Abstract
Acute liver failure (ALF) is a life-threatening illness, where a previously normal liver fails within days to weeks. Sudden loss of synthetic and detoxification function of liver results in jaundice, encephalopathy, coagulopathy, and multiorgan failure. The etiology of ALF varies demographically. The mortality of ALF is as high as 40–50%. The initial care of patients with ALF depends on prompt recognition of the condition and early detection of etiology. Management includes intensive care support, treatment of specific etiology if present and early detection of candidates for liver transplantation. Liver transplantation remains the only therapeutic intervention with proven survival benefit in patients with irreversible ALF. Living related liver transplantation, auxiliary liver transplantation, and ABO-incompatible liver transplantation are coming up in a big way. Liver assist devices and hepatocyte transplant remain experimental and further advances are required. Public health measures to control hepatitis A, B, E, and drug-induced liver injury will reduce the incidence and mortality of ALF.
Keywords: Acute liver failure, fulminant liver failure, hepatocyte transplantation liver assist devices, liver transplantation, molecular adsorbents recirculation system
Introduction
Acute liver failure (ALF) is a life-threatening illness, where a previously normal liver fails within days to weeks. Sudden loss of synthetic and detoxification function of liver results in jaundice, encephalopathy, coagulopathy, and multiorgan failure.[1,2] The incidence of ALF in developed world is between one and six cases per million people per year.[3] Incidence may be higher in developing world, but data are lacking.[2] The etiology of ALF varies demographically. In India, Acute viral hepatitis is the most common cause of ALF.[4,5] The mortality of ALF is as high as 40-50% and causes of death in ALF include brain herniation due to raised intracranial pressure (35%) and sepsis with multiorgan failure.[2] Liver transplantation remains the only therapeutic intervention with proven survival benefit in patients with irreversible ALF.[1]
Definition
In 1970, Trey and Davidson defined “fulminant hepatic failure” as a severe liver injury potentially reversible in nature and with the onset of hepatic encephalopathy within 8 weeks of first symptoms in the absence of preexisting liver disease.[6] In 1993, O'Grady et al. based on data from King's College subdivided ALF into hyperacute, acute, and subacute presentation depending on the interval from onset of disease to onset of encephalopathy.[7] Hyperacute when altered mental status occurs within 7 days of onset of jaundice, acute when altered mental state occurs between 7 and 21 days of onset of jaundice and subacute when altered mental state occurs between 21 days and 26 weeks of onset of jaundice.[7] The most widely accepted definition is by American association of study of liver disease who in 2005 defined ALF as a clinical syndrome characterized by evidence of coagulopathy (international normalised ratio [INR] >5) and any degree of altered mental status in a patient without preexisting liver disease and duration of illness <26 weeks.[8] Patients with Wilson's disease, vertically acquired hepatitis B, and autoimmune hepatitis may be included in spite of possibility of underlying liver disease.[8]
Etiology
Acute liver failure is the culmination of severe liver cell injury from a variety of causes including viral hepatitis, toxins, metabolic disorders, and vascular insults.[9] The etiology varies with geography. In India, viral hepatitis A and E are the most common cause for ALF.[4,5] In the west, toxic etiologies predominate.[9] About 15-22% of ALF occur without any identifiable cause.[10]
Viral Hepatitis
Hepatotrophic viruses are the most common cause of ALF in developing countries.[9,10] Hepatitis A and E viruses are transmitted via faeco-oral route and are common in India.[4,5] ALF occurs in <1% of cases of acute hepatitis A. Hepatitis A related ALF has a better prognosis (70% spontaneous survival) than ALF due to other causes.[11,12] Mortality usually occurs in elderly and those with underlying chronic liver disease.[13] ALF due to hepatitis E has a worse outcome in elderly, pregnant women, and patients with underlying chronic liver disease.[14] Vertical transmission of hepatitis E from women with acute infection leads to ALF in 50% of neonates.[14]
Hepatitis B spreads vertically or horizontally by contact with blood or blood products of an infected individual. ALF due to hepatitis B can occur not only from acute de novo infection but also from flare of a chronic infection.[15,16] Flares of chronic hepatitis B can be spontaneous, but more commonly due to treatment induced immunosuppression.[15,16] Flares of hepatitis B have higher mortality, and early identification of patients at risk and initiation of antiviral treatment reduces mortality. Acute hepatitis C rarely causes ALF. Other viral causes of ALF include herpes simplex virus 1 and 2, varicella-zoster virus, cytomegalovirus, yellow fever, and parvovirus B19.[12]
Drugs and Toxins
Drugs are the most common cause of ALF in the west.[12,16] Drug-induced liver injury may be dose-dependent and predictable as in Acetaminophen toxicity. ALF due to acetaminophen can occur if a large dose (150 mg/kg) is consumed as in deliberate self-poisoning.[17] It can also occur with substantial drug ingestion over hours to days as occurs in unintentional poisoning.[37] Malnutrition and alcoholism are risk factors for acetaminophen-induced liver injury.[17] Other form of drug-induced liver injury is idiosyncratic drug reaction. It is often unpredictable and independent of dose.[18] Unlike other causes of ALF, drug-induced ALF is more common in elderly. High mortality is seen with very high bilirubin, high aminotransferases, and advanced age.[19] Herbal medications and dietary supplements have also been associated with ALF.
