Abstract
Insertion of central venous catheter (CVC) is the most common procedure to be performed in Intensive Care Units. Addition of ultrasonographic guidance to this procedure, which was initially performed blindly, has improved safety of this procedure. Confirmation of endovenous placement of CVC though, is tricky, as methods for confirmation are either operator dependent, time-consuming or not available at bedside. Prospective observational study was carried out to study feasibility of use of sonobubble test to confirm the presence of CVC within central vein. After insertion of CVC in the internal jugular, subclavian or axillary vein, a 10 ml bolus of shaken saline microbubble is injected through port of CVC, and opacification of right atrium is observed in xiphoid view on ultrasonography. The Sonobubble test was helpful for dynamic confirmation of endovenous placement of CVC and prevented complications such as arterial puncture and cannulation. We recommend its use following CVC insertion.
Keywords: Bubble test, central venous catheter, ultrasonography
Introduction
Ultrasonographic (USG) guidance for the insertion of central venous catheter (CVC) is now almost a standard of care, leading to fewer failed attempts and complications.[1] However, the risk of inadvertent puncture of surrounding structure persists. Carotid artery puncture and/or cannulation may occur even if proper precautions are taken, sometimes with disastrous consequences.[2] Performing a USG “bubble test” as described previously by a few authors will confirm the endovenous presence of the catheter, thus preventing accidental or inadvertent arterial cannulation with no significant drawback.[3] But there are no reports about the use of such a test in Indian Intensive Care Unit (ICUs). The test appears simple, but there may be certain problems unique to Indian ICUs, which may not be obvious in western reports about this test. Presence of USG machine in ICU, presence of the person trained in use of USG, etc., may be some of the problems encountered in Indian ICUs. This study was undertaken to increase awareness of such a simple test which can be performed by any intensivist with little training in the use of USG. The test does not require any additional equipment, thus not adding to the cost of CVC insertion. We studied feasibility of use of the bubble test to confirm the presence of CVC inside the internal jugular, subclavian or axillary vein and how it compared with already existing methods for checking endovenous placement of the CVC.
Subjects and Methods
Prospective observational study of a convenience sample was conducted in 8-bedded surgical intensive care unit (SICU) of our medical college situated in Western India. Approval was obtained from the institutional ethics committee. Written informed consent was taken from all participants. CVC may be inserted with or without USG guidance. However, after insertion of the CVC, USG is needed for performing bubble test. USG thus helped in both insertions of the CVC as well as confirming the endovenous site of the CVC.
All patients who underwent CVC insertion with a real-time USG guidance from April 2013 to January 2014 were included. CVC's were inserted by experienced faculty of our SICU. Ultrasonography was performed on Seimens Sonoline G-60 machine using 10-5 MHz linear transducer by senior faculty of our SICU, especially trained in emergency ultrasound examination and were not the person inserting the CVC.
Central venous catheters were inserted using standard seldinger technique.[4] Confirmation of endovenous placement of CVC was done using “bubble test.” After puncturing vein and cannulating it, a bolus of shaken normal saline microbubble was injected through a 10 ml syringe into distal lumen of the catheter. Immediate opacification of the right atrium is observed by a point-of-care ultrasonography in the four-chamber view or subcostal (Xiphoid) view, confirming endovenous placement of CVC.[3] Endovenous location of CVC was also checked by tube manometry technique.[5]
A stopwatch was started when normal saline filled syringe was attached to the port of CVC. Time taken for performing bubble test was noted. This was until the opacification of the right atrium was noted. Stopwatch was allowed to run further and stopped when chest X-ray was taken or if more than 1 h elapsed after bubble test was completed without chest X-ray being taken. Once the location of the catheter was confirmed, injections and infusions were started through the CVC. Chest X-ray was performed to confirm the position of the tip of the catheter and to see for presence of any other complication, as usual. Data was collected regarding age, sex, diagnosis, indication for central line, site and side of catheterization, time taken to perform “bubble test” and for X-ray confirmation of the position of CVC. Occurrence of any complications, such as arrhythmias, prolonged oozing of blood at puncture site, hematoma, inadvertent carotid artery puncture, pleural puncture with or without pneumothorax or hemothorax, was noted. Bubble test was defined as failed if there was no opacification of the right atrium even 10 s after injection of shaken saline microbubble.
Results
During the study period, 814 patients were admitted to the SICU. Of these, 119 patients underwent CVC insertion. Out of these, 25 patients had a central line inserted under USG guidance. Bubble test was performed in all these 25 patients [Table 1]. Diagnoses of the patients ranged from post-laparotomy status to neck surgery to orthopedic surgery and others [Table 2]. Internal jugular vein (IJV) was cannulated in 20 (80%), subclavian vein in 2 (8%) while axillary vein was cannulated in 3 (12%). Out of 20 patients who had a CVC inserted into the IJV, 19 had it on the right side; whereas 1 had it on the left side. The time taken for performing bubble test ranged from 30 s to 60 s (mean 45 s). Time taken for the postcannulation chest X-ray ranged from 20 min to >1 h. Complications and failure of the bubble test did not occur in any patient. Bubble test was found to be 100% (95% confidence interval 80-100%) sensitive and 100% (95% confidence interval 80-100%) specific for endovenous placement of CVC.
