Abstract
Background:
The increased morbidity and mortality associated with nosocomial infections in the intensive care unit (ICU) is a matter of serious concern today.
Aims:
To determine the incidence of nosocomial infections acquired in the ICU, their risk factors, the causative pathogens and the outcome in a tertiary care teaching hospital.
Materials and Methods:
This was a prospective observational study conducted in a 12 bedded combined medical and surgical ICU of a medical college hospital. The study group comprised 242 patients admitted for more than 48 h in the ICU. Data were collected regarding severity of the illness, primary reason for ICU admission, presence of risk factors, presence of infection, infecting agent, length of ICU and hospital stay, and survival status and logistic regression analysis was done.
Results:
The nosocomial infection rate was 11.98% (95% confidence interval 7.89–16.07%). Pneumonia was the most frequently detected infection (62.07%), followed by urinary tract infections and central venous catheter associated bloodstream infections. Prior antimicrobial therapy, urinary catheterization and length of ICU stay were found to be statistically significant risk factors associated with nosocomial infection. Nosocomial infection resulted in a statistically significant increase in length of ICU and hospital stay, but not in mortality.
Conclusion:
Nosocomial infections increase morbidity of hospitalized patients. These findings can be utilized for planning nosocomial infection surveillance program in our setting.
Keywords: Intensive care unit, morbidity, mortality, nosocomial infection, risk factors
Introduction
A nosocomial infection is defined as an infection that is not present or incubating when the patient is admitted to hospital or other health care facility.[1] It has been reported that the incidence of nosocomial infections in the intensive care unit (ICU) is about 2 to 5 times higher than in the general in-patient hospital population.[2] The increased morbidity and mortality associated with nosocomial infections in the ICU is a matter of serious concern today. Serious medicolegal issues also arise in this context, since the patient or their families sometimes blame the hospital staff for the infection and demand compensation.[3] It has been reported that in hospitals with an effective program for nosocomial infection surveillance, infection rates can be reduced by approximately one-third.[4]
In our setting that of a busy ICU in a tertiary care teaching hospital in the public sector, survey of nosocomial infection has not been carried out in the recent past. The objectives of the present study were to determine the incidence of nosocomial infection, identify possible risk factors for these infections, to clarify the distribution of the causative pathogens and to evaluate the outcome of the infected patients in terms of length of ICU and hospital stay and mortality.
Materials and Methods
After approval from the Institutional Ethics Committee, we conducted this prospective observational study in the 12 bed combined medical and surgical ICU of a tertiary care medical college hospital between January 1 and June 30, 2012.
Out of the total of 455 patients admitted to the ICU during the 6-month study period, 242 patients staying for more than 48 h in the ICU were included in the study. All patients were monitored daily for the development of infection during their ICU stay and during the 72 h after discharge from the ICU. Patients who were re-admitted 72 h after discharge from the ICU were regarded as new admissions. Patients with infection at the time of admission were included in the noninfected group for the purpose of analysis. However, such patients were included in the group with ICU-acquired infection when they developed a new infection at a different anatomical site during the ICU stay.
All 242 patients in the study group were also followed-up till hospital discharge to acquire data on length of hospital stay and outcome in terms of mortality. Information on each patient was recorded on a structured case report form.
To assess the severity of illness on the 1st day in the ICU, the Acute Physiology and Chronic Health Evaluation II (APACHE II) score[5] was used. The patients were classified into seven groups according to the primary reason for ICU admission – cardiovascular, respiratory, neurological, renal, metabolic, gastrointestinal and surgical. Decision on infection or colonization was based on laboratory and clinical evidence. Nosocomial infections were diagnosed according to the standard definition of the (United States centers for disease control and prevention [CDC]).[6,7] Antimicrobial therapy was administered to the patients as necessary and cultures were requisitioned when infection was suspected. Patients were always sampled for microbial culture before starting a new antimicrobial. Appropriate essential investigations were regularly performed as needed.