Metabolic Causes
Wilson's disease accounts for 6-12% of cases of ALF. ALF due to Wilson disease occurs mainly in young females. It should be suspected when patient has very high serum bilirubin and low alkaline phosphatase at presentation.[20] Hemolysis, elevated liver enzymes, low platelet syndrome, and acute fatty liver of pregnancy are two overlapping syndromes occurring in the second half of pregnancy.[21] Early diagnosis and prompt delivery are critical in achieving good outcomes.
Vascular Causes
Acute Budd-Chiari syndrome can rarely present as ALF.[12] Early recognition and prompt treatment can result in good recovery. Ischemic liver injury occurs in setting of cardiac arrest or intractable hypotension. Here, the aminotransferases will be markedly elevated and responds dramatically to stabilization of circulatory problem.[22]
Miscellaneous Causes
Acute liver failure occurs in <20% of autoimmune hepatitis. Presence of autoantibodies and a compatible picture on biopsy helps to make a diagnosis.[23] Amanita Phalloides mushrooms, heat stroke, and malignant infiltration of the liver are a rare causes of liver injury.[12]
Clinical Manifestations
The diagnosis of ALF is based on the triad of Jaundice, altered metal status, and coagulopathy.[1,2] The initial manifestation of ALF is nonspecific with anorexia, fatigue, abdominal pain, and fever. With advancing liver injury signs of ALF emerge. Patient develops jaundice, encephalopathy, coagulopathy, hemodynamic instability, acute renal failure, ascites, lung injury, sepsis, and metabolic abnormalities.[25] Rarely, ALF may be confused with systemic illness that manifest with jaundice and altered sensorium such as severe sepsis, systemic lupus erythematosus, Thrombotic thrombocytopenic purpura and disseminated intravascular coagulation.[26] At times, it may be difficult to differentiate severe sepsis from ALF and measurement of factor VIII levels may help. Factor VIII levels are low in sepsis while it is normal in patients with ALF.[26] In tropical countries like India, the differential diagnosis of ALF should include severe infections with Plasmodium Malaria, Dengue fever, Leptospirosis, Rickettsial infections, Enteric hepatitis, Hepatic tuberculosis, Amoebic liver abscess.[27] Early recognition of these conditions is essential as specific therapies can cure most of these conditions.
