Abstract
Aim:
Aim of the study isto assess the scope of physical activity among type 2 diabetes mellitus (T2DM) patients residing in an urban area of SouthIndia.
Materials and Methods:
A longitudinal interventional study was conducted for a period of 8months (January 2014–August 2014) among patients of T2DM accessing the healthcare services at an Urban Health and Training Center (UHTC) of a Medical College located in Kancheepuram district, Tamil Nadu. Universal sampling method was employed and all diagnosed T2DM patients attending UHTC during the month of January were enrolled in the study provided they satisfied the inclusion and exclusion criteria. Overall 151 participants were considered for final analysis and all of them were subjected to indulge in moderate type of aerobic exercise in the form of brisk walking for 2.5 h spread over a period of 1 week, for the next 6months. Before and after the exercise regimen, cases were subjected to clinical evaluation, measurement of weight and waist circumference, and estimation of fasting and postprandial blood sugar; and the results were compared with the baseline estimates. The associations were tested using paired t-test for continuous (mean ± standard deviation ( SD)) variables.
Results:
Majority (86, 57%) of the diabetics were from the age group of 40–60 years with a definite female preponderance (82/151) in contrast to males (69/151). A significant reduction in both fasting and postprandial sugar was observed before and after the exercise. However, from the perspective of the weight and waist circumference, although a reduction was observed, the association was not statistically significant.
Conclusion:
The findings of the present longitudinal study suggest that compliance with moderate type of physical activity can significantly improve the fasting and postprandial blood sugar, apart from reduction in weight of T2DM patients.
Keywords: Exercise, diabetes, India, physical activity, type 2 diabetes mellitus
INTRODUCTION
Diabetes mellitus (DM) is a lifestyle disease characterized by hyperglycemia resulting because of the absolute (type 1 DM (T1DM)) or relative (type 2 DM (T2DM)) deficiency of the insulin hormone.[1] It has been estimated that globally approximately 350 million people suffer from diabetes and this magnitude is expected to be doubled by 2030 in absence of any intervention.[2,3] As opposed to the previous notion that diabetes is more common in developed nations, recent estimates suggest that a remarkable surge in both the incidence and onset of the disease at an earlier age has been found in developing nations.[4,5,6] Furthermore, almost 80% of diabetes deaths occur in low- and middle-income nations and it has been estimated that it will be the seventh leading cause of death by the year 2030.[3,7]
India has been designated as “diabetes capital” of the world, owing to the share of the highest number of people with diabetes.[8] Infact, the number of cases of diabetes is projected to increase to almost 80 million by the year 2030 as opposed to 32 millionin2000.[8] The causation of DM is multifactorial, and includes both nonmodifiable (viz. age, genetic defects, family history) and modifiable (viz. obesity, sedentary lifestyle, diet, etc.).[2,9,10,11] The significance of exercise in the prevention and control of diabetes has been known since time immemorial.[12,13,14] Infact, some form of physical activity and exercise has been advocated for initial and ongoing management of type 2 diabetes.[12,15,16] A wide range of benefits like improved glycemic control, reduction in LDL levels, lowering of blood pressure, enhancement of weight loss, weight maintenance, stabilization of gait, reaction time, postural stability, maintenance of sympathovagal balance, improvement in the number of insulin receptors and their sensitivity, and reduction in HbA1c, have been attributed to exercise among diabetes patients.[17,18,19,20,21] Furthermore, increased physical activity in diabetes may enable reduction, or even discontinuation, of drugs in a major proportion of patients.[22]
Acknowledging the importance of physical activity and exercise components in the management of type 2 diabetes patients, and in absence of studies to ascertain the benefits of exercise on different aspects of diabetes, especially in Indian settings, the present study has been planned to assess the scope of physical activity among T2DM patients residing in an urban area of SouthIndia.