For the determination of risk factors associated with ICU acquired nosocomial infection, the following putative risk factors were recorded: Age, gender, site from where the patient was transferred to the ICU, cause of ICU admission and the APACHE II score during the first 24 h of admission to the ICU. The following factors were recorded as present (at any time during the ICU stay) or absent in a particular patient before the development of ICU acquired infection: Underlying disease, comorbidity, central venous catheterization, pulmonary arterial catheterization, invasive arterial catheterization, peripheral venous catheterization, urinary catheterization, endotracheal intubation, re-intubation, tracheostomy, nasogastric tube insertion, mechanical ventilation, surgical procedure, prior antimicrobial therapy, antacid and stress ulcer prophylaxis therapy, sedative-analgesic therapy, vasopressor therapy, parenteral nutrition, enteral nutrition, horizontal body position with head at <30°, blood transfusion, hypoalbuminemia, diabetes mellitus, chronic renal failure, chronic alcoholism, malnutrition and immunocompromise.
For statistical analysis, the APACHE II scoring was grouped into two classes of ≥13 and <13 taking the median value for APACHE score as the cut-off. For the determination of the incidence of nosocomial infection, infections rates were expressed as a percentage. Also, infection rates were calculated per 1000 patient-days or per 1000 device days (for specific device associated infections) according to the CDC recommended formulas.
For classification of the different causative pathogens associated with nosocomial infections, all the microorganisms isolated on culture from each of the patients with confirmed infection according to the CDC definitions were recorded and their relative frequency of isolation were determined as percentage.[6,7] Bacterial isolates were identified by Gram-stain, cultures on routine media (e.g. Blood agar, MacConkey agar) and where necessary, selective media and specific biochemical tests following standard protocols.[8,9] Fungal isolates were identified by cultures on Sabouraud dextrose agar, and Sabouraud dextrose chloramphenicol agar media followed by Gram-stain, lactophenol cotton blue mount and germ tube testing following standard protocols.[10] For assessing outcome, each patient was followed-up till ICU and hospital discharge or death. Length of ICU stay and hospital stay were recorded as the number of days from admission to discharge from the ICU and hospital respectively. The length of ICU and hospital stay in patients with and without nosocomial infections and also the ICU and hospital mortality rates in patients in both groups were statistically compared.
Data have been summarized by routine descriptive statistics. 95% confidence interval (CI) values have been calculated for key variables. Numerical variables have been compared between groups by Student's independent samples t-test when normally distributed or by Mann–Whitney U-test when otherwise. Fisher's exact test has been employed for intergroup comparison of independent proportions. Univariate analysis has been two-tailed, and P < 0.05 has been considered statistically significant. All variables returning P < 0.1 on univariate analysis were entered into a logistic regression model of risk factors for nosocomial infection. Univariate and adjusted odds ratios (ORs) from the logistic regression analysis have been reported. SPSS Statistics version 17 (Illinois, Chicago: SPSS Inc., 2008) software was employed for statistical analysis.
Results
Data were collected from 242 patients accounting for a total of 1736 patient days.
Intensive care unit acquired nosocomial infections were detected in 29 patients (11.98%; 95% CI: 7.89-16.07%). These 29 patients developed one type of nosocomial infection each. The most frequently diagnosed nosocomial infection was nosocomial pneumonia. Combining both ventilator associated pneumonia (VAP) and non-VAP, nosocomial pneumonia was found in 18 (62.07%; 95% CI: 44.41-79.73%) of the 29 infected patients. Taken separately, VAP was diagnosed in 10 (34.48%) and nonventilator associated nosocomial pneumonia was diagnosed in 8 (27.59%) of the infected patients. Urinary tract infection was diagnosed in 8 (27.59%) out of the 29 infections and central venous catheter related blood stream infection was detected in 3 (10.34%) patients. Hence, when judged separately, VAP was the commonest ICU acquired infection detected.