Table 1.
Results
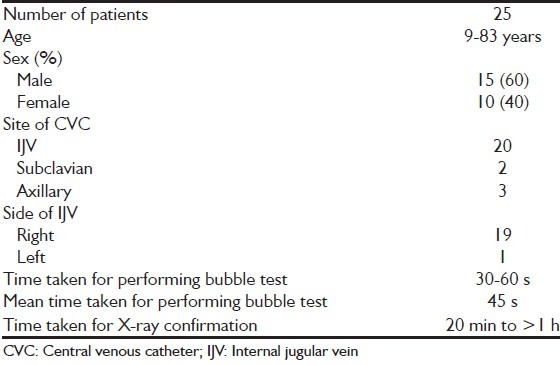
Table 2.
Diagnosis of the patients

Discussion
Central venous catheter insertion is one of the most common procedures performed in the ICU with over 5 million CVC inserted every year in the United States. In our ICU, during the period of study, CVC was inserted in 119 patients. Of these, 25 patients had a CVC inserted under USG guidance. Rest had CVC inserted using landmark technique. USG guidance for CVC insertion was used only when difficulty was anticipated (short neck, difficulty identifying neck structures, presence of coagulopathy/thrombocytopenia) and when person skilled in performing USG was present.
Traditional methods to check endovenous placement of CVC with their advantages and disadvantages[6] are as follows:
-
Aspiration of dark blood: In the syringe after puncture of the vessel
-
Absence of pulsatile flow from syringe hub: It gives an indirect inference that a punctured vessel is not an artery
-
Analysis of blood gases (ABG) of the aspirated blood:[8] Low pO2 and SpO2 may be diagnostic of venous blood
- Pro-may be diagnostic of arterial puncture if both pO2 and SpO2 are high
- Con-time consuming, cumbersome, nondiagnostic sometimes.
-
Analysis of the pressure waveform by pressure transducer:[9] It is an excellent method for confirmation of endovenous placement of CVC and has been included as part of CVC insertion protocol by some.[10] Even then, there is lack of awareness of this technique and is adopted by few
- Pro-more accurate than color and pulsatility of blood in diagnosing arterial puncture, has been shown to reduce incidence of arterial cannulation
- Con-need for assistant and additional equipment, cumbersome, difficult to maintain sterility of the procedural zone.
-
Analysis of the pressure waveform by simple tube manometry:[5,6,11] Using a short, sterile extension tube
- Pro-bedside test, not much additional equipment required
- Con-risk of air embolus in hypovolemic patients.
-
Computerized tomography imaging:
- Pro-accurate
- Con-time consuming, cumbersome, patient needs to be shifted to the radiology department.
Other novel tests include- fluoroscopy, chest radiography with simultaneous injection of contrast, and trans-esophageal echocardiography (TEE) to identify guidewire in the right atrium.[12]
Thus, drawbacks of the traditional methods range from increased costs to significant time delay to not being available bedside. The advantages of the bubble test over these traditional and novel methods are: No extra equipment required or additional cost incurred, can be done without significant increase in procedure time, direct visualization, prevent accidental arterial cannulation and its associated complications.
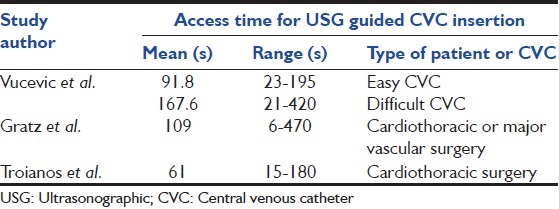
Time taken to place a CVC under USG guidance can range from 6 s to 470 s depending upon the clinical setting in which CVC is inserted[13] [Table 3]. Time taken to perform the bubble test ranged from 30 s to 60 s (mean 45 s). Hence performing bubble test in these patients will not add too much time to overall procedure duration. Another method of confirming endovenous placement (visualization of guidewire within lumen of central vein by USG) is also described which takes less than a minute.[14] Compared with these techniques requiring seconds or a minute, other methods described above to check endovenous placement of CVC (ABG, transducer analysis of pressure waveform, computed tomography-imaging, fluoroscopy, TEE) will need at least from tens of minutes to a few hours to be completed.
Table 3.
Access time for CVC insertion under USG guidance in various studies[13]
Time taken for confirmation of the position of the tip of CVC by Chest X-ray ranged from 20 min to >1 h. Bubble test may eliminate this “confirmatory” chest X-ray, need of which is being questioned, anyway.[15] Hence, administration of drugs as well as intravenous fluids can be started immediately after insertion of the CVC without waiting for confirmation by chest X-ray.