MATERIALS AND METHODS
Settings and design
A longitudinal interventional study was conducted for a period of 8 months (January 2014–August 2014) among patients of T2DM accessing the healthcare services at an Urban Health and Training Center (UHTC) of a Medical College located in Kancheepuram district, Tamil Nadu.
The method of sampling employed was universal sampling, which meant that all diagnosed T2DM patients attending UHTC during the month of January were enrolled in the study provided they satisfied the inclusion and exclusion criteria.
Inclusion criteria
All type 2 diabetes patients who were
Willing to participate in the study
Normal ECG findings before inclusion in the study
Normal blood pressure response to standing (viz. under normal physiological circumstances a fall in blood pressure is observed when a person shifts from supine to standing position—fall in systolic and diastolic blood pressure to <20 mmHg and <10 mmHg, respectively)
No evidence of peripheral vascular disease on clinical examination, and
No evidence of retinopathy and/or macular edema on fundoscopy.
Exclusion criteria
All those who were not willing to participate or were planning to go outside in the next 6months (n = 3); presence of comorbid condition like associated bronchial asthma, severe hypertension with end organ damage (n = 2); and patient on regular short-acting human insulin (n = 1), were excluded from the study.
Methodology
In the month of January 2014, total 167 T2DM patients visited the UHTC for their routine follow-up. Out of them, six patients were excluded as mentioned above. The remaining 161 patients were then subjected to clinical evaluation, ECG, and fundoscopy examination (with the assistance of an ophthalmologist) to assess their inclusion in the study. This led to the exclusion of additional four subjects, and thus for final analysis 157 subjects were selected.
A semistructured questionnaire was used for eliciting the sociodemographic and economicdetails of the study participants. These selected participants were then subjected to measurement of blood pressure, weight and waist circumference, and estimation of fasting and postprandial blood sugar. The obtained results were considered as the baseline data.
Each of the selected diabetes patients was individually explained about the benefits associated with indulgence in physical activity and exercise. They were counseled to indulge in moderate type of aerobic exercise in the form of brisk walking for 2.5 hours spread over a period of 1 week, that is, atleast 30 min of brisk walking daily for any 5 days in a week, for the next 6months (February–July 2014).[23] Each of the participant was counseled about symptoms of hypoglycemia andalso informed to carry glucose biscuits along with them while going for walking; to take glucose biscuits if symptoms of hypoglycemia (viz. feeling of uneasiness, giddiness, excessive sweating, etc.) occur during exercise; to report to the hospital in the event of experiencing any discomfort; and continue their routine monthly follow-up.
During each follow-up visits, study subjects were clinically evaluated and even motivated to continue their physical activity as prescribed. However, six subjects could not stick with the prescribed regimen and thus excluded from the study. Thus at the end of 6months of prescription of moderate type of physical activity, total 151 T2DM patients completed the exercise regimen. The investigators relied only on self-reported compliance to the prescribed exercise regimen during each of their monthly follow-up visits.
All these 151 patients were again subjected to clinical evaluation, measurement of blood pressure, weight and waist circumference, and estimation of fasting and postprandial blood sugar after completion of 6months of prescribed physical activity regimen, and the results were compared with the baseline estimates.
Ethical considerations
Institutional ethical clearance was obtained prior to the start of the study. Written informed consent was obtained from the study participants after explaining them the purpose of the study. Utmost care was taken to ensure confidentiality.
Statistical analysis
Data entry and statistical analysis was done using Statistical Package for Social Sciences (SPSS) version 18. Frequency distributions and percentages were computed for all the variables. The statistical significance was set at P < 0.05. The associations were tested using paired t-test for continuous (mean ± SD) variables.
RESULTS
Table 1 represents the distribution of study subjects based on their sociodemographic and economicattributes. Almost 86 (57%) diabetics were from the age group of 40–60 years with the youngest and oldest participant of 31 and 67 years, respectively. The results clearly reflect the phenomenon of early onset (32/151) of type 2 diabetes among the study participants. Most of the study subjects were females (82/151) and married (138/151). However, around 105 (70.2%) diabetic patients were either retired or home-makers (mostly females - 77).