On the calculation of the infection rate per 1000 patient's days or per 1000 device days, the following values were obtained:
Overall nosocomial infection rate = 16.71/1000 patient days
Nosocomial pneumonia rate (both VAP and non-VAP) =10.37/1000 patient days
VAP rate = 26.6/1000 ventilator days
Non-VAP rate = 4.61/1000 patient days
Urinary tract infection = 7.44/1000 catheter days
Central venous catheter associated bloodstream infection rate = 2.46/1000 central venous catheter days.
Upon comparison of putative risk factors of nosocomial infection by univariate analysis [Table 1], prior antimicrobial therapy, antacid use, hypoalbuminemia, malnutrition, urinary catheterization, endotracheal intubation, re-intubation, tracheostomy, placement of nasogastric tube, mechanical ventilation, APACHE II score >13 and length of ICU stay were found to be statistically significant. The logistic regression model tested a large number of predictors for possible association with the outcome of nosocomial infection as shown in Table 2. Out of these, prior antimicrobial therapy, urinary catheterization and length of ICU stay were found to be statistically significant risk factors for nosocomial infection by multivariate analysis. The model fit was good with a Nagelkerke R2 value of 0.754, indicating that over 75% of the variability in the model could be explained by the predictors selected. However, the limited sample size has resulted in relatively large 95% CI of adjusted ORs of the individual predictors.
Table 1.
Comparison of putative risk factors for nosocomial infections by univariate analysis
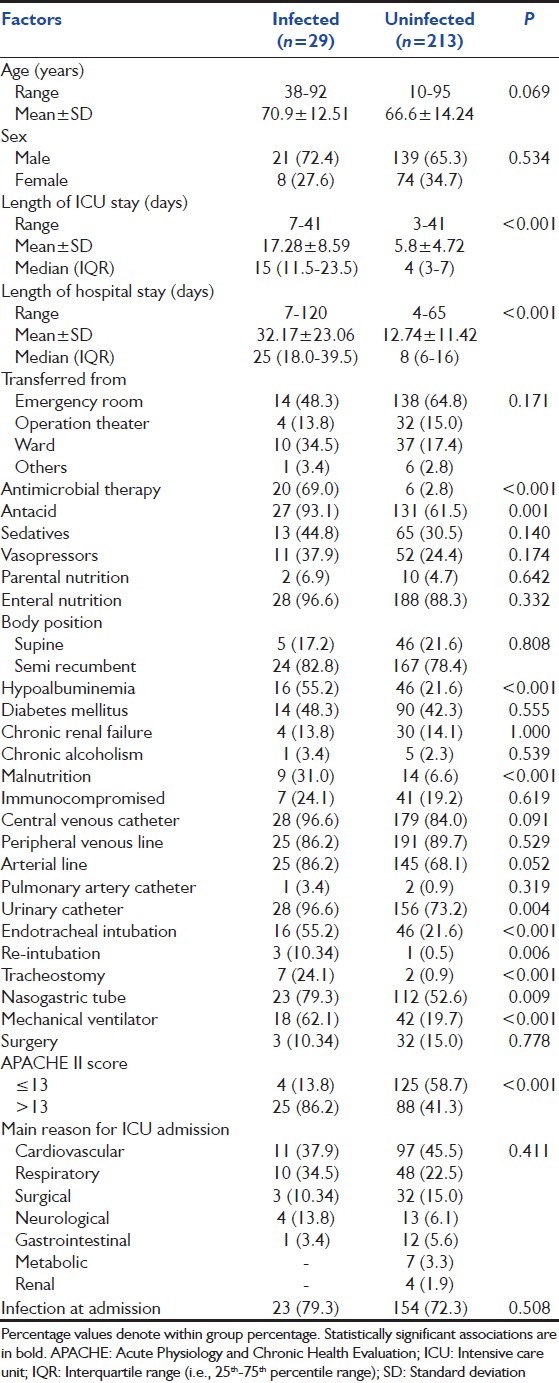
Table 2.