Management
General consideration
Management consists of intensive care support, treatment of specific etiology if present and early detection of candidates for liver transplantation.[1,2] Special attention should be given to coma care, fluid management, hemodynamics, metabolic parameters, and infection control. Coagulation parameters complete blood count, metabolic panel, and arterial blood gases should be checked frequently.[3] Early restoration of intravascular volume and systemic perfusion can prevent multiorgan failure.[1] In patients who continue to be hypotensive in spite of adequate volume replacement, vasopressors should be used.[25] Patients with grade III or IV coma should be intubated and sedated to facilitate general care and prevent aspiration pneumonia.[25] ALF is a state of functional immunosuppression carries a high risk for sepsis. High standards of infection control should be practiced. Frequent sputum, blood and urine culture should be done to detect infection early. Broad spectrum antibiotics may be administered preemptively in patients with coagulopathy, grade III or IV encephalopathy or multiorgan failure.[1,10] Overt bleeding is uncommon in ALF. The administration of coagulation factors should be avoided except to treat bleeding or before invasive procedures.[1]
Etiology specific therapy
Depending on the etiology, specific therapies may be effective. Such treatment should be started early in the course of the disease, and careful assessment of disease progression is necessary to prevent delay or failure to successful liver transplantation.[1,2] N-acetyl cysteine, when administered early, can reduce liver damage and hasten recovery in patients with acetaminophen-induced ALF.[28] A multicenter, double-blind, randomized controlled trial has shown N-acetyl cysteine to be effective in nonacetaminophen ALF.[29] Corticosteroids may be tried in ALF due to autoimmune hepatitis.[30] However, patients not responding within 2 weeks should be listed for transplantation. Antiviral therapy has shown to improve outcome in hepatitis B[31] and herpes simplex related ALF but no randomized controlled trials are available. In patients with Amanita phalloides ingestion, early administration of activated charcoal is recommended as it may improve survival by binding to amatoxin.[24] Other therapies include administration of silibinin and penicillin G.[24] ALF due to Wilson disease typically requires liver transplantation; however, plasma exchange with fresh frozen plasma replacement may improve survival.[20] Pregnancy-related ALF must be treated with prompt delivery of the fetus.[21]
Cerebral edema and encephalopathy
Cerebral edema is present in 25-35% of patients with grade III encephalopathy and in approximately 75% of those with grade IV encephalopathy.[32] Cerebral edema in ALF is caused by a combination of cytotoxic and vasogenic edema.[33,34] Excess ammonia and glutamine alter cerebral osmolality, increase free radical production, alter glucose metabolism, and cause calcium-mediated mitochondrial injury leading to astrocyte swelling.[33,34] Alteration in cerebral blood flow and activation of inflammatory cytokines can aggravate cerebral edema.[34] All patients with encephalopathy should be managed with the head end of the bed elevated to 30°, maintenance of neck neutral position, endotracheal intubation, minimizing painful stimuli and control of arterial hypertension.[33,34] Factors such as hypercapnia, hyponatremia, frequent movements, neck vein compression, fluid overload, fever, hypoxia, coughing, sneezing, seizures, and frequent endotracheal suctioning should be avoided.[33,34] Propofol may be used for sedation and fentanyl for pain.[33] Measures to lower arterial ammonia-like lactulose, gut decontamination and ornithine aspartate has not shown any benefit in ALF and lactulose may aggravate the abdominal distension and bloating.[1] Seizures should be treated with phenytoin or short-acting benzodiazepines.[1,33] There is no role for the prophylactic phenytoin.
The aim of therapy in ALF is to maintain intracerebral pressure (ICP) <20 mm of Hg and cerebral perfusion pressure (CPP) >60 mm of Hg.[35] ICP monitoring may be indicated in a subset of patients.[35] However, a retrospective study on the impact of ICP monitoring did not show any difference in the outcome in two groups. The study concluded that it might be hazardous in the presence of severe coagulopathy.[36] In patients with ICP >20 mm of Hg intravenous mannitol or hypertonic saline should be used to lower ICP and maintain CPP. Therapeutic hypothermia may be used as a bridge to transplant in patients with raised ICP who do not respond to intravenous mannitol or hypertonic saline.[39] A recent systematic review on the use of therapeutic hypothermia in ALF patients concluded that there was limited data on safety and efficacy of moderate hypothermia for treatment of intracranial hypertension in ALF.[37] Hyperventilation to achieve a PaCO2 between 30 and 35 mm of Hg will reduce ICP acutely but should not be used for prolonged periods.[5] Intravenous indomethacin and barbiturates should be used only as the last resort when all other treatments fail to reduce ICP.
Circulatory failure
High blood levels of nitric oxide and cGMP in ALF lead to a state of high cardiac output, low mean arterial pressure and low systemic vascular resistance.[38] This situation is further aggravated by volume depletion due to poor oral intake, extravasation of fluid into the third space, and rarely gastrointestinal bleed. The initial management of hemodynamic instability is fluid resuscitation.[39] In Patients who does not respond to fluid resuscitation, norepinephrine should be used to achieve a mean arterial pressure of 75 mm of Hg.[39] Vasopressin or its analog terlipressin may be used as adjuvant to potentiate the effects of norepinephrine.[39] Adrenal insufficiency should be suspected and corrected in patients who do not respond to fluid resuscitation and vasopressors.