Table 1.
Sociodemographic and economic attributes of study participants
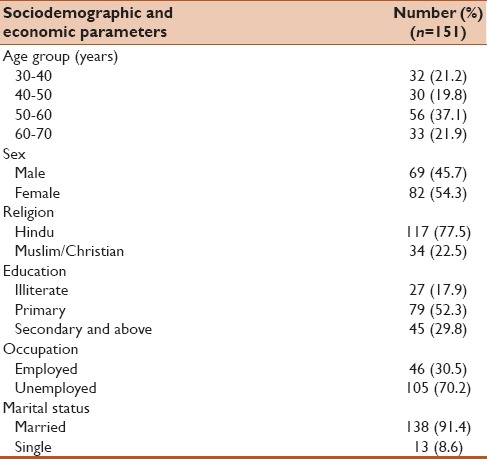
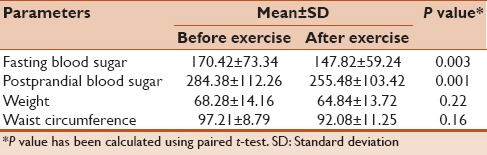
Table 2 reflects the association between anthropometric/biochemical estimates at the start of the study and after a period of 6months of the exercise. The findings of the study suggest that a significant difference in both fasting and postprandial sugar was observed before and after the exercise, that is, after the completion of prescribed exercise regimen significant reduction in blood sugar was obtained. The mean reduction in systolic blood pressure was observed to be 12 ± 4 mmHg and that in diastolic blood pressure was found to be 4 ± 2 mmHg. The difference was not found to be statistically significant. However, from the perspective, weight and waist circumference among the study participants, although a reduction was observed, nevertheless the association was not statistically significant. On clinical examination, none of the study participants developed any diabetes associated complications at the end of the prescribed exercise regimen.
Table 2.
Association between anthropometric and biochemical estimates before and after exercise
DISCUSSION
The current study is a longitudinal study to assess the impact of moderate exercise (viz. brisk walking) for a period of 6months on the clinical, anthropometric, and biochemical attributes of the type 2 diagnosed diabetic patients. Although, a major proportion of the study participants were found to be more than 40-years-old (119/151), around 32 (21.2%) of the type 2 diabetes patients belonged to the agegroup of 30–40 years. Findings of studies done in different settings have also revealed similar results suggesting a shift on the left (early onset) for T2DM.[24,25] The present study revealed that more number of female subjects (82/151) were having diabetes in contrast to the males (69/151).
In the current interventional study, a statistically significant improvement was observed pertaining to their fasting and postprandial blood sugar levels, among the study subjects who regularly practiced moderate type of physical activity for a period of 6months. In most of the studies where exercise/physical activity has been included as one of the factors in the management of T2DM, quite favorable results have been observed especially with regard to blood sugar levels.[19,21,26,27] The benefit associated with physical activity in management of diabetes is because of the increase in burning of the muscles glycogen (in early stages), followed by consumption of free fatty acids and fats deposited in the adipose tissue.[15,28,29]
Despite the fact that, a mean reduction in weight (from 68.28 kg before exercise to 64.84 kg after exercise) was observed among the study participants, but the association was not significant on employing paired t-test. In contrast, a significant reduction in weight among type 2diabetic patients has been observed in systematic reviews or studies done in different settings.[30,31,32]
The strength of the present study is that it considered most of the sociodemographic and anthropometric variables associated with exercise and T2DM. Also, it is one of the few longitudinal studies from South India which has attempted to explore the impact of exercise on clinical, biochemical, and anthropometric attributes among T2DM patients. In limitation, no full-proof mechanism was employed to assess participant's adherence to the prescribed exercise regimen, and some of other laboratory investigations like HbA1c were not performed, due to infrastructure constraints. Also, as there was no control group in the study, findings of the study could not be generalized to the entire population.