Results of univariate and multivariate (logistic regression) analysis of potential risk factors for nosocomial infections in the intensive care environment
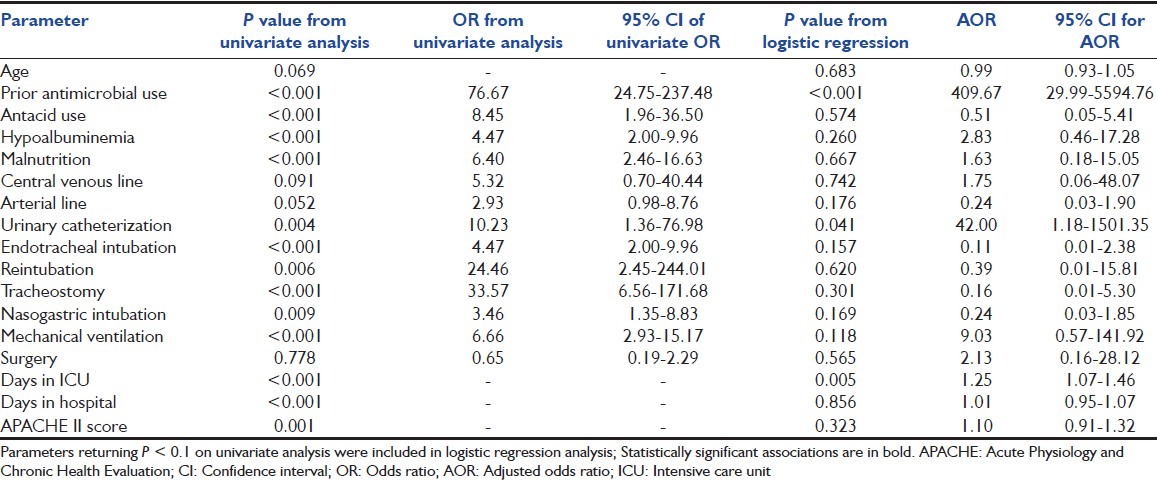
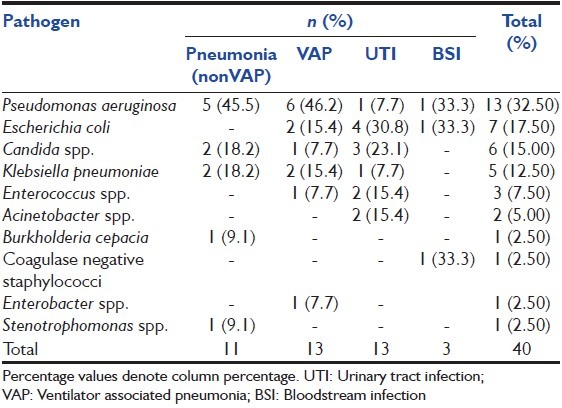
Table 3 summarizes the distribution of pathogens responsible for the nosocomial infection cases in this study, categorized by site of infection. A total of 40 pathogens were isolated on culture and accounted for the nosocomial infections in 29 patients. Some infections were polymicrobial. Gram-negative Enterobacteriaceae were the most frequently isolated pathogens (n = 15; 37.5%) closely followed by Pseudomonas species (n = 14; 35%, Pseudomonas aeruginosa = 13, Burkholderia cepacia = 1).
Table 3.
Distribution of causative micro-organisms of nosocomial infections by site
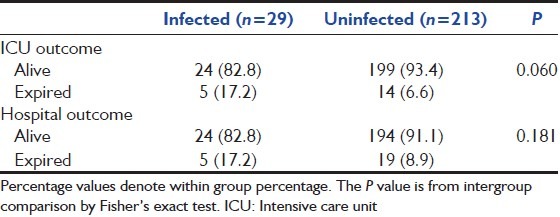
Regarding outcome, the length of total hospital and ICU stays have been depicted and compared in Table 1. Table 4 compares the outcome of ICU stay and total hospital stay, in terms of mortality, between the two groups. There was no statistically significant difference between the hospital mortality rates among the patients with and without nosocomial infection (P = 0.181). There was a trend toward greater mortality in the ICU in patients with nosocomial infection than in patients without (17.2% vs. 6.6%), although this did not reach statistical significance (P = 0.060).