Renal dysfunction
About 50-80% of ALF have renal failure.[40] The etiology of renal failure in ALF is multifactorial. Drug-induced nephrotoxicity; acute tubular necrosis; and abdominal compartment syndrome are the main causes.[40] Every effort should be made to prevent renal failure by improving hemodynamics, avoiding nephrotoxic drugs, and early treatment of infections. In patients who require dialysis a continuous mode of renal replacement therapy should be used.[41]
Infections
Acute liver failure is an immunocompromised state due to dysfunction of monocytes, neutrophils, kupffer cells, and complement system.[42] Most common infections are bacterial pneumonia, urinary tract infection, intravenous catheter-induced sepsis, and spontaneous bacterial peritonitis.[42] Fungal infections occur in 30% of patients with ALF. The most common organism is Candida Albicans. Infections are associated with hemodynamic instability, progression of hepatic encephalopathy and renal failure. But prophylactic antibiotics or antifungals have not been shown to improve outcomes in ALF.[42] However, empirical antibiotics may be used in all patients with grade III or IV encephalopathy or systemic inflammatory response syndrome. Similarly, selective gut decontamination with nonabsorbable antibiotics has not been shown to improve survival in ALF.[42]
Coagulopathy
Decreased synthesis as well as increased consumption of fibrinolytic proteins, anticoagulant proteins and procoagulant factors occurs in ALF. However, overt bleeding is rare in ALF.[43] Stress ulcer prophylaxis with an H2 blocker or proton pump inhibitor is to be given to all patients with ALF. Fresh frozen plasma is indicated only for control of active bleeding or to maintain INR <1.5 when an invasive procedure is planned.[43] Recombinant factor VIIa should be considered when fresh frozen plasma fails to correct INR adequately. Cryoprecipitate is recommended in patients who have hypofibrinogenemia (<1 g/L).[43] Thrombocytopenia should be corrected if platelet count is <10,000 cells/mm3, in the presence of active bleeding or when an invasive procedure is planned.[43]
Metabolic factors
Patients with ALF are prone to develop recurrent hypoglycemia because of glycogen depletion and defective glycogenolysis and gluconeogenesis.[44] Hyperlactatemia can occur because of poor systemic microcirculation as well as due to failure of liver to clear lactate. Hyperlactatemia can aggravate hemodynamic instability and should be treated aggressively.[44] Serum levels of phosphorus, potassium, and magnesium are usually low and should be supplemented. Early enteral feeding should be initiated in all patients and in patients whom enteral feeding is contraindicated parenteral nutrition should be considered.[44]
Prognostic evaluation
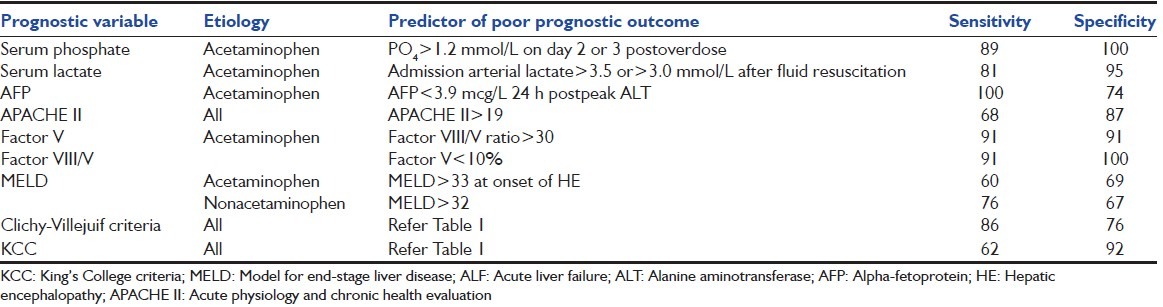
Early identification of patients who require liver transplantation is of great practical importance. The two key factors determining outcome in ALF are etiology and mental status at admission.[45] In general acetaminophen, Hepatitis A, ischemic hepatitis, and pregnancy have 60% short-term survival whereas drug-induced liver injury; autoimmune hepatitis and indeterminate cases have only 30% spontaneous survival.[45] Patients with early grades of encephalopathy at presentation have a better prognosis than those presenting with an advanced coma.[45] Various prognostic evaluation systems have been used to identify candidates for transplantation. The most well-characterized evaluation system till date is King's College criteria [Table 1]. The King's College criterion is used to assess the severity of ALF with a sensitivity of 68–69% and a specificity of 82–92%.[45,46] The other prognostic criteria evaluated include the clichy criteria, acute physiology, and chronic health evaluation-II score, model for end-stage liver disease, sequential organ failure assessment, the ALF study group index, serum lactate, serum phosphorus, factor V and VII/V ratio and alpha-fetoprotein levels [Table 2]. But none of these scoring systems have the sensitivity and specificity to be used in clinical practice.[46] The survival after ALF is multifactorial and depends on etiology, grade of coma on admission, ability to regenerate a healthy liver, and the absence of complications.
