees JA, Courtney CH, et al. Joint British Diabetes Societies. Joint British Diabetes Societies guideline for the management of diabetic ketoacidosis. Diabet Med. 2011;28:508–15. doi: 10.1111/j.1464-5491.2011.03246.x. [DOI] [PubMed] [Google Scholar]
- 3.Zargar AH, Wani AI, Masoodi SR, Bashir MI, Laway BA, Gupta VK, et al. Causes of mortality in diabetes mellitus: Data from a tertiary teaching hospital in India. Postgrad Med J. 2009;85:227–32. doi: 10.1136/pgmj.2008.067975. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. National Diabetes Surveillance System. [Last accessed 2012 May 17]. Available from: http://www.cdc.gov/diabetes/statistics/dkafirst/fig1.htm .
- 5.Lin SF, Lin JD, Huang YY. Diabetic ketoacidosis: Comparisons of patient characteristics, clinical presentations and outcomes today and 20 years ago. Chang Gung Med J. 2005;28:24–30. [PubMed] [Google Scholar]
- 6.Otieno CF, Kayima JK, Omonge EO, Oyoo GO. Diabetic ketoacidosis: Risk factors, mechanisms and management strategies in sub-Saharan Africa: A review. East Afr Med J. 2005;82:S197–203. doi: 10.4314/eamj.v82i12.9382. [DOI] [PubMed] [Google Scholar]
- 7.Smiley D, Chandra P, Umpierrez GE. Update on diagnosis, pathogenesis and management of ketosis-prone Type 2 diabetes mellitus. Diabetes Manag (Lond) 2011;1:589–600. doi: 10.2217/DMT.11.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sehgal V, Jit Singh Bajwa S, Kitabchi A. Coronary artery bypass grafting: A precipitating factor for perioperative diabetic ketoacidosis. Int J Endocrinol Metab. 2013;11:126–8. doi: 10.5812/ijem.7183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Naveed D, Bilal N, Nasir B, Lodhi BU. Precipitating factors for diabetic ketoacidosis. Kust Med J. 2009;1:6–8. [Google Scholar]
- 10. [Last accessed on 2014 Jun 06]. Available from: http://us.bestpractice.bmj.com/best-practice/monograph/162/basics/etiology.html .
- 11.Gershengorn HB, Iwashyna TJ, Cooke CR, Scales DC, Kahn JM, Wunsch H. Variation in use of intensive care for adults with diabetic ketoacidosis. Crit Care Med. 2012;40:2009–15. doi: 10.1097/CCM.0b013e31824e9eae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. [This page was Last accessed on 2014 Dec 02]. HYPERLINK “http://en.wikipedia.org/wiki/Syria” \l “cite_note-data.worldbank.org-123” ; http://en.wikipedia.org/wiki/Syria#cite_note-data.worldbank.org-123 . HYPERLINK “http://data.worldbank.org/about/country-classifications/country-and-lending-groups” . Data.worldbank.org . “Country and Lending Groups”.
- 13. [This page was Last accessed on 2014 Dec 06]. Available from: http://en.wikipedia.org/wiki/Damascus_Governorate .
- 14.Usher-Smith JA, Thompson MJ, Sharp SJ, Walter FM. Factors associated with the presence of diabetic ketoacidosis at diagnosis of diabetes in children and young adults: A systematic review. BMJ. 2011;343:d4092. doi: 10.1136/bmj.d4092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Usher-Smith JA, Thompson M, Ercole A, Walter FM. Variation between countries in the frequency of diabetic ketoacidosis at first presentation of type 1 diabetes in children: A systematic review. Diabetologia. 2012;55:2878–94. doi: 10.1007/s00125-012-2690-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Limenis E, Shulman R, Daneman D. Is the frequency of ketoacidosis at onset of type 1 diabetes a child health indicator that is related to income inequality? Diabetes Care. 2012;35:e5. doi: 10.2337/dc11-1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Imran SA, Ur E. Atypical ketosis-prone diabetes. Can Fam Physician. 2008;54:1553–4. [PMC free article] [PubMed] [Google Scholar]
- 18.Gooderick D, Dashora U, Kumar S. Ketoacidosis in type 2 diabetes- is it type 1 and ½ diabetes? BMJ Case Rep. 2011;2011 doi: 10.1136/bcr.07.2011.4460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ganie MA, Koul S, Razvi HA, Laway BA, Zargar AH. Hyperglycemic emergencies in Indian patients with diabetes mellitus on pilgrimage to Amarnathji yatra. Indian J Endocrinol Metab. 2012;16(Suppl 1):S87–90. doi: 10.4103/2230-8210.94267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Al-Rubeaan KA, Aftab SA, Alotaibi MS, Alghamdi AA, Rafiullah MR. Clinico-laboratory characteristics of diabetic keto acidosis in adults in a tertiary hospital in Saudi Arabia. Eur Rev Med Pharmacol Sci. 2011;15:1202–6. [PubMed] [Google Scholar]
- 21.Weinert LS, Scheffel RS, Severo MD, Cioffi AP, Teló GH, Boschi A, et al. Precipitating factors of diabetic ketoacidosis at a public hospital in a middle-income country. Diabetes Res Clin Pract. 2012;96:29–34. doi: 10.1016/j.diabres.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 22.Wolfsdorf J, Craig ME, Daneman D, Dunger D, Edge J, Lee WR, et al. International Society for Pediatric and Adolescent Diabetes. ISPAD clinical practice consensus guidelines 2006-2007. Diabetic ketoacidosis. 2007;8:28–43. [Google Scholar]
- 23.Anthanont P, Khawcharoenporn T, Tharavanij T. Incidences and outcomes of hyperglycemic crises: A 5-year study in a tertiary care center in Thailand. J Med Assoc Thai. 2012;95:995–1002. [PubMed] [Google Scholar]
- 24.Kitabchi AE, Umpierrez GE, Murphy MB, Kreisberg RA. Hyperglycemic crises in adult patients with diabetes: A consensus statement from the American Diabetes Association. Diabetes Care. 2006;29:2739–48. doi: 10.2337/dc06-9916. [DOI] [PubMed] [Google Scholar]
- 25.MacIsaac RJ, Lee LY, McNeil KJ, Tsalamandris C, Jerums G. Influence of age on the presentation and outcome of acidotic and hyperosmolar diabetic emergencies. Intern Med J. 2002;32:379–85. doi: 10.1046/j.1445-5994.2002.00255.x. [DOI] [PubMed] [Google Scholar]
- 26.Skinner TC. Recurrent diabetic ketoacidosis: Causes, prevention and management. Horm Res. 2002;57(Suppl 1):78–80. doi: 10.1159/000053320. [DOI] [PubMed] [Google Scholar]