Table 4.
ICU stay and hospital stay outcome compared
Discussion
The prevention of ICU acquired infections demands knowledge of the infection rates and of the sources, the pathogens involved as well as the common risk factors for infection. The incidence of nosocomial infections varies according to the setting, that is, the type of hospital or ICU, the patient population and the precise definition and surveillance techniques used to identify a nosocomial infection.[11] A large cohort multicentric international study has reported at least one ICU acquired infection in 18.9% of patients, with an incidence ranging from 2.3% to 49.2% across the centers.[12] In a 1-day point prevalence study involving 1265 ICU s from 76 countries (extended prevalence of infection in intensive care [EPIC II] study), 51% patients were found to have nosocomial infection. However, the rates of infections varied considerably according to the country, with Greece and Portugal having the highest and Switzerland and Germany and the Netherlands having the lowest infection rates.[13] Other studies[14,15] have reported incidence rates between 9% and 37%, depending largely on the populations studied. Crude infection rates might not be representative of the overall problem since they do not take into account the patients' intrinsic risk of infection or extrinsic risks associated with exposure to medical interventions.[16] The findings in our study were found to be closer to the lower range of incidence rates reported in the other studies referred above. This difference in findings is not necessarily related to better quality of care, since many other factors may be responsible including difference in the criteria for patient selection, the case mix, ICU type, length of stay, rate of device utilization and discharge criteria.[17,18] The patients from a single institution can present with different risk of infection in the context of differing case mix, severity of illness and utilization rates of invasive devices.[19]
In the EPIC II study,[13] the most frequently reported sites for ICU acquired infections were the lungs (64%), abdominal (19%), and blood stream (15%). Data from the United States National Nosocomial infections surveillance system showed that the nosocomial pneumonia accounted for 31% of all nosocomial infections followed by urinary tract infections and blood stream infections.[19] The site distribution of nosocomial infections in this study broadly conforms to the findings of earlier and larger studies mentioned above.
The precise pattern of causative organisms, whether bacterial or fungal, varies across countries and between ICUs according to patient case mix, site of infection, antibiotic protocols, infection control practice and local ecology and resistance patterns.[20] Although recent years have seen swings in the pathogen pattern toward Gram-positive bacterial infections,[21,22] still, most studies report that more than half of the nosocomial infections occurring in the ICU are due to Gram-negative bacteria.[13,19] In our study too, the most commonly isolated organisms were Gram-negative Enterobacteriaceae followed closely by Pseudomonas species. The detection of Candida species in 15% of the isolates in the present study is also consistent to some extent with the studies of Pittet and Wenzel[23] and Edgeworth et al.,[24] who have reported that fungal pathogens are also becoming increasingly common among patients with nosocomial bloodstream infections.
Intensive care unit acquired infections have been reported to be associated with increased length of ICU and hospital stays.[25] Correa and Pittet[26] reported an additional cost of about $3.5 billion/year due to ICU acquired infections. The findings in the present study are corroborative. Crude mortality rates associated with nosocomial infection vary from 12% to 80%, dependent on the population studied and the definitions used.[20] Whereas some studies do report increased mortality associated with nosocomial infections,[27,28] other studies, like those of Rello et al.,[29] have not shown higher mortality, emphasizing the problems in defining cause-effect relationship in these individuals. In the study by Rosenthal et al.,[30] crude mortality rate for patients with device associated infections ranged from 35.2% (for central venous catheter associated blood stream infection) to 44.9% (for VAP). In the present study there was a trend, but no statistically significant difference in ICU mortality rate in the patients with compared to those without nosocomial infection despite a significantly greater proportion of infection patients falling in the higher APACHE II category. A probable explanation for the lack of difference could be a variation in the baseline severity of illness mentioned before and described by Vincent.[20] Another factor that may have prevented the trend from becoming statistically significant is the relatively small number of deaths in both arms observed over the 6-month study period. A longer study may have produced more deaths leading to the observed difference becoming statistically significant.