Table 1.
Prognostic scoring systems in ALF
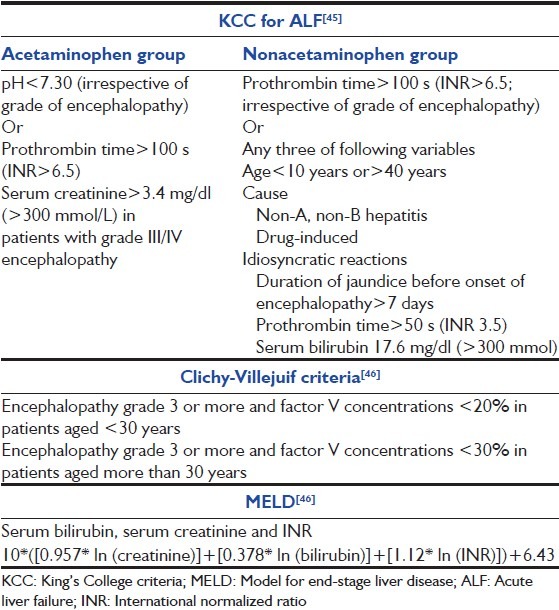
Table 2.
Alternative prognostic variables suggested for use in ALF[46]
Liver transplantation
Orthotopic liver transplantation (OLT) remains the only definite therapy for patients with irreversible liver injury. With OLT, the overall survival of ALF has improved to 60%. The majority of deaths occurs within 3 months of transplant and is due to neurologic complications or sepsis.[46] Living-related liver transplant (LDLT) is common in Asia.[47] For ALF, LDLT may reduce waiting time and provide better timing compared to deceased donor liver transplantation. Recent data from Asia with right lobe LDLT have shown improved survival of adult patients with ALF.[48] ABO incompatible grafts are increasingly being used in acute settings. ABO incompatible grafts have a less favorable outcome with 30–60% 1-year survival.[47] Auxiliary liver transplant retains recipient liver and uses a partial right or left lobe of donor liver as a temporary liver support. Once the native liver recovers immunosuppression is gradually withdrawn and donor liver shrinks. Overall survival for auxiliary liver transplant is 60–65%.[47]
Future
Artificial and bioartificial liver (BAL) support systems are intended to support the patient till his or her liver regenerates or till liver transplantation is available.[49] Artificial liver support systems are filtration and adsorption devices that remove accumulated toxins from the blood. In addition to the removal of water soluble substances, these systems remove lipophilic albumin-bound substances such as bilirubin, bile acids, medium chain fatty acids, metabolites of aromatic amino acids, and cytokines.[49] In BAL devices, hepatocytes in bioreactors come into contact with patient's plasma or blood through a semipermeable membrane. Hepatocytes are derived from animals, discarded human donor liver, or immortalized hepatoma cell lines. BAL combines detoxification with synthetic and regulatory function of hepatocytes.[49] Three major systematic reviews on liver support systems showed it to be safe and resulted in improvement of encephalopathy, however did not show any survival advantage for artificial or BAL support systems in ALF.[49]
Hepatocyte transplantation has been tried in ALF. Here human hepatocytes are infused into the splenic or hepatic portal vascular bed or peritoneal cavity. After translocation into the hepatic sinusoids donor hepatocyte integrates into the liver plates and repopulate the recipient liver.[50] It is successfully used to treat inborn errors of metabolism. Its role in ALF remains controversial. The cell mass infused represents only 5% of liver mass which is insufficient in patients with ALF, and it is difficult to sustain viability and function of hepatocytes in ALF.[50] The reported survival after hepatocyte transplant is 36%.[50] The treatment will probably serve as a bridge to support liver function while awaiting definitive liver transplantation. Two trials are underway to further investigate this.