CONCLUSION
The findings of the present longitudinal study suggest that compliance with moderate type of physical activity can significantly improve the fasting and postprandial blood sugar, apart from reduction in weight of T2DM patients. Furthermore, the results of this study can be utilized by the program managers to include physical activity as one of the crucial component in ensuring adequate control of blood sugar in diabetic patients. Thus, physical activity, in conjunction with therapeutic management of diabetes, ensuresa comprehensive strategy for appropriate management of DM.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.World Health Organization. Definition, diagnosis and classification of diabetes mellitus and its complications. Geneva: WHO press; 1999. [Google Scholar]
- 2.Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ, et al. Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Blood Glucose). National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: Systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet. 2011;378:31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- 3.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kinra S, Bowen LJ, Lyngdoh T, Prabhakaran D, Reddy KS, Ramakrishnan L, et al. Sociodemographic patterning of non-communicable disease risk factors in rural India: A cross sectional study. BMJ. 2010;341:c4974. doi: 10.1136/bmj.c4974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chuang LM, Tsai ST, Huang BY, Tai TY. Diabcare-Asia 1998 Study Group. The status of diabetes control in Asia-a cross-sectional survey of 24 317 patients with diabetes mellitus in 1998. Diabet Med. 2002;19:978–85. doi: 10.1046/j.1464-5491.2002.00833.x. [DOI] [PubMed] [Google Scholar]
- 6.Narayanappa D, Rajani HS, Mahendrappa KB, Prabhakar AK. Prevalence of prediabetes in school-going children. Indian Pediatr. 2011;48:295–9. doi: 10.1007/s13312-011-0061-6. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. Global status report on non-communicable diseases-2010. Geneva: WHO press; 2011. [Google Scholar]
- 8.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 9.Park K. Epidemiology of chronic non-communicable diseases and conditions. In: Park K, editor. Text Book of Preventive and Social Medicine. 20th ed. Jabalpur: Banarsidas Bhanot Publishers; 2009. pp. 341–5. [Google Scholar]
- 10.Majgi SM, Soudarssanane BM, Roy G, Das AK. Risk factors of diabetes mellitus in rural Puducherry. Online J Health Allied Scs. 2012;11:4. [Google Scholar]
- 11.World Health Organization. Preventing chronic diseases: A vital investment. Geneva: WHO press; 2005. [Google Scholar]
- 12.Sato Y. Principle of physical exercise for diabetes: Exercise prescription. Nihon Rinsho. 2002;60:256–60. [PubMed] [Google Scholar]
- 13.Barengo NC, Tuomilehto J. Diabetes: Exercise benefits in type 2 diabetes mellitus. Nat Rev Endocrinol. 2012;8:635–6. doi: 10.1038/nrendo.2012.182. [DOI] [PubMed] [Google Scholar]
- 14.Dunstan D. Diabetes: Exercise and T2DM-move muscles more often! Nat Rev Endocrinol. 2011;7:189–90. doi: 10.1038/nrendo.2011.35. [DOI] [PubMed] [Google Scholar]
- 15.Jessen N, Goodyear LJ. Diabetes: Exercise and type 2 diabetes mellitus-good for body and mind? Nat Rev Endocrinol. 2010;6:303–4. doi: 10.1038/nrendo.2010.47. [DOI] [PubMed] [Google Scholar]
- 16.Nagi D, Gallen I. ABCD position statement on physical activity and exercise in diabetes. Pract Diabetes Int. 2010;27:158–63. [Google Scholar]
- 17.Colberg SR. Increasing insulin sensitivity. Diabetes Self Manag. 2007;24:47–50. [PubMed] [Google Scholar]