Although there is a plethora of studies detailing the risk factors for various type of nosocomial infections in various groups of patients, more commonly identified risk factors can be divided into four groups: (a) Those related to underlying health impairment; (b) those related to the acute disease process; (c) those related to use of invasive procedures and (d) those related to other treatment modalities. Diverse studies have described various features of underlying health impairment, like chronic lung disease,[31] immunocompromise, increased age,[14] malnutrition,[32] etc., as independent risk factors for nosocomial infections. It has been reported in some studies[17,33] that the risk of developing nosocomial infections increased with high APACHE II score. Invasive device utilization like central venous or urinary catheterization, intubation, tracheostomy and mechanical ventilation have been reported as significant risk factors for infection in many studies.[13,17,18,33] The EPIC II study[13] reported medical admission, admission after emergency surgery or trauma, referral from the hospital floor, emergency room, or other hospital, the presence of chronic obstructive pulmonary disease, cancer, HIV, older age, mechanical ventilation, renal replacement therapy and greater SAPS II score were found to be independently associated with a higher risk of infection. The findings in this study are partly in agreement with earlier studies.[27,33]
Conclusion
In this prospective observational study, nosocomial infections were diagnosed in 11.98% of the patients. Nosocomial pneumonia (both ventilator and nonventilator associated) was the most frequently detected infection, followed by urinary tract and central venous catheter associated bloodstream infections. Length of ICU stay, prior antimicrobial therapy and urinary catheterization were found to be significant risk factors associated with the acquisition of nosocomial infections. Gram-negative Enterobacteriaceae, as a group, were the most frequently isolated pathogens, while P. aeruginosa was the single most frequent causative organism. The acquisition of nosocomial infections in the ICU resulted in significantly increased length of ICU and hospital stay, but did not result in statistically significant increase in ICU or hospital mortality.
These findings can now be utilized toward planning a surveillance program for nosocomial infection in our ICU setting as a first step toward a better infection control strategy.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988;16:128–40. doi: 10.1016/0196-6553(88)90053-3. [DOI] [PubMed] [Google Scholar]
- 2.Ewans TM, Ortiz CR, LaForce FM. Prevention and control of nosocomial infection in the intensive care unit. In: Irwin RS, Cerra FB, Rippe JM, editors. Intensive Care Medicine. 4th ed. New York: Lippincot-Ravan; 1999. pp. 1074–80. [Google Scholar]
- 3.House of Commons Committee of Public Accounts. The management and control of hospital acquired infection in acute NHS trusts in England. [Last accessed on 2003 Feb 19]. Available from: http://www.publications.parliament.uk/pa/cm199900/cmpubacc/306/30603.htm .
- 4.Haley RW, Culver DH, White JW, Morgan WM, Emori TG, Munn VP, et al. The efficacy of infection surveillance and control programs in preventing nosocomial infections in US hospitals. Am J Epidemiol. 1985;121:182–205. doi: 10.1093/oxfordjournals.aje.a113990. [DOI] [PubMed] [Google Scholar]
- 5.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: A severity of disease classification system. Crit Care Med. 1985;13:818–29. [PubMed] [Google Scholar]
- 6.Horan TC, Gaynes RP. Surveillance of nosocomial infections. In: Mayhall CG, editor. Hospital Epidemiology and Infection Control. 3rd ed. Philadelphia: Lippincott Williams and Wilkins; 2004. pp. 1659–702. [Google Scholar]
- 7.CDC/NHSN surveillance definition of healthcare-associated infection and criteria for specific types if infections in the acute care setting. [Last accessed on 2003 Feb 19]. Available from: http://www.cdc.gov/nhsn/PDFs/pscManual/17pscManual/17pscNosInfDef-current.pdf .