Summary
Acute liver failure in spite of all advances remains a condition with high mortality. Early identification of ALF and prompt intensive care management is critical improve outcome. Liver transplant remains the only intervention with survival benefit. Liver assist devices and hepatocyte transplant remain experimental and further advances are required. Public health measures to control hepatitis A, B, E, and drug-induced liver injury will reduce the incidence and mortality of ALF.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Bernal W, Wendon J. Acute liver failure. N Engl J Med. 2013;369:2525–34. doi: 10.1056/NEJMra1208937. [DOI] [PubMed] [Google Scholar]
- 2.Lee WM. Acute liver failure. Semin Respir Crit Care Med. 2012;33:36–45. doi: 10.1055/s-0032-1301733. [DOI] [PubMed] [Google Scholar]
- 3.Bower WA, Johns M, Margolis HS, Williams IT, Bell BP. Population-based surveillance for acute liver failure. Am J Gastroenterol. 2007;102:2459–63. doi: 10.1111/j.1572-0241.2007.01388.x. [DOI] [PubMed] [Google Scholar]
- 4.Khuroo MS, Kamili S. Aetiology and prognostic factors in acute liver failure in India. J Viral Hepat. 2003;10:224–31. doi: 10.1046/j.1365-2893.2003.00415.x. [DOI] [PubMed] [Google Scholar]
- 5.Acharya SK, Dasarathy S, Kumer TL, Sushma S, Prasanna KS, Tandon A, et al. Fulminant hepatitis in a tropical population: Clinical course, cause, and early predictors of outcome. Hepatology. 1996;23:1448–55. doi: 10.1002/hep.510230622. [DOI] [PubMed] [Google Scholar]
- 6.Trey C, Davidson CS. The management of fulminant hepatic failure. Prog Liver Dis. 1970;3:282–98. [PubMed] [Google Scholar]
- 7.O'Grady JG, Schalm SW, Williams R. Acute liver failure: Redefining the syndromes. Lancet. 1993;342:273–5. doi: 10.1016/0140-6736(93)91818-7. [DOI] [PubMed] [Google Scholar]
- 8.Polson J, Lee WM. American association for the study of liver disease. AASLD position paper: The management of acute liver failure. Hepatology. 2005;41:1179–97. doi: 10.1002/hep.20703. [DOI] [PubMed] [Google Scholar]
- 9.Bernal W, Auzinger G, Dhawan A, Wendon J. Acute liver failure. Lancet. 2010;376:190–201. doi: 10.1016/S0140-6736(10)60274-7. [DOI] [PubMed] [Google Scholar]
- 10.Larson AM. Diagnosis and management of acute liver failure. Curr Opin Gastroenterol. 2010;26:214–21. doi: 10.1097/MOG.0b013e32833847c5. [DOI] [PubMed] [Google Scholar]
- 11.Ichai P, Samuel D. Etiology and prognosis of fulminant hepatitis in adults. Liver Transpl. 2008;14(Suppl 2):S67–79. doi: 10.1002/lt.21612. [DOI] [PubMed] [Google Scholar]
- 12.Willner IR, Uhl MD, Howard SC, Williams EQ, Riely CA, Waters B. Serious hepatitis A: An analysis of patients hospitalized during an urban epidemic in the United States. Ann Intern Med. 1998;128:111–4. doi: 10.7326/0003-4819-128-2-199801150-00006. [DOI] [PubMed] [Google Scholar]
- 13.Vento S, Garofano T, Renzini C, Cainelli F, Casali F, Ghironzi G, et al. Fulminant hepatitis associated with hepatitis A virus superinfection in patients with chronic hepatitis C. N Engl J Med. 1998;338:286–90. doi: 10.1056/NEJM199801293380503. [DOI] [PubMed] [Google Scholar]
- 14.Dalton HR, Bendall R, Ijaz S, Banks M. Hepatitis E: An emerging infection in developed countries. Lancet Infect Dis. 2008;8:698–709. doi: 10.1016/S1473-3099(08)70255-X. [DOI] [PubMed] [Google Scholar]
- 15.Yeo W, Zee B, Zhong S, Chan PK, Wong WL, Ho WM, et al. Comprehensive analysis of risk factors associating with Hepatitis B virus (HBV) reactivation in cancer patients undergoing cytotoxic chemotherapy. Br J Cancer. 2004;90:1306–11. doi: 10.1038/sj.bjc.6601699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reuben A, Koch DG, Lee WM. Acute Liver Failure Study Group. Drug-induced acute liver failure: Results of a U.S. multicenter, prospective study. Hepatology. 2010;52:2065–76. doi: 10.1002/hep.23937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Larson AM, Polson J, Fontana RJ, Davern TJ, Lalani E, Hynan LS, et al. Acetaminophen-induced acute liver failure: Results of a United States multicenter, prospective study. Hepatology. 2005;42:1364–72. doi: 10.1002/hep.20948. [DOI] [PubMed] [Google Scholar]