Conclusions
Bubble test offers a dynamic confirmation of endovenous placement of CVC during its insertion under USG guidance. It is easy to perform without consuming too much extra time. There are no known contraindications or complications. Larger studies are needed to decide if it can be performed in all patients who undergo USG guided CVC insertion thus eliminating accidental arterial cannulation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Leung J, Duffy M, Finckh A. Real-time ultrasonographically-guided internal jugular vein catheterization in the emergency department increases success rates and reduces complications: A randomized, prospective study. Ann Emerg Med. 2006;48:540–7. doi: 10.1016/j.annemergmed.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 2.Blaivas M, Adhikari S. An unseen danger: Frequency of posterior vessel wall penetration by needles during attempts to place internal jugular vein central catheters using ultrasound guidance. Crit Care Med. 2009;37:2345–9. doi: 10.1097/CCM.0b013e3181a067d4. [DOI] [PubMed] [Google Scholar]
- 3.Prekker ME, Chang R, Cole JB, Reardon R. Rapid confirmation of central venous catheter placement using an ultrasonographic “Bubble Test”. Acad Emerg Med. 2010;17:e85–6. doi: 10.1111/j.1553-2712.2010.00785.x. [DOI] [PubMed] [Google Scholar]
- 4.Smith RN, Nolan JP. Central venous catheters. BMJ. 2013;347:f6570. doi: 10.1136/bmj.f6570. [DOI] [PubMed] [Google Scholar]
- 5.Ezaru CS, Mangione MP, Oravitz TM, Ibinson JW, Bjerke RJ. Eliminating arterial injury during central venous catheterization using manometry. Anesth Analg. 2009;109:130–4. doi: 10.1213/ane.0b013e31818f87e9. [DOI] [PubMed] [Google Scholar]
- 6.Bowdle A. Arterial cannulation during central line placement: Mechanisms of injury, prevention, and treatment. [Last accessed on 05 Jan 2014]. Available from: http://www.miradorbiomedical.com/wp-content/uploads/2012/01/review_arterial cannulation.pdf .
- 7.Jobes DR, Schwartz AJ, Greenhow DE, Stephenson LW, Ellison N. Safer jugular vein cannulation: Recognition of arterial puncture and preferential use of the external jugular route. Anesthesiology. 1983;59:353–5. [PubMed] [Google Scholar]
- 8.Aghdami A, Ellis R. High oxygen saturation does not always indicate arterial placement of catheter during internal jugular venous cannulation. Anesthesiology. 1985;62:372–3. doi: 10.1097/00000542-198503000-00036. [DOI] [PubMed] [Google Scholar]
- 9.Bowdle A, Kharasch E, Schwid H. Pressure waveform monitoring during central venous catheterization. Anesth Analg. 2009;109:2030–1. doi: 10.1213/ANE.0b013e3181bea01d. [DOI] [PubMed] [Google Scholar]
- 10. [Last accessed on 05 Jan 2014]. Available from: http://www.ihi.org/IHI/Topics/CriticalCare/IntensiveCare/Tools/CentralLineInsertionChecklist.htm .
- 11.Oliver WC, Jr, Nuttall GA, Beynen FM, Raimundo HS, Abenstein JP, Arnold JJ. The incidence of artery puncture with central venous cannulation using a modified technique for detection and prevention of arterial cannulation. J Cardiothorac Vasc Anesth. 1997;11:851–5. doi: 10.1016/s1053-0770(97)90119-1. [DOI] [PubMed] [Google Scholar]
- 12.Arellano R, Nurmohamed A, Rumman A, Day AG, Milne B, Phelan R, et al. The utility of transthoracic echocardiography to confirm central line placement: An observational study. Can J Anaesth. 2014;61:340–6. doi: 10.1007/s12630-014-0111-3. [DOI] [PubMed] [Google Scholar]
- 13.Espinet A, Dunning J. Does ultrasound-guided central line insertion reduce complications and time to placement in elective patients undergoing cardiac surgery. Interact Cardiovasc Thorac Surg. 2004;3:523–7. doi: 10.1016/j.icvts.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 14.Stone MB, Nagdev A, Murphy MC, Sisson CA. Ultrasound detection of guidewire position during central venous catheterization. Am J Emerg Med. 2010;28:82–4. doi: 10.1016/j.ajem.2008.09.019. [DOI] [PubMed] [Google Scholar]
- 15.Lessnau KD. Is chest radiography necessary after uncomplicated insertion of a triple-lumen catheter in the right internal jugular vein, using the anterior approach? Chest. 2005;127:220–3. doi: 10.1378/chest.127.1.220. [DOI] [PubMed] [Google Scholar]