- 8.Collee JG, Marr W. Culture of bacteria. In: Collee JG, Fraser AG, Marmion BP, Simmons A, editors. Mackie and McCartney Practical Medical Microbiology. 14th ed. Philadelphia: Churchill Livingstone; 1999. pp. 113–29. [Google Scholar]
- 9.Collee JG, Miles RS, Watt B. Tests for the identification of bacteria. In: Collee JG, Fraser AG, Marmion BP, Simmons A, editors. Mackie and McCartney Practical Medical Microbiology. 14th ed. Philadelphia: Churchill Livingstone; 1999. pp. 131–49. [Google Scholar]
- 10.Milne LJ. In: Mackie and McCartney Practical Medical Microbiology. 14th ed. Collee JG, Fraser AG, Marmion BP, Simmons A, editors. Philadelphia: Churchill Livingstone; 1999. pp. 695–717. [Google Scholar]
- 11.Gastmeier P, Sohr D, Just HM, Nassauer A, Daschner F, Rüden H. How to survey nosocomial infections. Infect Control Hosp Epidemiol. 2000;21:366–70. doi: 10.1086/501774. [DOI] [PubMed] [Google Scholar]
- 12.Alberti C, Brun-Buisson C, Burchardi H, Martin C, Goodman S, Artigas A, et al. Epidemiology of sepsis and infection in ICU patients from an international multicentre cohort study. Intensive Care Med. 2002;28:108–21. doi: 10.1007/s00134-001-1143-z. [DOI] [PubMed] [Google Scholar]
- 13.Vincent JL, Rello J, Marshall J, Siva E, Anzueto A, Martin CD, et al. The extended prevalence of infection in the ICU study: EPIC II. JAMA. 2009;302:2323–9. doi: 10.1001/jama.2009.1754. [DOI] [PubMed] [Google Scholar]
- 14.Rebollo MH, Bernal JM, Llorca J, Rabasa JM, Revuelta JM. Nosocomial infections in patients having cardiovascular operations: A multivariate analysis of risk factors. J Thorac Cardiovasc Surg. 1996;112:908–13. doi: 10.1016/S0022-5223(96)70090-9. [DOI] [PubMed] [Google Scholar]
- 15.Papia G, McLellan BA, El-Helou P, Louie M, Rachlis A, Szalai JP, et al. Infection in hospitalized trauma patients: Incidence, risk factors, and complications. J Trauma. 1999;47:923–7. doi: 10.1097/00005373-199911000-00018. [DOI] [PubMed] [Google Scholar]
- 16.Gaynes RP. Surveillance of nosocomial infections: A fundamental ingredient for quality. Infect Control Hosp Epidemiol. 1997;18:475–8. doi: 10.1086/647651. [DOI] [PubMed] [Google Scholar]
- 17.Erbay H, Yalcin AN, Serin S, Turgut H, Tomatir E, Cetin B, et al. Nosocomial infections in intensive care unit in a Turkish university hospital: A 2-year survey. Intensive Care Med. 2003;29:1482–8. doi: 10.1007/s00134-003-1788-x. [DOI] [PubMed] [Google Scholar]
- 18.Richards MJ, Edwards JR, Culver DH, Gaynes RP. Nosocomial infections in medical infections surveillance system. Crit Care Med. 1999;27:887–92. doi: 10.1097/00003246-199905000-00020. [DOI] [PubMed] [Google Scholar]
- 19.Richards MJ, Edwards JR, Culver DH, Gaynes RP. Nosocomial infections in combined medical-surgical intensive care units in the United States. Infect Control Hosp Epidemiol. 2000;21:510–5. doi: 10.1086/501795. [DOI] [PubMed] [Google Scholar]
- 20.Vincent JL. Nosocomial infections in adult intensive-care units. Lancet. 2003;361:2068–77. doi: 10.1016/S0140-6736(03)13644-6. [DOI] [PubMed] [Google Scholar]