- 18.Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, et al. Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34.e1. doi: 10.1053/j.gastro.2008.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Björnsson E, Olsson R. Outcome and prognostic markers in severe drug-induced liver disease. Hepatology. 2005;42:481–9. doi: 10.1002/hep.20800. [DOI] [PubMed] [Google Scholar]
- 20.Korman JD, Volenberg I, Balko J, Webster J, Schiodt FV, Squires RH, Jr, et al. Screening for Wilson disease in acute liver failure: A comparison of currently available diagnostic tests. Hepatology. 2008;48:1167–74. doi: 10.1002/hep.22446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joshi D, James A, Quaglia A, Westbrook RH, Heneghan MA. Liver disease in pregnancy. Lancet. 2010;375:594–605. doi: 10.1016/S0140-6736(09)61495-1. [DOI] [PubMed] [Google Scholar]
- 22.Birrer R, Takuda Y, Takara T. Hypoxic hepatopathy: Pathophysiology and prognosis. Intern Med. 2007;46:1063–70. doi: 10.2169/internalmedicine.46.0059. [DOI] [PubMed] [Google Scholar]
- 23.Stravitz RT, Lefkowitch JH, Fontana RJ, Gershwin ME, Leung PS, Sterling RK, et al. Autoimmune acute liver failure: Proposed clinical and histological criteria. Hepatology. 2011;53:517–26. doi: 10.1002/hep.24080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Escudié L, Francoz C, Vinel JP, Moucari R, Cournot M, Paradis V, et al. Amanita phalloides poisoning: Reassessment of prognostic factors and indications for emergency liver transplantation. J Hepatol. 2007;46:466–73. doi: 10.1016/j.jhep.2006.10.013. [DOI] [PubMed] [Google Scholar]
- 25.Stravitz RT, Kramer AH, Davern T, Shaikh AO, Caldwell SH, Mehta RL, et al. Intensive care of patients with acute liver failure: Recommendations of the U.S. acute liver failure study group. Crit Care Med. 2007;35:2498–508. doi: 10.1097/01.CCM.0000287592.94554.5F. [DOI] [PubMed] [Google Scholar]
- 26.Fontana RJ. Acute liver failure. In: Sleisenger MH, Fordtran JS, editors. Gastrointestinal Disease: Pathophysiology, Diagnosis, and Management. 10th ed. Philadelphia: Saunders; 2010. [Google Scholar]
- 27.Deepak NA, Patel ND. Differential diagnosis of acute liver failure in India. Ann Hepatol. 2006;5:150–6. [PubMed] [Google Scholar]
- 28.Smilkstein MJ, Knapp GL, Kulig KW, Rumack BH. Efficacy of oral N-acetylcysteine in the treatment of acetaminophen overdose. Analysis of the national multicenter study (1976-1985) N Engl J Med. 1988;319:1557–62. doi: 10.1056/NEJM198812153192401. [DOI] [PubMed] [Google Scholar]
- 29.Lee WM, Hynan LS, Rossaro L, Fontana RJ, Stravitz RT, Larson AM, et al. Intravenous N-acetylcysteine improves transplant-free survival in early stage non-acetaminophen acute liver failure. Gastroenterology. 2009;137:856–64.e1. doi: 10.1053/j.gastro.2009.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Czaja AJ. Corticosteroids or not in severe acute or fulminant autoimmune hepatitis: Therapeutic brinksmanship and the point beyond salvation. Liver Transpl. 2007;13:953–5. doi: 10.1002/lt.21088. [DOI] [PubMed] [Google Scholar]
- 31.Miyake Y, Iwasaki Y, Takaki A, Fujioka S, Takaguchi K, Ikeda H, et al. Lamivudine treatment improves the prognosis of fulminant hepatitis B. Intern Med. 2008;47:1293–9. doi: 10.2169/internalmedicine.47.1061. [DOI] [PubMed] [Google Scholar]
- 32.Scott TR, Kronsten VT, Hughes RD, Shawcross DL. Pathophysiology of cerebral oedema in acute liver failure. World J Gastroenterol. 2013;19:9240–55. doi: 10.3748/wjg.v19.i48.9240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang DW, Yin YM, Yao YM. Advances in the management of acute liver failure. World J Gastroenterol. 2013;19:7069–77. doi: 10.3748/wjg.v19.i41.7069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pyleris E, Giannikopoulos G, Dabos K. Pathophysiology and management of acute liver failure. Ann Gastroenterol. 2010;23:257–65. [Google Scholar]