- 18.Colberg SR, Sigal RJ, Fernhall B, Regensteiner JG, Blissmer BJ, Rubin RR, et al. American College of Sports Medicine, American Diabetes Association. Exercise and type 2 diabetes: The American College of Sports Medicine and the American Diabetes Association: Joint position statement executive summary. Diabetes Care. 2010;33:2692–6. doi: 10.2337/dc10-1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Colberg SR. Physical activity, insulin action, and diabetes prevention and control. Curr Diabetes Rev. 2007;3:176–84. doi: 10.2174/157339907781368986. [DOI] [PubMed] [Google Scholar]
- 20.Morrison S, Colberg SR, Parson HK, Vinik AI. Exercise improves gait, reaction time and postural stability in older adults with type 2 diabetes and neuropathy. J Diabetes Complications. 2014;28:715–22. doi: 10.1016/j.jdiacomp.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 21.Colberg SR, Grieco CR, Somma CT. Exercise effects on postprandial glycemia, mood, and sympathovagal balance in type 2 diabetes. J Am Med Dir Assoc. 2014;15:261–6. doi: 10.1016/j.jamda.2013.11.026. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organization: Global recommendations on physical activity for health. 2011. [Last accessed on 2014 Aug 22]. Available from: http://www.who.int/dietphysicalactivity/leaflet-physical-activity-recommendations.pdf?ua=1 .
- 23.Jeon CY, Lokken RP, Hu FB, van Dam RM. Physical activity of moderate intensity and risk of type 2 diabetes: A systematic review. Diabetes Care. 2007;30:744–52. doi: 10.2337/dc06-1842. [DOI] [PubMed] [Google Scholar]
- 24.Lerman-Garber I, Aguilar-Salinas C, Tusie-Luna T, Velasquez D, Lobato-Valverde M, Osornio-Flores M, et al. Early-onset type 2 diabetes mellitus. The experience from a third level medical institution. Gac Med Mex. 2010;146:179–84. [PubMed] [Google Scholar]
- 25.Jali MV, Kambar S, Jali SM, Gowda S. Familial early onset of type-2 diabetes mellitus and its complications. N Am J Med Sci. 2009;1:377–80. doi: 10.4297/najms.2009.7377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Colberg SR, Castorino K, Jovanovic L. Prescribing physical activity to prevent and manage gestational diabetes. World J Diabetes. 2013;4:256–62. doi: 10.4239/wjd.v4.i6.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Colberg SR. Physical activity: The forgotten tool for type 2 diabetes management. Front Endocrinol (Lausanne) 2012;3:70. doi: 10.3389/fendo.2012.00070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boon H, Blaak EE, Saris WH, Keizer HA, Wagenmakers AJ, van Loon LJ. Substrate source utilisation in long-term diagnosed type 2 diabetes patients at rest, and during exercise and subsequent recovery. Diabetologia. 2007;50:103–12. doi: 10.1007/s00125-006-0482-2. [DOI] [PubMed] [Google Scholar]
- 29.Aguiar EJ, Morgan PJ, Collins CE, Plotnikoff RC, Callister R. Efficacy of interventions that include diet, aerobic and resistance training components for type 2 diabetes prevention: A systematic review with meta-analysis. Int J Behav Nutr Phys Act. 2014;11:2. doi: 10.1186/1479-5868-11-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tudor-Locke C, Schuna JM., Jr Steps to preventing type 2 diabetes: Exercise, walk more, or sit less? Front Endocrinol (Lausanne) 2012;3:142. doi: 10.3389/fendo.2012.00142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reiner M, Niermann C, Jekauc D, Woll A. Long-term health benefits of physical activity - A systematic review of longitudinal studies. BMC Public Health. 2013;13:813. doi: 10.1186/1471-2458-13-813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Frost J, Garside R, Cooper C, Britten N. A qualitative synthesis of diabetes self-management strategies for long term medical outcomes and quality of life in the UK. BMC Health Serv Res. 2014;14:348. doi: 10.1186/1472-6963-14-348. [DOI] [PMC free article] [PubMed] [Google Scholar]