- 21.Friedman G, Silva E, Vincent JL. Has the mortality of septic shock changed with time. Crit Care Med. 1998;26:2078–86. doi: 10.1097/00003246-199812000-00045. [DOI] [PubMed] [Google Scholar]
- 22.Edmond MB, Wallace SE, McClish DK, Pfaller MA, Jones RN, Wenzel RP. Nosocomial bloodstream infections in United States hospitals: A three-year analysis. Clin Infect Dis. 1999;29:239–44. doi: 10.1086/520192. [DOI] [PubMed] [Google Scholar]
- 23.Pittet D, Wenzel RP. Nosocomial bloodstream infections. Secular trends in rates, mortality, and contribution to total hospital deaths. Arch Intern Med. 1995;155:1177–84. doi: 10.1001/archinte.155.11.1177. [DOI] [PubMed] [Google Scholar]
- 24.Edgeworth JD, Treacher DF, Eykyn SJ. A 25-year study of nosocomial bacteremia in an adult intensive care unit. Crit Care Med. 1999;27:1421–8. doi: 10.1097/00003246-199908000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Pittet D, Tarara D, Wenzel RP. Nosocomial bloodstream infection in critically ill patients. Excess length of stay, extra costs, and attributable mortality. JAMA. 1994;271:1598–601. doi: 10.1001/jama.271.20.1598. [DOI] [PubMed] [Google Scholar]
- 26.Correa L, Pittet D. Problems and solutions in hospital-acquired bacteraemia. J Hosp Infect. 2000;46:89–95. doi: 10.1053/jhin.2000.0803. [DOI] [PubMed] [Google Scholar]
- 27.Appelgren P, Hellström I, Weitzberg E, Söderlund V, Bindslev L, Ransjö U. Risk factors for nosocomial intensive care infection: A long-term prospective analysis. Acta Anaesthesiol Scand. 2001;45:710–9. doi: 10.1034/j.1399-6576.2001.045006710.x. [DOI] [PubMed] [Google Scholar]
- 28.Craven DE, Kunches LM, Lichtenberg DA, Kollisch NR, Barry MA, Heeren TC, et al. Nosocomial infection and fatality in medical and surgical intensive care unit patients. Arch Intern Med. 1988;148:1161–8. [PubMed] [Google Scholar]
- 29.Rello J, Ochagavia A, Sabanes E, Roque M, Mariscal D, Reynaga E, et al. Evaluation of outcome of intravenous catheter-related infections in critically ill patients. Am J Respir Crit Care Med. 2000;162:1027–30. doi: 10.1164/ajrccm.162.3.9911093. [DOI] [PubMed] [Google Scholar]
- 30.Rosenthal VD, Maki DG, Salomao R, Moreno CA, Mehta Y, Higuera F, et al. Device-associated nosocomial infections in 55 intensive care units of 8 developing countries. Ann Intern Med. 2006;145:582–91. doi: 10.7326/0003-4819-145-8-200610170-00007. [DOI] [PubMed] [Google Scholar]
- 31.Torres A, Aznar R, Gatell JM, Jiménez P, González J, Ferrer A, et al. Incidence, risk, and prognosis factors of nosocomial pneumonia in mechanically ventilated patients. Am Rev Respir Dis. 1990;142:523–8. doi: 10.1164/ajrccm/142.3.523. [DOI] [PubMed] [Google Scholar]
- 32.Hanson LC, Weber DJ, Rutala WA. Risk factors for nosocomial pneumonia in the elderly. Am J Med. 1992;92:161–6. doi: 10.1016/0002-9343(92)90107-m. [DOI] [PubMed] [Google Scholar]
- 33.Ponce de León-Rosales SP, Molinar-Ramos F, Domínguez-Cherit G, Rangel-Frausto MS, Vázquez-Ramos VG. Prevalence of infections in intensive care units in Mexico: A multicenter study. Crit Care Med. 2000;28:1316–21. doi: 10.1097/00003246-200005000-00010. [DOI] [PubMed] [Google Scholar]