- 35.Shawcross DL, Wendon JA. The neurological manifestations of acute liver failure. Neurochem Int. 2012;60:662–71. doi: 10.1016/j.neuint.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 36.Vaquero J, Fontana RJ, Larson AM, Bass NM, Davern TJ, Shakil AO, et al. Complications and use of intracranial pressure monitoring in patients with acute liver failure and severe encephalopathy. Liver Transpl. 2005;11:1581–9. doi: 10.1002/lt.20625. [DOI] [PubMed] [Google Scholar]
- 37.Larsen FS, Murphy N, Bernal WL. Prophylactic effect of mild hypothermia to prevent brain edema in patients with acute liver failure: Results of a multicenter, randomized, controlled trial. J Hepatol. 2011;54:S26. doi: 10.1016/j.jhep.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 38.Siniscalchi A, Dante A, Spedicato S, Riganello L, Zanoni A, Cimatti M, et al. Hyperdynamic circulation in acute liver failure: Reperfusion syndrome and outcome following liver transplantation. Transplant Proc. 2010;42:1197–9. doi: 10.1016/j.transproceed.2010.03.097. [DOI] [PubMed] [Google Scholar]
- 39.Lee WM, Stravitz RT, Larson AM. Introduction to the revised American Association for the Study of Liver Diseases Position Paper on acute liver failure 2011. Hepatology. 2012;55:965–7. doi: 10.1002/hep.25551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang DW, Yin YM, Yao YM. Advances in the management of acute liver failure. World J Gastroenterol. 2013;19:7069–77. doi: 10.3748/wjg.v19.i41.7069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Davenport A. Continuous renal replacement therapies in patients with liver disease. Semin Dial. 2009;22:169–72. doi: 10.1111/j.1525-139X.2008.00539.x. [DOI] [PubMed] [Google Scholar]
- 42.Leber B, Spindelboeck W, Stadlbauer V. Infectious complications of acute and chronic liver disease. Semin Respir Crit Care Med. 2012;33:80–95. doi: 10.1055/s-0032-1301737. [DOI] [PubMed] [Google Scholar]
- 43.Agarwal B, Wright G, Gatt A, Riddell A, Vemala V, Mallett S, et al. Evaluation of coagulation abnormalities in acute liver failure. J Hepatol. 2012;57:780–6. doi: 10.1016/j.jhep.2012.06.020. [DOI] [PubMed] [Google Scholar]
- 44.Wang DW, Yin YM, Yao YM. Advances in the management of acute liver failure. World J Gastroenterol. 2013;19:7069–77. doi: 10.3748/wjg.v19.i41.7069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.O'Grady JG, Alexander GJ, Hayllar KM, Williams R. Early indicators of prognosis in fulminant hepatic failure. Gastroenterology. 1989;97:439–45. doi: 10.1016/0016-5085(89)90081-4. [DOI] [PubMed] [Google Scholar]
- 46.Neuberger J, Gimson A, Davies M, Akyol M, O'Grady J, Burroughs A, et al. Selection of patients for liver transplantation and allocation of donated livers in the UK. Gut. 2008;57:252–7. doi: 10.1136/gut.2007.131730. [DOI] [PubMed] [Google Scholar]
- 47.Petrowsky H, Busuttil RW. Evolving surgical approaches in liver transplantation. Semin Liver Dis. 2009;29:121–33. doi: 10.1055/s-0029-1192060. [DOI] [PubMed] [Google Scholar]
- 48.Liu CL, Fan ST, Lo CM, Yong BH, Fung AS, Wong J. Right-lobe live donor liver transplantation improves survival of patients with acute liver failure. Br J Surg. 2002;89:317–22. doi: 10.1046/j.0007-1323.2001.02035.x. [DOI] [PubMed] [Google Scholar]
- 49.Struecker B, Raschzok N, Sauer IM. Liver support strategies: Cutting-edge technologies. Nat Rev Gastroenterol Hepatol. 2014;11:166–76. doi: 10.1038/nrgastro.2013.204. [DOI] [PubMed] [Google Scholar]
- 50.Hughes RD, Mitry RR, Dhawan A. Current status of hepatocyte transplantation. Transplantation. 2012;93:342–7. doi: 10.1097/TP.0b013e31823b72d6. [DOI] [PubMed] [Google Scholar]


